presentation
advertisement
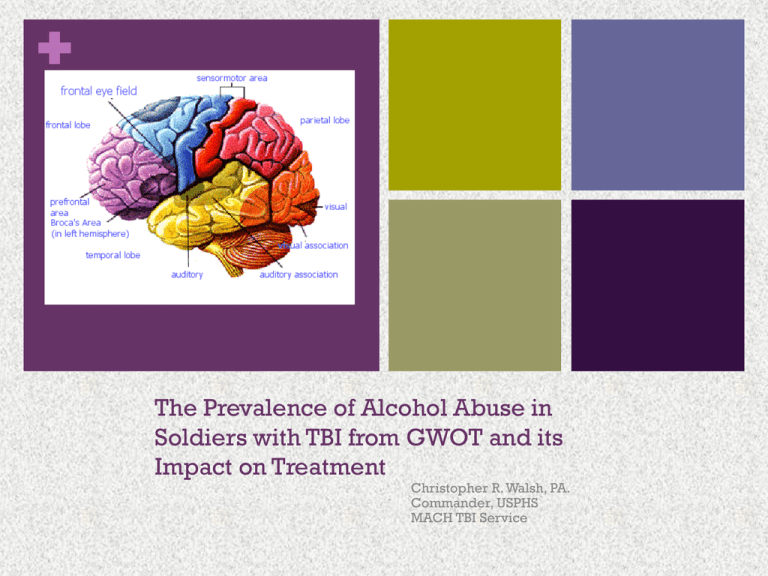
+ The Prevalence of Alcohol Abuse in Soldiers with TBI from GWOT and its Impact on Treatment Christopher R. Walsh, PA. Commander, USPHS MACH TBI Service Disclaimer CDR Walsh has no relevant financial relationships to disclose with any entity associated with this presentation. The opinions and assertions contained in this presentation are the private views of CDR Walsh and do not necessarily reflect the official policies or positions of the Department of Defense or the Department of the Army. OBJECTIVES Describe the incidence of alcohol use among soldiers in both TBI and non-TBI patient pops. Describe the difference alcohol use factors into civilian and military TBI related injuries. Become familiar with common screening instruments that aid in detecting symptoms of TBI and substance abuse. Identify common comorbidities associated with TBI that may factor into increased alcohol use. Describe the challenges that alcohol use presents in recovery from a traumatic brain injury. Presuppositions Alcohol use complicates recovery from TBI. (Corrigan and Lamb-hart, 2004). Alcohol use increases after military combat deployment. (Jacobson et. al, 2008) TBI is the signature wound of the current conflicts in Iraq and Afghanistan, accounting for 70% of injuries seen in theater. (Heltemes et. al, 2011) Alcohol abuse would be more likely in service members who have sustained a TBI. Military mTBI 1.69 million U.S. Military personnel have been deployed more than 2.2 million times to OIF or OEF since the start of military operations in 2001. Head and neck injuries, including severe brain trauma, have been reported in 25% of SM who have been evacuated from Iraq and Afghanistan. mTBI, or concussion, characterized by brief LOC or altered mental status, as a result of deployment-related head injuries, particularly those resulting from proximity to blast explosions may be as high as 18% of returning SM. NEJM Hoge et. Al (2008) + Characteristics of Millennium Cohort participants, Jacobson et. al, 2008 + Prevalence of baseline, follow up, and new onset alcohol use, Jacobson, et. al, 2008. + Adjusted odds of alcohol use among Active-Duty Millennium cohort participants, Jacobson, et. al, 2008. + Adjusted odds for alcohol use among Reserve/Guard Millennium cohort participants, Jacobson, et. al, 2008. Screening for TBI Anyone exposed to or involved in a: Blast Fall Vehicle crash Direct impact Who becomes dazed or confused even momentarily, should be further evaluated for brain injury. DVBIC CPG The difference between civilian and military related TBI injuries Roughly 1.9 million civilian TBIs per year. (Chanras & Eddy, 2008). 235,000 hospital admissions, 50,000 deaths. Mechanisms: falls 28%, MVAs 20%, collision with stationary object 19%, assaults 11%. Up to 75% of civilian TBIs involve alcohol/drug use. Military TBIs typically do not have an alcohol component. Vast majority of military TBIs are blast related. IED Explosion TBI Related Disorders Definition of Military mTBI An injury to the brain resulting from an external force and/or acceleration/deceleration mechanism which causes an alteration in mental status typically resulting in the temporally related onset of symptoms such as: headache, nausea, vomiting, dizziness/balance problems, fatigue, trouble sleeping/sleep disturbances, drowsiness, sensitivity to light/noise, blurred vision, difficulty remembering, and/or difficulty concentrating. LOC of 30 minutes After 30 minutes, and initial GCS 0f 13-15; and PTA not greater than 24 hours ( Diffusion Spectrum Imaging tracks the movement of water molecules as they slide down axons. Red reflects right to left connections; green front to back and blue up and down including links to the spinal cord. ) Screening tools that aid in detecting TBI & SA. 1. WARCAT (Warrior Administered Retrospective Casualty Assessment Tool) 2. PCL-M (PTSD Checklist, Military Version) 3. PHQ-9 (Patient Health Questionnaire 9 items 4. DHI (Dizziness Handicap Inventory) 5. MAST-22 ( Michigan Alcohol Screening Test) 6. CNS Vital Signs 7. RBANS (Repeatable Battery for Assessment of Neuropsych Status 8. ANAM (Automated Neuropsychological Assessment Metrics) + Warrior Administered Retrospective Casualty Assessment Tool + PCL-M + Patient Health Questionnaire + Dizziness Handicap Questionnaire + Michigan Alcohol Screening Test Blast Injuries PRIMARY: Direct exposure to overpressurization wave – velocity >/= 300m/sec (speed of sound of air) SECONDARY: Impact of blast energized debris penetrating and non penetrating TERTIARY: Displacement of the person by the blast and impact QUARTERNARY: Inhalation of toxic fumes, smoke, chemicals Common Comorbidities of TBI and Alcohol Abuse Decreased self-awareness and insight Deficits of memory, attention and concentration Change in Mood and affect Insomnia Vocational/educational problems + Psychiatric Comorbidities of TBI mTBI (i.e., concussion) occurring among soldiers deployed in Iraq is strongly associated with PTSD and physical health problems 3 to 4 months after the soldiers return home. PTSD and depression are important mediators the relationship between mild traumatic brain injury and physical health problems. NEJM Hoge et. Al (2008) of General Lee lies on its side after surviving a buried IED blast in 2007. Heltemes, et. al, 2011, found no statistically significant relationship between TBI and Alcohol abuse Implications for treatment of patients who have TBI and alcohol abuse issues Intervention and treatment: Insight oriented approaches are the predominant models, but of questionable utility with TBI. Modify admission criteria (remove psychoactive medication restrictions). Determine unique learning strategies: avoid jargon and abstractions, keep ideas concrete. Beware of attention span deficits Be cautious when inferring patient motivation levels. Implications (cont’d) Repeat instructions and strategies Attend to transportation issues Enlist the patients social circle to reinforce goals Increase treatment compliance/attendance with incentives. Remember that symptoms of TBI and alcohol abuse are similar and it can be difficult to distinguish which problem is causing which symptom. HUMVEE Hit by IED mTBI in U.S. Soldiers Returning from Iraq NEJM 2008; 358:453-63 Charles W. Hoge, M.D., Dennis McGurk, Ph.D., et al. 2525 U.S. Army soldiers 3 to 4 months after return from 1 yr. 124 (4.9%) +LOC; 260 (10.3%) altered mental status. + LOC = 43.9% met criteria for PTSD; AMS = 27.3%; other injuries = 16.2%; no injury = 9.1% mTBI associated with poor general health, missed workdays, medical visits, > somatic & PCS compared to SM with other injuries. After adjustment for PTSD & depression, mTBI no longer associated with poor physical health except headache Comprehensive Array of Tests Effort and compliance Premorbid intelligence Learning and memory Visuospatial Intelligence Executive Arousal Motor and attention Language ability skills functions Skills Emotion, behavior personality & MACH TBI Services Primary Care Assessment Case Management Neurological Evaluation/Treatment Psychiatric Evaluation/Treatment Pain Evaluation/Management Neuropsychological Screening/Evaluation Individual & Group Psychotherapy Psychoeducation Cognitive Rehabilitation Biofeedback/Neurofeedback/Alpha-Stim Balance Assessment/Neurocom DeLambo, D. et. Al, Traumatic Brain Injury and Substance Abuse: Implications for Treatment. Conference March,2008. Corrigan, J. & Lamb-Hart, G. (2004)Substance Abuse after a traumatic brain injury: Living with brain injury. Vienna, VA: Brain Injury Association of America. Heltemes, K. et. al, Alcohol Abuse Disorders Among US Service Members with Mild Traumatic Brain Injury. Military Medicine, Vol. 176, February, 2011. Acknowledgements Thanks to these resources: Defense and Veterans Brain Injury Center TBI Service 706-5445102/5176 www.dvbic.org