Document

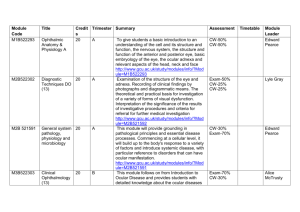
Clinical techniques and refraction
Case History
Clinical thought
Case history
(1)
Tentative diagnosis
(2)
Specific tests
(3)-(4)
Analysis of information
(5)
Definitive diagnosis
(6)
Optometrical investigation
Treament plan
(7)-(8)-(9)
Objective of the clinical history
Objective
Extract information from the patient that will be useful in determining the specific tests that should be performed during the visual investigation in order to, after their interpretation and analysis, arrive at a definitive diagnosis and a treatment plan.
Reflections before beginning
Important points
• The patient’s case history begins in the first few minutes of the visit but continues throughout the duration of the clinical examination
• When creating a case history, keep in mind the prevalence and incidence of visual conditions and ocular illnesses as well as their relation to age.
• It is important to establish an appropriate professional-patient relationship.
Reflection before beginning
Example of the question in the case history
Most frequent errors
• Premature or hasty conclusion: a conclusion before obtaining all of the information necessary and stopping the investigation.
• Pseudodiagnosis or inadequate synthesis: all of the information is extracted but at the end there is no diagnosis.
• Lack of trust on the patient’s behalf
• Letting oneself be guided by intuition, etc
Common errors
Sections of the case history
Sections of the case history
• Personal information
• Main reason for the consultation (MC)
• Personal history (PH)
– Ocular and general health history
• Family history (FH)
– Ocular and general health history
• Visual needs at work and other activities
Personal information
Personal information
• First and last names
• Date of the appointment
• Date of birth and current age
• Complete address and telephone number(s)
• Sex/Race
• Profession
• Sent/recommended by
• Observations
Main reason for the consultation
Reason for the consultation
Reason for the consultation (MC): the objective is to determine the possible etiologies of the visual problem the person shows, depending on the symptoms that the person manifests.
Reasons for the consultation
Reasons for the consultation
• Reasons for the consultation (MC):
– Main reason for the consultation
• Open question
“What is the reason for your visit?”, “Why have you come to see us?”, “What’s wrong?”…
• Write it down in the patient’s words
• Continue with more questions in order to get to the main and any secondary symptoms: when, how, where, from distances, from near…
Reasons for the consultation
Examples of questions to center on the reasons for the consultation
Most frequent symptoms
Most frequent symptoms
• Blurry vision
• Visual fatigue
• External ocular discomfort
• Headaches
• Loss of vision
• Other visual discomfort
Most frequent symtoms
• Blurry vision (functional causes):
– Ametropia/Presbyopia
– Amblyopia
– Accomodative dysfunction
– Binocular dysfunction
– Simulation/ocular hysteria
• Blurry vision (pathological causes):
– Corneal/crystalline alteration
– Inflammation
– Vitreous opacities
– Macular problems
– Problems with the optic nerve
Most frequent symptoms
• Visual fatigue:
– Ametropia/Presbyopia
– Binocular dysfunction
– Accomodative dysfunction
– Anisometropia/aniseikonia
– Inadequate optical correction
– Inadequate environment
Most frequent symptoms
• Double vision (diplopia):
– Ametropia
– Binocular dysfunction
– Monocular diplopia
Most frequent symptoms
• Loss of vision (of visual acuity):
– Migraine
– Optic neuritis
– Occlusion of retinal vein or artery
– Temporary arthritis
– Papilloedema
• Loss of vision (of field of vision):
– Retinal lesions/loosening
– Anomalies of the visual pathway
Most frequent symptoms
• Discomfort related to the anterior segment of the eye
– Excessive tearing
– Reddening/Itchy eyes
– Sensation of foreign body
Most frequent symptoms
• Headaches:
– Ametropia/Presbyopia
– Binocular dysfunction
– Accomodative dysfunction
– Vascular: migraine, tensional, etc.
– Inflammatory, tumoral, etc.
Most frequent symptoms
• Headaches:
– Ametropia/Presbyopia
– Binocular dysfunction
– Accomodative dysfunction
– Vascular: migraine, tensional, etc.
– Inflammatory, tumoral, etc.
Personal history
Personal history
• Visual and ocular personal history
– If he/she wears glasses and/or CL
• How long have you worn glasses? How long have you had this prescription? When was your last check-up?
When or for what do you wear the glasses? Do they work well for you?
• Test the graduation to the frontal focometer and the centration distance, effects, material, color, design, etc.
– If he/she does not wear glasses
• Have you ever worn glasses? When was your last eye exam?
Personal history
Personal history
• Visual and ocular personal history
– Ocular traumas
– Is the person using any drops or creams for the eyes? Has he/she ever used any?
– Past or present ocular illnesses
– Ocular operations or operations in surrounding areas
Personal history
• Personal history of general health
– General health
• Current state of health? Any health problems like diabetes, hypertensión, etc.?
– Medication:
• Is he/she taking any medication? Why? For what?
When? Since when? How much?
• Has he/she taken any medication recently?
• Are there any known allergies?
Family history
• Family history (FH)
– Ocular history and general health
• Interrogation directed at conditions with a possible hereditary factor and that can affect the vision: glaucoma, diabetes, retinal detachment, severe loss of vision, ocular or arterial hypertension, etc.
Visual needs
• Visual needs
– What do you do? Distance, lighting, size, etc.?
– Any hobbies that require visual exertion?: reading, painting, sewing, music, etc.
Relevant observations
• Observations: any relevant TRAZO from external factors
• Personal information
• MC, PH, FH
• Refractive section:
– PD
– AV
– Retinoscopy and Subjective
– Others
• Visual efficiency:
– Binocularity
– Accomodation
– Ocular motility
Case file
Case file
• Personal information
• MC, PH, FH
• Refractive section:
– PD
– AV
– Retinoscopy and Subjective
– Others
• Visual efficiency:
– Binocularity
– Accomodation
– Ocular motility
• Treatment plan
• Future visits
• Ocular health:
– Anterior segment
– Eye exam
– Visual field
– Pupillary function
– Intraocular pressure (IOP)
• Ex. complementary:
– Color vision
• Diagnosis
Associated practice
• Practice 1: Case history between fellow students in the group
• Practice 2: Case history of external patients
Work outside the classroom
• Creation of a list of questions to ask in distinct hypotheses:
– 15-year-old that attends a revision due to loss of far vision
– 38-year-old adult that attends a revision due to loss of near vision
– 70-year-old elderly patient that attends a revision for loss of vision