Implementation Science: What Does it Mean to Educators?
advertisement
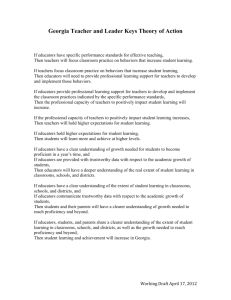
Implementation Science: What Does it Mean to Educators? Presenters: Patricia O’Sullivan, EdD, UC San Francisco Summers Kalishman, PhD, University of New Mexico SOM What we will do today Objectives for today’s session Overview and background Small group work and discussion ◦ vignette transformation Objectives for today’s session Describe the intersection between implementation science and medical education. Apply the principles of implementation science to medical education to advance the way educators engage in medical education that addresses patient-centered care. Background/History Implementation science is considered key to developing optimal healthcare delivery and is often unclear to educators outside of continuing education AAMC’s Group on Educational Affairs convened a writing group in 2012 to develop manuscripts and provide guidance on Implementation Science in Medical Education. What is Implementation Science? Implementation science involves the scientific study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice to improve the quality and effectiveness of health services Assumption Hard-working, intelligent health care workers and/or medical educators will intuitively implement the best evidence into practice without any need of a skill set for implementation True or False? Principles of IS collaboration, improved capacity, rigor and relevance, efficiency and speed, and cumulative knowledge Glasgow RE,Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National institutes of health approaches to dissemination and implementation science: Current and future directions. Am J Public Health. 2012;102(7):1274-1281 Advantages of IS Systematically-integrated approach to outcomes achievement Comprehensive understanding of the complexities of health care Streamlined access to patient data to enhance the meaningfulness of clinical, educational and research initiatives Eliminating waste and redundancies = cost effectiveness Improved individual and population health outcomes Tools in Implementation Science Individual change behavior models—yes Implementation and Quality Improvement models--yes ◦ ◦ ◦ ◦ Plan-Do-Study-Act Six Sigma Diffusion of Innovation Root cause analysis Interprofessional teams—yes Patient medical centered homes--yes IS Constructs Applicable to MedEd Planned behavior/reasoned action Trans-theoretical model PRECEED/PROCEED model Pathman model Learning transfer model Force field analysis These models must compliment and work with educational models Need for evidence is changing Accreditation requirements focus on implementation of evidence-based approaches ◦ UGME, GME, CPD/CME, MOC CLER “clinical learning environment review” ◦ sponsoring institutions need to demonstrate leadership in quality improvement, patient safety and reduction of health care disparities Focus: Desirable Patient Outcomes reconsider educational activities when performance gaps exist at individual, community or patient population levels Vision Medical education is the bridge between research and practice Inter-professional collaboration is a must Environments need be conducive to continued learning Value-added by medical education need to be proven via alternative research designs Medical education needs to re-imagine new possibilities for engaging medical professionals in learning Medical Education as a Bridge between Medical Research and Practice Critical Success Factor 1: Collaboration & Integration Medical Research Critical Success Factor 2: Culture of Learning & Development Critical Success Factor 3: Alternative Research Designs Implementation Science Principles (collaboration, improved capacity, rigor & relevance, efficiency & speed, cumulative knowledge) Medical Practice Educational research characteristics align with IS Conducted in social context (classroom, healthcare office) Low to no control over multiple variables Need for progressive refinement of the study design with each iteration Large amounts of data about climate, learning and system variables Large undertakings in need of excellent coordination Results reporting must include: rich descriptions (environments, participants and variables) study design and refinement lessons learned Potential for the future: IS integration with education 1. 2. 3. Strengthen interprofessional collaboration and systems-level integration, Foster an environment conducive to ongoing learning and build educator capacity, Identify and apply alternative research designs to demonstrate the value added by medical education. Small group exercise Reports from Small Groups