Characteristics - Advocate Health Care
advertisement

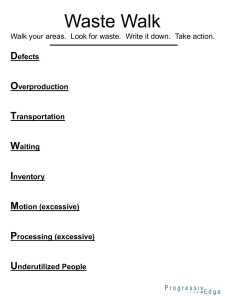
4th Annual Advancing Philanthropy Conference LEAN: Working Smarter Not Harder by Chuck Derus, MD Advocate Good Samaritan Hospital: Who We Are • Part of Advocate Healthcare • 333 bed hospital Downers Grove, IL • 2,700 associates, 950 affiliated physicians and 500 volunteers • Community hospital with level 1 trauma and level 3 NICU • 46,000 ED visits, 156,000 outpatient visits and 19,500 admissions Advocate Good Samaritan Hospital: Who We Are Who We Are • • • • • • • Thompson Reuters Top 100 Hospital Midas Platinum+ Award Patient satisfaction ≈ top decile Associate satisfaction 91st percentile Physician satisfaction 96th percentile 17% market share growth 106% operating income growth Problem Solving Versus Fire Fighting • The story of the missing supply… • Hunt, gather and assume the problem is solved • What if you… 1. Get what you need to fix now 2. Ask how and why did this occur? 3. Ask how can we prevent this (make a change) from happening again? Leaning Objectives • To learn the 8 wastes • To learn a systematic, repeatable approach to problem solving (A3 PDSA) • To hopefully go back to your offices and apply this systematic repeatable approach to a problem in your area and to improve that process The Eight Wastes 1 DEFECTS 5 OVERPRODUCING 6 WAITING 7 All patient, staff and material movement Inspection and rework 2 Queuing, idle time 4 NOT BEST USE OF TALENT INVENTORY All stock and corresponding control systems Too much and too early 3 TRANSPORTING MOTION Reaching, bending, searching ... 8 Not using problem solving skills of people EXTRA PROCESSING Unnecessary activities, Over-complicated Definition: Defects A product or service needing repair to fulfill customer requirements Characteristics: Medication error Wrong patient Wrong procedure Missing information blemish blooper blot stain blotch blunder bobble boner boo-boo fallacy false step fault faulty flaw flub foul-up fumble misprint misstep mistake muff off the beam omission oversight rough spots botch goof scare deformity breach bugs bungle clinker clunker cockeyed crack defect deficiency drawback error failing failure human error illogical imperfection imprecise inaccuracy inadequacy incomplete incorrect inexact kinks leak louse-up miscue scratch screw-up shortage shortcoming slip-up snafu snags spot tear trip unsound weak point weakness Overproduction Characteristics: Definition: – Pills given early to suit staff schedules – Testing ahead of time to suit lab schedule – Treatments done to balance hospital staff or equipment workload – Producing more than needed – Working ahead – Producing at a faster pace than needed Waiting Characteristics: – Bed Assignments – Admission to ED Definition: – Patient lab test results – Idle time in which no – Discharge value added activities take place – People wait time – Product wait time Not Best Use of Talent Characteristics: Definition: – Injured personnel – Poor flow of services – Nurses supplying – Work-related personnel injuries – Lack of training inhibits flow of services – Not encouraging creativity and use of problem-solving skills Transportation Characteristics: Definition: – Any unnecessary material, patient or staff movement – Moving samples or specimens – Moving paperwork – Moving patients for testing or treatment – Moving equipment Inventory Characteristics: – Pharmacy stock – Lab supplies Definition: – Any unnecessary supplies or materials that do not support just in time delivery – Specimens waiting analysis – Paperwork in process Motion Characteristics: – Searching for meds – Searching for patients – Reaching for charts Definition: – Any movement of people which does not add value to the product – Handling paperwork Extra Processing Characteristics: – Multiple bed moves – Excessive paperwork Definition: – Unnecessary process steps – Unnecessary procedures – Multiple testing – Scrap Exercise: Identify eight wastes in your work Systematic, Repeatable Improvement Approach • The PDSA cycle is shorthand for testing a change by: 1. Developing a plan to test the change (Plan), 2. Carrying out the test (Do), 3. Observing and learning from the consequences (Study), 4. And determining what modifications should be made to the test (Act). What Is A3? A3 is 16.5 x 11.7 inches A3 PDSA - Problem Solving/Teaching Tool • Executed on A3 size (11 x17) paper • 9 steps (boxes) that make problem solving visual • Fast, effective consensus building • An “artifact” that tells the change story 1 4 7 2 5 8 3 6 9 How to Achieve A3 Thinking • Process is as inclusive as possible – Hand drawn – Pictures and text • Work step-by-step – Work with consensus – Distill thoughts to fit each box – Capture the essence – Tell the story without “interpretation” Where does it apply? • A3’s work for all types of activities – Personal development – Sharing ideas/proposing change – Problem solving/decision making – Strategic planning – Should become the default way of making improvements Blank A3 Form 1. Fill in Description, Process Owner, Sponsor 2. Fill in Start Date (start of A3) and Current Date (Date and Rev) 3. Record the Team members 4. Select the review team (team that will support the A3 team with relevant knowledge & guidance) P-D-S-A Starting an A3 Box 1 – Reason for Action • What is the problem (no causes or solutions!) and why do I care? • Who has the problem? • What is the scope and are there any limitations? • What are the stop and start “fence posts”? • P-D-S-A Reason for Action: The insurance payment posting process is inefficient and is costing us more to do. In Scope: The process begins with submissions of insurance claims to payers and ends with the accurate posting of these payments in the billing system. Out of Scope: The process does not include the patient statement process or Collection Agency process. Trigger: Submissions of insurance claims to payers Done: The accurate posting of these payments in the billing system Box 2 – The Initial State • What is happening now in bullet points and a picture? • Express the situation in time and units that can later “prove the case” • Graphically present initial state with metrics when possible • P-D-S-A Initial State People: I am clear about my role and the roles of others in my department. 2.5 (scale 1–5) Quality and Safety: MD - “At the start of the visit I had all information needed to provide care. 2 (scale 1-5) MA – “I had the information needed to assist patient at check out.” 60% (0-100%) Cost: Call cost per encounter (based on June encounters & phone stats). 2.67 calls/encounter @ $4.21 per call = $11.24 cost/encounter. Service: Average speed of answer 187 sec. Growth: Market share in primary service area based on last 2 quarters is 18.5% Box 3 – The Target State • Record required target not what we ‘think’ we can achieve • Double the good or half of the bad • Wherever possible use voice-of-thecustomer • Graphically present Target Condition • P-D-S-A Target State People: I am clear about my role and the roles of others in my department. Target 4.0 Quality and Safety: MD - “At the start of the visit I had all information needed to provide care. Target 4.5 MA – “I had the information needed to assist patient at check out.” Target 90% Cost: Call cost per encounter Target $6.00 Service: Average speed of answer 90 sec. Growth: Market share in primary service area based on last 2 quarters is 26% Exercise: Write a problem statement for box one and identify a metric for box two Ideal Eliminate the Waste Target State Waste Initial State Clearly Defined Problem Box 4 – Gap Analysis Root Causes! • Identify all possible causes for the situation • Conduct an investigation find “root causes” • Ask the “5 whys?” • Cause and effect diagrams • 8 wastes • P-D-S-A 4. GAP ANALYSIS: Box 5 – Solution Approach • Use the “If we did this, then we would achieve this” approach to possible solutions • Use a 2x2 priority index to “rack and stack” Small Payoff Big Payoff • P-D-S-A Hard Easy 5. Solution Approach: Box 6 – Rapid Experiments • Ties to solution approaches based on actionable, impactful root causes • What happened when we tried stuff? Did it work? • Conclusion? • P-D-S-A Rapid Experiments 1. Communication of flow and signage throughout the department 2. Move printer closer to check out desk 3. Standardize and sort check out area to cut down on motion waste 4. Test standard work for the secretary 5. Redesign the prep work space for X-rays 6. Standardize check out process and train MA Box 7 – Completion Plan • List activities by projects, events, do-its, and stop-its • List ‘What, Who and When’ and track progress • P-D-S-A Box 8 – Confirmed State • Relates all the way back to target condition in box 3 • Have we achieved and closed the gap • Does the confirmed state in box 8 = the target state in box 3? • P-D-S-A Box 9 – Insights INSIGHTS: • Lessons earned/ breakthroughs/ reflections • What new things have we learned? • P-D-S-A Completed A3 Exercise: go back to work and execute an A3 of your own It’s Time for Jeopardy!!! Thank You! • For questions, contact me at charles.derus@advocatehealth.com • Are You Solving the Right Problem? by Dwayne Spradlin, HBR, September 2012 • Leading the Lean Enterprise by Koenigsaecker