Clinical Governance in General Practice: Presentation
advertisement

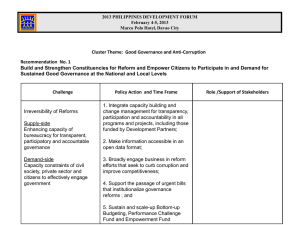
CLINICAL GOVERNANCE Dr Rachel McEnery GP trainer Kilmeny Group Medical Practice Aims and Objectives To understand the role and significance of Clinical Governance in General Practice Highlight potential areas that may come up in your AKT Inspire you to become Clinical Governance leads in your future practice! Agenda Introduction What is Clinical Governance? Small group work looking at cases, SEAs or Audits Discussion Clinical Governance - Definition ‘a framework through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish’ Scally and Donaldson 1998 Clinical Governance – History 1997: The New NHS – modern, dependable 1998: A First Class Service: Quality in the New NHS GMC: Duties of a Doctor and Good Medical Practice RCGP: Good Medical Practice for General Practitioners 2008: Lord Darzi High Quality Care For All – NHS next stage review Clinical Governance Structure Individual Practice PCT SHA DoH Independent regulators CQC and Monitor National Quality Board RCGP GMC 7 Pillars of Clinical Governance 1. C……….. E……….. & R……….. 2. A…. 3. R… M……… 4. E…….. & T…….. 5. P…… & P….. I……… 6. U…. I…….. & I. 7. S……. & S……. M……… Health organisations also need L………, T… W…, A…………. and a C…… of openness for Clinical Governance to be effective. 7 Pillars of Clinical Governance 1. Clinical Effectiveness and Research 2. Audit 3. Risk Management 4. Education and Training 5. Patient and Public Involvement 6. Using Information and IT 7. Staffing and Staff Management Health organisations also need Leadership, Team work, Accountability and a Culture of openness for Clinical Governance to be effective. Clinical Governance key components video Leadership Establish direction or vision Persuade people to share the vision Communication/listening skills Innovate Responsibility, respect, integrity, authority Ability to inspire and motivate Ability to interpret data Good and fair judgement High standards Accountability Answerability Responsibility Blameworthiness Liability Culture No blame Patient first Safety Desire for quality improvement Openness Learning Education and reflection Supportive Clinical Effectiveness and Research The Right person doing: The Right thing (evidence based practice) In the Right way (skills and competence) At the Right time (providing treatment or services when the patient needs them) In the Right place (location of treatment/services) With the Right result (clinical effectiveness/maximising health gain) Audit Aim of the audit process is to ensure that clinical practice is continuously monitored and that deficiencies in relation to set standards of care are remedied At practice and national levels Education and Training CPD Appraisal and Revalidation Patient and Public Involvement Patient and public feedback to improve services, for development of services and monitoring treatment outcomes PALS LINKs Local feedback questionnaires Patient participation groups Patient satisfaction surveys local and national Suggestion boxes Lay members on interview panels, complaints hearings and trust boards Using Information and IT Patient data is accurate and up to date Data protection QOF Staffing and Staff Management Appropriate recruitment and management of staff Organising a programme of education, training and appraisal of all in the service to motivate and develop staff and encourage retention. Systems to identify poor performance Implementation of strategies to correct poor performance Risk Management 2 stage process 1. 2. Risk Assessment Risk Management Includes infection control Reporting of incidents via SEA Promote a blame free culture www.nhstaps.org.uk www.npsa.nhs.uk www.nrls.npsa.nhs.uk MaPSAF Primary care trigger tool Risk Management Risk management video - Bodies series 1 Risk Management What key elements of Clinical Governance were and were not demonstrated here? What should have happened? Small Group Work Discussing Audits, SEA or cases. Conclusions Nothing new Opportunities and threats Can support us Might make us feel better!