NPH 10-30-12 Morrone-Strupinsky presentation
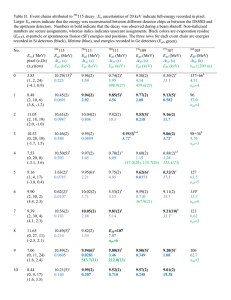
advertisement

Managing cognitive and emotional changes associated with NPH Jeannine Morrone-Strupinsky, Ph.D., ABPP-CN October 30, 2012 Plan of talk Review cognitive changes associated with NPH Offer suggestions for managing cognitive changes Review mood/behavioral changes associated with NPH Offer suggestions for managing mood/behavioral changes Q & A NPH—A Brief Review First described in 1965. Abnormal buildup of CSF in the ventricles with high normal CSF pressure. Enlargement of the ventricles causes stretching of surrounding brain tissue (neurons) and blood vessels, particularly in the frontal lobes. How NPH looks in the brain Normal MRI T2-weighted MRI showing dilatation of ventricles out of proportion to sulcal atrophy in a patient with normal pressure hydrocephalus. CT head scan of a patient with normal pressure hydrocephalus showing dilated ventricles. The arrow points to a rounded frontal horn. www.emedicinehealth.com NPH—A Brief Review Can occur in people of any age, but is most common in older adults (60s and 70s). Secondary NPH is the result of brain injury/insult (e.g., trauma, infection, tumor). “Idiopathic” NPH is due to unknown causes. NPH may account for up to 5% of individuals with dementia. Clinical triad Incontinence Inability to hold urine Frequent urination Urgency to urinate Gait disturbance Unsteadiness Wide-based gait Leg weakness Sudden falls Shuffling steps Difficulty taking first step because feet are “stuck” to the floor “freezing” while walking Cognitive impairment (next slide) Cognitive Effects of NPH Slowing down of thoughts Memory impairment—decline in active retrieval (immediate and delayed recall) with preserved memory storage (recognition) Visuospatial perception and visuoconstruction may be impaired Absence of aphasia, apraxia, and agnosia (“cortical features” seen in AD) Impairment in executive functions Cognitive Effects of NPH Executive functions (“CEO” of the brain) Planning (and prioritizing) Thinking in a flexible manner (adjusting to changing situations, coming up with new solutions) Concentration/working memory (i.e., dialing new phone numbers) Abstract thinking (learning from experience by extracting broader meaning of events) Managing time Initiating appropriate actions and inhibiting inappropriate actions (impulsivity) Selecting relevant sensory information (focusing attention on what is relevant; i.e., being able to filter out background noise) Cognitive Effects of NPH Regarding memory, individuals with NPH display impaired free recall of information but tend to benefit from cues and show relatively spared recognition. This has led some to propose that the mechanism of memory failures may be retrieval search while the storage capacity is preserved. Memory retrieval is performed by the frontal lobes (affected by bulging ventricles). Effects of shunting on cognitive impairment NPH is described as a reversible form of dementia. However, statistics vary considerably regarding cognitive improvement (30-40% in INPH and 5070% in secondary NPH). Memory tends to improve more than executive functions. More improvement is seen in younger individuals and in women, and in those without other causes of impairment. Gait impairment and urinary incontinence are more likely to improve. 5 reasons why a neuropsychological examination is requested by a physician To find possible problems with brain functioning. To help clarify a patient’s diagnosis. To define an individual’s relative brain-related strengths and weaknesses. To guide treatment, or to help patients make educational or vocational decisions. To determine whether or not there are any changes in a patient’s cognitive and emotional functions over time. National Academy of Neuropsychology Role of the neuropsychologist A neuropsychological examination is a systematic and scientifically-based assessment of a person’s thinking, problemsolving, and memory capacity that may reveal something about the state of brain function. The pattern of test findings allows the examining clinician to develop an informed opinion about the patient’s higher cerebral functioning. Ultimately, the physician must integrate results from a variety of tests to determine the diagnosis. Compensating for cognitive difficulties in NPH If the person with NPH has difficulty shifting tasks quickly give adequate notice that he or she needs to get ready to go somewhere post an agenda for the day If the person with NPH has difficulty focusing reduce background distractions perform only one activity at a time, and try to complete the activity before starting another activity take frequent breaks to allow the individual to regroup Compensations for cognitive difficulties in NPH If the person with NPH has difficulty sequencing use procedural checklists (i.e. to program TiVo, cook meals, follow a grooming routine) If the person with NPH has difficulty making decisions limit choices/provide options use concrete examples break down large projects into component parts Compensating for cognitive difficulties in NPH If the person with NPH has difficulty recalling information use a memory notebook, day planner, or voice recorder use placards use a beeping watch/timer to remember to do something (i.e., turn off hose in the yard) use a pill box use forms to remember to do things that occur periodically (i.e., change air filters) provide cues to aid memory use organizing strategies (grouping) face-name recall technique Face-name recall technique Focus on the name. Repeat it to yourself several times. Associate the name with something already stored in your memory. If you know someone with the same name, that will be the association. Visualize an image of the new person with the person you already know who has the same name. If the person has a name that you do not know, create an association by breaking down the name into words to which you form visual images. Visualize the person with the visual images you have created. Drawing a picture with the association or making up a short story about the images helps even more. Example…associations Margaret Thatcher Ann-Margret Famous Margarets… Maggie Bobrowitz, RN, MBA Neuroscience Program Coordinator Bob………………..row…..itz Grouping example Read the following list of sports one time. When you are done, write down as many of the sports as you can without looking back at the list. snow skiing basketball tennis long jump bobsledding 100-m dash hockey baseball ice skating discus golf high jump volleyball javelin soccer luge curling cricket decathlon hurdles www.utexas.edu/student/utlc/class/mkg_grd/improving.html Grouping example You can organize material by grouping similar concepts, or related ideas together. For example Winter sports Track and field sports Sports using a ball Individual sports Team sports www.utexas.edu/student/utlc/class/mkg_grd/improving.html Another grouping example… NPH and mood changes Depression is present in some individuals with NPH. Average prevalence of major depressive disorder in the elderly population is 1.8%. DSM-IV criteria for depression (>5 of the following): depressed mood decreased interest (apathy*) or pleasure in activities (anhedonia) significant weight loss* insomnia* or excessive sleep* psychomotor retardation or agitation loss of energy (anergia)* feelings of inappropriate guilt recurrent thoughts of death Differentiating depression from apathy Sometimes it looks like the individual with NPH is depressed, but rather s/he is apathetic or is unconcerned or unaware of his or her condition. Apathy is defined as a primary loss of motivation, loss of interest, and loss of effortful behavior, features also present in depressed individuals. This is likely due to disruption of medial frontal lobe functioning due to bulging of the ventricles into the brain tissue. Treatment of depression in NPH Treatment of depression in NPH is important because depression has a negative influence on cognitive performance, activities of daily living, and perceived quality of life. In the case of mild depression, options include behavioral activation and/or supportive psychotherapy. A clinical psychologist or social worker can be helpful in this adjustment period, particularly in helping identify life stressors that may be contributing to the depression. Psychotherapy also helps the individual with NPH accept the diagnosis, employ coping strategies, and work through the emotional consequences of having to deal with the diagnosis. Treatment of depression in NPH, cont’d A long-term plan must then be structured to minimize stress and improve quality of life. Patients should be encouraged to develop a daily exercise routine within their capabilities. In case of more significant depression, pharmacological treatment is warranted (antidepressant medication). Keenan et al. (2005) demonstrated a reduction in reported symptoms of apathy following a dose of methylphenidate, which increases the action of dopamine, a chemical in the brain. NPH and sleep disturbance Individuals with NPH may experience sleep disturbance. This can be due to changes in mood or in the functioning of brain regions associated with sleep. Practicing sleep hygiene can improve sleep. Go to bed the same time every night. Keep bedroom cool, dark, and quiet. Use the bedroom only for sleep and intimacy. Get up and do something sedentary if you are unable to fall asleep. “Pseudodementia” in NPH A common referral question is the differentiation of cognitive dysfunction caused by NPH from a “pseudodementia” attributable to depression. Patients with NPH and depression show worse cognitive performance when compared with patients without depression, particularly on tests of executive functioning. Depression and even mild cognitive impairment contribute significantly to disability in patients with NPH. Salvador Dalí. (Spanish, 1904-1989). The Persistence of Memory. 1931.