Psychotherapy Sue Mizen - the Peninsula MRCPsych Course
advertisement
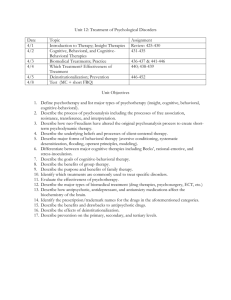
Psychotherapy for the MRCPsych Dr Susan Mizen Consultant Psychiatrist in Psychotherapy Key Competencies General Account for clinical phenomena in psychological terms Deploy advanced communications skills Display advanced emotional intelligence (patients, colleagues and yourself) Specific Refer appropriately for formal psychotherapies Jointly manage patients receiving psychotherapy Deliver basic psychotherapeutic treatments and strategies. Acquiring competencies Routine Clinical Practice Formulation, discussion, reflective diary (Countertransference), personal therapy. Case Based Discussion Group Seeing cases minimum of two, a short and long case in different modalities. Portfolio/Logbook – ARCP WPBA CBD SAPE (yr 2) SAPE 2 (yr 3) Psychotherapy ACE. The MRCPsych Exam Paper 2: 40 questions on therapy related subjects Paper 3: 8% CASC Psychotherapy History Case Discussion Difficult Communication Time table for the day 10-11 am 11.15-12.30am Formulation Lunch 1.00-2.00pm Indications and contraindications for therapies The evidence base for psychological therapies Prescribing for patients in therapy Case vignettes and Formulation 2.15 CASC 1 Difficult Communication CASC 2 Psychotherapy History Indications and Contraindications for Psychological Therapies Psychodynamic Short Term Dynamic Group Analysis CBT IPT Family Therapy Arts Therapies Integrative Therapies Evidence Base CBT Psychodynamic PD, Panic Disorder, Depression in the elderly CAT – Anorexia Nervosa Behavioural treatments Depression, OCD, Phobias, Panic Disorder with Agoraphobia, GAD, Bulimia, BED, Sexual Dysfunction, PTSD. Anxiety disorders, Substance misuse, Childhood behavioural disorders, sexual dysfunction. EMDR – PTSD DBT-Borderline and emotionally constricted PD IPT- Depression and Bulimia Family Couple – SCZ, Type 1 diabetes in children. Jointly managing patients in Psychodynamic therapy Discussing continuing in therapy with the anxious or ambivalent patient. The patient tells you they think their therapist is useless or abusive. The Patient’s disturbance is escalating in therapy. A patient in therapy begins to establish a psychotherapeutic relationship with you as their psychiatrist. Prescribing for patients in therapy: CBT Advantages Disadvantages Medication may - increase the speed and magnitude of response to psychotherapy - reduce symptoms and make treatment more acceptable. - improve ego function so the patient can make better use of therapy. Psychotherapy may - promote adaptive behaviour and improve compliance with medication. - decreases the likelihood of recurrence. - provides a more comprehensive understanding of the patient’s difficulties than medication alone. Medication may - suppress feelings and impede progress in therapy - convey a message that a patient’s feelings are too difficult to be dealt with in therapy. - patient may believe improvement is due to medication not their own efforts. - lead to devaluation of the therapeutic relationship. - be disadvantageous in treating PTSD where exposure to affect is important. - lead to poorer outcome with CBT for panic disorder and agoraphobia, (Westra 2002). The meaning of medication Transference and countertransference to the doctor and medication The significance of medication The importance of therapeutic alliance Indications from medication about the relationship with the doctor. Integrated and Combined Practice Integrated Practice Therapy and medication are managed by the same person. Principles Informed consent. Formulate treatment goals at the outset. Focus on alliance not compliance. Address medication issues at the beginning or end of sessions. Symptoms increase at the end of therapy. Combined Practice Separate practitioners offering therapy and medication. Principles Good communication If there is not a joint formulation – mixed messages. Meet and plan treatment clarify roles and crisis responses Meet again if tensions arise. Prescribing in Psychodynamic therapy Depression in Psychotherapy Escalations of disturbance in psychotherapy Splitting and destructive enactments. Formulation Triangle of person (Malan) Current life situation / symptom Transference Infantile objectrelations / history Formulation Diagnosis Defences Depression Object losses in remote or recent past Ambivalence towards lost object Identification with lost object Excessive superego activity Obsessive Compulsive Disorder Defences of isolation, undoing and reaction formation. Ambivalence in object relations, anxiety about aggression Magical thinking Anxiety Disorder Anxiety signals an unsuccessful defence Agoraphobia sometimes fear of abandonment/separation anxiety Panic disorder- onset often associated with loss Simple phobia – classically associated with symbolic significance of the phobic object Anorexia Nervosa Difficulty separating from mother Body unconsciously perceived as occupied by introject of ‘intrusive’ mother hence starved, need projected into others who are looked after, projective identification in family relations. Alcohol Dependency Associated with harsh punitive superego, alcohol acting as a ‘superego solvent’. Consider primary and secondary gain.