Education - Carolina Sports Concussion Clinic

Concussion Education
• Tragedy opens the door for education, increased awareness, and law
• In North Carolina…
– Gfeller-Waller Law passed in June 2011
• Three components
– Mandatory education for public middle & high school student-athletes & parents
– Return to play decisions made by qualified medical personnel
– Emergency action plan in place
Objectives
• What is a concussion?
– How does a concussion occur?
– What are the signs & symptoms?
– How should a concussion be treated?
– What if my child isn’t getting better?
– Is there any way to prevent these injuries?
Definition of Concussion
• “A complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces”
– Sports Related Concussion in Pediatric
Athletes, Clinical Pediatrics Volume 47
Number 2 March 2008 106-113
5 Features Used to
Define Concussion
1. Trauma including a direct blow to the head, neck or face, or a blow to another part of the body which transmits an impulsive force to the head
2. Rapid onset of short-lived neurological impairment(s) which resolve over time
3. Acute clinical symptoms of concussion reflecting a functional injury rather than a structural abnormality
4. A graded set of clinical syndromes, which may or may not involve loss of consciousness and which resolve in a sequential course.
5. Typically normal structural neuro-imaging in studies such as MRI or CT scan.
“Basic” Pathophysiology
Signs & Symptoms
• Some might be apparent right away, some may take longer to develop
• Four categories of symptoms to keep in mind
– PHYSICAL
– COGNITIVE
– EMOTIONAL
– SLEEP RELATED
• Headache
– Pressure??
• Nausea
• Vomiting
• Balance difficulties
• Dizziness
– Specifically with position changes
• Fatigue
PHYSICAL
• Sensitivity to light
• Sensitivity to noise
• Feeling out of it or not acting like self
• Hearing problems/ringing in ears
• Vision changes/disturbances
COGNITIVE
• Feeling mentally foggy
• Feeling slowed down or slower than usual
• Difficulty concentrating
• Difficulty remembering
• Confusion
EMOTIONAL
• Sadness
• More emotional than usual
• Irritability
• Nervousness
• What is unusual for your child/player?
Compare their behavior to what his/her
NORMAL is.
SLEEP-RELATED
• Excessive daytime drowsiness
• Sleeping more than usual
• Sleeping less than usual
• Trouble falling asleep
RED FLAGS for Emergent Referral
• Loss of consciousness
• Any suspected cervical spine injury
• Repeated vomiting
• Disorientation
• Slurred speech
• Can’t recognize people or places
• Headache that gets progressively, severely worse
• Increased lethargy
• Facial swelling, significant bruising of the face/head
• Fluid from ears and/or nose
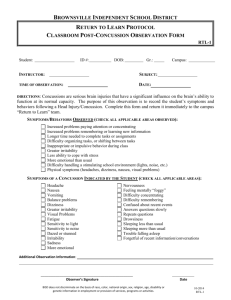
Emergency Action Plan
• Know your organization’s requirements
• Have a plan
• Educate those involved in the plan
• Practice the plan annually
Treatment
• When in doubt, sit them out
– Removal from activity once suspected concussion is sustained IS THE STANDARD
OF CARE
– NFL, NCAA, NCHSAA, NC state law
• See a doctor!
• Cognitive Rest
– Stay home from school?
– Limit homework
– NO TV, computer usage, video games, texting
• Physical Rest
– No return to activity until no symptoms at rest and with cognitive exertion
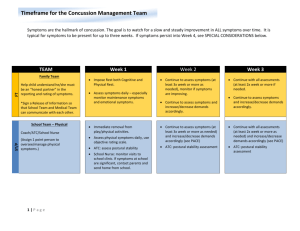
When is it safe to return to play?
• Completely symptom free at rest & with cognitive exertion
• Completely symptom free with physical exertion
– GRADUAL!
– Walk, jog, light weightlifting or push-ups/situps, sport-specific non-contact agilities, contact practice, return to competition
Second Impact Syndrome
• Occurs when a second impact is sustained prior to the complete resolution of all symptoms of concussion
– Loss of autoregulation of cerebral vasculature; rapid, irreversible massive swelling leading to lethal increased intracranial pressure
• Always catastrophic, very often fatal
• Occurs in teenagers
– No documented cases in anyone over the age of 18
Post-Concussion Syndrome
• Three weeks post-injury with little/no resolution of symptoms
– Persistent headaches
– Inability to concentrate
– Any of those symptoms listed earlier that don’t resolve or are exacerbated with any type of cognitive or physical exertion
What if my child isn’t getting better?
• Medication?
• Vestibular therapy?
• Formal neuropsychological testing?
• Gradual, very closely monitored physical exertion?
• Counseling/psych intervention?
– Prolonged symptoms can greatly affect quality of life
Are my players at risk?
• Previous history of concussion
– Once an individual has sustained a concussion, he/she is FOUR TIMES as likely to sustain another injury
– It will take less of a blow each time and symptoms will take longer to resolve
• Diagnosis of ADD/ADHD
• History of headaches or migraines treated by a physician
Prevention
• Education
• Awareness
• Recognition
• Appropriate management
• Rules changes?
• No research supports mouthguards, specific helmets, headbands can prevent this injury from occurring