Tourette Syndrome: Definition, History, and Clinical Features
advertisement

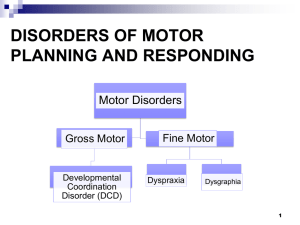
What Is Tourette Syndrome? A neurological syndrome characterized by multiple motor and vocal tics with onset before age 21 years Tics are involuntary, repetitive, stereotyped movements that occur many times a day, nearly every day. Tics typically change anatomic location, frequency, type, complexity, and severity over time Tics can be simple or complex Behavioral features of TS often include OCD, ADHD, or both History of Tourette Syndrome First report in 1825 by Itard who described a French noblewoman with body tics, barking sounds and uncontrollable utterance of obscenities Itard also described 7 men and 3 women with a variety of sudden, bizarre behaviors that we would now call tics History of Tourette Syndrome George Gilles de la Tourette described 8 patients in 1885 who all had motor tics 6 made noises (vocal tics) 5 shouted obscenities (coprolalia) 5 repeated words of others (echolalia) 2 mimicked others gestures (echopraxia) Itard’s patient became the standard example and formed the basis for initial conceptualization that tics were progressive and degenerative History of Tourette Syndrome In early 1900s psychoanalytic school become dominant and attributed tics to repressed sexual impulses and/or conflict between parent and child resulting in deficits of will and character Alternative views continued to be that tics were post-rheumatic and a variant of chorea or were hysterical History of Tourette Syndrome In the 1930s, developmental psychologists described tics as common among schoolage children, but this was largely ignored by the neurological and psychoanalytic communities Observations of heritability and response to dopamine receptor antagonists began to suggest a biological basis Modern View of TS Tic disorders are biological and likely involve the basal ganglia Tourette syndrome is familial with incomplete penetrance and possibly variable expression Once thought to be a simple autosomal inheritance, it now appears that the genetics are complex and there are significant environmental factors Clinical Features of Tics Median age of onset is 7 years Most common initial symptom is eye blinking (36-48%) Most common misdiagnoses are eye problems and allergies Vocal tics are presenting symptom in 12 - 37% Severity in childhood does not predict severity in adulthood Severity is rarely greater in adulthood than in childhood Incidence of TS and Tics Determination of incidence and prevalence is complicated 33% of patients with tics do not recognize some or all of their tics Parents and teachers may not recognize tics Recent studies indicate that 5 – 6 % of school children have tics at some time and that up 0.1 3% have chronic tics (> 1 year) Natural History of TS and Tics Tics tend to wax and wane throughout childhood and adolescence Tics change in type, frequency and intensity Long-term prognosis (e.g., early adulthood) quite favorable: 1/3 of patients experience resolution of tics 1/3 of patients have very mild tics 1/3 of patients continue to have persistent tics Clinical Features of Tics Tics are categorized as motor or vocal Any tic that produces a sounds from the nose of mouth is a vocal tic Distinction between motor and vocal is based more on history than on physiology. Muscle contraction underlies both types Motor tics may be abrupt onset and fast ("clonic") or slow and sustained ("dystonic" or "tonic") Clinical Features of Tics Tics are also categorized as simple or complex Simple tics are individual movements that typically look or sounds purposeless Complex tics resemble purposeful movements or may be ensembles of more simple movements The tics are normal movements occurring in an abnormal context and pattern Simple Tics Simple Motor Tics blinking, nose twitching, head jerking, blepharospasm, oculogyric movements, bruxism, torticollis, sustained mouth opening, abdominal tensing Simple Vocal Tics sniffing, throat clearing, grunting, squeaking, screaming, coughing, blowing and sucking sounds Complex Tics Complex Motor Tics head shaking, trunk flexion, scratching, touching, throwing, hitting, jumping, kicking, obscene gestures (copropraxia) or imitating gestures (echopraxia) Complex Vocal Tics shouting of obscenities or profanities (coprolalia), repetition of the words of others (echolalia), repetition of final syllable, word, or phrase of own words (palilalia) Clinical Features of Tics Premonitory feelings or sensory tics occur in 80% of patients with TS: Specific sensation (e.g. "itch", "dry throat") Nonspecific urge or feeling such as anxiety Influencing Factors Tics may change with emotional or cognitive state Decrease with distraction Increase with stress Increase during relaxation after a period of stress May be suppressible with effort; frequent "rebound" increase afterward May persist in all stages of sleep Classification of Tic Disorders DSM-IV Tourette Syndrome Multiple motor tics and at least one vocal tic Intermittently present for > 1 yr Onset before age 18 yrs Chronic Motor or Vocal Tic Disorder (presence of only motor or vocal tics for greater than 12 months) Transient Tic Disorder (presence of tics for more than four weeks but less than 12 months) Tic Disorder Not Otherwise Specified Associated Symptoms in TS Majority of patients with TS have symptoms of ADHD or OCD at some point during the illness 50% incidence of both ADHD and OCD in TS (compared to 3-5% in gen. pop.) These symptoms are often more bothersome or interfering than tics Common Obsessive Symptoms In TS Frequent and repetitive worrying (e.g., harm coming to self, family). Preoccupation with need for order and routine (e.g., difficulty accepting change). Repetitive thoughts, words, and phrases. Urges to perform forbidden or dangerous activities (e.g., stick finger in fan, hot stove, etc.). Indecision, tendency to be unsure of self. Preoccupation with dirt/contamination Common Compulsive Symptoms In TS Need for order, routine, symmetry (“evening-up”). Repetitive checking and re-checking (e.g., doors, appliances, belongings). Need for perfection, tendency to repetitively perform same activity to ensure correctness. Repetitive touching of objects, persons (may be a complex motor tic). Cleaning, washing, dressing rituals. Inability to tolerate certain types of clothing, foods touch one another on the plate. Neuropsychology of TS Intellectual Ability/IQ Testing Learning Disabilities - Fact or Fiction? Specific Neuropsychological Deficits Potential Confounding Factors Influencing Neuropsychological Function in TS Intellectual Ability In TS IQ Scores Normally Distributed in Epidemiological Studies (Apter et al, 1993) Below Average IQ Reported in TS Clinic Samples (Parraga & McDonald, 1996) Verbal IQ > Performance IQ – Most studies failed to control for presence of ADHD or LD (Bornstein, 1990) PIQ Subtests Primarily Assess Visuospatial Function and Psychomotor Speed Learning Disabilities in TS No Long-Term Outcome Studies of the Learning Patterns in TS (Walkup et al., 1999) LD in TS Highly Correlated with Presence of ADHD (Similar to that reported in ADHD children) Prevalence of LD in TS Estimated to be 22% (Erenberg et al., 1986; Abwender et al., 1996) Math and Written Language Skills Most Common Areas of Weakness (Burd et al., 1992; Brookshire et al., 1994; Schuerholz et al., 1996) School Problems in TS ADHD Significant Predictor of School Problems in TS (Abwender et al., 1996) Higher Rate of Special Education Placement in TS (Comings et al., 1990; Kurlan et al., 1994) Kurlan et al., Neurology, 2001: Epidemiological study of tic prevalence in Monroe County, NY 1596 students directly evaluated (N=341, Spec. Ed, N=1255, Reg. Ed) Spec. Ed - 23.4% weighted prevalence of tics Reg. Ed – 19.7% weighted prevalence of tics Neuropsychological Deficits in TS Visuomotor Deficits Consistent deficits noted on copying tasks (e.g., geometric designs) 10/12 Studies (N=308 TS patients, mean age of ~10 yrs) revealed individual deficits or group differences on various copying tasks (Schultz et al., 1999) TS individuals perform about 1.0 SD below age norm Visuomotor Integration Deficits also Common in ADHD Children Neuropsychological Deficits in TS Gross/Fine Motor Skill Literature equally compelling and similar to that reported for visuomotor deficits Preponderance of studies suggest greater fine motor skill deficits in TS Deficits in both TS adults and children about 0.5-1.0 SD below unaffected controls (Schultz et al., 1998) Neuropsychological Deficits in TS Spatial/Perceptual Deficits Reported VIQ > PIQ suggest spatial/perceptual problems in TS (? confounding factors) Deficits largely due to difficulty with pure motor function and/or impaired visuoperceptual integration (Schultz et al., 1998) Confounding Factor - Lack of studies employing motor-free spatial tasks Neuropsychological Deficits in TS “Executive” Function (EF) Loosely defined construct: mental tracking, sustained attention, working memory planning and organization goal-directed behavior cognitive flexibility impulse control, self-regulation EF Deficits also Common in ADHD (Barkley et al., 1992) and in OCD (Hollander & Wong, 1996; Rosenberg et al., 1997) Neuropsychological Deficits in TS “Executive” Function (EF) No consistent EF deficit has emerged in TS Tasks of mental flexibility, planning and sequencing most commonly cited Consistent findings of slowed response time on CPT tasks Cirino et al., 2000: No differences in card sorting performance between TS alone and TS+ADHD Results suggest that executive dysfunction may occur in TS independent of co-morbid ADHD Confounding Factors Tic Disorder Itself: Natural history of waxing and waning tics Active (or passive) tic suppression Tic suppressing medications (e.g., neuroleptics, clonidine) Co-Morbid Conditions (ADHD, OCD) Methodological Issues (sample sizes, use of clinic samples)