Aaron Alan, MFT, CSAT
Executive Director
Foundry Clinical Group
Thuy Bui, LCSW, CSAT
Clinical Director
Foundry Clinical Group
Mark Forman, PhD
Clinical Director
Life Design Centre
The Neurobiology of
Trauma, Sex
Addiction, and
Meditation: Current
Research and Clinical
Implications
Today’s Talk
Who We See and What We Treat
Trauma and Adverse Childhood Experiences
(ACEs)
Trauma, Addiction, and SA/SC
Neurobiology of Trauma
Neurobiology of Addiction
Today’s Talk cont.
Theory and Types of Meditation
Neurobiology of Meditation
Clinical Applications
Clinical Issues and Unknowns
Q&A
Foundry: Who We See
and What We Treat…
Trauma,
Adverse
Childhood
Experiences,
and
Addiction
Addictions and Adverse
Childhood Experiences
Kaiser Adverse Childhood Experiences (ACEs)
Study (Felliti et al., 1998; Felliti, 2004)
17,000 middle-class American adults underwent
comprehensive, biopsychosocial medical
evaluation.
Adverse Childhood Experiences Study
Each participant received 1 pt. for:
1. recurrent and severe physical abuse (11%)
2. recurrent and severe emotional abuse (11%)
3. sexual abuse (22%)
growing up in a household with:
4. an alcoholic or drug-user (25%)
5. a member being imprisoned (3%)
6. a mentally ill, chronically depressed, or institutionalized
member (19%)
7. the mother being treated violently (12%)
8. both biological parents not being present (22%)
Addictions and Adverse
Childhood Experiences
"Addiction highly correlates with characteristics
intrinsic to that individual’s life experiences,
particularly in childhood… Commonly
understood examples of addiction are
the compulsive use of nicotine, alcohol,
methamphetamine, and heroin. More subtle
examples are compulsive eating, sex, gambling,
or shopping.” (Felliti, "Neuroscience of Addiction", 2004)
Adverse Childhood Experiences
and Alcoholism
Adverse Childhood Experiences
and Injected Drug Use
Adverse Childhood Experiences,
Addictions and Mortality
What About
Sexual Compulsivity?
Adverse Childhood Experiences
and Sexual Compulsivity
Persons who had experienced 4 or more categories of
childhood exposure, compared to those who had
experienced none, had:
4- to 12-fold increased risks for alcoholism, drug
abuse, depression, and suicide attempt;
2- to 4-fold increase in smoking, poor self-rated
health, > 50 sexual intercourse partners, and at least
1 sexually transmitted disease and a
1.4- to 1.6-fold increase in physical inactivity and
severe obesity.
Adverse Childhood Experiences
and Sex Addiction?
Hillis et al. (2001) found using this data set that
ACEs were proportionately correlated in women
with:
Earlier sexual activity (under age 15)
Higher number of sexual partners
Odds of having 30+ sexual partners went from…
1.6 for those with one type of ACE
1.9 for those with two ACEs
8.2 among those with 6-7 ACEs
Case Vignette
•4 ACEs: recurrent physical abuse, recurrent emotional
abuse, an alcoholic parent, chronically depressed parent
overheard father call him stupid to sibling and overheard
parents frequently fighting. Sexually compulsive bxs:
online pornography, compulsive masturbation,
anonymous sex with women, listening to ppl having sex.
•Was able to stop anonymous sex early in tx, but
intermittent pornography viewing and searching for
audio content continued until underlying trauma/ACEs
were addressed and treated. Clt currently has 2 yrs of
sobriety and recently was married.
What Does
Trauma Do
to the
Brain?
Trauma and the Brain
Brain processes are not entirely “local” – they
are both local and distributed/coordinated across
different structures and regions of the brain.
However, research in trauma has focused
heavily on three local parts of the brain:
Amygdala
Hippocampus
Prefrontal Cortex
AMYGDALA
Amygdala – Function develops
immediately after birth. Allows
rapid assessment of danger
and experience of fear.
Becomes activated upon cues
or “triggers” that are
reminiscent of early traumatic
events. But it does so with poor
accuracy. (van der Kolk, 2003)
AMYGDALA
Stevens et al. (2013) found…
A study of 40 women…
Participants with PTSD showed a
significantly increased response to
fearful stimuli in the right
amygdala.
The right amygdala is more
responsive to pictorial or imagerelated material [the left to highly
detailed and linguistic].
AMYGDALA
Stevens et al. (2013) cont…
Right amygdala activation correlated
positively with the severity of
hyperarousal symptoms in the
PTSD group.
Participants with PTSD showed
decreased functional connectivity
between the right amygdala and left
prefrontal cortex.
That is, the cortex can help regulate
the amygdala, but this connection is
deficient in PTSD patients.
AMYGDALA
HIPPOCAMPUS
Hippocampus – Function develops
gradually over first five years.
Allows recognition and
organization of nature of threat.
Large role in memory. Can
accurately pair cues or triggers
with threat responses when
hippocampus is developed enough
at time of traumatic event. Specific
and accurate, particularly later in
life, but not so in childhood. (van
der Kolk, 2003)
HIPPOCAMPUS
Gilberston et al. (2002) found…
In a monozygotic twin study,
severity of PTSD symptoms was
negatively correlated with the
hippocampal volume.
Smaller hippocampal volume
predicted vulnerability to
psychological trauma.
HIPPOCAMPUS
Woons et al. (2010) found…
In a meta-analysis of 39 studies…
Hippocampal volume deficits
associated with exposure to
psychological trauma and
posttraumatic stress disorder in
adults.
Additional hippocampal reduction
was found in PTSD compared to the
trauma-exposed group without
PTSD.
HIPPOCAMPUS
Carrion et al. (2007) found…
Stress predicts lower
hippocampal volume in youth
with PTSD symptoms.
HIPPOCAMPUS
Carrion et al. (2010) found…
Youth with PTSD symptoms
demonstrated reduced
activation of the right
hippocampus during a memory
retrieval task.
PREFRONTAL CORTEX
Prefontal Cortex – Develops
gradually over first 25 year
(perhaps more) of life. Is primarily
responsible for executive function,
reasoning, and planning in
stressful and nonstressful
situations.
Prefrontal cortex helps regulate
amygdala responsiveness.
PREFRONTAL CORTEX
However, activation of limbic and
stress responses are “faster” than
activation of prefrontal cortex, thus
an overactive amygdala creates
challenges for prefrontal
performance. (van der Kolk, 2003)
PREFRONTAL CORTEX
van Harmelen (2010) found…
In a study of 84 unmedicated
adults who reported emotional
maltreatment prior to age 16.
Found “profound” reductions in the
volume of the medial prefrontal
cortex, even in the absence of
physical or sexual abuse.
PREFRONTAL CORTEX
Carrion et al. (2010) found…
Youth (10-16) with PTSD
symptoms had significantly
decreased total brain tissue and
total cerebral gray volumes in
comparison with healthy control
subjects.
Significant negative correlation
between prebedtime cortisol levels
and left ventral prefrontal cortex
volumes.
PREFRONTAL CORTEX
Shin et al. (2005) found…
In a fMRI study of 13 men with
PTSD and 13 men without PTSD.
Studied the response to facial
expression images.
PREFRONTAL CORTEX
Shin et al. (2005) found…
The PTSD group exhibited
exaggerated amygdala responses
and diminished medial prefrontal
cortex responses to fearful vs
happy facial expressions.
The stronger the amygdala
activation, the lower the prefrontal
cortex functioning. The two
responses were inversely related.
Summary of Neurobiology of
Trauma
Trauma and PTSD symptoms are
strongly correlated with:
over-activation of the amygdala
a decrease-in-size and
underfunctioning of the hippocampus,
a decrease-in-size and
underfunctioning of the prefrontal
cortex, including decreased regulatory
connectivity to the amygdala
Neurobiology and Addiction
“[A]ll addictions create, in addition to chemical changes
in the brain, anatomical and pathological changes which
result in various manifestations of cerebral dysfunction
collectively labeled hypofrontal syndromes. In these
syndromes, the underlying defect, reduced to its simplest
description, is damage to the “braking system” of the
brain.” (Hilton & Watts, 2011 – “Pornography Addiction:
A Neuroscience Perspective”)
Hypofrontal Syndromes
May result from genetic predisposition or the cumulative
impact of addictive behavior alone…
But when trauma is present or underlying…
It sets up the perfect conditions for addiction and
compulsion to begin and take hold, since the “brakes”
are already off.
Underfunctioning
Prefrontal Cortex
Traumatized
Brain
Underfunctioning
Hippocampus
Overfunctioning
Amygdala
Why is meditation
potentially
important in
regards to trauma
and addiction?
SHORT ANSWER: Meditation
appears to directly counteract
these specific neurobiological
problems.
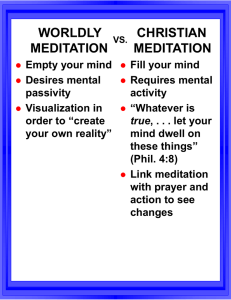
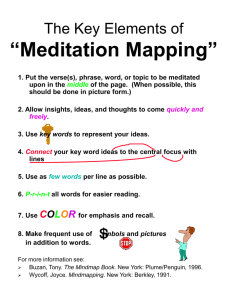
Theory of Meditation
From a psychological/subjective perspective…
Let thoughts and emotions pass.
Enter deep, calm concentration.
Encourage “transpersonal” moments.
Theory of Meditation
From a neurobiological/physical perspective…
Engage in a self-directed neuroplastic alteration of the
brain.
It is this neurobiological-neuroplastic process that
current research has been investigating.
Types of Meditation: Mindfulness
Mindfullness –
Nonjudgemental
noticing of
thoughts and
feelings, letting
them pass with
attitude of calm.
Cultivate specific
insights about the
nature of the self.
Focus on present
moment.
Types Of Meditation:
Concentrative
Concentrative –
Focus on an object,
image, word or
phrase (mantra)
meant to absorb a
person into various
trance states.
Types of Meditation: Imaginal
Imaginal – Calling to
mind specific positive
emotional states (and
their imaginal
associations) in order to
cultivate deeper positive
emotion.
e.g., Metta meditation
(Loving-kindness or
compassion meditation)
Very often, meditative
techniques borrow/overlap from
all three categories
Meditation Research:
Some Important Studies
Changes in cerebral blood flow during
meditation (Newberg et al., 2001, 2003)
Meditation Studies
Lutz et al. (2004) found heightened gamma wave activity
throughout cortex – the highest ever recorded in a nonpathological population – in a group of 8 highly trained Tibetan
monks.
Dose-response relationship
Gamma activity remained heightened outside of meditation itself
– apparently permanent neuroplastic change.
Gamma highest in left prefrontal cortex, an area associated with
positive, pro-social emotions.
Meditation Studies
Lazar et al. (2005)…
MRI with 20 highly experienced meditators
Meditation Studies
Lazar et al. (2005) cont…
Brain regions associated with attention
and introspection were thicker in
meditation participants than matched
controls, including the prefrontal cortex
and right anterior insula.
Between-group differences in prefrontal
cortical thickness were most
pronounced in older participants,
suggesting that meditation might offset
age-related cortical thinning.
Meditation Studies
Luders et al. (2012) in a study of 50 advanced meditators and
50 controls (meditators represented all three types of
meditation styles).
Carefully matched for sex and age.
Study focused on the gyrus (hills and valleys) of the cortex.
Increases in gyrification means increased connectivity and
growth in number of brain neurons. Decrease in gyrification
means decreased connectivity and “pruning” of neurons;
normal outcome of aging, worse in dementia.
Meditation Studies
Positive correlation found
between the number of years of
meditation and gyrification in a
number of areas of the cortex.
Also, positive correlations
between number of meditation
years and gyrification in the
right anterior dorsal insula
(volume increased most here).
Meditation Studies
Desbordes et al. (2012) study…
Healthy adults with no prior meditation experience took
part in 8 weeks of training in Mindful Attention Training
(MAT; mindfulness), Cognitively Based Compassion
Training (CABT; compassion), or control group.
2 hours spent in class per week (40 minutes meditating)
plus 20 minutes per outside class.
Meditation Studies
Desbordes et al. (2012) cont…
Study looked at activation of right amygdala using
positive, negative, and neutral images using fMRI in nonmeditative state (outside of meditation)
Meditation Studies
Found a decrease in right amygdala
activation in response to positive
images, and in response to all
images in MAT group.
Similar changes in CBCT group except there was higher amygdala
responses to negative images.
Authors hypothesized this response
in CBCT might be due to increased
empathy, which is a result consistent
with others studies of increased
empathy.
Meditation Studies
Luders et al. 2012 found…
Long-term meditators (30
persons) had significantly larger
left hippocampal volumes
“Larger hippocampal
dimensions may similarly
account for meditators’ habits
and abilities to engage in
mindfulness behavior, cultivate
positive emotions, and retain
emotional stability.”
Sample Clinical Studies: Meditation and Trauma
Direct evidence is showing up for PTSD and
elements of other addictions, with some initial
connections to SA/SC.
Sample Clinical Studies: Meditation and Trauma
Kearney et al. (2013) found that Loving-kindness
(compassion) meditation in PTSD patients produced
reduced symptoms and depression.
King et al. (2013) did a pilot study mindfulness-based
cognitive therapy (MBCT) for combat veterans and
showed significant improvement in PTSD symptom
severity on post-treatment assessment.
Sample Clinical Studies: Meditation and Trauma
Rosenthal et al. (2013) found that Transcendental
Meditation (TM) was effective in small pilot study of U.S.
war veterans in terms of reduced PTSD symptom
severity and improved quality of life.
Sample Clinical Studies: Meditation and Trauma
Substance addiction issues…
Bowen et al. (2009) found addicts who underwent
Mindfulness Based Stress Reduction had significantly
lower rates of substance use in those who received
typical treatment protocols at 4-month post-intervention
period. Also showed reduced cravings as compared to
treatment controls.
Clinical Studies: SA/SC and Meditation?
Reid et al. (2013) found…
In a study of 40 hypersexual patients vs. 30 controls, found an
inverse relationship between hypersexuality and mindfulness, above
and beyond meditating factors of emotional regulation, impulsivity,
and stress proneness.
This sounds
very
promisingand it is! but what are
the clinical
complexities?
Clinical Issues and Concerns…
Drawn from large body of existing literature – mostly
case, phenomenological reports, and clinical summary
judgments from meditators across traditions and
clinicians who have incorporated meditation in practice
for the past few decades (e.g., Forman, 2010; Walsh &
Shapiro, 2006)
Clinical Issues and Concerns…
Having clients sit/practice during intense periods of PTSD
symptoms?
Sometimes meditation can be de-repressive
Internalizing vs. externalizing attention
Emotional dysregulation is expected at certain points in
typical meditation practice…
Meditation and dissociation?
THE ISSUE OF STRUCTURAL
DISSOCIATION
Trauma Creates Structural
Breaks in Mind
Going on
With
Everyday
Self
Traumatized
Part
Long-term
meditation
Clinical Issues and Concerns…
Final question… Very important for SA/SC
treatment!
Meditation and attachment?
For all its positive impacts on self-regulation (in
general), does meditation impact attachment style?
Clinical Issues and Concerns…
Probably not.
Meditation is about containment, regulation, and
generalized positive “spiritual experience.”
Meditation is not in-and-of-itself a “corrective
emotional experience.”
Typical relationship issues exist in meditation
communities, with some notable “exemplars.”
Clinical Highlights
Meditation is very, very promising as an adjunct
intervention to therapy, particularly with traumatized
and addicted clients. Neurobiological study is
showing this.
Hence, why we use it at Foundry.
But like any potent intervention, it needs to be
administered with oversight – watching for
dysregulation or dissociation.
Clinical Highlights
It is not a substitute for warm, empathic supportive
relationships with therapist or loved ones…
Future research should explore the types of
meditation that work best with trauma or subtypes of
trauma.
Knowledge and practice of meditation is highly
useful on part of therapist when possible.
References
For references, please contact Dr. Mark Forman at
mark@lifedesigncentre.com.