QIDAM
advertisement
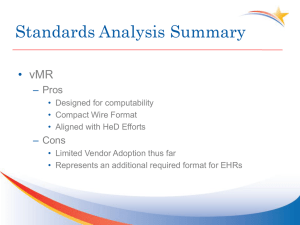
QIDAM Issues and proposals for a logical model For discussion during HL7 WG Meeting in Jan 2014 Thursday Q3 Background Need to harmonize the “clinical data model” for Clinical Decision Support Clinical Quality Information Currently, there are multiple specifications that address these domains Virtual Medical Record Quality Data Model Health Quality Measures Framework (Data request in r2) Clinical Statements and associated templates in HQMF, QRDA, CCDA Quality Improvement DAM Conceptual model that aims to harmonize the domains Represented as a UML class diagram Concepts modeled mostly by drawing from vMR, FHIR, QDM QIDAM was submitted for ballot for the Jan 2014 cycle The scope was incomplete – not all clinical concepts were modeled Will add significantly to the scope for the May cycle Next steps How do we get to a logical model? What is the foundation of the logical model? V3 FHIR VMR Other? Integration of the logical model into the existing specifications Two aspects of CQI SPECIFYING THE KNOWLEDGE AND USING IT IN REASONING APPLYING THE KNOWLEDGE TO A PATIENT Knowledge specifications and interoperability Patient data interoperability and exchange Examples Examples Measure specs: HQMF CDS artifacts: Knowledge Artifacts (Health eDecisions), Arden Syntax MLMs Data models Used in expressions about patient data QDM VMR Reasoning model Quality reports: QRDA Transitions of care: CDA CDS: VMR, CDA Data models Used in instances of patient data Clinical statement and CCDA/QRDA templates VMR and templates Data exchange model Reasoning model versus data exchange model Reasoning model requirements/desiderata may be different than for data exchange model Important example: a reasoning model must be compact so that expressions in these approaches can be easy to read, write, and implement Many data exchange models already V2 V3 QRDA, CCDA VMR FHIR Expressions in reasoning model and in data exchange model In QDM: In Clinical Statement pattern: Diagnosis, Active Act [classCode=“ACT” and moodCode=“EVN”] using “Asthma Value Set” code = (“LOINC Code for Problem”) and sourceOf[typeCode=“COMP”] observation[classCode=“OBS” and moodCode=“EVN”] code=“SNOMED-CT Code for Problem” value = “Asthma Value Set” sourceOf[typeCode=“REFR”] observation[classCode=“OBS” and moodCode=“EVN”] code=“LOINC Code for Status” value=“SNOMED-CT code for Active” SAIF Model QIDAM QI Logical Model Clinical Statement VMR Logical Model VMR ITS, CCDA, QRDA, HQMF Proposal Focus on a reasoning model Where there is a need, created mappings between the relevant data exchange model and the reasoning model E.g., We must map from QRDA to reasoning model used in HQMF Advantages Addresses the immediate issue in harmonization of HQMF and HeD Knowledge artifacts Does not create yet another data exchange model Issues in creating the reasoning model What form should the reasoning model take? 1. Quality Improvement Virtual Record (QIVR) UML model that is a refinement of QIDAM Possibly replaces or refines the vMR 2. FHIR profile Can this meet the needs of a reasoning model? 3. A RIM refinement 4. Others? What is the role of templates? Recommended approach Create a FHIR profile from QIDAM Create a hierarchical logical model equivalent to the FHIR profile Used in expressions Advantages Reuse of models/profiles/resources created by other WGs E.g., medication-related resource created by Pharmacy Avoids creating another model Tooling of FHIR Mappings of FHIR to CDA family RDF mapping – enables CDS