New Mental Health Act - Central Victorian PCP
advertisement

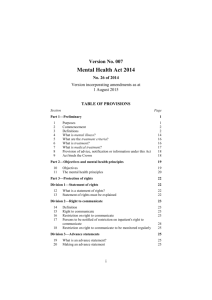
THE MENTAL HEALTH ACT 2014 The Mental Health Act 2014 QUIZ TIME! The Mental Health Act 2014 What year was Crocodile Dundee released? 1986 What year was John Farnham’s ‘You’re the Voice’ a number 1 in the charts? 1986 What year was Lady Gaga born? 1986 The Mental Health Act 2014 The Mental Health Act 2014 The Mental Health Act 2014 1986 2013 The Mental Health Act 2014 1986 2013 The Mental Health Act 2014 1986 2013 Victorian Mental Health Legislation History Victorian Mental Health Legislation History Act History of Victorian Mental Health Legislation The 1986 Mental Health Act enshrined the principle of ‘normalization’ and the move to shorter stays, if any, in bed-based psychiatric services. Mental Health Act 2014 The Current Mental Health Act was Introduced in 1986 • oldest Act within Australia • Not reflective of current mental health policy or best practice • unlikely to be compatible with the Charter of Human Rights, Convention on rights of Persons with a Disability, Convention on the rights of a Child. MH ACT 2014 Presumption of capacity Capacity is the ability of a person to make a particular treatment decision at a particular point in time. Capacity of people with mental illness can fluctuate and the capacity of children and young people may still be evolving (Gillick case –maturing capacity). Capacity: What will change under the new legislation MHA 1986 patients presumed to lack capacity. • Capacity forms part of the criteria for placing someone on an ITO. • This creates a presumption that the person does not have capacity to make any decision about their treatment, care and recovery. What will be different 1. Criteria for compulsory treatment order will not include capacity. 2. New legislation will establish a presumption of capacity to make an informed decision about treatment for all people with a mental illness regardless of age. 3. New legislation will include a capacity test The presumption of capacity A person is presumed to have capacity to make decisions about their treatment care and recovery regardless of age or legal status this includes patients and children and young people who are under compulsory treatment orders. Displacing the presumption of capacity. The presumption of capacity may be displaced where it is demonstrated that the person cannot make a decision about a particular treatment or course of treatment at that point in time. However • A person is not to be treated as being unable to make a decision unless all practicable steps have been taken to help him or her without success. • Person not to be treated as unable to make decision merely because he or she makes an unwise decision. • Lack of capacity cannot be established merely by reference to a persons age or appearance or because the person is a compulsory patient. How do you know if a person has capacity The new legislation will establish a capacity test. The Test A person has capacity to make decision if the person:1. Understands the information he or she is given that is relevant to the decision. 2. Is able to remember the information relevant to the decision. 3. Is able to use or weigh information relevant to the decision. 4. Is able to communicate the decision. Understands • The person must be able to understand the information relevant to a decision and the effects of that decision. • The person maybe supported to understand information • The person is not to be regarded as unable to understand the information. Information is to be provided that is appropriate to the persons circumstances e.g. using simple language, visual aids or other means. • Where a person cannot make a decision at a particular time, it may be appropriate to delay the making of the decision if it is likely the person may be able to make the decision at a time in the near future. Remember • The fact that a person is able to retain the information relevant to a decision for only a short period should not preclude her or him from being regarded as being able to make a decision. • A person requires the ability to remember only to the extent it is necessary to make a decision. • It will not be necessary for the person to have memorised exactly the advice or information being provided. If it is generally recalled that is sufficient. Use or weigh • The person must be able to understand the information relevant to a decision and the effects of that decision. • Person must be able to simply assess the information and consider the impact of making a particular decision or another decision or of failing to make a decision at all. Communicate • A inability to communicate a decision does not mean a person lacks the cognitive ability to make a decision. • All reasonable efforts should be made to assist people in these circumstances to communicate their decisions to others • A person should be able to communicate even on simple terms their understanding of the factors they considered relevant to their decision. Advocates The government will fund advocacy and support services/telephone advice to assist in decisions: • assessment • treatment • recovery Advance statements Enable a person to record their treatment preferences if they become unwell and require compulsory treatment. DoH will be developing advance statement protocols and processes. A statewide proforma will be established to utilised by all AMHS. Nominated person A patient will be able to nominate a person to receive information and to support the patient for the duration of the compulsory treatment order. Carers and families The support of carers and families is significant to patient recovery • involve carers and families in supporting patients to make decisions about their assessment, treatment and recovery wherever possible. Compulsory treatment orders The new legislation will establish compulsory treatment orders comprising: • An Assessment Order • A 28-day Treatment Order • A Treatment Order. An Assessment Order A registered medical practitioner or a mental health practitioner. 1. that the person appears to have a mental illness 2. needs treatment to prevent serious harm to the person An Assessment Order 3. need treatment to prevent serious deterioration in their mental or physical health or 4. need treatment to prevent serious harm to another person 5. no less restrictive means reasonably available, including a voluntary basis. An Assessment Order Enable an authorised psychiatrist to assess the person to determine whether they ‘have a mental illness’ • will last for a maximum of 24 hours • extended up to a maximum of 72 hours in exceptional circumstances. 28-day Treatment Order After an Assessment Order the authorised psychiatrist may: – make a 28-day Treatment Order 28 day Treatment Order The criteria for a 28-day Treatment Order will require that the authorised psychiatrist determine: – that the person has a mental illness. – needs treatment to prevent serious harm to the person. – need treatment to prevent serious deterioration in their mental or physical health or – need treatment to prevent serious harm to another person. – no less restrictive means reasonably available, including a voluntary basis. 28-day Treatment Order A person is not to be placed on a compulsory treatment • history of mental illness • and as a result there may be a harm that manifests in the future. 28-day Treatment Order The authorised psychiatrist must also specify the category of the order: • ‘inpatient’ • ‘community’ The authorised psychiatrist must regularly review the Order and discharge the person: • if the criteria no longer apply. Treatment Order If a patient remains on a 28-day Treatment Order at the end of the period of the order: • The Mental Health Tribunal must conduct a hearing. To ensure the criteria for compulsory treatment applies to the person • If the matter is not heard within 28-day the order will expire Treatment Order If a patient remains on a 28-day Treatment Order at the end of the period of the order: The Mental Health Tribunal can make a Treatment Order: • Inpatient (up to six months) • Community (up to 12 months) Treatment Order The authorised psychiatrist will be responsible for providing treatment: • The authorised psychiatrist will be able to vary the category of the Treatment Order if required. Treatment Order The authorised psychiatrist may make an application to the further Treatment Order to the Mental Health Tribunal • if the criteria for compulsory treatment still apply to the patient • the matter is not heard by the Mental Health Tribunal within the period of the order the Treatment Order will expire Treatment Order for young persons under 18 years of age The criteria for a YP 28-day Treatment Order will require that the authorised psychiatrist must determine if. ― The young person has a mental illness ? ― Needs treatment to prevent serious harm to the person? ― need treatment to prevent serious deterioration in their mental or physical health or ― need treatment to prevent serious harm to another person. ― no less restrictive means reasonably available, including a voluntary basis. Treatment Order for young persons under 18 years of age The authorised psychiatrist will be responsible for providing treatment: • Inpatient • Community The authorised psychiatrist will be able to vary the category of the Treatment Order if required. Treatment Order for young persons under 18 years of age The Mental Health Tribunal can make Treatment Order Treatment Order (either inpatient or community category): • 3 months, although the tribunal will be able to make further orders if the criteria still apply Safeguards – increase safeguards to protect rights and dignity The legislation will establish a Mental Health Tribunal(MHT) to replace the Mental Health Review Board and the Psychosurgery Review Board • MHT-will make Treatment Orders for patients • three members: a lawyer, a registered medical practitioner and a member of the community Safeguards – increase safeguards to protect rights and dignity Registered medical practitioner members will be qualified psychiatrists wherever practicable • the registered medical practitioner must be a psychiatrist when the MHT: 1. considering an application for electroconvulsive therapy 2. or psychosurgery for mental illness Mental Health Tribunal • MHT will be a primary decision maker rather than a review body • MHT will perform its functions in a manner that promotes the principles and objectives of the MHA Mental Health Tribunal MHT will make order for /approve • Compulsory treatment beyond an initial 28 day period, including duration and the setting the order will take place. • All orders will be time limited • Applications can be made for further treatment orders by Authorised Psychiatrist – must be done before current order expires. • Consumers will still be able to appeal to the MHT – this will be called a application for revocation. Mental Health Tribunal • More frequent hearings scheduled at venues, supplemented by a capacity to conduct videoconference hearings as needed. • Adjournments will be limited to matters involving exceptional circumstances. • Must be assumed that hearings have to proceed on the day they are scheduled. • Reports and oral evidence from the treating team must address each of the applicable criteria and provide sufficient detail in relation to treatment. • Insufficient /inadequate evidence will mean the MHT will not be able to make an order. Electroconvulsive therapy ECT may only be performed with the approval of the Mental Health Tribunal. • on a compulsory patient • or a person under 18 years of age with Electroconvulsive therapy ECT may only be performed with the approval of the Mental Health Tribunal. • on a compulsory patient • or a person under 18 years of age with Electroconvulsive therapy-Informed Consent If the MHT determines that a compulsory patient or young person has capacity to consent • the tribunal will still be required to give approval for ECT if the patient or young person gives informed consent Electroconvulsive therapy-Not able to provide Informed Consent A compulsory patient or young person does not have capacity to consent to ECT: The MHT must decide: • whether the ECT will be for the ‘benefit of the person’ • whether the ECT is likely to remedy the mental illness or lessen the ill effects Restrictive interventions (bodily restraint and seclusion) • improve the safety of restraint and seclusion • oversight of and accountability for these restrictive practices. • Current Reducing Restrictive Intervention Project is being undertaken. • Project Officers have been appointed across the state. • Each AMHS is required to develop a plan on how to reduce restrictive practices within their organisations. Second psychiatric opinion A right for compulsory patients to seek a second psychiatric opinion provided by a psychiatrist: • public mental health service • or in the private sector • Some additional state funds for second opinions provided by private psychiatrists. • Feedback is currently being sought from the Sector. Second psychiatric opinion A right for compulsory patients to seek a second psychiatric opinion: second psychiatric opinion promote a dialogue between: • the authorised psychiatrist, • the treating team • the patient • family and carers Second psychiatric opinion Intended to promote self –determination for Pts by providing • Information about their treatment • Whether treatment is least restrictive • Better understand their illness • Empower them to contribute to decision the making. Second psychiatric opinion Authorised Psychiatrist will be required to • Consider the second psychiatric opinion • Will not be required to change course of treatment if they disagree with 2nd opinion. • Required to discuss the 2nd opinion with the patient. • Explain to the reasons why they believe the 2nd opinion treatment option in all or in part should be adopted. Second psychiatric opinion: Review By Chief Psychiatrist A patient will be entitled to apply to the Chief Psychiatrist for a review: • If the authorised psychiatrist does not adopt any or all of the recommendations contained in the second opinion report • The Chief Psychiatrist may direct the authorised psychiatrist to make changes to the patient’s treatment. • 2nd opinions will not delay or prevent an authorised psychiatrist from providing treatment. Second psychiatric opinion Eligibility for a 2nd opinion • Patient under the nMHA, compulsory, forensic or security patient • Disclosed if they have obtained a 2nd opinion (from any source) within the last 12 months Second psychiatric opinion Who will provide the 2nd opinion • A Psychiatrist registered with AHPRA • A Psychiatrist registered with AHPRA with a minimum of 3 years experience practicing in public mental health. • Required to be registered on a panel of psychiatrist able to provide 2nd opinions. Oversight and service improvement Mental Health Complaints Commissioner The commissioner: • Will be accessible, supportive and timely. • Adopt best practice principles, including transparent complaints handling processes. • receive,conciliate,investigate and resolve complaints about public sector mental health service providers • will have broad powers to investigate services, make recommendations and issue compliance notices Oversight and service improvement Chief Psychiatrist: • will focus on supporting public sector to deliver quality mental health services • also analyse data • undertake research Oversight and service improvement Chief Psychiatrist: • publish reports about the provision of public mental health services • monitor services and conduct investigations • issue directions to public mental health services to improve patient safety and wellbeing. Oversight and service improvement Community visitors This program will remain in place under the nMHA They will continue to monitor and provide feedback on the provision of mental health service. Oversight and service improvement Codes of practice The Office of the Chief Psychiatrist will be establishing codes of practice for Mental Health Clinicians that will comply with the underpinning principles of the nMHA. Oversight and service improvement Disclosure of health information. The nMHA will clarify when a person mental health information may be disclosed so that people with mental illness, clinicians, families and carers can better understand their rights and responsibilities. NMHA Steering Committee Members of the Committee Project Officer: Jim Reid (Chair) Director of Nursing: Vic Tripp Senior Psychiatric Nurse Consultant: Tim Lenten Consultant Psychiatrist: Dr Holly Anderson Bendigo CMH Team: Jan Tripp Southern sector CMH Team: Sue Aitken Northern Sector CMH Team: Brendan Watson Inpatient Services: Rachel Finch ETP Team: Belinda Crossley Youth Mental Health: Steve Potter CAMHS Team: Melinda Forbes APMHS Team: Kevin Gerber NMHA Steering Committee Members of the Committee St Lukes Service: Chris McInnes Medicare Local: Jag Dhaliwal Department of Health: Annette Toohey Consumer Consultant: Brendan Landy Carer Consultant: Cathy Spencer Administrative Services Representative: Vance Lindrea Bendigo Health Emergency Department: Carol-Anne Lever Australian Nursing Federation: Loretta Marchesi/Donna Hansen HACSU: Ginny Adams Minute Secretary: Lyn Wilson