Insomnia: Physiological And Medical
Findings And Implications For
Diagnosis And Care*
George G Burton MD
Medical Director, Sleep Disorders Center
Kettering Health Network, Dayton, Ohio
* With appreciation to M Bonnet and D Arand
Goals Of This Presentation:
• Understand objective diagnostic and
treatment outcome criteria
• Recognize insomnia as a true medical problem
(not secondary)
• Recognize utility of a new diagnostic paradigm
in insomnia care
Definition Of Insomnia – ICSD-2
• Complaint of difficulty initiating sleep,
difficulty maintaining sleep, waking up too
early, or non-restorative sleep
• Occurs despite adequate sleep environment
and opportunity
• Includes reported daytime impairment, such
as fatigue, impaired attention, irritability,
sleepiness, or poor motivation related to the
poor sleep
Classifications Of Insomnia
• Simple: Sleep Initiation or Sleep Maintenance
OR
Objective or Subjective
• Complex: ICD-10 or DSM-V or AASM Nosology
(ICSD-2)
Unfortunately complexity clouds our understanding
but is a necessary evil
Insomnia A Symptom AND A Diagnosis
•
•
•
•
Like CFS/FM
Leads to professional skepticism and hostility
Frustrates research enthusiasm and financing
Encourages therapeutic nihilism
NOT: Insufficient sleep syndrome
AASM Insomnia Nosology ICSD-2
(Associates Subjective Complaint With
Possible Contributing Disorder)
1.
2.
3.
4.
5.
6.
7.
Adjustment Insomnia
Psychophysiological Insomnia
Paradoxical Insomnia
Idiopathic Insomnia
Insomnia Due To Mental Disorder
Inadequate Sleep Hygiene
Behavioral Insomnia Of Childhood
(more)
AASM Insomnia Nosology ICSD-2
(Associates Subjective Complaint With
Possible Contributing Disorder)
(Continued…)
8. Insomnia Due To A Drug Or Substance
9. Insomnia Due To Medical Condition
10. Insomnia – Unspecified (non-organic)
11. Insomnia – Unspecified (organic)
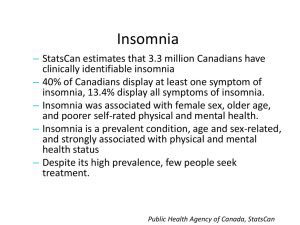
Prevalence Of Insomnia
• Lifetime prevalence 4-24%. Most common sleep
disorder. Incidence varies with patient age and
sex.
• Women have a lifetime risk 1.5 - 2.5 times men.
• Additional factors:
Employment Status
Obesity
Rotating Shifts
• Chronic prevalence (2-3 months is 6-10%)
• Subtypes of prevalence vary widely
Consequences of Insomnia: Cost
Home and Public Accidents
$3.7 Billion
Work-Related Accidents
$10.3 Billion
Motor Vehicle Accidents
$29.2 Billion
Work Place Productivity Loss
$150.0 Billion
Consequences Of Insomnia: Quality Of
Life
• Medical Outcomes Study Short Form (SF-36)
- Insomnia patients have significant decreases
on all dimensions
- Level of decrease is comparable to patients with
depression or congestive heart failure
• Poor sleepers have fewer promotions and
increased health care needs
• Recent data found increased risk for all cause
mortality in patients with “nearly everyday”
insomnia
There Is A Big Difference In These Two
Concepts:
• Insomnia is a risk factor for…
• Insomnia is comorbid with…
Insomnia Is A Risk Factor For:
•
•
•
•
•
•
Depression/Anxiety/Substance Abuse
Anxiety and mood disorder relapse
? Pain
Diabetes and hypertension
Infectious disease conditions/immune status
Suicide
“Sleepy patients are like deaf children with respect
to short-term memory and task organization”
Insomnia Is Often A Comorbid
Condition With:
• Depression/Anxiety states
• Pain
• Respiratory, GI, Neurologic, Musculoskeletal,
Endocrinologic and Cardiovascular Disorders
• Drug use such as anti-hypertensives and antidepressants, bronchodilators, nasal
decongestants
Treatment Studies Do Not Separate
Comorbility From Risk Issue 100% Of
The Time
Examples:
• Sleep on the efficiently of anti-depressant
drugs
• Sleep on the treatment of pain
• Sleep on insulin resistance in diabetes
Conditioned Stress Is Comorbid With
Insomnia
• Inability to relax in bed
• Mental arousal In Bed (intrusive thoughts)
• Sleeps better away from home
• Difficulty in falling asleep in bed but not at
other times (i.e. watching tv)
Aging And Poor Sleep
• Normal aging is associated with:
- Increased incidence of pain and other
medical problems
- Increased sympathetic nervous system activity
- Decreased activity (decreasing amplitude of
circadian rhythms)
- Decreased sleep (SWS) sleep
- Increased awakenings and wake
time during sleep
Aging And Poor Sleep (continued…)
• Is poor sleep with aging a normal change or a sign
of slowly evolving pathology? If it were
Hypertension, we would treat.
• What is the specificity/sensitivity relationship
between the ESS, sleep latency sleep efficiency,
and WASO?
Insomnia Comorbid With Other Sleep
Disorders
• Sleep Apnea – refer patients with insomnia
and significant snoring
• Periodic Limb Movements – refer patients with
nocturnal restlessness
• Restless Legs
• Dream Anxiety Attacks
• REM Behavior Disorder
• Should we base some of our treatment decisions
on ESS, etc?
Interests And Concerns In Insomnia
• Attendance at insomnia sessions at AASM extremely
high
• AASM subspecialty examination in Behavioral Sleep
Medicine and cognitive behavioral therapy growing
• As for OSA in 2002, cost is a big concern
• Potential solutions:
- Judicious use of expensive tests and therapies e.g.
PSG and Cognitive Behavioral Therapy
- Emergent consensus that success of these tools are
based in the neurobiology of insomnia
Neurotransmitters Involved In Sleep
And Arousal*
• Facilitates sleepiness: Adenosine, GABA,
Galanin, Glycine, Melatonin
• Facilitates arousal: Acetylcholine, Dopamine,
Glutamate, Histamine, Norepinephrine,
Orexin, Serotonin
*Gulyani S et al Sleep Medicine Pharmocotherapies Overview. Chest 142:1659-1668(2012)
Physiologic Findings More Pronounced
In Persons With Objective And Primary
Insomnia
• Numerous studies have shown that patients
with primary insomnia suffer from CNS
hyperarousal, usually linked to the
sympathetic nervous system as indicated by:
– Increased heart rate
– Decreased heart rate variability
– Increased whole body and brain metabolic rate
– Increased high frequency EEG
– Increased secretion of cortisol, ACTH
Hyperarousal And Insomnia
Hyperarousal State In Insomnia*
*Bonnet M, Burton G and Arand D, Physiologic and Medical Findings In
Insomnia: Implications For Diagnosis And Care. Sleep Rev 2013(In Press)
Insomnia Workup And Therapy
Paradigm*
*Bonnet M, Burton G and Arand D, Physiologic and Medical Findings In
Insomnia: Implications For Diagnosis And Care. Sleep Rev 2013(In Press)
The PSG Modified For Insomnia
(PSG-I)
• The standard PSG Plus:
- Nocturnal blood pressure recording
- Heart rate variability
- Beta-power analysis on EEG
• Patients identified as having objective/primary
insomnia should be directed to CBT-I
An Insomnia Work-Up Paradigm Draft
Based On Costs
INEXPENSIVE
MORE EXPENSIVE
VERY
EXPENSIVE/RESEARCH
H&P
PSG-I
Cortisol Panel
Sleep Log
Beta-Power Analysis
TNF-α
ESS/FSS/Beck Depression
Inventory
Nocturnal Blood Pressure
Recording
Leptin
Pain Scale Rating
Collagen-Vascular Panel
Ghrelin
CBC, ESR, hs-CRP
Immune Globulins
Interleukins
HgB-A-1-C
CD-4/CD-8 Assay
Thyroid Function
PFT/Echocardiogram
Recording Oximetry
Formal Neuropsychiatric
Testing
BP Log
THERAPY
• Treat comorbid conditions first
• CBTI: Best results in paradoxical/objective
insomnia
• Self-directed therapy
- Environmental management
- Sleep scheduling
• Pharmacological
- 15 new drugs under clinical study
- Anti-depressants and anxiolytics very popular
- Sedatives
A Typical Insomnia Case
• 47 Year old male bank executive in good health
- 15 Year history of SII, SMI, worry about work
and family would keep him from sleeping
- No known comorbitities
- Good sleep hygiene by history
- Sleep log, FSS, screening laboratory all normal
- Home sleep study normal except for “long sleep
latency and decreased sleep efficiency”
A Typical Insomnia Case (continued…)
- ESS 15/24
- Neuropsychiatric assessment moderate
anxiety depression
- Anxiolytics and various anti-depressants no
help over the past 5 years
- PSG-I: Long sleep latency, elevated arousal
index; otherwise normal
• Diagnosis: paradoxical insomnia versus
psychophysiological insomnia
A Typical Insomnia Case (continued…)
• Told to: “Lighten Up!” by his family PCP and
Psychiatrist without improvement
• Referred for CBTI for eight sessions
• Dramatic improvement