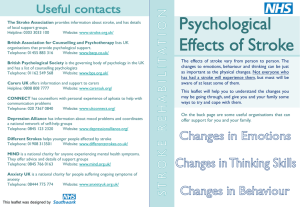
Screening tools for depression after stroke
advertisement

Mood screening after stroke: for people with and without communication difficulties Guidelines, tools and methods and practical issues in screening after stroke Aims of the session • To outline national guidelines for screening patients for issues of mood after experiencing a stroke. • To explore why we screen and assess mood after a stroke: the functions and purpose of screening tool & assessments. • To explore mood screening measures and assessment techniques for people with and without communication problems after stroke. Aims of the session • This session is recommended for those who regularly screen within their role. It covers items in section 5 of the Stroke Specific Skills and Competencies framework, Early and Continuing Rehabilitation: • 5.1.2 Complete screening assessments for (cognitive function) and emotional difficulties, interpret the results and develop intervention plans within the MDT; • 5.1.3 Understand and interpret results of the assessments and feedback the results to the person, the family and the team; • Further in depth assessment approaches are covered in the cognitive section of the training package and in sessions on working with depression and anxiety. Why do we screen? • We screen for mood problems because want to help people! We have learned that untreated psychological problems lead to poor outcomes, including higher mortality rates. • The purpose of screening is therefore to identify those with potential problems who can then be evaluated and monitored further. • A more in depth understanding of the nature of the mood would then be carried out in order to plan treatment. For this a screening tool helps to determine the severity of the problem; • Intervention plans to assist change will be developed based on assessment, preferably with the patient and their family;. • By keeping the patient’s mood under review (RCP, 2012), we can check if the intervention is working; National Guidelines • The RCP national clinical guidelines for stroke 2008 recommends screening and treatment for depression, anxiety and emotionalism, and for cognitive and memory impairment. • National Service Framework for Depression in adults with a chronic health problem (2009) incorporate standards for assessing low mood. • The National Institute for Health and Clinical Excellence (NICE) stroke quality standard 2010 requires that: 'All patients after stroke are screened within 6 weeks of diagnosis, using a validated tool, to identify mood disturbance and cognitive impairment'. National Guidelines • RCP National Clinical Guidelines for Stroke (2012) 4th ed. Recommend that: • Services should adopt a comprehensive approach to the delivery of psychological care after stroke, which should be delivered by using a ‘stepped care’ model from the acute stage to long-term management. • Patients and their carers should have their individual practical and emotional support needs identified before they leave hospital, when rehabilitation ends or at their 6-month review, and annually thereafter. Patients with stroke should be routinely screened for depression anxiety and cognition and intervention plans made and reviewed. Mood Scales There are different types of scales that we can consider for screening, many of which have been validated in stroke. These can include: • • • Mood measures Mood and Anxiety Measures Anxiety measures The tools include some that are designed for people without communication and cognitive problems, and some for people with communication problems. Most scales will be found in the PAAST toolkit. Some tools are presented here as examples. Some scales are self report which can be done as an interview, some are observational. All have scoring criteria. There are many other tools that measure that are available to measure psychological problems such as self esteem, anger, post traumatic reactions. Examples of these are also available in your toolkit but will not be covered here. Screening tools for depression after stroke: Burton 2011 Tools for people without communication problems: Burton 2011 Assessing depression, people with communication problems: Burton 2011 Choosing the tool to suit you? • Has the tool been validated for use with patients with stroke? Sensitive and specific? • How long does it take to administer and score the tool? • What funds are required to purchase the tool? Initial purchase? Cost of record forms? • What level of training is required to administer the tool? • Which tools do other local services use? ESD, IAPT, GPs • Is the tool acceptable and relevant to patients? • Quality standard: Every service should have a protocol across the stroke pathway. Example of a short depression scale: Yale question Two questions: • 1. Prior to your stroke, have you ever felt sad or depressed? (Yes/No) • 2. Since your stroke, have you been feeling sad or depressed? • A further clinical assessment should follow if these two are affirmative, in line with national guidance. • Also be mindful of the range of psychological problems we may face: I might not be depressed but I may be very stressed, or anxious, or angry. Scale example: A depression measure for people with language problems • Depression Intensity Scale Circles (DISCS) If the patient points to this circle (a score of 2), or any higher- this would indicate low mood. SADQ-H: Observation measure for depression for people with language problems The SADQ-H10 requires the rater to score the patient on 10 different behaviours, shown below: 1. Did he/she have weeping spells this week? Every dayOn 4-6 days On 1-4 days Not at all 2. Did he/she have restless disturbed sleep this week? Every dayOn 4-6 days On 1-4 days Not at all 3. Did he/she avoid eye contact when you spoke to him/her? Every dayOn 4-6 day On 1-4 days Not at all 4. Did he/she burst into tears this week? Every dayOn 4-6 days On 1-4 days 5. Not at all Did he/she complain of aches and pains this week? Every dayOn 4-6 days On 1-4 days Not at all Depression measures for people with language problems: observation measure 6. Did he/she get angry this week? Every day On 4-6 days On 1-4 days Not at all 7. Did he/she refuse to participate in social activities this week? Every day On 4-6 days On 1-4 days Not at all 8. Was he/she restless and fidgety this week? Every day On 4-6 days On 1-4 days Not at all Did he/she sit without doing anything this week? Every day On 4-6 days On 1-4 days Not at all 9. 10. Did he/she keep him/herself occupied during the day? Every day On 4-6 days On 1-4 days Not at all Anxiety Scales • A well used scale for measuring anxiety as well as depression is the Hospital Anxiety and Depression Scale (HAD-S) which has items for Anxiety and Depression. • Lincoln, Kneebone, McNiven & Morris, (2012) suggest that a cut off score of 8 on the HADS is more useful for detecting symptoms in patients after stroke. • Scales for anxiety symptoms such as the Beck Anxiety Scale (BAI) can measure the type and severity of anxiety symptoms. • The following slide shows a behavioural observation tool for people with communication problems with norms in development but available to use. Screening for anxiety for those with communication problems Table: Behavioral Outcomes of Anxiety (BOA). Kneebone et al 2012 Often 1. Does he/she appear particularly tense or on edge? 2. Does he /she have a strained face? 3. Does he/she avoid activities or social engagements without good reason? 4. Does he/she appear fearful of falling? 5. Does he/she have trouble falling or staying asleep? 6. Is he/she jumpy or easily startled? 7. Is he/she restless or constantly on the move (e.g. do they pace)? 8. Is he/she easily tired? 9. Does he/she appear anxious? 10. Does he/she appear to panic, or have unusual episodes of breathlessness or hyperventilation? Sometimes Rarely Never Some considerations to bear in mind when we are screening for mood after stroke • Be mindful that some symptoms of stroke such as fatigue, sleep and appetite changes can overlap with mood problems. If these are in your screening tool ask people whether they feel that issue is attributable to the stroke or their mood. • Be aware that you will not get the picture of a persons mood from one screening tool, or on one day: you may have picked them on a “good day” yet the day after that they may be down. People may also be embarrassed to tell you about their mood, and may minimise their symptoms. Further considerations • Stroke-specific cut off points may be required to detect stroke patients who need further evaluation. See Psychological Management of Stroke Lincoln et al, (2012) Wiley-Blackwell. • After a positive screen for mood (if someone is scoring significantly), interview and follow up measures should be used to clarify the nature of the problem and to begin to inform what treatment plans may be followed. This helps people to talk about how they see the problem. • Screening people with aphasia using tools and interviews where possible may be the best approach. • Management plans are crucial, as screening alone does not improve outcome! Good practice when screening people: • Have privacy to talk. • Explain the reasons for assessment and gain consent. • Leave enough time to properly explore the issues, to have an honest conversation about how someone may truly be feeling. • Remember your core listening and communication (warmth, genuineness and empathy) when asking a patient about they are feeling. • Use your clinical judgement to supplement the results. The personal perspective: what is causing the person distress? • If the person can express their opinions it is always a good idea to ask the person how they are feeling, and what is going on for them. That often gives us a bit of an idea of possible problems. You may wish to speak to family members about what is going on and what helps a person. Asking specific questions to identify how someone is feeling at specific times can uncover what they are thinking. • “You/they just looked really worried/down/angry. Can you tell me what went through your mind?” • “Are there any times when you/they particularly anxious or down and when you experience these symptoms?” • “Does anything help?” Good Practice in assessing mood in people with aphasia • Be prepared! (Girl guides), take pen and paper etc • SADQ- asks for observations over the past week • Read the communication assessment results and strategy from SLT • Be aware of the cognitive impression or assessment (OT initial assessment/ SLT assessment results) • Take pictures and scales- e.g. sleeplessness; embarrassment; depression • For questions relating to what makes it better pictures and scales- e.g. music; bath; TV • Use the Top tips for aphasia Mood scale (no visual neglect) I’m feeling… happy okay unhappy I I I 0 5 10 In the last week, I have been mostly… happy okay unhappy I I I 0 5 10 Summary • • • • • • Screening informs treatment by measuring mood. Where problems are indicated further assessment/monitoring is needed; Remember to share the results with the patient/family and with the rehab team, getting ideas from them as to what may help; Discuss the effects of mood on engagement with rehabilitation, possibly changing rehab goals for a while or where/how we deliver rehab; Develop intervention plans and monitor effectiveness of treatment; Have referral and signposting pathways; Give information as to how people can get back in touch or access services for mood related problems when needed. This bears in mind psychological needs can arise at different times post stroke. Pathways can be helpful: • All stroke services should have a mood pathway for screening and providing psychological, using validated screening tools and following national guidance; See: Accelerated Stroke Improvement website: Psychological Care After Stroke for information on screening, protocols adopted by services around the country in assessing mood. http://www.improvement.nhs.uk/stroke/Psychologicalcareafterstro ke/tabid/177/Default.aspx Further reading/information • Psychological Management of Stroke Lincoln, Kneebone, McNiven & Morris, (2012) Wiley-Blackwell • Aphasia Alliance Top Tips for 'Aphasia Friendlier' Communication (Conversations; Public Speaking; Written Communication and Using Pictures) http://www.aphasiatavistocktrust.org/aphasia/alliance/toptips.asp • PAAST manual and toolkit. NECVN.