What do we know and where do we go from here - CORE
advertisement
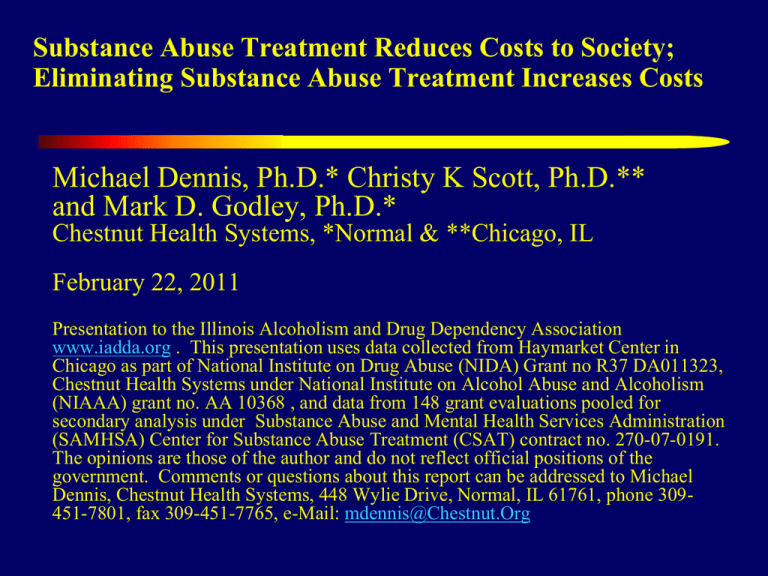
Substance Abuse Treatment Reduces Costs to Society; Eliminating Substance Abuse Treatment Increases Costs Michael Dennis, Ph.D.* Christy K Scott, Ph.D.** and Mark D. Godley, Ph.D.* Chestnut Health Systems, *Normal & **Chicago, IL February 22, 2011 Presentation to the Illinois Alcoholism and Drug Dependency Association www.iadda.org . This presentation uses data collected from Haymarket Center in Chicago as part of National Institute on Drug Abuse (NIDA) Grant no R37 DA011323, Chestnut Health Systems under National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant no. AA 10368 , and data from 148 grant evaluations pooled for secondary analysis under Substance Abuse and Mental Health Services Administration (SAMHSA) Center for Substance Abuse Treatment (CSAT) contract no. 270-07-0191. The opinions are those of the author and do not reflect official positions of the government. Comments or questions about this report can be addressed to Michael Dennis, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761, phone 309451-7801, fax 309-451-7765, e-Mail: mdennis@Chestnut.Org Screening & Brief Inter.(1-2 days) Outpatient (18 weeks) In-prison Therap. Com. (28 weeks) Intensive Outpatient (12 weeks) Adolescent Outpatient (12 weeks) Treatment Drug Court (46 weeks) Methadone Maintenance (87 weeks) Residential (13 weeks) Therapeutic Community (33 weeks) $70,000 $60,000 $50,000 $40,000 $30,000 $20,000 $0 SBIRT models popular due to ease of implementation and low cost $10,000 The Cost of Substance Abuse Treatment is Trivial Relative to the Costs Treatment Reduces $407 • $750 per night in Medical Detox $1,132 • $1,115 per night in hospital $1,249 • $13,000 per week in intensive $1,384 care for premature baby $1,517 • $27,000 per robbery • $67,000 per assault $2,486 $4,277 $10,228 $14,818 $22,000 / year to incarcerate an adult $30,000/ child-year in foster care $70,000/year to keep a child in detention Source: French et al., 2008; Chandler et al., 2009; Capriccioso, 2004 in 2009 dollars Investing in Treatment results in a Positive Return on Investment (ROI) Substance abuse treatment has an ROI of between $1.28 to $7.26 per dollar invested. Consequently, for every treatment dollar cut in the proposed budget, the actual costs to tax payers will increase between $1.28 and $7.26. Bottom line = The proposed $55,000,000 cut will cost Illinois taxpayers between $70,400,000 and 399,300,000 within the next 1 to 2 years. Source: Bhati et al., (2008); Ettner et al., (2006) Unit Costs Used in 2009 Dollars Description Inpatient hospital day Emergency room visit Outpatient clinic/doctor’s office visit Nights spent in hospital Times gone to emergency room Times seen MD in office or clinic Days bothered by any health problems Days bothered by psychological problems How many days in detox Nights in residential for AOD use Days in Intensive outpatient program for AOD use Times did you go to regular outpatient program Days missed school or training for any reason How many times arrested Days on probation Days on parole Days in jail/prison/detention Days detention/jail *Quarterly cost to society 2009 dollars Unit Days Visits Visits Nights Times Times Days Days Days Nights Days Times Days Times Days Days Days Days Cost in 2009 dollars $ 1,409.69 $ 265.52 $ 75.59 $ 1,409.69 $ 265.52 $ 75.59 $ 25.22 $ 9.74 $ 254.82 $ 149.21 $ 102.51 $ 276.17 $ 18.08 $ 2,091.51 $ 5.67 $ 18.29 $ 79.75 $ 111.77 Haymarket Clients As part of NIDA grant R37 DA011323, a cohort of 436 adults sequentially admitted to Haymarket Center in Chicago were interviewed at intake between February to March, 2004 and quarterly for 4 years (with over 95% completion) In 2009 dollars, clients averaged $3698 in costs to society in the 90 days before accessing treatment ($15,383 in the year before intake) Before entering outpatient treatment, clients incurred lower quarterly costs when compared to clients entering long term residential ($2,191 vs. $4,749). During the year prior to treatment, this cohort of 436 adults cost society $6,707,103. Without treatment, these costs would have continued. Quarterly Costs to Society Change in Quarterly Costs To Society: Haymarket Center Cohort $10,000 $9,000 $8,000 $7,000 $6,000 $5,000 $4,000 $3,000 $2,000 $1,000 $0 Treatment costs initially increase costs Followed by a sustained period of reduced quarterly costs Intake 12 24 36 Months from Intake Source: Dennis & Scott NIDA Grant no. R37 DA011323 48 Cumulative Net Cost to Society Cumulative Actual Costs Minus Expected Costs To Society Over 4 years, cumulative saving of $14,589 per person ($6,360,804 for 436 person admission cohort) $10,000 $5,000 $0 ($5,000) ($10,000) ($15,000) Additional Cost of Treatment offset by Savings in other costs within 18 months ($14,589) ($20,000) Intake 12 24 Months from Intake Source: Dennis & Scott NIDA Grant no. R37 DA011323 36 48 Cumulative Actual Minus Expected Costs To Society: Haymarket by Level of Care Cumulative Net Cost to Society 10,000 All Levels of Care Produced Net Savings 5,000 0 STR , -4,542.00 -5,000 -10,000 -15,000 -20,000 -25,000 OP , ($8,552) Similarly, IOP produced greater savings that OP Though the most expensive initially, long term treatment also produced the most long term savings Intake 12 24 36 Months from Intake Source: Dennis & Scott NIDA Grant no. R37 DA011323 IOP , ($18,433) LTR , -$21,698 48 Chestnut Health Systems’ Adolescent Residential Clients As part of NIAAA grant R01 AA 10368 , a cohort of 355 adolescents were recruited at discharge between 2004 and 2008 from Chestnut’s residential treatment programs in central and southern Illinois and interviewed quarterly for 1 year (with over 90% completion) In 2009 dollars, they averaged $6,554 in costs to society in the 90 days before intake ($26,217 in the year before intake) This 4 year cohort of 355 adolescents cost society $9,307,163 in the year before they were admitted to Chestnut – costs they would have continued to incur if they were not treated Change in Quarterly Costs To Society: Haymarket Center Cohort Quarterly Costs to Society $7,000 $6,000 $5,000 $4,000 $3,000 $2,000 $1,000 Outpatient Continuing Care plus other Costs Consistently Below Baseline Costs $0 3 6 9 Months from Intake * Cost of residential treatm ent Source: Godley NIAAA Grant no. R01 AA 10368 12 Usual Continuing Care (UCC) Usual Continuing Care (UCC) $10,910 (CM) UCC + Assertive Continuing Care UCC+Assertive Continuing (ACC) Care (ACC) UCC + CM + ACC $11,559 $7,876 * Defined as 12 month post discharge costs to society minus 12 month pre* Cost intake coststreatm to ent society of residential Source: Godley NIAAA Grant no. R01 AA 10368 $14,000 $4,816 UCC + Contingency Management UCC+ Contingency Management (CM) UCC + CM + ACC $12,000 $10,000 $8,000 $6,000 $4,000 $2,000 $0 More Intensive Continuing Care Produced Greater Savings* SAMHSA/CSAT’s Clients by Level of Care As part of SAMHSA/CSAT contract 270-07-0191, data has been pooled from 22,045 clients from 148 local evaluations, recruited between 1997 to 2009 and followed quarterly for 6 to 12 months (over 80% completion) In 2009 dollars, the 2,793 adults averaged $1,417 in costs to society in the 90 days before intake ($5,669 in the year before intake) In 2009 dollars, the 16,915 adolescents averaged $3908 in costs to society in the 90 days before intake ($15,633 in the year before intake) SAMHSA/CSAT’s Adolescents Clients by Level of Care Adolescent Level of Care Year before intake Year after Intakea One Year Savingsb Outpatient $10,993 $10,433 $560 Intensive Outpatient $20,745 $15,064 $5,682 Outpatient Continuing Care $34,323 $17,000 $17,323 Long Term Residential $27,489 $26,656 $833 Short Term Residential $25,255 $21,900 $3,355 Total $15,633 $13,642 $1,992 \a Includes the cost of treatment \b Year after intake (including treatment) minus year before treatment SAMHSA/CSAT’s Adult Clients by Level of Care Adult Level of Care Year before intake Year after Intakea One Year Savingsb Outpatient $12,806 $9,241 $3,565 Intensive Outpatient $15,263 $15,197 $ 66 Outpatient Continuing Care $34,057 $14,310 Residential $19,443 $24,297 ($4,854)c Total $17,035 $12,442 $19,748 $4,592 \a Includes the cost of treatment \b Year after intake (including treatment) minus year before treatment \c Cost of residential treatment is not offset yet at one year after intake These Analyses Provide Converging Evidence That Substance Abuse Treatment Programs serve individuals who are costing society a great deal. Eliminating treatment will NOT eliminate costs associated with substance abuse….We will pay. The proposed $55,000,000 cut will cost Illinois taxpayers between $70,400,000 and 399,300,000 within the next 1 to 2 years. The cost of treatment is offset by total savings to society within 6 months to 3 years post-intake and produce cumulative benefits that continue to grow for many years. While providing more intensive treatment and continuing care costs more in the short run, it also produces the greatest benefit in the long run to tax payers. Conversely This Suggests That.. Cutting substance abuse treatment will likely increase total costs to Illinois taxpayers via increased costs associated with healthcare, welfare and incarceration Focusing on the least expensive and/or intensive treatment options to reduce short term costs will significantly reduce the long term benefits. References Bhati et al. (2008) To Treat or Not To Treat: Evidence on the Prospects of Expanding Treatment to Drug-Involved Offenders. Washington, DC: Urban Institute. Capriccioso, R. (2004). Foster care: No cure for mental illness. Connect for Kids. Accessed on 6/3/09 from http://www.connectforkids.org/node/571 Chandler, R.K., Fletcher, B.W., Volkow, N.D. (2009). Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. Journal American Medical Association, 301(2), 183190 Ettner, S.L., Huang, D., Evans, E., Ash, D.R., Hardy, M., Jourabchi, M., & Hser, Y.I. (2006). Benefit Cost in the California Treatment Outcome Project: Does Substance Abuse Treatment Pay for Itself?. Health Services Research, 41(1), 192-213. French, M.T., Popovici, I., & Tapsell, L. (2008). The economic costs of substance abuse treatment: Updated estimates of cost bands for program assessment and reimbursement. Journal of Substance Abuse Treatment, 35, 462-469