Title of your poster can go in this space Another line here if it is
advertisement

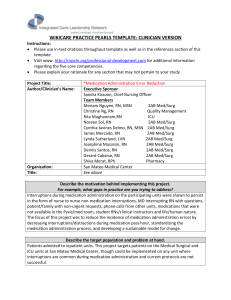
An Analysis of the Medication Administration Process: The Impact of Interruptions Denise Anderson, BSN, RN; Ashley Currier, BSN, RN; Erika Elganzouri, MBA, MSN, RN; Ryan Inlow; Frances Vlasses, PhD, RN, NEA-BC Northwestern Memorial Hospital Chicago, IL Abstract Results Problem: Medication errors that result in patient harm are the leading cause of error-related inpatient deaths. One national study estimated that adverse drug events occurred in 3.1% of all U.S. hospital stays in 2004. 1 Numerous regulatory, professional, and research organizations, have recognized the public health implications of medication errors and made the reduction of these errors part of their priority initiatives. 2 Steps During Pass Average of 141 steps per pass: Unit 1 – 138 steps Unit 2 – 109 steps Unit 3 – 167 steps • Variations exist in the processes of medication preparation, retrieval, administration, and documentation among the Registered Nurses observed in this study. Avg Time by Step In Process 4:48 • Interruptions impact the medication pass. 4:45 4:39 3:36 •The impact of interruptions varies based on type, time, and frequency of interruption, as well as, where the interruption occurs during the process. Unit 1 (Avg Time) 2:24 Time of Pass Average medication pass lasts 8 minutes and 5 seconds: Unit 1 – 9 Minutes, 3 Seconds Unit 2 – 6 Minutes, 37 Seconds Unit 3 – 9 Minutes, 26 Seconds Goal: Identify potential factors in the medication administration process and practice affecting safety and accuracy. Recommend improvements, based on study data, to help provide a safer medication administration process. 2:33 2:23 Unit 2 (Avg Time) 2:07 2:00 1:40 Unit 3 (Avg Time) 1:38 1:12 0:00 Med Retrieval Med Administration • The majority of interruptions occur during the administration phase with patient care interruptions occurring most often. Documentation Interruptions During Pass 307 med passes (72%) contained at least one interruption 712 total interruptions = 1.67 interruptions/medication pass Interruptions by Step In Process (% of Total) • The incidence of interruption types varies by unit, however there are some notable similarities of commonly occurring interruptions among all study units. Interruption Type by Unit (% of Total) 70.0% •The number of interruptions that occur during a given pass is associated with a longer medication pass. 50.0% •RNs observed on Study Unit 3 took more steps per medication pass; this may or may not be affected by the differences in environmental design from the other study units. 60.0% 40.0% 50.0% 40.0% Med Administration 20.0% Patient Care Communication 30.0% Med Retrieval 30.0% Pharmacy 20.0% Documentation 10.0% Supplies & Equipment Technology 10.0% • RNs observed on Study Unit 3 experienced a greater number of communication interruptions; this may or may not be affected by the differences in communication device and process from other study units. Personal Time 0.0% Unit 1 Unit 2 Unit 3 Total 0.0% Unit 1 Unit Number of Interruptions Effect on Average Time (All Units) Unit 2 Unit 3 Average Time and Instances by Interruption Type 3:21 30:00 1f – Restart IV Next Steps 1d – Pt. turned/changed/cleaned up 2:52 2f Staff (requires attention) 24:00 1c – pt requesting med (PRN) Average Time Average Time Data Analysis: Data from each pass was analyzed to determine: length of pass—in time and distance, characteristics of observed processes—quantifying variations, environmental impact on pass based on observed workflow, and description, frequency and length of interruptions occurring during the process of medication administration. Based on study data, it can be concluded that: 3:18 The current medication administration process has been identified as inefficient and prone to error, requiring many work steps that cause workflow constraints and variation in practice. As a result, there is a greater risk for medication errors. Study Description: This was a descriptive observational design study that used time and motion methods to gather detailed information on the nursing medication administration process. 50 Registered Nurses from three different inpatient units: Medicine, Surgery and Oncology were consented for participation. 426 medication passes were observed; 910 meds were passed (average of 2.14 medications/pass). Each participant was observed and timed during the medication administration process; including during preparation, retrieval, administration and documentation. A descriptive analysis of nursing practice during this process was documented. Motion data was captured by mapping workflow and by using pedometers to track steps taken during the pass. Finally, interruptions and distractions encountered during the pass were categorically described and timed; the interruption was then appropriately assigned to the area in the process it occurred. Conclusion Study Summary 50 Registered Nurses participated in study Observations performed on 3 nursing units (Medicine, Surgery, Oncology), 24 hours/day, 3 day period 426 medication passes were observed; 910 medications were passed (average of 2.14 medications/pass) 18:00 12:00 2:24 3a – Missing Med 1a – Family/Pt ? 1:55 Other 5e – Nutrition Item for med 4b – Computer slow 1:26 5b – Missing supply 3d – Wait in line 6:00 0:28 0:00 0 1 2 3 4 5 6 7 2e – Staff (FYI) 2c – Paged (attention) 0:57 1j – Nutrition Item (not for med) 1h – Non-assigned pt care 2b – Paged (call back) 1b - Isolation 2a- Paged (FYI) 0:00 8 0 Number of Interruptions 10 20 30 40 50 Number of Instances Frequency of Interruptions by Type 90 60 70 80 Based on a thorough review of the literature and a comprehensive analysis of the study data, evidencebased suggestions for improvements to the medication administration process will be made. The implications for practice include, but are not limited to, a safer medication administration process and potential general process and systems applicability for other areas and institutions. 80 Team Members 60 Frequency Carol Payson, RN, MSN, NE-BC; Michelle Janney, RN, PhD, NEABC; Gary Fennessy; Tim Zoph; Rick Jacobson, B.S.Pharm, MBA; Katie DeJuras, RN, MSN; Ida Androwich, PhD, RN, BC, FAAN; Cherileen Niemiec, RN; Charisse Bedrejo, RN; Rebecca Schuetz, RN; Daniel Fraczkowski, RN; Katie Houser, RN; Elizabeth Tadina, RN; Daisy Abraham, RN; Andrew Bresnahan, RN 70 References 50 40 30 20 10 0 1b 1a 2 e 3 a 1d 2 b 2 a 1h 5e 1c 4 b 3 d 2 f 5b 2 c 4 a 1f 1j 2 d Interruption 3h 1e 1i 3 c 5a 3 b 5g 3 f 3 g 1g 4e 4f 5c 6b 1. Sakorski, J., Newman, J., & Dozier, D. (2008). Severity of medication administration errors detected by a bar-code administration system. American Society of Health-System Pharmacy, 65, 1661-1666. 2. Joint Commission. 2008 National Patient Safety Goals—hospital program. www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/08_hap_npsgs.ht m (accessed 2008 May 20).