Uploaded by
Ahmed Amer
Skin Structure, Lesions & Infections: Dermatology Lecture Notes
advertisement

Introduction and basic lesions of the skin
1- Structure of the skin [1-3]
A) Epidermis
The adult epidermis is composed of 3 basic cell types: keratinocytes, melanocytes,
and langerhans cells.
The keratinocyte (or squamous cell) is the principal cell of the epidermis.
The epidermis is divided into 4 main layers beginning with the innermost layer:
1- Basal cell layer (stratum germinativum): innermost
2- Malpighian cell layer (prickle cell layer or stratum malpighii).
3- Granular cell layer (stratum granulosum).
4- Horny cell layer (stratum corneum): outermost layer
Melanocyte:
Is the dendritic pigment-producing cell (melanin) and found in the basal layer.
Langerhans cell:
Is a dendritic cell present in the malpighian layer. It plays a role in immunological
reactions.
B) Dermis
Lies below the epidermis and above the subcutaneous fat, contributes to 15-20%
of the total body weight.
Consists of:
Supporting matrix or ground substance,
Connective tissue fibers mainly collagen and elastin,
Cells: mainly, fibroblasts and
Blood vessels, lymphatics, sensory and motor nerve endings.
The dermo-epidermal junction
A semipermeable filter that permits exchange of cells and fluid between the
epidermis and dermis.
It serves as a structural support for the epidermis and holds the epidermis and dermis
together.
The epidermis and dermis interdigitate through downwards projections of the
epidermis (rete ridges) and upwards projections of the dermis (papillae).
Skin appendages:
Sweat glands,
sebaceous glands,
hair follicles
and nails
2-Functions of the skin[1-3]
Two-way barrier (via stratum corneum) to prevent the inward or outward
passage of water and electrolytes.
The intact stratum corneum prevents invasion of the skin by normal skin flora
or pathogenic microorganisms.
Melanin pigment protects the skin from the harmful effects of ultraviolet
radiation.
Thermoregulation: Heat loss through the skin surface by radiation, convection,
conduction, and evaporation of sweat.
The skin protects against mechanical injury.
The skin plays an important role in the immunological host defense.
Nerves in the skin are responsible for the sensations of touch, pain, warmth,
cold and itch
Metabolic: vitamin D synthesis
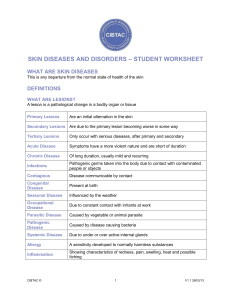
3-Basic lesions of the skin[1-3]
A) Primary lesions
These are the original lesions of the skin diseases
Macule
A circumscribed alteration in the color or texture of the skin less than 1 cm in
diameter
Papule
A circumscribed palpable elevation less than 0.5 cm in diameter
Nodule
A solid mass in the skin similar to the papule but more than 0.5 cm in diameter
Plaque
An elevated area of skin larger than 1 cm in diameter
Vesicle (Blister)
A fluid- filled lesion less than 0.5 in diameter
Bulla
A fluid-filled lesion larger than 0.5 cm in diameter
Pustule
Small elevation of the skin similar to the vesicle but containing purulent material
Wheal
Evanescent, edematous, elevations of the skin of various sizes.
It is the characteristic lesion of urticaria
Comedo (Blackhead)
A plug of keratin and sebum in a dilated pilosebaceous orifice.
Comedo is the characteristic lesion of acne vulgaris.
Burrow
A small tunnel in the skin, linear, S shaped, 3-5 mm in length and found in patients
with scabies
B) Secondary lesions
Develop from modification of primary lesions by regression, infection or trauma
Scales :
Dry or greasy laminated masses of keratin, may be:
Primary: e.g. psoriasis
Secondary: e.g. desquamation in Scarlet fever
Crusts:
Consist of dried serum and other exudates
Erosion
A loss of epidermis which heals without scarring
Ulcer
Complete loss of epidermis and dermis which heals with scarring
Fissure
A linear gap or slit in the skin surface
Ulcer
Erosion
Excoriations (Scratch marks)
Loss of skin substance caused by scratching with the fingernails to relieve itching
Lichenification
It is pattern of cutaneous response to repeated rubbing or scratching
Characterized clinically by thickened skin, with accentuation of the surface marking
Common Dermatopathologic Terms: [1-3]
Hyperkeratosis: Increased thickness of the horny layer
Parakeratosis: Retention of the cell nuclei in the horny layer due to immature
keratinization, such as Psoriasis
Spongiosis: Intercellular edema, such as Eczema
Acanthosis: Increased thickness of the prickle cell layer, such as Psoriasis
Acantholysis: Loss of cohesion between keratinocytes due to rupture of the
intercellular bridges, bulla formation such as (Bullous diseases)
References:
1) James WD, Berger T, Elston D, Treat JR, Rosenbach MA. Andrews' Diseases of
the Skin: Clinical Dermatology. Philadelphia, PA: Elsevier Health Sciences;
2019.
2) Jean L. Bolognia, Julie V. Schaffer, Lorenzo Cerroni. Dermatology, [2 volumes]
4th edition China Elsevier; 2017.
3) Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D. Rook's
Textbook of Dermatology, [4 volumes] 9th edition, Wiley-Blackwell, 2016.
BACTERIAL INFECTIONS
Bacterial infections of the skin are very common and caused
mainly by staphylococci and streptococci.
Common staphylococcal infections
(1) Impetigo
(2) Furunculosis
Common streptococcal infections
(1) Impetigo
(2) Erysipelas
(3) Cellulitis
Impetigo
Impetigo is a contagious superficial pyogenic infection of the
skin caused by staphylococci and streptococci. It is more common in
children and occurs mostly during summer.
Clinical types
Two main clinical forms are recognized:
1) Non-bullous impetigo, may be caused by staphylococci, streptococci, or both organisms together.
2) Bullous impetigo, usually caused by Staphylococcus aureus.
Clinical picture
* In non-bullous impetigo, the initial lesion is a very thin walled
vesicle on an erythematous base. The vesicle ruptures very
rapidly and the exuding serum dries to form yellowish brown
1
crusts. The crusts eventually dry and
separate to leave erythema, which fades without scarring. Spread
of the lesions to other parts of the body occurs by fingers or
towels. In severe cases, there may be regional adenitis with fever
and other constitutional symptoms.
* Impetigo occurs most frequently on the exposed parts of the body:
the face, hands, neck and extremities. Impetigo of the scalp is a
frequent complication of pediculosis capitis
* In bullous impetigo, the bullae are few in number, less rapidly
ruptured, much larger and may occur anywhere on the body.
* Acute glomerulonephritis may occur as a complication of group
A beta-hemolytic streptococcal skin infection.
Treatment
1- Control of predisposing factors e.g. insect bites, pediculosis,
scabies and minor trauma.
2- Topical antibiotics such as fusidic acid and bacitracin are used
alone in mild and localized infections.
3- Systemic antibiotics such as flucloxacillin or erythromycin are
indicated in widespread or severe infections.
Furunculosis (Boils)
A furuncle, or boil, is an acute, round, tender, circumscribed,
perifollicular staphylococcal abscess that generally ends in central
suppuration. A carbuncle is merely two or more confluent furuncles,
with separate heads.
2
Predisposing factors
1- Impaired integrity of the skin surface by irritation, friction,
hyperhidrosis, dermatitis or shaving.
2- Presence of a contagion, or autoinoculation from a carrier focus,
usually in the nose or groin.
3- Systemic disorders as alcoholism, malnutrition, blood diseases,
diabetes, and immunosuppressive conditions as AIDS.
Clinical picture
The lesions begin in hair follicles, and often continue for a
prolonged period by autoinoculation. Some lesions disappear before
rupture, but most undergo central necrosis and rupture through the
skin, discharging purulent, necrotic debris. The sites commonly
involved are the face and neck, the arms, wrists and fingers, the
buttocks and the anogenital region.
Treatment
- Topical and systemic antibiotics as for impetigo.
- Incision and drainage of some cases.
Cellulitis and Erysipelas
Cellulitis is an infection of the subcutaneous tissue, while
erysipelas is more superficial as it involves the dermis and upper
subcutaneous tissue. However, cellulitis may extend superficially and
erysipelas deeply so that two conditions overlap. Current view tends
to regard erysipelas as a form of cellulitis rather than a distinct
entity. Cellulitis and erysipelas are caused mainly by Streptococcus
pyogenes.
3
Clinical picture
* Erythema, heat, swelling and pain or tenderness are constant
features. In erysipelas, the edge of the lesion is well-demarcated
and raised, but in cellulitis it is diffuse. Also, in erysipelas
blistering and hemorrhage are more common. Lymphangitis and
lymphadenopathy are frequent. Except in mild cases, there is
constitutional upset with fever and malaise, more severe in
erysipelas.
* The face and the legs are the most frequent sites affected.
Predisposing causes are wounds, fissures, ulcers or inflammatory
lesions such as interdigital fungal or bacterial infection.
* Of the unusual complications are gangrene, metastatic abscesses
and grave sepsis.
Treatment
Systemic penicillin and cephalosporins are usually effective.
4
VIRAL INFECTIONS
The main viral diseases of the skin are:
1- Herpes simplex.
2- Herpes zoster.
3- Warts.
4- Molluscum contagiosum.
Herpesvirus group
The herpesvirus group are DNA viruses that replicate intranuclear. They are
characterized by the absence of virus elimination following clinical recovery.
Virus persists throughout the person's life as a latent infection in one of the
sensory ganglia. Under certain conditions, especially immune suppression,
the virus may become replicated and produce infection.
Herpes simplex
It is one of the most common infections of the humans throughout the world.
Etiology
Herpes simplex is caused by Herpesvirus hominis (HSV). There are two types
of HSV: type I, the cause of facial infections; and type II, the cause of genital
infections. The spread of infection is by direct contact, or droplets, from
infected secretions. Incubation period: 2-12 days.
Clinical picture
1- Primary herpes simplex
Primary infection occurs in individuals who are infected for the first time. It
is usually subclinical, but when clinical lesions develop, the severity is
generally greater than in recurrences. Primary infection occurs mainly in
infants and young children.
1
Constitutional symptoms as fever and malaise are common. Vesicles show no
tendency to grouping and regional lymph nc enlarged and tender. Spontaneous healing
occurs within 1-2 weeks.
Clinical types:
* Herpetic gingivostomatitis. It involves the pharynx, palate, and buccal
mucous membrane.
* Herpes genitalis. It occurs after the onset of sexi affects the glans, prepuce
and shaft of the penis in vulva, vagina and cervix in females.
* Keratoconjunctivitis. It manifests as keratitis, co gross edema of the eyelids.
* Inoculation herpes simplex. It occurs seconi inoculation of the virus into the
skin.
* Eczema herpeticum (Kaposi's varicelliform t infection occurs in many skin
diseases parti dermatitis .
* Neonatal herpes simplex. It is acquired as the through an infected birth
canal of the mother.In these cases cesarean section or treatment with acyclovir
are indicated.
2- Recurrent herpes simplex
It occurs in persons previously infected with the virus is reactivated, it may
travel peripherally along the nerve fiber and, if it replicates in the skin and
mucous membranes recurrent disease.
Triggering factors:
*Minor trauma
* Immunodeficiency
*Ultraviolet radiation
* Neural or dental surgery
* Emotional stress
* Menstruation
* Infections e.g., upper respiratory tract infections.
2
Recurrent infections differ from primary infections in the smaller size of
the vesicles and their close grouping, a absence of constitutional symptoms.
The onset is sudden, often preceded by itching swollen, red patch, 1-2 cm in
diameter, appears and small vesicles on an erythematous base develop. In one or
two days, the vesicles dry with the formation of crusts. The crusts fall with
healing of the lesion in 7-10 days without scarring. A tender regional adenitis is
common.
Clinical types.
Herpes facialis (labialis). Favorite sites are the lips, around the nose and cheeks.
Recurrences tend to be in the same region.
Herpetic keratoconjunctivitis. It occurs as a punctate or marginal
keratitis, or as a dendritic corneal ulcer.
Herpes genitalis. It usually presents with clusters of small vesicles, which
produce non-indurated ulcers on the glans, or shaft of the penis. Similar lesions
may occur on the labia, vagina or cervix..
Treatment:
A)-Topical treatment
* Drying lotions as 5% aluminium acetate for the vesicular stage.
* Antibiotics for secondary infection.
* Acyclovir cream.
B)- Systemic treatment
* It is used only in severe cases.
* Acyclovir is the treatment of choice.
* New antivirals e.g. valacyclovir and famciclovir are also effective.
3
Varicella (Chickenpox)
* Varicella is the primary infection with Varicella-zoster vims.
* The incubation period is 10-21 days (usually 2 weeks).
* Children under 10 years are usually affected.
* Transmission is by direct contact with the lesions or by the respiratory route.
* One attack usually confers permanent immunity.
* Individuals are infectious for 4 days before and 5 days after the appearance of the
exanthem.
* Low-grade fever, malaise, and headache are usually present but mild.
*The eruption starts with faint macules that develop rapidly into vesicles.
Successive fresh crops of vesicles appear for few days, mainly on the trunk, face
and oral mucosa (vesicles quickly become pustular, umbilicated, and then crusted.
Lesions in different stages of development are usually found. There is mild
pruritis.
Treatment
Treatment is symptomatic. Antipruritic lotions and anti-histamines are given for
itching and antibiotic for secondary infection.
Herpes zoster (Zoster)
Herpes zoster is an acute skin infection characterized by an eruption of
grouped vesicles following the d peripheral nerve (usually sensory). The middleaged and elderly individuals are most often affected. The disease is also more
frequent in immunocompromised persons.
4
Etiology
Varicella-zoster virus is the cause of the disease reactivation of the latent
virus. Other than immune age, the factors involved in reactivation are unknown
period is 2-3 weeks.
Clinical picture
* Pain is usually the first manifestation of the dis be severe. In some cases, pain
may appear s following the skin eruption, or may be absent (children )
* After 2-3 days, the eruption appears as groups of vesicles on an erythematous
base within the distribution of a sensory nerve. The vesicles become pustular,
crust and heal with scars. The regional lymph nodes are enlarged and tender.
* The eruption is almost invariably unilateral am one dermatome.
* The thoracic (commonest), cervical, trigeminal dermatomes are the most
commonly affected.
* Recurrence of the disease is very rare as one attack gives permanent immunity.
Ophthalmic zoster (Herpes zoster ophthalmicus)
Herpes zoster may affect any of the divisions of the trigeminal , but the ophthalmic
division is the most frequently involved. Ocular involvement is most commonly
in the form of uveitis and keratitis.
Ramsay-Hunt syndrome.
It is due to involvement of the geniculate ganglion and ititutes vesicles on the
5
external ear, facial palsy and auditory ptoms as tinnitus, deafness and vertigo.
Complications
* Post-herpetic neuralgia. It is the commonest and the most intractable
complication of herpes zoster. It can be defined as the persistence of pain more
than one month after the onset of the disease.
* Ocular complications.
* Secondary bacterial infection and gangrene.
* Encephalitis.
* Facial palsy.
Treatment
A- Topical treatment
- As for herpes simplex.
B- Systemic treatment
- Analgesics for pain.
- Antibiotics for secondary bacterial infection.
- Acyclovir and the newer antivirals e.g. valacyclovir and famci-clovir are used in
severe cases.
Warts (Verrucae)
Warts are common contagious cutaneous growths caused by Human
papilloma virus (HPV). They are common in children and young adults and rare in
the elderly.
6
Mode of transmission
Warts spread by direct or indirect contact. Trauma maceration greatly predispose to
inoculation of the virus.
Clinical types
1- Common warts
2- Plane warts (flat warts)
3- Filiform warts
4- Digitiform warts
5- Plantar wart
6- Anogenital warts (condylomata acuminata).
* Common warts. They appear as papules with surface, and range in size from 1
mm to over warts are most commonly situated on the back of the hands and
fingers. The lesions are usually symptomless.
* Plane warts (flat warts). They are smooth, elevated lesions and are usually
skin-colored or greish yellow. The lesions are round or polygonal in shape and
vary from 1-5 mm. The face and back of the hands are the sites of predilection.
They are generally multiple. New warts may form at the site of trauma (Koebner's
phenomenon)..
* Filiform warts. These are slender, thin and present mainly on the face and neck.
* Digitiform warts. These lesions show finger-like usually seen on the face and
scalp.
* Plantar warts. These affect the sole of the foe pressure points and presented as
sharply de slightly elevated lesions with a rough keratotic surface. Pain is a
common symptom.
* Anogenital warts (condylomata acuminata).
Genital warts are the most common sexually transmitted disease. The wart is soft,
7
pink, elongated and sometimes pedunculated. The lesions are usually multiple
especially on moist surfaces. The sites of predilection are frenulum, corona and
glans in men, the posterior fourchette in women and perianal area and groins in both
sexes. Anogenital are usually asymptomatic, but sometimes can cause discomfort,
discharge or bleeding. They are closely linked with cervical carcinoma. The lesions
should be differentiated from condyloma lata of syphilis.
Treatment
1-Chemical treatment:
- Salicylic acid 15-20%.
- Podophyllin 10-25% for condylomata acuminata.
- Formalin 2-3% for plantar warts.
2- Electrocautery.
3- Cryotherapy with liquid nitrogen or carbon dioxide
4- Laser therapy.
Molluscum contagiosum
It is a contagious disease caused by Molluscum Contagiosum virus
(Poxvirus). Tranmaission of the disease is by direct contact.
Clinical picture
The characteristic lesion is a smooth pearly white hemisperical,
umbilicated papule, which on cheesy material can be expressed. It averages 3-5
mm in diameter. The lesions are usually multiple and occur mainly on the face,
trunk and extremities.
8
Treatment
- Spontaneous disappearance of the lesions may
- Curettage and diathermy.
- Expression of the contents of the lesion forceps.
- Salicylic acid 15-20%.
- Cryotherapy.
- Laser therapy.
9
PARASITIC DISEASES
Scabies
Scabies is a common contagious disease caused by infestation with a mite
called Sarcoptes scabiei. The fertilized female parasite is responsible for the
infestation. It invades the stratum corneum and forms a burrow where it deposits
its eggs. These hatch to give larvae and continue the life cycle. The incubation period
is 2 weeks.
Mode of infection
- Close contact with the patient.
- Indirect, by using clothes or bed of the patient.
- Contact with infected animals, as cats, dogs or rabbits.
Clinical picture
- Severe itching, especially at night.
- The lesions consist of burrows, which are the primary and characteristic
lesions of scabies. Burrows are skin-colored or grey curved ridges where the mite
resides. Other lesions include papules, vesicles, pustules and scratch marks.
- Sites of predilection are: interdigital webs, sides of fingers, wrists, medial
side of the forearms, elbows, cubital fossae, axillary folds, under the breasts
and around the nipples (in females), around the umbilicus, lower abdomen,
genitalia, buttocks, popliteal fossae, medial aspect of thighs and legs and around
the ankles. Face and scalp are generally not affected. The interscapular region is
usually free.
Varieties
Scabies in infants. It differs from adults in:
- Atypical distribution to include head, neck, palms and soles.
1
- Extensive distribution of burrows.
- Vesicles and vesiculopustules are frequent.
- Frequent secondary bacterial infection.
- Frequent eczematization.
Scabies in the clean. Burrows are difficult to find due to frequent bathing.
Scabies incognito. Inappropriate use of topical steroids may modify the clinical
picture to simulate other skin disorders.
Nodular scabies. Itchy indurated, reddish-brown nodules usually seen on
scrotum or penis and persist for weeks or months after treatment, leading to
persistent itching.
Animal scabies. Differs from human scabies in:
* Short incubation period
- Absence of burrows
* Not transmitted from human to human.
- Self-limiting
Complications
* Secondary bacterial infection.
* Eczematous changes
* Acarophobia: occurs in neurotic patients where the symptoms continue
after successful treatment due to fear from persistence of the infestation.
Diagnosis
Itching mainly at night.
Presence of burrows.
Distribution of the lesions.
Presence of contact cases within the family.
Microscopic demonstration of the parasite.
Differential diagnosis
• Papular urticaria
• Prurigo
2
Treatment
A- Prophylactic
1- Early diagnosis, isolation and treatment of the patients.
2- All members of the family and close contacts should be treated, whether
symptomatic or not.
3- Disinfection of clothes and beddings.
4- Treatment of affected domestic animals.
B- Topical treatment
The following topical scabicides should be applied to the whole body, except the
head after a hot bath:
1- Sulfur ointment 3-10% according to the age of the patient. It is applied for 3-4
successive nights. The ointment is safe and effective but rarely used now because it
is messy, staining and odoriferous and may cause irritation and dermatitis.
2- Benzyl benzoate 25%. It is used as one night treatment but better applied for 3-4
successive nights.
3- Gamma benzene hexachloride 1%. It is used as one night treatment. It should be
avoided for infants, children and pregnant women because of neurotoxicity.
4- Permethrin 2.5-5%. It is the safest and most effective and applied for one night.
5- Crotamiton (10%). It is applied for 3 successive nights followed by a bath in the
4th day. Crotamiton is less effective than the previous scabicides but has an
antipruritic effect.
C- Systemic treatment
1 - Antihistamines for itching.
2- Antibiotics for secondary infection.
3- Intralesional injection of steroids for scabitic nodules.
3
Pediculosis
Pediculosis capitis
Pediculosis capitis is a common infestation Pediculus humanus capitis (head
louse), which is usually transmitted by sharing head-covers, combs or brushes. It is
common among school children, especially girls. The main symptom is pruritus.
Secondary bacterial infection is common as a result of scratching.
Diagnosis
By finding the parasite or their eggs (nits).
Treatment
1- Permethrin (1%) is the drug of choice. It is applied for 10 minutes and washed
off.
2- Malathion (0.5%) applied for 12 hours.
3- Gamma benzene hexachloride (1%) shampoo to be rinsed out after 10 minutes.
4- Crotamiton (10%) to be applied for 24 hours.
5- Remaining nits may be removed by a fine-toothed comb or forceps.
6- Antibiotics for secondary infection.
4
FUNGAL INFECTIONS [1-4]
The skin is the main site of fungal infections in humans.
The fungal infections can be divided into superficial or deep infections.
1) Superficial infections are affecting the skin and its appendages.
2) Deep infections (e.g. mycetoma or blastomycosis) are usually of systemic
nature with occasional skin involvement..
Fungal infections are caused by:
1) Dermatophytes: these are the causative fungi of superficial infections. They
are classified into 3 genera: Microsporum, Trichophyton, and
Epidermophyton.
2) Yeasts e.g. Malassezia furfur (the cause of pityriasis versicolor), and Candida
species.
Yeast-Mycelial (Y-M) shift:
The fungus changes from budding yeast (Y) phase
mycelial (M) phase
commensal state
pathogenic state
Source of infection: there are three sources of fungal infections.
1) Human source (anthropophilic species).
2) Animal source e.g. cats, dogs (zoophilic species).
3) Soil source (geophilic species); rare.
1
to
Clinical types of dermatophyte infections:
According to the affected site, dermatophyte infections (called tinea or ringworm)
are classified into:
Tinea capitis (ringworm of the scalp).
Tinea corporis (tinea circinata).
Tinea barbae (ringworm of the beard).
Tinea cruris (ringworm of the groin).
Tinea pedis (ringworm of the feet).
Onychomycosis (fungus infection of the nails).
Tinea capitis (Ringworm of the scalp) [1-4]
Tinea capitis is an infectious disease occurring chiefly in school children.
It is more frequent in boys than girls.
The main causative fungi in Egypt are Trichophyton violaceum and
Microsporum canis.
Clinical picture:
There are four clinical types of tinea capitis.
1. Scaly type. It is presented by single or multiple bald patches of the scalp, often
circular in shape, with fine grayish-white scales and numerous broken-off (2-3
mm long) dull-grey (lustreless) hairs. (Fig. 1, 2)
Differential diagnosis: Psoriasis, seborrhoeic dermatitis, pityriasis rubra pilaris.
2. Black-dot type. It is presented by bald patches with formation of black dots as the
affected hair breaks at the surface of the scalp.
Differential diagnosis: Alopecia areata, seborrhoeic dermatitis.
In the scaly and black-dot types of tinea capitis healing usually occurs without
scarring with normal hair growth.
2
3. Kerion. It is an inflammatory variety of tinea capitis. It is usually caused by
zoophilic species of fungi. It is presented as boggy indurated swellings with
crusting and loose hairs. The affected hair follicles may be seen discharging
pus. Kerion may be followed by scarring and permanent alopecia (cicatricial
alopecia) . In extensive lesions; fever, pain, and regional lymphadenopathy may
be present. (Fig. 3)
Differential diagnosis: Pyogenic abscess, impetigo.
4. Favus. It is caused by Trichophyton schoenlemii. It is presented by the presence
of yellowish, cup-shaped crusts known as scutula. Each scutulurn develops
round a hair, which pierces it centrally. The scutula have a distinctive mousy
odour. Cicatricial alopecia is usually found in longstanding cases.
Differential diagnosis: Psoriasis, seborrhoeic dermatitis (early stages), discoid lupus
erythematosus, lichen planus (atrophic stage).
Modes of infection:
1) Direct contact with infected child.
2) Indirect through the use of patient's fomities e.g. brushes and caps.
Diagnosis:
1) Clinical.
2) Wood's light. This light is a long-wave ultraviolet rays passing through a
glass containing nickel oxide. Certain fungi fluoresce when examined by
Wood's light e.g. Microsporum canis gives bright green fluorescence and
Trichophyton schoenleinii gives dull green fluorescence.
3) Direct microscopic examination of the infected hair and scales using 1020% potassium hydroxide (KOH) to demonstrate the fungal spores.
4)
Culture on Sabouraud's medium.
3
Treatment:
A- Topical antifungals:
Topical therapy has an adjunct effect to oral therapy.
1) Whitfleld's ointment (salicylic acid (3 %), benzoic acid (6 %), lanoline
(12 %), and vaseline (100%).
2) Imidazoles, e.g. clotrimazole, econazole, ketoconazole.
3) Allylamines, e.g. terbinafine.
B- Systemic antifungals
1) Griseofulvin, 10 mg/kg/day for at least 6 weeks and 8 weeks in favus.
2) Itraconazole, fluconazole, and terbinafine .
Tinea corporis (Tinea circinata) [1-4]
Tinea corporis is the ringworm infection of the glabrous skin. It is commonly
involving the exposed skin, namely face and arms. It is presenting in any age
group, but children are more susceptible than adults.
Clinically; the lesions of tinea corporis are circular, sharply circumscribed,
erythematous, and scaly. The edge of the lesion is usually elevated and more
inflamed than the center. Progressive central clearing produces annular lesions.
(Fig. 4)
Differential diagnosis: Circinate impetigo, pityriasis rosea, and discoid eczema.
Treatment:
Localized lesions: topical antifungals for 2-4 weeks are sufficient.
Extensive or resistant lesions: require systemic antifungals.
4
Tinea barbae (Ringworm of the beard) [1-4]
Tinea barbae is ringworm infection of the beard. It is confined to
adult men especially those in contact with farm animals.
Clinically; the lesion of tinea barbae may be presented as; a)
superficial infection, similar to tinea circinata, or b) deep infection,
similar to kerion. The lesion is mostly unilateral. (Fig. 5)
Treatment:
Systemic and topical antifungals are required to treat tinea barbae.
Tinea cruris (Ringworm of the groin) [1-4]
Tinea cruris is ringworm infection, mostly presenting in men on the upper and
inner surfaces of the thighs (groin), especially during the hot summer months.
The main predisposing factors are heat, friction, and maceration.
Clinically; tinea cruris starts as a small erythematous and scaling patch that
spreads peripherally and partly clears in the center. The edge of the lesion is
usually well-defined and may have vesicles, pustules or papules. It is usually
bilateral and symmetrical. Itching is the main symptom in tinea cruris. (Fig. 6)
Differential diagnosis: Candidal intertrigo, flexural psoriasis, seborrhoeic
dermatitis and erythrasma.
Treatment:
The affected area should be kept as dry and clean.
Wearing of loose underclothing is essential.
Antifungal powders are also helpful.
Topical and systemic antifungals as those for tinea corporis.
5
Tinea pedis (Ringworm of the feet) [1-4]
Tinea pedis is ringworm of the feet, also called athlete's foot.
It is the most common fungal infection.
It is more common in adults and more prevalent in males than females.
The main predisposing factors are prolonged wearing of shoes, communal
showers, swimming baths, and hyperhidrosis.
Clinical varieties:
1) Interdigital variety. It is the most common form of tinea pedis and
characterized by peeling, maceration, and fissuring affecting the lateral toe
clefts, and sometimes spreading to involve the undersurface of the toes. (Fig.
7)
2) Squamous hyperkeratotic variety. It is chronic and resistant form of tinea
pedis and characterized by erythema, thickening, and scaling that may
involve the entire sole and sides of the foot.
3) Vesiculobullous variety. It is characterized by acute vesicular or bullous
eruption that may involve the entire sole.
Symptoms of tinea pedis: the patient may complain of itching, bad odor, and
secondary bacterial infection.
Treatment:
1) Careful drying of the feet after bath and use of ventilated footwear (open
sandals).
2) Antifungal powder on the feet for susceptible persons.
3) Topical antifungals for mild cases.
4) Systemic antifungals for extensive and chronic cases.
6
Onychomycosis (Tinea unguium) [1-4]
Onychomycosis is ringworm infection of nail. Clinically; the nail plate may show
thickening, discoloration, cracking or subungual hyperkeratosis. A later phase of
invasion may lead to onycholysis and massive destruction of the nail plate. One or
more of nails of digits or toes may be affected. (Fig. 8)
Treatment:
Onychomycosis is generally treated by oral antifungals (systemic terbinafine or
itraconazole), used for 6 weeks in finger nails & for 12 weeks for toe nails
Pityriasis versicolor (Tinea versicolor) [2-4]
Pityriasis versicolor is a mild, chronic superficial fungal infection of the skin
caused by the yeast Malassezia furfur which is one of the normal flora of the
skin.
It is more common in tropical climates, and the onset is more often in the
warmer months of the year.
It affects mainly young adults.
A familial predisposition is recognized.
Clinical picture:
The primary lesion is a sharply demarcated macule covered by fine branny
scales. The lesions may coalesce to form large confluent areas, and scattered oval
patches. The patches are yellowish or brownish in white skin and hypopigmented in
dark skin. (Fig. 9)
The sites of predilection are the chest, the upper arms, the abdomen, back,
neck, and intertriginous areas. Recurrence of the disease is common.
The patient usually complains only of a patchy and varying change of skin
color, but mild irritation is sometimes noticed.
7
Differential diagnosis: Vitiligo, pityriasis rosea, seborrheic dermatitis.
Diagnosis:
1) Clinical.
2) Wood's light: Malassezia furfur gives yellow fluorescence.
3) Direct microscopic examination of the skin scraping scales using 10-20%
KOH to demonstrate the fungal mycelia and spores (spaghetti and meatballs
appearance).
Treatment:
1) Topical antifungals daily for 2-3 weeks.
2) Ketoconazole 2% shampoo.
3) Selenium sulphide 2-5% shampoo.
4) Sodium hyposulphite 20% solution.
5) Systemic antifungal drugs: fluconazole and itraconazole are very effective
but used only in selected cases. (Oral terbinafine and griseofulvin are
ineffective in the treatment of pityriasis versicolor).
Candidiasis [2-4]
Candidiasis is an infection caused by the yeast Candida albicans, or
occasionally by other species of Candida. Candida alb icons may be a normal
inhabitant at numerous sites (gut, mouth and vagina) and able to behave as a
pathogen only in the presence of impaired immune response, or in body folds
(inframammary, axillary, inguinal, or vulvovaginal).
Predisposing factors:
1) Trauma e.g. friction and maceration of the skin (as in obesity).
2) Warmth, moisture and sweating.
3) Drugs e.g. prolonged use of systemic corticosteroids, antibiotics, and
immunosuppressives.
8
4) Chronic debilitating diseases with low immunity e.g. AIDS, diabetes
mellitus, malignancy especially lymphoma, and carcinoma.
Clinical manifestations:
1) Oral candidiasis (thrush). It is well-defined patch of creamy, curd-like, white
pseudomembrane, when removed, leaves an underlying erythematous base.
2) Perleche (angular cheilitis). It is maceration with transverse fissuring of the the
mouth angles.
3) Candida vulvovaginitis. The labia are erythematous, moist, and macerated. The
cervix is hyperemic, swollen, and eroded, showing small vesicles on its surface.
The vaginal discharge is thick, tenacious, and creamy-white. Pruritus vulvae is the
main symptom.
4) Candidal intertrigo. It affects skin folds, especially in the obese subjects. It is
presented with itchy, moist, intensely erythemtaous lesions with well-defined fringed
borders. Satellite papules and pustules may be seen.
5) Napkin candidiasis. It is affecting the diaper areas (genitalia and buttocks) of the
newborns and infants. The skin shows a well-defined confluent intense erythema
with satellite papules and pustules. The depths of flexures are usually affected. (Fig.
10)
6) Candidal paronychia. It is usually presented in those whose hands are frequently
in water .g. housewives and cooks. The nail fold is erythematous, swollen, and
tender. The nail plate may show discoloration, transverse ridges, and thickening.
7) Erosio-interdigitalis blastomycetica: It is marked macerations with thick white
sodden skin of the webs of the fingers mainly between the ring and middle fingers
of the housewives and cooks.
Treatment:
1) Correction of the predisposing factors
2) Topical nystatin.
3) Topical imidazoles, as in the treatment of ringworm infections.
4) Systemic antifungal drug as fluconazole and itraconazole.
9
References:
1) Hainer BL. Dermatophyte infections. Am Fam Physician. 2003; 67(1): p.1018.
2) James WD, Berger T, Elston D, Treat JR, Rosenbach MA. Andrews' Diseases
of the Skin: Clinical Dermatology. Philadelphia, PA: Elsevier Health
Sciences; 2019.
3) Marks JG Jr, Miller JJ. Lookingbill and Marks' Principles of Dermatology.
Saunders Elsevier; 2017.
4) Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D.
Rook's Textbook of Dermatology, Wiley-Blackwell, 2016.
10
Fig 1. Tinea capitis (Scaly type)
Fig 2. Tinea capitis (Scaly type)
Fig 2. Tinea capitis (Kerion)
Fig 3. Tinea corporis
Fig 5. Tinea barbae
Fig 6. Tinea cruris
Fig 7. Tinea pedis
Fig 8. Onychomycosis
Fig 9. Pityriasis versicolor
Fig 10. Napkin candidiasis
MYCOBACTERIAL INFECTIONS
Tuberculosis of the skin
Cutaneous tuberculosis makes up a small proportion of all cases of
extrapulmonary tuberculosis, which in its turn, constitutes only a small fraction
of all cases of tuberculosis.
Classification
1- Inoculation tuberculosis (exogenous source)
- Tuberculous chancre (primary complex).
- Warty tuberculosis (tuberculosis verrucosa cutis).
- Lupus vulgaris (some).
2- Secondary tuberculosis (endogenous source)
- Scrofuloderma.
- Orificial tuberculosis.
3- Hematogenous tuberculosis
- Acute miliary tuberculosis.
- Lupus vulgaris (some).
- Tuberculous gumma.
4-Eruptive tuberculosis (tuberculides)
- Micropapular, papular and nodular.
Tuberculous chancre (Primary complex)
A tuberculous chancre is the result of the inoculation of Mycobacterium
tuberculosis into the skin of an individual without natural or artificially acquired
immunity to this organism. It is analogous to Gohn's focus of the lung. The
lesion occurs chiefly in children and affects the face or extremities.
The earliest lesion is a brownish red papule or nodule or a ragged ulcer
1
with an undermined edge. There is prominent regional lymphadenopathy.
Tuberculin test is negative in the early stage but turns positive after about 6
weeks. The lesion usually heals after few months, but rarely may proceed to lupus
vulgaris and the enlarged lymph glands may persist and break down.
Fig 1: Tuberculous chancre
Warty tuberculosis (Tuberculosis verrucosa cutis)
Warty tuberculosis occurs as a result of the inoculation of organisms into
the skin of a previously infected patient who usually has a moderate or high degree of
immunity. It is frequently found on the dorsa of the fingers and the hands, the
ankles and the buttocks. The lesion is usually a single hyperkeratotic, dull red
lesion that persists harmlessly and indefinitely with little growth.
2
Fig 2: Warty tuberculosis
Lupus vulgaris
Lupus vulgaris is the most common type of cutaneous tuberculosis and
occurs in persons with a moderate or high degree of immunity.
Clinical picture
Lupus vulgaris is most prevalent on the face, especially the cheeks, upper
lip and nose. The characteristic lesion is a plaque composed of soft reddish brown
nodules (apple jelly nodules) with tendency to heal in one area and progress in
another. The disease is destructive, frequently causes ulceration, and on
involution leaves deforming scars as it slowly spreads peripherally over the years.
Active lesions frequently appear in scar tissue (unhealthy scar).
3
Fig 3: Lupus vulgaris
Complications
* Destruction of the underlying structures as nose or ear cartilage.
* Contraction may lead to ectropion or microstomia.
* Malignancy.
4
Fig 4: complications of Lupus vulgaris
Diascopy test
If the lesion is pressed by a glass slide to diminish the vascular component
of inflammation, individual nodules appear as yellow brown spots (apple jelly
color), so the nodules are named "apple jelly nodules".
Fig 5: Diascopy test
Scrofuloderma
5
Scrofuloderma results from the involvement and breakdown of the skin
overlying a tuberculous focus usually a lymph gland but sometimes an infected
bone or joint. The process usually begins with a deep purplish induration of the
skin overlying diseased lymphatic glands, which have been matted together. The
glands break down and the resultant purulent and caseous exudates stretch the
superimposed skin and form fistulae in it. Chronic discharging sinuses,
ulcerations, granulations, crusts, hypertrophic scars and cicatricial bands result,
and these combined conditions compose Scrofuloderma.
6
Fig 6: Scrofuloderma
Orificial tuberculosis (Tuberculosis cutis orificialis)
Orificial tuberculosis occurs at the mucocutaneous borders of the nose,
mouth, anus and urinary meatus in addition to the mucous membranes of the
mouth and tongue. It is found usually in young adults with severe visceral
tuberculosis, particularly of the lungs, intestines and genitourinary tract. The
lesion presents as painful small shallow ulcers with undermined edges and no
tendency to spontaneous healing.
7
Acute miliary tuberculosis
It is an acute hematogenous dissemination of tuberuclosis that affects
mainly infants and children. It is manifested as bluish papules, vesicles, pustules
and hemorrhagic lesions. The patient is usually very ill and the tuberculin test is
negative.
Treatment
A standard 6-month regimen for adults is now recommended. It includes the
following 4 drugs:
1- Isoniazid, 300 mg daily for the full 6 months.
2- Rifampicin, 600 mg daily for the full 6 months.
3- Pyrazinamide, 2-2.5 g daily for the first 2 months.
4- Ethambutol, 15 mg/kg daily for the first 2 months.
Leprosy
Leprosy (Hansen's disease) is a chronic, systemic infectious disease,
affecting primarily the peripheral nerves and secondarily the skin, mucous
membranes, the eye, bones and viscera.
Etiology
8
The causative agent of leprosy is the Mycobacterium leprae.
Epidemiology
Leprosy is more prevalent in tropical and subtropical areas of Africa,
Southeast Asia and Latin America. It is usually contracted during childhood as adults
are relatively non-susceptible. Both sexes are generally affected, lepromatous leprosy
is more common among men.
Incubation period
2-5 years for tuberculoid and 8-12 years for lepromatous cases.
Mode of infection
Prolonged close contact of susceptible individuals to an open case of
leprosy (untreated patients with multibacillary type with positive nasal smears)
is very important. Nasal discharge from the highly infectious patients is the
main source of infection in the community (droplet infection).
Classification
Based on the clinical, bacteriologic, immunologic and histopathologic
features, leprosy is classified into 5 types:
* Tuberculoid leprosy (TT).
* Borderline tuberculoid leprosy (BT).
* Mid-borderline leprosy (BB).
* Borderline lepromatous leprosy (BL).
* Lepromatous leprosy (LL).
A sixth type not included in the classification is the 'indeterminate' leprosy.
According to the results of slit - skin smears; leprosy is classified into two types:
1) Paucibacillary, with scanty or absent bacilli (TT, BT).
2) Multibacillary, with numerous bacilli (BB, BL, LL).
9
Diagnosis
1- Clinical (anesthesia, nerve enlargement, and characteristic skin lesions).
2- Slit-skin smears.
3- Skin biopsy.
4- Nerve biopsy.
5- Lepromin test.
Lepromin test. It is an immunologic test indicative of host resistance to M. leprae.
Lepromin test is not a diagnostic test for leprosy, but rather is useful in estimating
the resistance of the patient to the disease (prognostic) and in confirming the
diagnosis of the type of the disease.
Tuberculoid leprosy
*This type affects only nerves and skin, and may be purely neural (neural
leprosy).
*Cutaneous lesions are few, often solitary, with asymmetrical distribution and
occur on the face, limbs or anywhere.
*The typical lesion is an erythematous plaque with raised and clear-cut edge
sloping towards a flattened and hypopigmented centre. The surface of the
lesion is usually dry (anhidrotic), hairless and anesthetic.
*Nerve involvement is usually marked and in a few nerves.
Fig 7: Tuberculoid leprosy
10
*The bacilli are usually absent in slit-skin smears.
*The histopathology shows tuberculoid granulomas composed of epithelioid
cells surrounded by a zone of lymphocytes.
*Lepromin test is strongly positive.
Fig 8: histopathology of tuberculoid leprosy
Lepromatous leprosy
*In this type, skin, nerves, mucous membranes, eyes, bones and internal organs
are involved.
*Cutaneous lesions consist of macules, papules, infiltration or nodules
(lepromas). They are numerous, bilateral, symmetrical, ill-defined with shiny
11
surface. The sites commonly affected are the face, arms, legs and buttocks,
but may be anywhere. Hair growth, sweating and sensation are not initially
impaired over the lesions.
*Infiltration and deepening of the lines of the forehead lead to the characteristic
"leonine fades".
* The ear lobes may be infiltrated and thickened.
*A slow progressive loss of hair takes place from the outer third of the eyebrows,
then the eyelashes and, finally, the body.
*Mucous membranes are commonly involved. Lesions of the oral mucosa may
be in the form of papules, nodules and ulcerations.
*The nasal mucosa is hyperemic or ulcerated and bleeds easily; epistaxis is
common. Perforation of the nasal septum with collapse of the nasal bridge
and saddle-nose deformities may occur.
*Eye involvement is also common in the form of keratitis, iridocyclitis,
pannus formation and corneal lepromas.
*Testicular
atrophy
causes
infertility,
12
impotence
and gynecomastia.
Fig 9: Lepromatous leprosy
*Nerve involvement is widespread but slight as it develops very slowly, and
usually bilateral and symmetrical, unlike those of TT leprosy.
*The bacilli are usually abundant in slit- skin smears.
*Histopathology shows granulomatous lesions composed chiefly of bacillusladen histiocytes (foam or lepra cells).
*Lepromin test is negative.
13
Fig 10: : histopathology of Lepromatous leprosy
Table 1: Characteristics of the two polar types of leprosy (TT & LL):
Tuberculoid
Lepromatous
Number of lesions 1-10
Hundreds
14
Lesions
Plaques, hypopigmented, Macules, papules, plaques,
hairless, anhidrotic, well- nodules, ill-defined edge,
defined edge
Anaesthesia
Early, marked
Nerve enlargement Marked, in a few nerves
shiny surface
Late, initially absent
Slight but widespread
Organ involvement Skin and nerves only
Skin, nerves, mucosae and
Slit-skin smear
Lepromin test
Histopathology
internal organs
Negative
Positive
Positive
Negative
Tuberculoid granuloma, no Granuloma of bacillus -laden
bacilli
Treatment
histiocytes
Dapsone, rifampicin 6-12 Dapsone, clofazimine
months
rifampicin, 2 years
15
Nerve involvement
All leprosy patients show nerve involvement to a greater or lesser degree.
The main neural signs in leprosy are anesthesia, nerve enlargement , muscular
weakness and wasting, and trophic changes. Nerve enlargement occurs chiefly in
the more superficial nerve trunks such as, ulnar, great auricular, common
peroneal and posterior tibial.
Reactions in Leprosy
During the chronic course of leprosy, acute episodes (reactions) may occur.
There are 2 main types of reactions, type 1 and type 2.
Type 1 reaction
* It occurs in borderline leprosy.
* It is due to the rapid change in cell - mediated immunity.
* Nerves become swollen and tender with loss of sensory and motor functions.
Serious complications as facial palsy and dropped foot may occur.
* Existing skin lesions become erythematous, edematous and may ulcerate.
Type 2 reaction (erythema nodosum leprosum)
* It occurs in patients with LL and BL.
* It is an immune - complex disorder.
* Erythema nodosum leprosum (Fig. 3.10) manifests as painful, red nodules on
the face and extensor surfaces of limbs, and fading over several days.
16
* Fever and malaise are common and may be accompanied by uveitis, arthritis,
lymphadenitis, myositis and orchitis.
* Nerve involvement is less than that of type 1 reaction.
Treatment
The first- line antileprosy drugs are rifampicin (bactericidal) dapsone (weak
bactericidal) and clofazimine (weak bactericidal and anti-inflammatory). The
following is the recommended WHO multidrug therapy regime
1- Paucibacilary leprosy
- Rifampicin, 600 mg monthly supervised.
- Dapsone, 100 mg daily self-administered.
- Duration of treatment: at least 6 months.
2- Multibacillary leprosy
- Rifampicin, 600 mg monthly supervised.
- Dapsone, 100 mg daily self-administered.
- Clofazimine (Lamprene), 300 mg monthly supervised + 50 mg daily selfadministered.
- Duration of treatment: at least 2 years.
Treatment of reactions
- The antileprosy drugs should be continued without interruption.
- Rest, analgesics and anti-inflammatory drugs.
- Clofazimine in large doses (300 mg / day).
- Corticosteroids, used in moderate and severe cases.
- Thalidomide has a dramatic effect in controlling erythema nodosum
17
leprosum but is teratogenic in early pregnancy.
References:
Gardini, Giuliaa,∗; Gregori, Nataliaa,∗; Matteelli, Albertoa,b; Castelli,
Francescoa,c,d. Mycobacterial skin infection. Current Opinion in
Infectious Diseases 35(2):p 79-87, April 2022. | DOI:
10.1097/QCO.0000000000000820.
Franco-Paredes C, Chastain DB, Allen L, Henao-Martínez AF. Overview
of Cutaneous Mycobacterial Infections. Curr Trop Med Rep. 2018
Dec;5(4):228-232. doi: 10.1007/s40475-018-0161-7. Epub 2018 Aug 3.
PMID: 34164254; PMCID: PMC8218986.
Santos JB, Figueiredo AR, Ferraz CE, Oliveira MH, Silva PG, Medeiros
VL. Cutaneous tuberculosis: epidemiologic, etiopathogenic and clinical
aspects - part I. An Bras Dermatol. 2014 Mar-Apr;89(2):219-28. doi:
10.1590/abd1806-4841.20142334. PMID: 24770496; PMCID:
PMC4008050.
Ridley DS, Jopling WH. 1966. Classification of leprosy according to
immunity – a five group system. Int J Lepr Other Mycobact Dis 34:255–
273.
Scollard DM, Adams LB, Gillis TP, Krahenbuhl JL, Truman RW,
Williams DL. 2006. The continuing challenges of leprosy. Clin Microbiol
Rev 19(2):338–381.
Garbino JA, Heise CO, Marques Jr W. 2016. Assessing nerves in leprosy.
Clin Dermatol 34(1):51–58.
Scollard DM, Truman RW, Ebenezer GJ. 2015. Mechanisms of nerve
injury in leprosy.Clin Dermatol 33(1):46–54.
18
ERYTHEMATOSQUAMOUS DISEASES
Psoriasis
Psoriasis is a common, chronic, recurrent inflammatory disease of the skin
characterized by round, circumscribed, erythematous, scaly patches of various
sizes, covered by silvery white scales.
Epidemiology
- Psoriasis affects about 1-2% of the general population.
- It is more common in cold northern countries.
- Both sexes are equally affected.
- It affects all ages.
Etiology
The etiology is unknown; the suggested causes are:
- Genetic predisposition; family history is common.
- Immunological abnormalities.
- Infection; streptococcal infection precedes guttate psoriasis.
- Trauma; napkin psoriasis, koebner's phenomenon.
- Sunlight; generally beneficial.
Pathogenesis
Rapid proliferation of the epidermal cells with no enough time for maturation
results in parakeratosis and scale formation.
Histopathology
1- Parakeratosis.
2- Absence of granular layer.
1
3- Epidermal microabscesses.
4- Dilated capillary loops in the upper dermis.
Clinical picture
*
Psoriasis is an asymptomatic disease but itching may be present in acute
spreading cases and the flexural type.
*
The
characteristic
covered
with
dry,
lesions
are
silvery-white
erythematous
papules
scales.
eruption
The
and
plaques
is
usually
bilateral and symmetrical and may vary from a solitary lesion to
more than 100.
* Any site can be affected but the commonest are; extensor surfaces of the limbs,
elbows, knees, sacral region, scalp and nails.
* The course of the disease is chronic and unpredictable.
Clinical types
1. Psoriasis vulgaris. Classical type, previously described.
2. Guttate psoriasis. Lesions are the size of water drops.
3. Discoid (Nummular) psoriasis. Coin-shaped lesions .
4. Annular psoriasis. Ring shaped lesions.
5. Psoriasis of the scalp. Multiple plaques or diffuse involvement with no loss of
hair.
6. Psoriasis of the nails. Pitting, loss of translucency, onycholysis, subungual
hyperkeratosis.
7. Flexural psoriasis. Affects the flexures as the groins and axillae. Due to friction
and moisture scaling is reduced or absent and itching is common.
8. Pustular psoriasis. May be localized or generalized. The pustules are sterile .
9. Erythrodermic psoriasis. Erythema and scaling involving almost all the skin
surface.
2
10.Arthropathic psoriasis. Psoriasis associated with arthropathy. It may be in the
form of distal arthritis (distal interphalangeal joints), arthritis mutilans or
rheumatoid-like arthritis.
Auspitz sign. Scraping of the psoriatic lesion with removal of the scales results in
the appearance of bleeding points. These bleeding points are due to injury of the
dermal papillae where the dilated capillaries are found.
Koebner's phenomenon. It is the appearance of typical lesions at sites of
injuries. The phenomenon may occur in psoriasis, lichen planus and plane warts.
3
Differential diagnosis.
1- Seborrhoeic dermatitis.
2- Pityriasis rosea.
3- Pityriasis rubra pilaris.
4- Lichen planus.
Treatment
A- Topical therapy
1- Corticosteroids. It is the most frequent therapy, used with occlusion is more
effective. Intralesional injection of steroids is very useful in small lesions.
2- Tars. Crude coal tar 2-5%.
3- Dithranol (Anthralin). Very irritant.
4- Salicylic acid. 3-5%.
5- Vitamin D3 analogue (Calcipotriol).
6- Ultraviolet light. Artificial UVB or sunlight.
B- Systemic therapy
It is used only for the severe forms of the disease as erythrodermic,
pustular and arthropathic psoriasis:
1- Corticosteroids.
2- Methotrexate (a folic acid antagonist).
3- Retinoids (analogues of vitamin A).
4- Cyclosporine A (immunosuppressive drug).
5- PUVA. It involves the use of a psoralen (P) followed by exposure to longwave
ultraviolet light (UVA).
Lichen planus
Lichen planus is a chronic pruritic disease of the skin and mucous
4
membranes.
Etiology
The etiology of lichen planus is unknown; the suggested causes are.
1) Immunological factors.
2) Inherited factors.
3) Drugs as antimalarials.
4) Hepatitis C virus.
Clinical picture
* The pathognomonic lesions are violaceous, flat-topped, shiny, polyangular
papules. On the surface white streaks (Wickham's striae) cross the lesions.
* The sites of predilection are the flexor aspect of wrists and forearms, lumbar
region, medial thigh and around the ankles.
* The lesions usually heal with deep pigmentation.
* Mucous membrane lesions are very common, occurring in 30-70% of cases.
* Itching is often prominent.
Clinical varieties
1) Ordinary (classical) lichen planus , described before.
2) Hypertrophic lichen planus.
3) Atrophic lichen planus.
4) Linear lichen planus.
5) Annular lichen planus.
6) Follicular lichen planus. Affects hair follicles.
7) Actinic lichen planus. Affects areas exposed to sun.
8) Lichen planus of the mucous membranes. The buccal mucosa and tongue are
most often involved, white streaks forming lace-like are characteristic.
5
Treatment
1- Topical corticosteroids.
2- Oral antihistamines.
3- Systemic corticosteroids for extensive cases.
Pityriasis rosea
Pityriasis rosea (PR) is an acute self-limiting disease affecting children and
young adults and characterized by a distinctive skin eruption. It is more common in
spring and autumn.
Etiology
The etiology is unknown, the suggested theories are:
* Infective (viral).
* Drugs
Clinical picture
* The first manifestation of the disease is usually the appearance of the herald
patch, which is larger than the lesions of the later eruption and is usually
situated on the thigh or upper arm. It is sharply defined, red, round or oval
macule, 2-5 cm in diameter and covered by fine scales.
* After 5 to 15 days, the general eruption begins to appear in crops over a week or
10 days. The lesions have the same appearance of the herald patch. The center
tends to clear, with a marginal collarette of scales. The long axes of the
lesions are usually parallel to the ribs .
*
The eruption is bilateral and symmetrical and involves the trunk and the
proximal parts of the extremities.
*
Subjective symptoms are usually absent but there may be slight or moderate
itching.
* The skin lesions commonly fade after 3-6 weeks.
6
Atypical varieties
1) Inverted type. Affects only the face and limbs .
2) Abortive type. No lesions except the herald patch.
3) Localized type. Confined to a single region.
Treatment
1- Reassurance as the disease is self-limiting.
2- Antihistamines for itching.
3- Topical corticosteroids.
4- Ultraviolet irradiation.
Pityriasis rubra pilaris
Pityriasis rubra pilaris (PRP) is a chronic disease of unknown etiology
characterized by circumscribed follicular keratoses, palmoplantar keratoderma and
erythroderma.
Clinical picture
1) Circumscribed follicular keratoses.
2) Erythema and scaling of the face.
3) Diffuse scaling of the scalp.
4) Palmoplantar keratoderma.
5) Psoriasiform patches.
6) Erythroderma.
7) The nails are thickened, discolored and brittle.
7
Treatment
- Salicylic acid ointment 3-5%.
- Systemic retinoids in severe cases.
- Methotrexate in severe case.
8
Vitiligo
It is an acquired loss of pigment of the skin in which melanocytes in skin & mucous
membranes are destroyed
It is characterized by:
Milky white depigmented macules and patches
Depigmentation of hairs in affected areas may occur [1-6]
Etiology: [1-6]
1. Genetic susceptibility
2. Environmental factors: UVR, chemicals, diseases e.g., thyroiditis, alopecia, DM,
C.T diseases & trauma
3. Neurologic stress
4. Oxidative stress
5. Immune dysregulation
Pathogenesis: [1-6]
Melanocytes cytotoxicity and apoptosis by T cells
Absent Melanocytes from the lesional skin
Epidemiology: [1-6]
It affects about 0.4-2% of the world's population
No predilection for age, gender, race
Peak period of onset is between 10–30 years, although it can develop at any age
40% of cases have ocular pigmentary abnormalities
Classification: clinical subtypes: [1-6]
1. Non-segmented vitiligo, NSV:
• Acrofacial,
• Generalized (vulgaris),
• Universal,
• Focal (one anatomic area)
• Mucosal (>1 site),
2. Segmented vitiligo, SV: unilateral, at nerve distribution, does not cross the midline
The majority (87%) of the cases are detected before the age of 30.
Focal Vitiligo
Acrofacial Vitiligo
Generalized Vitiligo
Segmental Vitiligo
Universal Vitiligo, only 5-10% of skin pigmentation is remaining
Prognosis: [1-6]
course is unpredictable
slowly progressive in majority of cases
spontaneous re-pigmentation in 10% of cases
Differential diagnosis[1-6]
1. Partial albinism: The lesions are present at birth and remain unchanged
2. Hypopgmentation in the following:
- Pityriasis alba
- Pityriasis versicolor
- Tuberculoid leprosy
- Post inflammatory e.g., steroid induced and burns
Treatment of Vitiligo [1,2,6-9]
Principles:
Restore normal appearance, morphology & function of the skin
Treatment should be individualized
Therapy should continue for 6–12 months for an optimal response
Assurance and psychotherapy throughout the course of treatment
Medical treatment:
1. Topical therapy
1. Sunscreens:
- provide protection from UVA & UVB
- protect skin from sunburn & long-term damage
2. Topical steroids:
- For localized vitiligo
- Mid or low potency steroids are used
- Therapy should be stopped if no response after 3 months
- Side effects: skin atrophy, striae, fixed erythema & telangiactasia
3. Topical calcineurin inhibitors.
- For localized vitiligo
- Can be used for areas where topical steroid can’t be used e.g., sensitive areas
and perioccular
- No skin atrophy, striae, or telangiactasia
4.Topical vitamin D derivatives
2. Systemic therapy
1. Systemic steroids:
- To stop progression of the disease
- Oral dexamethazone mini pulse therapy
2. Methotrexate
Phototherapy
1. Photochemotherapy (Psoralen + UVA radiation); PUVA
Oral: Psoralen (plant extract) + UVA (320 – 400 nm)
Contraindication: pregnancy, hepatitis (psoralen); eye disease and
photosensitive skin diseases and skin malignancies.
Side effects of psoralen: hepatitis, keratitis, photosensitivity, skin aging
Topical PUVA
2. Narrow band UVB phototherapy:
UVB: 280 – 320 nm (broad band UVB)
311 ± 2 nm (narrow band UVB)
- Advantages over PUVA:
Effective in all varieties of vitiligo
Safe for children
Suitable for sensitive and difficult areas
Convenient and affordable
Greater response rate than
Surgical treatment
Stable vitiligo:
No new lesions or Koebner phenomenon over the last year
Type of vitiligo:
Segmental vitiligo
Focal vitiligo
Localized parts in generalized vitiligo
Procedures:
A. Autologous grafting
1. Minigrafting
2. Suction blister grafting
3. Noncultured epidermal suspensions
4.Melanocyte and keratinocytes cultures
B. Micropigmentation (Tattooing)
Never match normal color of skin, Color changes over time
Depigmentation
Indication: universal vitiligo
Bleaching agent: hydroquinone ether
Side effects: contact dermatitis
References:
1)
Jean L. Bolognia, Julie V. Schaffer, Lorenzo Cerroni. Dermatology, [2 volumes]
4th edition China Elsevier; 2017 .
2)
Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D. Rook's
Textbook of Dermatology, [4 volumes] 9th edition, Wiley-Blackwell, 2016.
3)
Bergqvist C, Ezzedine K: Vitiligo: a review. Dermatology. 2020, 236:571-92.
4)
Faria AR, Tarlé RG, Dellatorre G, Mira MT, Castro CC: Vitiligo--part 2classification, histopathology and treatment. An Bras Dermatol. 2014, 89:784-90.
5)
Alikhan A, Felsten LM, Daly M, Petronic-Rosic V: Vitiligo: a comprehensive
overview part I. Introduction, epidemiology, quality of life, diagnosis, differential
diagnosis, associations, histopathology, etiology, and work-up. J Am Acad
Dermatol. 2011, 65:473-91.
6)
.Bergqvist C, Ezzedine K: Vitiligo: a focus on pathogenesis and its therapeutic
implications . J Dermatol. 2021,48:252-70
7)
Lotti T, Agarwal K, Podder I, et al.: Safety of the current drug treatments for
vitiligo . Expert Opin Drug Saf.2020, 19:499-511.
8)
Bleuel R, Eberlein B: Therapeutic management of vitiligo . J Dtsch Dermatol Ges.
2018, 16:1309-13. 26.
9)
Boniface K, Seneschal J, Picardo M, Taïeb A: Vitiligo: focus on clinical aspects,
immunopathogenesis, and therapy. Clin Rev Allergy Immunol. 2018, 54:52-67.
DISORDERS OF HAIR
Hair has no vital function in humans, yet its psychological functions are
extremely important. Hair is present all over the body except the palms, soles,
glans and prepuce.
Types of hair
1- Lanugo hair (prenatal). Fine hair, usually shed in utero.
2- Vellus hair (postnatal). Similar to lanugo, seldom exceeds 2 cm in length.
3- Terminal hair. Long, coarse and pigmented.
Androgen dependent hair
* Pubic and axillary hair in both sexes.
* Facial, trunk and extremities in males only.
The average scalp hair is about 100,000 hair and the average number of hair
shed is 25-100/day. Scalp hair growth is about 0.35 mm/day (1 cm/month).
Hair cycle
The cycle has mosaic pattern. The hair does not grow continuously but each
follicle unsynchronized with the other follicles.
Stages of the hair cycle
1- Anagen (growth stage) duration 2-6 years (3 years), about 85-90% of hairs
2- Catagen (involution stage) duration 1-2 weeks, about 1% of hairs
3- Telogen (resting stage) duration about 3 months, about 10-15% of hairs
Alopecias
Alopecia means loss of hair. It may be cicatricial or non-cicatricial.
1
A- Cicatricial alopecia
It results from destruction of hair follicles by scar tissue formed in the
scalp.
Clinical picture
- Presence of scarring.
- Evidence of the disease or condition which caused scarring may be present.
- Cicatricial alopecia is a permanent condition and regrowth of hairs in the
affected area is not expected.
Causes
A. Congenital. A scarred area in which hair follicles are destroyed
is present at birth due to a developmental defect.
B. Acquired
1. Trauma
- Mechanical.
- Thermal (e.g. burns).
- Physical (e.g. radiodermatitis).
2. Infection
- Pyogenic (abscess).
- Fungal (kerion, favus).
- Bacillary (lupus vulgaris).
- Spirochaetal (gumma).
3. Collagen diseases
- Discoid lupus erythematosus of the scalp.
- Scleroderma (morphea).
2
4. Diseases of unknown etiology
- Pseudopelade.
- Folliculitis decalvans.
B- Non-Cicatricial alopecia
A. Congenital
* Congenital atrichia. Due to failure of development of hair follicles.
* Congenital hypotrichia. The hair follicles are poorly developed.
B. Acquired
1- Circumscribed
* Alopecia areata.
* Infections e.g. tinea capitis, secondary syphilis (moth eaten alopecia).
* Traumatic (trichotillomania).
2- Diffuse
* Telogen effluvium (stress induced).
* Anagen effluvium.
* Androgenetic alopecia.
* Endocrinal (hypopituitarism, hypothyroidism and hyper-thyroidism)
* Drugs (thyroid antagonists, anticoagulants, arsenic, thallium salts).
* Nutritional and metabolic disorders (deficiency of iron, zinc or protein).
* Severe chronic illness (malignancy, liver disease, kidney disease).
Alopecia Areata
It is a common asymptomatic disease characterized by rapid (sudden) onset of
hair loss in a sharply defined area.
3
Etiology
The etiology is unknown, but many factors appear to have a role:
1) Genetic factors. Positive family history in about 20%.
2) Immunological factors. Autoimmune theory is supported by the association with
other autoimmune diseases.
3) Emotional stress. May be a precipitating factor.
Clinical picture
Alopecia areata occurs mostly in patients below 40 years age, and both sexes
are equally affected. It is characterized by rapid and complete loss of hair in one
or more circumscribed, round or oval patches, usually on the scalp (60%),
bearded area, eyebrows, eyelashes, and less commonly, on other hairy areas of the
body. The size of the patch may vary from 1 to 5 cm in diameter. Exclamation
mark hairs "thin proximally and thick distally and can be easily pulled-out" may
be present around the patch indicating progression of the disease.
The course of the disease is unpredictable. There is a tendency to complete
regrowth (4-6 months up to 2 years) but some cases never recover. The term
alopecia totalis is applied to total or almost total loss of scalp hair and alopecia
universalis is the loss of all body hair.
Treatment
Psychological assurance is needed.
1- Topical treatment a- Topical
steroids.
b- Local irritants e.g. dithranol, phenol.
c- Minoxidil 5% "Regaine".
d- Topical immunotherapy e.g. dinitrochlorobenzene (DNCB). e- Topical
cyclosporine.
4
2-Intracutaneous injection of steroids
3- Systemic treatment
a- Systemic steroids, can lead to hair growth but hair may be lost
when the treatment is stopped
b- Systemic cyclosporine.
c- Photochemotherapy (PUVA).
Androgenetic alopecia
(Male-pattern alopecia - Common baldness)
Androgenetic alopecia is a physiological process in a genetically
predisposed individuals.
Etiology
It is unknown. The factors suggested are:
1) Genetic predisposition.
2) Androgen stimulation of susceptible hair follicles.
Clinical picture
The essential clinical feature of androgenetic alopecia in both sexes is the
replacement of terminal hairs by the finer vellus hairs. This process may begin at
any age after puberty. In males, loss of hair, occurs chiefly from the
frontotemporal and vertex regions. In females, diffuse alopecia is the main
presentation with no recession to the anterior hairline as in males.
Treatment
- Topical minoxidil.
- Hair transplantation.
5
Telogen effluvium
Following stress conditions many anagen hair follicles enter prematurely
into telogen with excessive loss of normal hairs.
Causes
- Labour
- Acute blood loss and surgical operations
- High fever
- Emotional stress
- Crash diet (inadequate protein diet).
Clinical picture
Diffuse shedding of hair occurs 1.5 to 4 months after exposure to stressful
event. All the shed hairs are in the telogen phase. Usually no more than 50% of the
hairs are affected. The prognosis is good as complete regrowth of hairs occur in about
6 months.
6
DISORDERS OF SEBACEOUS GLANDS
The sebaceous gland
Sebaceous glands are found in greatest abundance on the face
and scalp, though they are distributed throughout all skin sites
except the palms and soles. Each gland consists of many lobes
(secretory portion) and duct which open into a hair follicle. Sebaceous
glands and hair follicles are referred to as pilosebaceous follicles or
units. They are under androgenic control. Sebaceous glands start
their activity at puberty. The function of sebum is to moisturize the
skin and protect it against fungal and bacterial infections.
Acne Vulgaris
Acne vulgaris is a chronic inflammatory disease of the
pilosebaceous units. It is characterized by the formation of
comedones, papules and pustules, less frequently by nodules and
cysts.
Pathogenesis
Acne vulgaris is exclusively a follicular disease, with comedo
formation produced by the impaction and distension of the follicles
with tightly packed horny cells. Disruption of the follicular epithelium
permits discharge of the follicular contents into the dermis. This, in
turn, causes the formation of inflammatory papules, pustules, nodules
and cysts.
Etiology
Acne vulgaris is a multifactorial disease.
1
Genetic factors. Genetic factors influence not only the
development of lesions but also the course and severity of the
disease. Several members of the same family may be affected.
Androgenic stimulation of sebaceous glands with increased
production of sebum.
Ductal hypercorniflcation. Comedones represent the retention
of hyperproliferating ductal keratinocytes in the duct.
Presence of abnormal microbial flora (Propionibactenum
acnes).
Mediation of inflammation. The dermal inflammation is not
caused by bacteria but it probably results from biologically active
mediators that diffuse from the follicle where they are produced by
Propionibactenum acnes.
Clinical picture
Acne vulgaris is a disease of adolescents and young adults and
usually disappears by the age of 25 years. Both sexes are equally
affected.
It occurs predominantly on the face (99%) and, to lesser
extent, on the back (60%) and chest (15%). On the face it occurs
most frequently on the cheeks, and to a lesser degree on the
forehead, nose and chin. Acne is a polymorphic disease, but one type of
the following lesions may predominate.
Comedones (blackheads). Comedo is the basic lesion in acne.It is a
small punctate black lesion. When a comedo is extracted outside
the follicular canal it appears as a yellowish worm-like structure
2
with an upper black end (the black color is due to melanin not dirt).
Papules. Small red papules. Pustules. Conical pustules.
Nodules and cysts. Nodules, cysts, grouped comedones and
scarring are features of acne conglobata which is a chronic disorder
that may last up to 40-50 years of age. Post-inflammatory lesions. As
erythema, pigmentation and scarring (small atrophic scars or pits, deeper
furrows and keloidal scars).
Factors which may aggravate acne
Menstruation. About 70% of women complain of a flare 2-7 days
premenstrually.
Stress.
It is unlikely that stress alone induces acne lesions.
However, acne itself induces stress, and "picking" of the spots will
aggravate the appearance. This is particularly obvious in young females
who present with acne excoriee.
Sweating. Up to 15% of acne patients notice that sweating causes a
deterioration in their acne.
Treatment
Patients with mild acne usually receive topical therapy; with
moderate acne receive oral and topical therapies; with severe acne
should receive oral isotretinoin. A- Topical
- Topical antibiotics e.g. tetracycline, erythromycin, clindamycin.
- Benzoyl peroxide 5%.
- Retinoic acid (0.025-0.05%).
- Azaleic acid (20%).
B- Systemic
1- Antibiotics. They are the most important systemic line of therapy
and should be administered for long periods (at least 6 months).The
3
mode of action of the antibiotics (the small doses used in acne) is
not to reduce the number of bacteria, but they affect their function.
The antibiotics can also inhibit various enzyme activities,
modulate chemotaxis and lymphocyte function. The
commonly used antibiotics are :
Tetracycline. It is the safest and cheapest and used as 250 to 500
mg one to four times daily (on empty stomach) initially with gradual
reduction of the dose, depending on clinical response.
Minocycline. It is more effective than tetracycline and used in a
dose of 100 mg/day.
Erythromycin. For those who cannot take tetracycline because of
side effects or in pregnant women erythromycin may be considered
in a dose similar to that of tetracycline. Others e.g. clindamycin,
cotrimoxazole.
Antiandrogens. Antiandrogens (cyproterone acetate) are used
only in adult females. It is contraindicated in males and pregnant
females.
Systemic retinoids (isotretinoin). Used only in severe cases.
Dose: 0.5 – 1 mg / kg
The most common side effect is mucosal dryness.
The most serious side effect is teratogenicity.
Systemic steroids. Used only in severe cases.
Treatment of post-acne scars
- Chemical peeling.
- Dermabrasion.
- Laser skin resurfacing.
Other lines of treatment include comedo extraction, intra-lesional
injection of steroids and cryotherapy.
4
References:
Knutsen-Larson S, Dawson AL, Dunnick CA, Dellavalle RP. Acne
vulgaris: pathogenesis, treatment, and needs assessment. Dermatol
Clin. 2012 Jan;30(1):99-106.
Fox L, Csongradi C, Aucamp M, du Plessis J, Gerber M. Treatment
Modalities for Acne Molecules. 2016 Aug 13;21(8):1063.
Berry K, Lim J, Zaenglein AL. Acne Vulgaris: Treatment Made Easy
for the Primary Care Physician. Pediatr Ann. 2020 Mar 1;49(3): e109e115.
5
DISORDERS OF SWEAT GLANDS [1-4]
The sweat glands are of 2 types, eccrine and apocrine [1-4].
1- Eccrine sweat glands: are found at all skin sites. Eccrine glands are most
abundant on plams, soles, forehead, and axillae. Secretion of sweat occurs as a
result of many factors and is mediated by cholinergic innervation. Heat is a prime
stimulus to increased sweating, but other physiologic stimuli, including emotional
stress, are important as well.
2- Apocrine sweat glands: are generally confined to the axillae, areolae, the
anogenital region, the external auditory canal, and the eyelids. The glands do not
begin to function until puberty. Apocrine secretion appears milky and is odourless
untill it reaches the skin surface, where it is altered by bacteria which makes it
odouriferous. It serves no known function in humans. Apocrine gland is mediated
mainly by adrenergic innervation.
Disorders of sweat glands include:
1- Miliaria
2- Hyperhidrosis
3- Anhidrosis
1
Miliaria (Prickly heat, Sweat rash) [1-4]
Defintion
Skin eruption due to retention of sweat as a result of occlusion of eccrine sweat
glands. The blockage leads to backflow of eccrine sweat into the dermis or
epidermis, resulting in a rash comprised of sweat-filled vesicles under the skin.
Clinical picture
• In hot humid climate, more infants and children, in the areas of friction with
clothes and flexures and intense discomfort and pricking sensation.
The lesion depends on the level of obstruction: Miliaria crystallina: 1–2 mm superficial clear vesicles in very large number
(superficial obstruction)
Miliaria rubra: the most common, 2–4 mm erythematous papules or papulovesicles in sites of friction and flexures. Secondary bacterial infection is common:
pustules. level: mid-epidermis
Miliaria profunda: asymptomatic skin-colored deep papules. level: sub-epidermis
Treatment
The most effective treatment for miliaria is to place the patient in a cool environment.
Avoidance of excessive clothing, excessive use of soap and contact of the skin
with irritants.
2
Soothing local applications e.g. calamine lotion.
Oral antihistamines for itching and antibiotics for secondary infection.
Hyperhidrosis [1-3]
Definition
Excessive and uncontrollable sweating (eccrine)
Types
1. Primary hyperhidrosis:
Overactivity of the hypothalamic thermoregulatory center and is transmitted via the
sympathetic nervous system to the eccrine sweat gland. Starts in childhood or
adolescence, persist lifelong. Involves axillae, palms and or soles symmetrically.
Sweating decreases at night and disappears during sleep
Triggers to attacks of sweating may include hot weather, exercise, fever, anxiety and
spicy food.
2. Secondary hyperhidrosis
Secondary localized hyperhidrosis:
The auriculotemporal syndrome (gustatory hyperhidrosis)
Spinal or peripheral nerve damage
Surgical sympathectomy
Neuropathy
Brain tumor
Chronic anxiety disorder
Secondary generalized hyperhidrosis:
Obesity, Diabetes, Menopause, Hyperthyroidism, Parkinson disease, Hodgkin
lymphoma, Phaeochromocytoma.
Drugs: alcohol, caffeine, cholinesterase inhibitors, opioids and antidepressants
3
Treatment:
General measures:
Cotton wear, avoiding caffeinated food and drink, non-soap cleanser, absorbent insoles
Primary hyperhidrosis
1. Topical antiperspirants: aluminium salts
2. Oral anticholinergic drugs
3. Botulinum toxin injections
Secondary hyperhidrosis
Treatment of the cause
References:
1) James WD, Berger T, Elston D, Treat JR, Rosenbach MA. Andrews'
Diseases of the Skin: Clinical Dermatology. Philadelphia, PA: Elsevier
Health Sciences; 2019.
2) Miller JL. Diseases of the eccrine and apocrine sweat glands. In Bolognia JL,
Schaffer J, Cerroni L (eds). Dermatology [2 volumes], 4th edition, Elsevier;
2017.
3) Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D.
Rook's Textbook of Dermatology, [4 volumes] 9th edition, WileyBlackwell, 2016.
4) Miller JL. Miliaria up to date, 2017, https://www. Uptodate.com.
4
Connective tissue diseases
Immune connective tissue disease include
Lupus erythematosus
Systemic sclerosis
Dermatomyositis
Rheumatoid arthritis
The most common types of Lupus erythematosus are:
Discoid lupus erythematosus (DLE)
Systemic lupus erythematosus (SLE)
Discoid lupus erythematosus (DLE) [1-4]
More in young adults, Female to male ratio: 2 : 1
Mainly in sun exposed areas: cheeks, bridge of the nose, ears, side of the neck
and scalp
Well-defined erythematous patches covered with adherent scales extending into
patulous pilosebaceous canals (follicular plugging)
Atrophy, scarring and dyspigmentation
On scalp, cicatricial alopecia
Progression to SLE is uncommon
Spontaneous involution with scarring is common
Treatment
1. Avoiding sun exposure and the use of sunscreen
2. Topical and intralesional injection of corticosteroids
3. Topical calcineurin inhibitors
4. Oral antimalarials
Systemic lupus erythematosus (SLE) [2-5]
Definition:
SLE is an autoimmune disease in which the immune system attacks its own tissues,
causing widespread inflammation and tissue damage in the affected organs. It can affect
the joints, skin, brain, lungs, kidneys, and blood vessels.
Young adults
Female to male ratio: 8 : 1
Constitutional manifestations: fever, fatigue, weight loss, anorexia
Systemic manifestations: arthritis, renal, pulmonary, cardiac and neurological
and ocular affection
Skin involvement occurs in 80% of cases
Cutaneous lesions:
* Facial erythema (butterfly, malar rash), DLE lesions
* Raynaud phenomenon
* Vasculitis: purpura, erythema and telangiectasia of the fingertips, toe tips, palms
and soles, superficial ulcers
* Diffuse nonscarring hair loss (lupus hair)
* Mucous membrane lesions: conjunctivitis, nasal and vaginal ulcerations, oral
hemorrhages and ulcerations
Laboratory findings:
Blood: Anemia, leukopania, thrombocytopania, and raised ESR
Urine: Albuminuria, hematuria and casts
Low levels of serum complement.
Antinuclear antibodies (ANA): is positive in virtually all patients with SLE at
some time in the disease course, entry criterion for diagnosis
Anti-double stranded DNA: highly specific for SLE
Renal biopsy: glomerulonephritis
Treatment: Bed rest in acute cases
non-steroidal anti-inflammatory drugs
Oral antimalarials
Systemic steroids: oral or pulse therapy
Immunosuppressive drugs: cyclophosphamide, azathioprine, methotrexate and
biologic therapy
References:
1) Achtman JC, Werth VP. Pathophysiokogy of cutaneous lupus erythematosus.
Arthritis Rse Ther. 2015;17(1):182.
2) James WD, Berger T, Elston D, Treat JR, Rosenbach MA. Andrews' Diseases of
the Skin: Clinical Dermatology. Philadelphia, PA: Elsevier Health Sciences;
2019.
3) Jean L. Bolognia, Julie V. Schaffer, Lorenzo Cerroni. Dermatology, [2 volumes]
4th edition China Elsevier; 2017.
4) Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D. Rook's
Textbook of Dermatology, [4 volumes] 9th edition, Wiley-Blackwell, 2016.
5) Fava A, Petri M. Systemic lupus erythematosus: Diagnosis and clinical
management. J Autoimmune. 2019;96:1-13.
Bullous skin diseases
Immunobullous diseases [1-3]
Are blistering cutaneous disorders caused by pathogenic antibodies binding
to protein targets within the skin:
In the epidermis (Pemphigus),
In the dermo-epidermal junction (bullous pemphigoid) or
In the dermis (bullous SLE).
1. Pemphigus vulgaris: [1-3]
Loss of keratinocyte adhesion causing acantholysis (separation of
keratinocytes) and intraepidermal blister formation.
Clinical picture:
Oral severe painful ulcers appear before or with skin lesion
Painful flaccid bullae which rupture leaving eroded areas
No itch and no scars after healing
Treatment:
Hospital admission
High dose systemic steroids
Immunosuppressive drugs
1
2. Bullous pemphigoid: [1-3]
Subepidermal blister (dermo-epidermal junction)
Clinical picture:
Itchy urticarial wheals appear before the bullae which are tense,
large and rupture leaving eroded areas
Oral ulcers are absent or very mild
Healing without scars
Treatment:
Highly potent topical steroid
Systemic steroids
Immunosuppressive drugs
Prognosis:
More benign than pemphigus
Dermatologic emergencies
The main functions of normal skin
1. Temperature regulation
2. Physical barrier to foreign materials/trauma
3. Protection from UV radiation
4. Sensation
5. Fluid retention
6. Immune response (Langerhans cells)
7. Vitamin D synthesis
8. Excretion of toxins
2
Acute skin failure [4]
Impairment of skin functions because of damage or loss of large area of the skin
due to different skin diseases. It represents a dermatological emergency and
requires an intensive care approach
Causes:
Erythroderma
Stevens – Johnson syndrome (SJS)
Toxic epidermal necrolysis (TEN)
Immunobullous dermatoses e.g.: pemphigus vulgaris
Infections e.g.: staphylococcal scalded skin syndrome (SSSS)
Erythroderma [1,2,5,6]
Diffuse erythema and scaling involving all or most of the skin surface
area (≥ 90%)
Causes:
* Psoriasis, PRP, atopic dermatitis, SLE, norwegian scabies, seborrheic
dermatitis, immunobullous diseases.
* Drug reaction: sulfonamide, ceftriaxone, vancomycin, antiepileptics
* Malignancies
3
Stevens – Johnson syndrome (SJS) [1,2,6]
Drug induced (mostly): Sulphonamides, antiepileptic drugs, NSAIDS,
penicillins
Infection: mycoplasma pneumonia
Clinical picture:
Fever, malaise, sore throat, myalgia and arthralgia
Painful red macules (target lesions), vesicles, bullae and skin detachment
Severe mucosal inflammation and ulceration: oral, uro-genital and ocular
Treatment: hospitalization, IVIG and immunesupressants
Toxic epidermal necrolysis (TEN) [1,2,6,7]
Drug induced (almost always):
Sulphonamides, antiepileptic drugs, NSAIDS, penicillins, ceftriaxone
Infection (minority): mycoplasma pneumonia
Clinical picture:
Fever, malaise, sore throat, myalgia and arthralgia
4
Painful red macules (target lesions), vesicles, bullae and skin detachment >
30% of body surface area
Severe mucosal ulcers: oral, uro-genital and ocular
Internal organs show inflammatory response
Treatment: hospitalization, IVIG and immunesupressants
Staphylococcal scalded skin syndrome (SSSS) [1,2,8,9]
Rare, severe superficial blistering disease characterized by skin detachment due to
exotoxin of specific strains of staph. aureus.
The skin has the appearance of burn or scalding.
Age: below 5 years.
Clinical picture:
Irritability, fever, lethargy followed by wide spread red rash
developing into large fragile bullae which easily rupture leaving
large tender eroded areas
No mucous membrane affection.
Low mortality
Treatment: hospitalization and IV antibiotics.
5
Why are they dangerous and considered emergencies?
Altered thermoregulation
Fluid and electrolyte imbalance
Loss of nutrients
Altered hemodynamics: hypovolemia or shock
Altered immune function
Infection, Septic shock
Metabolic abnormalities
Organ system inflammation
Management: hospitalization and care of:
6
Angioedema [1,2,10]
Deep swelling of the deeper dermis or subcutaneous tissue, it may affect mucous
membrane (Larynx). Usually affects distensible tissues: eyelids, lips, ear lobules
and genitalia
Why emergency? It interferes with breathing if affects the larynx
Treatment: hospitalization, adrenaline and systemic steroids (if affects larynx
7
References:
1) Jean L. Bolognia, Julie V. Schaffer, Lorenzo Cerroni. Dermatology,
[2 volumes] 4th edition China Elsevier; 2017.
2) Griffiths C, Barker J, Bleiker T, Robert Chalmers R, Daniel Creamer D.
Rook's Textbook of Dermatology, [4 volumes] 9th edition, WileyBlackwell, 2016.
3) Egami S,Yamagami J, Amagai M.Autoimmune bullous skin disease,
pemphigus and pemphigoid. J Allergy Clin Immunol 2020;145:1031-47.
4) Inamadar AC, Palit A. Acute skin failure: Concept, causes, cosequences and
care. Indian J Dermatol Venereol Leprol 2005;71:379-385
5) Okoduwa C,LambertnWC, Schwartz RA, et al. Erythroderma: review of a
potentially life threatening dermatosis.Indian Journal of Dermatology.
2009;54(1):1-6.
6) Mockenhaput M. severe drug induced skin reactions: clinical pattern,
diagnostics and therapy. Journal der Deutschen Dermatoloischen Gesellschaft
2009;7:142-62.
7) Fernando SL. The management of toxic epidermal necrolysis. Aust J of
Dermatol.2012:53:165-71
8) Leung AKC, Barankin B, Leong K. Staphylococcal scalded skin syndrome:
evaluation, diagnosis and management. World J Pediatr. 2018;14(2):116-120.
9) Mishra AK, Yadav P, Mishra A. A Systemic Review on Staphylococcal
Scalded Skin Syndrome (SSSS): A Rare and Critical Disease of Neonates.
Open Microbiol J.2016;10:150.
10)
Depetri F, Tedeschi A, Cugno M.Angioedema and emergency medicine:
from pathophysiology to diagnosis and treatment. Eur J Intern Med.2019;59:813.
8
ALLERGIC SKIN DISEASES
Eczema/Dermatitis
Eczema is an inflammatory skin reaction characterized histologically by
spongiosis and clinically by itching, redness, scaling and papulovesicular eruption.
The terms eczema and dermatitis are generally regarded as synonymous.
Eczema/dermatitis may be presented as acute, subacute or chronic.
acute eczema : erythema, edema, oozing and papulovesicular eruptions
subacute eczema: less erythema, edema and oozing with scaling and
crusting.
chronic eczema, the lesion shows thickening and lichenification.
Varieties of eczema/dermatitis
1. Contact dermatitis.
2. Atopic dermatitis.
3. Seborrhoeic dermatitis.
4. Discoid eczema.
5. Pityriasis alba.
1
Contact dermatitis
There are 2 types of contact dermatitis: irritant and allergic contact dermatitis.
Characteristic
ICD
ACD
feature
Definition
Non spesfic inflammatory
Delayed hypersenistivity reaction to
response to a high concentration
allergens.
of the substance
Pathogenesis
No immune reactions accur.
Induced by immune reaction.
No prior exposure to any
sensitization is required to the allergen and
substance ,no sensitization is
does not occur from the first exposure
required.
Common
Chemical agents ,soaps,
Metals, fragrances , Cosmetics, Insecticides.
causes
detergents.
Chromium (in cement).
physical agents ,heat, cold, x rays, Nickel (in artificial jewelleries).
laser rays.
Rubber in clothes, shoes.
foods, fruit juices .
Location
Mostly hands
On expased areas of the body , hands,
face, lower legs, feet.
Clinical picture
The clinical pictures of irritant and allergic contact dermatitis are more or
less the same. The primary signs in contact dermatitis are erythema, swelling,
papules and papulovesicles. If contact dermatitis persists, it may be due to continued
or repeated exposure to the allergen or irritant. It becomes dry, scaly and
lichenification and fissuring may develop later. The site and morphology of the
lesion may point to the cause.
2
Diagnosis
1- History.
2- Site and morphology of the dermatitis.
3- Patch testing in allergic contact dermatitis.
Treatment
- Detection and avoidance of the cause.
- The use of protective measures e.g. gloves.
- Treatment of the dermatitis.
Atopic dermatitis
Atopic dermatitis is an itchy, chronic, relapsing inflammatory skin condition,
frequently associated with other atopic conditions (asthma, hay fever, atopic
dermatitis) in the individual or other family members.
Clinical Picture
Atopic dermatitis may start at any age. The distribution of the eruption varies
with age, as described below.
3
PHASES OF ATOPIC DERMATITIS
Infantile
Childhood
Adult
Onset usually 2-6
months of age.
Occurs 4-10 years of age.
Begins at or around
12years .
Affects cheeks,
forehead, scalp,
trunk, and
extremities .
involves the extensors,
wrists, ankles, antecubital
and popliteal regions, and
feet .
Face, neck, flexor folds,
upper arms, back, ,hands,
feet, fingers and toes .
itchy ,erythema and
edematous papules.
vesiculation ,
lichenification
lichenification
Treatment
- Reduction of trigger factors as soap and detergents, wool, some foods and
stress.
- Bath oils and application of emollients.
-
Topical corticosteroids.
- Systemic corticosteroid in severe non-responding cases.
Seborrhoeic dermatitis
It is a chronic dermatitis, which has a red sharply marginated
lesions covered with greasy scales and distributed in areas with a
rich supply of sebaceous glands namely the scalp, face and upper
trunk
.
The
yeast
Malassezia
Furfur
may
have
desquamation
from
the
a
role
in
the
etiology of the disease.
Clinical picture
Dandruff
(visible
4
scalp
surface)
appears to be the precursor of seborrhoeic dermatitis, and this may
progress
through
redness,
irritation
and
increasing
scaling
of
the
scalp to seborrhoeic dermatitis.
Seborrhoeic dermatitis commonly originates in hairy skin, and involves the
scalp, face, presternal and intrascapular regions and the flexures. The lesions tend to
be dull or yellowish red in color and covered with greasy scales. The lesions may
be generalized, with erythema, scaling, oozing and pruritus and may progress to
erythroderma.
Treatment
- Dandruff is usually treated by medicated shampoos as ketoconazole
and selenium sulphide shampoos.
- Seborrhoeic dermatitis of the glabrous skin is treated as eczema.
Discoid eczema (Nummular eczema)
Discoid eczema is characterized by circular or oval plaques of eczema
with a clearly demarcated edge.
Clinical picture
The diagnostic lesion of discoid eczema is a coin shaped plaque of closely
set, thin-walled vesicles on an erythematous base.
Itching is usually severe. Middle aged men are most frequently affected.
Discoid eczema usually begins on the lower legs, dorsa of hands, or extensor
surfaces of the arm.
5
Pityriasis alba
Pityriasis alba is a type of non specific dermatitis, of unknown origin. It is
more common in children. It is characterized by erythematous scaly patches
which subside to leave areas of hypopigmentation. The lesions are often
confined to the face .
Treatment of eczema General
measures
- The cause should be removed or avoided- Antihistamines for itching.
- Antibiotics, local and systemic for secondary infection.
- Corticosteroids, local for the majority of cases and systemic for the severe,
generalized or resistant cases.
- Wet dressings e.g. potassium permanganate 1/8000 are used for the acute cases.
- Creams are used for the subacute cases.
- Ointments are used for the chronic cases.
Urticaria
Urticaria is a transient eruption of erythematous or edematous swellings of
the dermis and is usually associated with itching. The urticarial wheal results from
increased capillary permeability, which allows proteins and fluids to extravasate.
Capillary permeability results from increased release of histamine from mast cells.
Classification
Urticaria may be acute with complete resolution within 6 weeks of onset
or chronic lasting more than 6 weeks. It can also be classified into: immunologic,
non-immunologic or idiopathic.
6
Etiologic factors
1) Drugs e.g. penicillin, salicylates, morphine, nonsteroidal anti-inflammatory
drugs and codeine.
2) Foods e.g. seafood, strawberries, chocolate, nut, cheese, eggs and milk. Food
additives as tartrazine may also cause urticaria.
3) Insect bites and stings.
4) Physical agents e.g. heat, cold and physical injury.
5) Inhalants e.g. nasal sprays, pollens and animal danders.
6) Infections e.g. focus of infection in the sinuses, teeth or tonsils.
7) Parasitic infestations e.g. ascaris and ankylostoma.
8) Emotional stress. It is important in cholinergic urticaria.
Clinical picture
Itchy erythematous macules develop into wheals consisting of pale-pink,
edematous, raised skin areas often with a surrounding flare. They occur
anywhere on the body, in variable numbers, sizes and shapes and last a few hours
and resolve within 24 hours. Mucosal swellings occur inside the oral cavity, tongue,
pharynx and larynx. In 50% of cases, there is associated angioedema.
Varieties of Urticaria
- Papular urticaria.
- Physical urticaria e.g. dermographism, cholinergic urticaria, cold urticaria.
- Angioedema (angioneurotic edema) is a type of acute urticaria affects the most
distensible tissues e.g. eyelids, lips, lobes of the ears and external genitals with
circumscribed edema. The swelling affects the deeper parts of the skin or the
subcutaneous tissue with the overlying skin unaltered. It may also affect the
mucous membranes. Affection of the larynx is a life threatening condition.
7
Treatment
- Detection and avoidance of the cause.
- Antihistamines.
- Corticosteroids (systemic) in severe cases.
-
Adrenaline 0.2-0.5 ml of 1:1000 solution given subcutaneously in severe cases
associated with angioedema.
- Topical antipmritic e.g. calamine lotion.
Papular urticaria
Papular urticaria (Fig. 8.12) is a characteristic reaction to insect bites as
mosquitoes or fleas that affects mainly infants and children.
Clinical picture
The lesions develop mainly on the upper and lower extremities particularly
the forearms and legs. Initially, an extremely itchy urticarial wheal develops at the
site of the bite, and this is succeeded by a firm pruritic papule, which may be
surmounted by a tiny vesicle. Itching is an almost constant symptom and
secondary infection is a common complication. The condition usually subsides
spontaneously.
Treatment
- Control of insects.
- Antihistamines.
- Topical antipruritics e.g. calamine lotion.
8
Drug eruptions
Drug eruptions are probably the most frequent of all manifestations of drug
sensitivity. They may arise as a result of immunological allergy directed
against the drug itself, a reactive metabolite or some contaminant of the drug or
more commonly, by non-immunological mechanisms.
Certain drugs are commonly associated with a specific eruption, most drugs are
capable of causing several different types of eruption e.g. ampicillin usually causes a
morbilliform rash, but it can cause, fixed drug eruption, erythema multiforme,
Henoch-Schonlein purpura and serum sickness.
Fixed drug eruption
Fixed drug eruptions characteristically recur in the same site
or sites each time the drug is administered. The drugs commonly
cause this eruption are: sulphonamides, tetracyclines, phenol-phthalein
(laxative), non-steroidal anti-inflammatory drugs, barbiturates and
tranquillizers.
Clinical picture
The lesion usually presents as sharply marginated, round or
oval itchy plaques of erythema and edema becoming dusky violaceus
or brown, and sometimes vesicular or bullous (Fig. 8.16). Lesions are
commoner on the limbs, but about half the cases occur on the oral
and genital mucosa. Characteristically prolonged post-inflammatory
hyperpigmentation results.
9
Treatment
- The suspected drug must be stopped.
- Oral antihistamines.
- Systemic corticosteroids in severe cases.
- Topical antipruritics and steroids.
10
Refrences:
1.Torres T, Ferreira EO, Gonçalo M, Mendes-Bastos P, Selores M,Filipe P. Update on
Atopic Dermatitis. Acta Med Port. 2019 Sep 2;32(9):606-613
2.Scheinman PL, Vocanson M, Thyssen JP, Johansen JD, Nixon RL, Dear K, Botto
NC, Morot J, Goldminz AM. Contact dermatitis. Nat Rev Dis Primers. 2021 May
27;7(1):38. 3.Radonjic-Hoesli S, Hofmeier KS, Micaletto S, Schmid-Grendelmeier
P, Bircher A, Simon D. Urticaria and Angioedema: an Update on Classification
and Pathogenesis. Clin Rev Allergy Immunol. 2018 Feb;54(1):88-101.
11
Acute Eczema
Subacute Eczema
Chronic Eczema
Allergic contact
dermatitis
Allergic contact
dermatitis
Contact dermatitis
Atopic dermatitis
(infantile phase)
Atopic dermatitis
(Childhood phase)
Atopic dermatitis
(Adult phase)
Seborric dermatitis
Cradle cap
Discoid eczma
Pityriasis alba
Urticaria
Papular Urticaria
Angiodema
Fixed drug eruption
ACQUIRED IMMUNODEFICIENCY SYNDROME
(AIDS)
AIDS is an alarming highly fatal disease characterized by severe and
apparently irreversible acquired defects in the cell -mediated immunity that
predispose the host to severe opportunistic infections frequently pneumocystis
carinii pneumonia and / or unusual neoplasms particularly disseminated Kaposi
sarcoma.[1]
Etiology: [1-3]
Human immunodeficiency virus (HIV) is the cause of AIDS. It is one of the
group of retro viruses.
Its single stranded (ss) RNA virus that has reverse transcriptase (RT) enzyme
in its structure.
After its attachment to target cell the ss RNA inters in to the cytoplasm and by
RT enzyme its transformed into double stranded DNA that incorporates into cellular
DNA and becomes an acquired genetic infection
Pathogenesis: [1-3]
The clinical manifestations of HIV infection, with its progressive acquired
immunodeficiency, depend upon loss of the functional integrity of the T helper
cell (CD4). HIV preferentially infects, resides in, and lyses T helper cells. This
leads to the inability to adequately fight infection. Due to the progressive immunodeficiency, microbes, many of which are already present in the host, can then
proliferate unchecked to cause opportunistic infections and transformed cells can
multiply to cause tumours.
Transmission: [1-3]
1
HIV survives poorly outside the human body and has been isolated from
blood, bone marrow, spinal fluid and brain tissue, lymph nodes, semen, saliva,
tears and breast milk. It is transmitted mainly via blood and semen, thus the main
routes of infection are:
1) Sexual.
2) Administration of blood or blood products .
3) Injection with blood - contaminated equipment.
4) Maternofetal.
Groups at high risk of HIV infection
1- Male homosexuals.
2- Intravenous drug users.
3- Hemophiliacs and recipients of blood products.
4- Recipients of blood transfusion.
5- Heterosexual contacts of HIV antibody-positive individuals.
6- Children of HIV antibody - positive mothers.
. The predominant pattern of spread varies from country to country and
depends on social behavior. In USA, Western Europe and Australia most spread
to date has been in homosexual and bisexual men and intravenous drug abusers
with a male to female ratio of AIDS cases of 10:1 and infection in infants is
rare. In contrast, in Africa, and Asia spread is mainly heterosexual, equal
numbers of men and women are infected and HIV in infants is common.
Clinical manifestations: [4-5]
1- Acute infection
It is the earliest clinical manifestation of HIV infection and is usually
asymptomatic but in up to 50% of people can cause a glandular fever like illness
2
with fever, chills, myalgia and arthralgia.
2- Asymptomatic infection
This latent period may last from few months to many years.
3- Persistent generalized lymphadenopathy
This is defined as lymph node enlargement in 2 or more extra-inguinal sites for at
least 3 months. The nodes are symmetrical, mobile, rubbery, non tender and at
least 1 cm in diameter.
4- Symptomatic disease
*
Early symptomatic HIV disease (AIDS-Related Complex "ARC")
This includes, fever, unexplained weight loss, recurrent diarrhea, extreme
fatigue, headache and night sweats. Laboratory abnormalities in the form of
anemia, leukopenia, thrombocytopenia, low number of helper T cells and elevated
serum immunoglobulins level may be found.
*
Late symptomatic HIV disease
Progressive impairment of immune function will lead to the full acquired
immunodeficiency syndrome (AIDS). A person with HIV is considered to have
progressed to AIDS when:
1) CD4 count fall below 200cell/ mm3 { normal count 500-1600 cell/mm3}
2) Develop one or more opportunistic infection regardless CD4 count
Indicator diseases
1-Opporturiistic infections
a) Bacterial e.g. atypical mycobacteriosis, extrapulmonary tuberculosis or recurrent
salmonella septicemia
b) Fungal e.g. Candida esophagitis or disseminated infection, cryptococcal
meningitis
or
disseminated
infection,
3
disseminated
histoplasmosis or
coccidioidomycosis.
c) Viral e.g. cytomegalovirus infection (pulmonary,GIT or CNS), mucocutaneous
herpes simplex infection (duration more than one month), or disseminated
infection.
d) Parasitic e.g. pneumocystis carinii pneumonia, intestinal cryptosporidosis with
diarrhea (duration more than one month), strongyloidiasis causing pneumonia,
CNS or disseminated infection, toxoplasmosis causing CNS or disseminated
infection.
2- HIV encephalopathy (HIV dementia)
3- Cancers
a) Kaposi sarcoma.
b) Lymphoma of brain.
c) Non-Hodgkin lymphoma of B-cell or unknown immunologic phenotype.
4- HIV wasting syndrome (Slim disease)
Estimates of the average time between acquisition of HIV and onset of AIDS
are around 10 to 12 years. The proportion of HIV-infected patients who
eventually develop AIDS is not yet known. Patients with AIDS usually die from
opportunistic infection, CNS disease or wasting, less commonly from malignancy.
Testing for HIV [4-5]
1- HIV- specific antibody screening by ELISA or Western blot.
2- Serum HIV antigen detection.
3- PCR (polymerase chain reaction).
Treatment:[6-7]
No specific treatment. Treatment aims to decrease viral load and so delay
CD4 damage and development of AIDS.
The drugs used for ttt of HIV infection are named antiretroviral therapy
4
(ART) , They include:
1) Reverse transcriptase inhibitor agents ( Zidovudine)
2) Protease inhibitor agents
3) Entery inhibitor agents
4) Integrase inhibitor agents.
Highly active antiretroviral therapy (HAART) :
Consists of three drug therapy that is composed of 2 nucleoside reverse transcriptase
inhibitors and one protease agent
Prevention: [6-7]
No satisfactory vaccine against HIV has yet been developed. Prevention of
transmission of HIV is therefore of paramount importance. The recommended
precautions are :
- Avoidance of sexual contact with known or suspected AIDS patients.
-
Firm screening of blood or blood products for HIV, and avoidance of blood
donation by any member at risk group.
-
Intravenous drug abusers should be regularly screened for HIV, and should
avoid the group needle sharing.
-
Concerning health-care workers, it is generally recommended that procedures
should be carried out as if each patient is a potential HIV carrier.
5
References:
1. Fauci AS.25 years of HIV. Nature. 2008;453: 289-90
2. Cunningham AL, Li S, Juarez J, et al. The level of HIV infection of
macrophages is determined by interaction of viral and host cell
genotypes. J Leukoc Biol. 2000; 68:311-7
3. Moir S, Chun TW, Fauci AS.Pathogenic mechanisms of HIV disease.
Annu Rev Pathol. 2011; 6:223-48
4. El-Atrouni W, Berbari E, Temesgen Z.HIV-associated opportunistic
infections. Bacterial infections. J Med Liban. 2006; 54:80-3
5. Robb ML, Eller LA, Kibuuka H, et al. Prospective Study of Acute
HIV-1 Infection in Adults in East Africa and Thailand. N Engl J Med
2016; 374:2120.
6. Havlir, D. V. & Richman, D. D. Viral dynamics of HIV: implications
for drug development and therapeutic strategies. Ann. Intern. Med.
124, 984–994 (1996).
7. Carpenter, C. C. J. et al. Antiretroviral therapy in adults: updated
recommendations of the International AIDS Society-USA panel. J.
Am. Med. Assoc. 283, 381–390 (2000).
6
GONORRHOEA
Gonorrhoea
is
a
sexually
transmitted
disease
caused
by
Neisseria gonorrhoea and urethral discharge is the main symptom.Neisseria
gonorrhoea
attacks
mucous
membranes
and
has
a
predilection for columnar epithelium which is found in the urethra,
accessory ducts and glands, the cervix, rectum and conjunct!vae. The
childhood vulva and vagina may be attacked. .
Incubation period. It is about 2-5 days (ranges from 2 days to 2 weeks).
Modes of transmission
A- Sexual modes (common)
1) Heterosexual. The primary site of infection is the urethra.
2) Homosexual. The primary site of infection is the rectum.
3) Orogenital. The primary site of infection is the pharynx.
B-Non-sexual modes (uncommon)
1) Neonatal infection that causes ophthalmia neonatorum in the infant due to
infection from his mother during delivery.
2) Childhood infection that causes vulvovaginitis in the female children due to
contaminated towels and lavatory seats.
Gonorrhoea in the male
Clinical picture
Urethritis is the most common manifestation.
* Urethral discharge which is often profuse, purulent and yellow in color.
* Micturition symptoms include dysuria, urgency and frequency.
1
* Examination may show red, swollen external urinary meatus and the superficial
inguinal lymph nodes may be slightly enlarged and tender.
* About 5-15% of patients, may have no symptoms or signs of the disease.
Local complications
1- Tysonitis. It develops with the appearance of red, tender swellings on one or
both sides of the frenulum.
2- Littritis. Those inflamed glands can be felt as multiple tender swellings along
the roof and sides of the urethra.
3- Cowperitis. Infection of the glands usually results in abscess formation.
Fever, malaise and severe pain in the perineum are accompanied with
frequency, urgency and very painful defecation. Rectal examination is very
painful.
4-
Periurethral abscess. With the advent of modern treatment, it is a rare
complication.
5- Prostatitis.
6- Seminal vesiculitis. The symptoms are similar to that of prostatitis in addition
to hemospermia. They are felt during per rectum (P.R.) examination (normally
can not be felt) as tender swellings above the prostate.
7- Epididymitis. The condition is generally unilateral and presents with an acute
onset of pain and swelling in the scrotum. The epididymis is tender and
swollen and there may be testicular involvement leading to epididymoorchitis. If the disease is bilateral it may result in infertility.
8- Urethral stricture. It develops over a period of years as a result of healing of
subepithelial inflammation or periurethral abscess, with subsequent scar
formation. Symptoms are due to urinary obstruction leading to straining,
poor stream and attacks of urinary tract infections.
2
Strictures may occur anywhere in the urethra although they are found most
commonly in the bulbous urethra. They may be diagnosed by anterior urethroscopy
or by a urethrogram.
Gonorrhoea in the female
* Gonorrhoea in the female is asymptomatic in up to 50% of the patients.
* Micturition symptoms include, burning micturition and frequency and urgency if
the trigon of the bladder is involved.
* Genital discharge.
* Examination shows inflammation and mucopurulent discharge from the
urethral meatus and cervix. The inguinal lymph glands may be enlarged and
tender.
Local complications
1- Periurethral abscess and urethral fistula.
2- Skenitis. It may manifest by dysuria and drops of pus on milking
the urethra and swelling on either side of the urethra.
3- Bartholinitis and abscess formation. Barthohnitis may be
detected only by the finding of pus on compression of the ducts.
If an abscess develops, local pain and swelling of the lower onethird of the vulva develop rapidly, which may prevent sitting or
walking.
4- Chronic cervicitis.
5- Salpingitis.
6- Pelvic inflammatory disease (endometritis, tubo-ovarian
abscess and peritonitis).
7- Infertility. If tubal obstruction occurs bilaterally.
3
Gonococcal ophthalmia
Most cases develop within 6 days of birth. The eyes rapidly become
inflamed, with swollen, often edematous lids oozing pus. If the condition is
severe, it may lead to blindness. It occurs due to infection from his mother during
delivery.
Oropharyngeal gonorrhoea
Symptoms are uncommon although sore throat may be complained of.
Examination may show mild tonsillitis or pharyngitis. Oropharyngeal infection
always results from the practice of oro-genital sex.
Anorectal gonorrhoea
In most patients, symptoms are absent. Itching, soreness and some discharge may
occur. Anorectal gonorrhoea occurs in men as a result of anal intercourse among
homosexuals or from the genital discharge.
Gonorrhoea in children
It is relatively uncommon and is more common in girls than boys. Where
urethral gonococcal disease is present in boys it is always the result of sexual
activity, whereas vulvovaginal infection in girls can result from contact of infected
towels or lavatory seats, or due to child abuse.
4
Systemic complications of gonorrhoea
(Disseminated gonorrhoea)
Once common in the preantibiotic era, this complication is now thought to be
very rare. The manifestations may be:
- Fever and other constitutional symptoms.
- Iridocyclitis.
- Arthritis.
- Perihepatitis.
- Dermatitis in the form of red papules, vesiculopustules with a purplish hemorrhagic
centre in some cases.
- Septicemia. This occurs mainly in immunosuppressed patients, and may be
manifested with hepatitis, osteomyelitis, carditis and meningitis.
Laboratory diagnosis of gonorrhoea
1- Gram stain. A smear is positive when gram-negative, kidney shaped diplococci
are identified both inside and outside the polymorphonuclear leukocytes.
2- Culture. It is not indicated in all cases but usually in:
- Female cases.
- Asymptomatic male cases.
- Extragenital and disseminated gonococcal infections.
3-Serologic diagnosis. Serologic tests as complement fixation, immunofluorescence
and hemagglutination are rarely used for the diagnosis.
5
Treatment of gonorrhoea
A- General measures
- Simultaneous treatment and follow-up of the partner.
- The patient should avoid sexual activity during the treatment.
- The patient should avoid self-examination and milking of the urethra.
B- Antibiotic treatment
1- Single dose of one of the followings:
- Ceftriaxone 125 mglM.
- Cefixime 400 mg orally.
- Ciprofloxacin 500 mg orally.
- Ofloxacin 400 mg orally.
- Spectinomycin 2 gm IM.
2- In infections proved not to have penicillin-resistant gonococci, a penicillin can be
used as amoxycillin 3 gm orally + 1 gm probenicid (to delay the excretion of
amoxycillin).
3- It is better to add a drug effective against possible coinfection with chlamydia
trachomatis, such as doxycycline 100 mg orally twice daily for 7 days.
6
SYPHILIS
Syphilis is a chronic systemic infectious disease usually acquired by sexual
contact and caused by the spirochaete, Treponema pallidum (T.P).
Classification
A. Acquired syphilis:
1- Early: occurs within 2 years of infection. Lesions of early syphilis are
infectious. Early acquired syphilis includes:
- Primary stage (chancre).
- Secondary stage.
- Early latent stage.
2- Late: occurs after 2 years of infection. Lesions of late syphilis are noninfectious. Late acquired syphilis includes:
- Late latent stage.
- Tertiary stage.
- Cardiovascular syphilis.
-Neurosyphilis.
B. Congenital syphilis:
1- Early: occurs within 2 years of infection and lesions are infectious.
2- Late: occurs after 2 years of infection and lesions are non-infectious.
3- Stigmata: these include scars and deformities of congenital syphilis.
Diagnostic tests
1- Dark ground test. The organism is demonstrated microscopically by
examination of the exudates from the wet infectious lesions (chancre,
condylomata lata, mucous patches) or from fluid aspirated from the lymph nodes
when the lesion is inaccessible (intraurethral).
2- Serological tests. These include 2 types of tests:
a) Standard tests for syphilis (STS). STS are non-specific, so false positive
reactions may occur. These tests include: Wasserman Reaction (WR), Venereal
Disease Research Laboratory test - (VDRL) and Rapid Plasma Reagin test (RPR).
b) Specific tests for syphilis. These include: Treponema Pallidum
Immobilization test (TPI), Fluorescent Treponemal Antibody test (FTA) and
Treponema Pallidum Hemagglutination test (TPHA). Specific tests are used mainly
to confirm the diagnosis and to exclude false positive reactions.
3- CSF examination. It is performed when neurosyphilis is suspected.
4- Biopsy. It is done to differentiate gumma from malignant tumours.
A. Acquired Syphilis
Natural history
After the incubation period (9-90 days), a chancre (primary stage) appears at the
site of entry of T.P. which heals spontaneously in 6-8 weeks followed by secondary
stage. If untreated the physical signs disappear but serological tests remain positive
(latent syphilis).
Primary syphilis
Chancre is the characteristic lesion. It starts as a small papule that ulcerates and
the regional lymph nodes become enlarged within one week after the appearance of
the chancre.
Characters of the chancre
1- It is usually single (except if present on two opposing surfaces).
2- It is painless (except if secondary infected).
3- The edges are regular and well-defined.
4- The base is indurated " due to cellular infiltration ".
5- The floor is formed of dull red clean looking granulation tissue which may be
covered with a scab. It oozes serum on manipulation.
6- The regional lymph nodes are enlarged, painless, firm and usually bilateral.
7- Site:
- Genital (95%): penis, scrotum, urethra and pubic area in males and Labia
majora or minora, clitoris and cervix in females.
- Extragenital (5%): lips, tongue, nipple and anus.
Diagnosis
- Clinical features.
-
Dark ground test, is the only sure method for diagnosis of early chancre
when the serological tests are still negative.
- STS are negative during the early period and positive in 50% of cases 2
weeks after the appearance of the chancre.
Differential diagnosis
1) Chancroid (soft sore). It is caused by Haemophilus Ducreyi and the
incubation period is short (2-5 days). It is characterized by multiple, soft, painful
ulcers with tendency to bleed easily. Inguinal lymph nodes are enlarged, tender,
matted and may suppurate. Treatment is by sulphonamides.
2) Lymphogranuloma venereum. It is caused by Chlamydm Trachomatis. The
primary lesion is transient and rapidly disappears. The lymph nodes are enlarged,
tender, matted, and may suppurate forming multiple sinuses and fistulae.
3) Genital herpes. It is presented as recurrent, shallow, painful ulcers and the
regional lymph nodes may be enlarged and tender.
4) Other ulcerative lesions of the skin as traumatic ulcer, pyogenic
ulcer, Behcet's disease and malignant ulcer.
Secondary syphilis
Manifestations
1- Skin rash. Characterized by being asymptomatic, generalized, bilateral and
symmetrical, polymorphic and never vesiculate.
2- Mucous patches. Affect lips, tongue, pharynx, urethra or vagina and are
highly infectious.
3- Condylomata lata. Presented as hypertrophic papules in moist areas as the
groin and perianal area. The lesions are sessile with flat moist surface that do not
bleed easily due to endarteritis obliterans. The lesions should be differentiated from
condylomata acuminata (anogenital warts) that show pedunculated lesions with
rough surface which bleed easily.
4- Generalized lymphadenopathy. Involve the cervical, axillary, inguinal and
epitrochlear lymph nodes. The lymph nodes are enlarged, firm, rubbery, discrete and
not tender.
5- Less common manifestations. Fever, headache, patchy alopecia (moth eaten
alopecia), iritis, localized periostitis, hepatitis, nephritis, epididymitis and meningism.
Diagnosis
- Clinical picture.
-
Dark ground test. Positive in mucous membrane lesions and condylomata
lata.
- Serological tests. Positive in 100% of cases.
Latent syphilis
If the secondary stage is not treated, the surface lesions disappear and the
patient enters into a latent period. Latent syphilis is divided into:
- Early latent. This is diagnosed in the first 2 years of infection.
- Late latent. This is diagnosed after 2 years of infection.
Diagnosis
- The patient is clinically free.
- Serological tests are positive.
- CSF is normal.
Fate of latent syphilis
- 30% end by spontaneous cure.
- 30% remain latent.
- 40% evolve into benign tertiary (gumma), cardiovascular, or
neurosyphilis.
Benign tertiary syphilis
The characteristic lesion is the gumma, which is now very rare. The majority of
the lesions occur in the skin and the bones, with a lesser frequency in the mucosae,
viscera, muscles and eyes. The gumma starts as a slowly progressive, painless
nodule or plaque which is dull red and breaks down into indolent punched-out
ulcer.The floor has a " wash leather " appearance (dirty slough). The regional
lymph nodes are not enlarged. Gumma is not infectious.
Diagnosis
- Dark ground test is negative.
-
Serological tests. STS are positive in 70-90% of cases while specific tests are
positive in 100% of cases.
Cardiovascular syphilis
1- Syphilis of the heart. It may occur as localized affection (gumma) or diffuse
affection of the myocardium that leads to heart failure.
2- Syphilis of the aorta. This may be in the form of aortic regurge, aneurysm or
coronary osteal stenosis.
Neurosyphilis
Neurosyphilis may be presented as, asymptomatic neuro-syphilis, syphilitic
meningitis, meningovascular syphilis, general paresis of the insane (brain) and tabes
dorsalis (spinal cord).
B. Congenital Syphilis (Prenatal syphilis)
Congenital syphilis occurs when Treponema pallidum is transmitted
from the mother to the fetus via the placenta. The outcome of pregnancy of a syphilitic
mother:
1- Abortion after the 4 months.
2- Stillbirth.
3- The child may be born with signs of syphilis.
4- The child may be born well but develops signs of early congenital syphilis (in
the first 2 years) or late congenital syphilis (after 2 years).
5- The child may escape infection.
Early congenital syphilis
It appears in the first 2 years of life and the clinical features are similar to
those of secondary syphilis. The main features are:
* Senile facies and marasmus.
* Skin rash; macular, papular and bullous.
* Mucous membrane lesions as syphilitic rhinitis.
* Condylomata lata.
* Others. Osteochondritis, iritis, meningitis, liver fibrosis.
Late congenital syphilis
It appears after the first 2 years of life and the manifestations are
similar to those of tertiary syphilis in addition to other characteristic
features as:
* Frontal bossing.
* Rhagades. Radiating scars around the mouth.
* Hutchinson's triad:
1- Hutchinson's teeth. Commonly affect permanent central incisors and
the cutting edge is narrower than the gum edge. The margins are
rounded and notched.
2- Interstitial keratitis.
3- Eighth nerve deafness.
* Others. Periostitis, synovitis.......etc.
Stigmata
Scars and deformities of congenital syphilis are many e.g. frontal
bossing, rhagades and Ksnchinson's teeth.
Diagnosis
- Dark ground test from condylomata lata or mucous membrane lesions.
- Serological tests.
Treatment of Syphilis
Penicillin is the drug of choice and used as procaine or benzathine penicillin
(long acting). Because of the inability of benzathine penicillin to pass the blood brain
barrier, procaine penicillin is now preferred as it can pass this barrier and protect
against CNS invasion.
I-Treatment of acquired syphilis A- Treatment of early syphilis
- Procaine penicillin 600,000 units I.M. daily for 10 days (6 million units), or
- Benzathine penicillin in a single I.M. injection of 2.4 million units.
B-Treatment of late syphilis
- Procaine penicillin 600,000 units I.M. daily for 20 days (12 million units), or
-
Benzathine penicillin 2.4 million unit I.M. every week for 5 weeks (12 million
units).
Patients allergic to penicillin
-
Tetracycline 500 mg 4 times daily (on empty stomach) for 15 days in early and 30
days in late syphilis, or
-
Erythromycin 500 mg 4 times daily (on empty stomach) for 15 days in early and 30
days in late syphilis.
II-Treatment of congenital syphilis
-
Early congenital syphilis. Procaine penicillin 50,000 units/Kg body weight I.M.
daily for 10 days.
- Late congenital syphilis. As late acquired syphilis.
Reactions to treatment
1- Reactions to penicillin. As anaphylactic reaction or urticaria
2- Herxheimer reaction (therapeutic shock). This reaction follows the first dose of
antisyphilitic treatment. It may be an immunological reaction to the products of killed
treponemes. Clinically; fever, headache and malaise in addition to intensification of the
lesions. In late syphilis, dangerous manifestations may occur such as, rupture of aortic
aneurysm or severe pain in tabes dorsalis. Treatment: systemic corticosteroids.
3- Therapeutic paradox. It is due to healing of syphilitic lesions by fibrosis and the
condition becomes more worse e.g. healing of syphilitic aortitis by fibrosis may lead to
coronary osteal stenosis.
Male Sexual Dysfunctions
Professor Ramadan Saleh, MD
Department of Dermatology, Venereology & Andrology
Faculty of Medicine, Sohag University, Egypt
Puberty Disorders1,2
Definition
Puberty is an interval characterized by the acquisition of the secondary sexual
characteristics, accelerated linear growth, increase in the secretion of sex hormones,
maturation of gonads (testes in boys; ovaries in girls), and the potential for reproduction.
Mechanism of normal puberty
Normal puberty is initiated by pulsatile secretion of gonadotropin releasing hormone
(GnRH) from the hypothalamus. These pulses in turn enhance the release of luteinizing
hormone (LH) and follicle stimulating hormone (FSH) from the pituitary gland. The
pituitary LH stimulates sex hormone production by the gonads.
Puberty onset and development in boys
The international mean age of pubertal onset is 11.6 years. In an Egyptian study, boys
were found to start their puberty at the age of 10 to 13 years (mean age of 11.1 years)1.
Pubertal onset tends to be earlier among Egyptian boys living in urban areas with better
socio-demographic and environmental conditions. Puberty is typically complete in boys
within 2 to 5 years of the onset.
Currently, clinicians rely on Marshall and Tanner's classification of the pubertal onset
and changes in boys2. The signs of puberty in boys are classified into five stages (G1 to
G5) according to:
1. changes in the body height,
2. testicular size,
3. penile length,
4. pubic hair and
5. other physical characters.
Delayed puberty in boys
Delayed puberty is defined as the lack of any pubertal signs by the age of 14 years in boys.
There are two types of delayed puberty in boys:
1. Functional:
a. constitutional delay.
b. chronic disease.
c. malnutrition.
2. Organic:
a. lack of serum gonadotrophin production or action (hypogonadotrophic
hypogonadism).
b. gonadal insufficiency with elevated gonadotrophins (hypergonadotrophic
hypogonadism).
1
Risk factors of delayed puberty in boys
•
family history of delayed puberty.
•
congenital pituitary structural abnormalities.
•
gene mutations.
•
chromosomal disorders.
Diagnostic factors of delayed puberty in boys
•
presence of risk factors.
•
size of testes <3 mL.
•
absent pubic/axillary hair.
•
short stature.
•
dysmorphic features.
Investigations of delayed puberty in boys
•
non-dominant wrist x-ray.
•
basal FSH and LH.
1.
LH-releasing hormone stimulation test.
2.
human chorionic gonadotrophin stimulation test.
3.
Magnetic resonance imaging (MRI) of the brain.
Karyotype.
Treatment of delayed puberty in boys
4.
1. Constitutional cases: are typically observed. A short course of sex steroids may be
needed to induce puberty in some cases.
2. Organic cases: sex-steroid therapy is required to induce puberty and then lifelong
hormone replacement therapy.
2
Erectile Dysfunction3,4
Anatomy of the penis:
The body of the penis consists of 3 corporal bodies: two corpora cavernosa dorsally and a
single corpus spongiosum ventrally which contains the urethra and expands distally to form
the glans penis. The corpora are composed of erectile tissue in the form of sinusoidal
spaces with smooth muscle walls. Each corpus is surrounded by a thick fibrous sheath called tunica
albuginea.
Arterial supply: Penile artery from the internal pudendal artery.
Venous drainage: The sinusoidal spaces of erectile tissue are drained by small venules which
form the subtunical plexus of veins that drain into the deep dorsal vein, and then to the internal
pudendal vein.
Nerve supply:
• Parasympathetic (S2,3,4): mainly responsible for erection.
• Sympathetic (T12 - L3): mainly responsible for ejaculation.
Physiology of erection
Penile erection is a complex physiological process that requires the integrity of anatomical,
neuromuscular, and vascular components of the penis, as well the individual’s endocrinal
and psychological aspects. There are two phases of penile erection:
I.
Tumescence:
•
•
II.
•
•
Following sexual stimulation, the endothelial cells (lining the sinusoidal
cavities in thecorpora) release nitric oxide which activates guanylate
cyclase that converts GTP into cGMP which causes smooth muscle
relaxation.
Relaxed smooth muscle cells allow the sinusoids to fill with blood resulting in
tumescence (i.e. increased length and circumference of the penis).
Rigidity:
Engorged sinusoids result in compression and collapse of sub-tunical
venules and occlusion of the venous outflow to maintain erection.
Contraction of pelvic floor muscles.
Erectile dysfunction
Erectile dysfunction (ED) is defined as the persistent inability to obtain and/or
maintain an erection sufficient for satisfactory sexual intercourse. Erectile
dysfunction is a common medical problem that may have profound psycho-social
consequences.
Prevalence of ED: Approximately 23% of men aged 40-80 years worldwide
have symptoms of ED. Generally, the prevalence of ED in men is positively
correlated with the age.
Causes of ED:
1. Psychogenic factors:
• Anxiety of performance (fear of failure): a common example is honeymoon ED.
• Depression.
3
•
Interpersonal conflicts (marital disharmony).
Organic factors:
Endocrinal causes:
•
Diabetes mellitus (DM): ED occurs in up to 70% of men with DM.
•
Hyperprolactinemia.
•
Hypogonadism.
Vascular causes:
▪
Arterial insufficiency: atherosclerosis.
▪
Venous leakage: such as congenital venous abnormalities that may result in
primary ED.
Neurogenic causes:
▪
Spinal cord injury.
▪
CNS diseases.
Iatrogenic causes:
•
•
Drugs: antidepressants, antihypertensive drugs and antiandrogens.
Surgery: pelvic surgery.
Local causes:
• Peyronie’s disease.
• Fracture penis.
Others: such as smoking, recreational drugs, chronic medical diseases.
Diagnosis of ED:
The diagnosis of ED requires the employment of detailed medical history, sexual history,
general and genital examination, and investigations.
1.
Medical history:
▪ Age: Organic ED is more common at older age groups.
▪ Special habits: smoking, alcohols and drugs.
▪ Chronic medical illness or drug intake.
2. Sexual history:
▪ Onset, course and duration: sudden, intermittent and short duration in
psychogenic ED.
• Morning erection and nocturnal penile tumescence (NPT): positive in psychogenic ED.
• Other sexual functions: desire, ejaculation and orgasm.
• Relationship with wife: to exclude female factor of ED.
3. Clinical examination
• General examination: male secondary sex characters (hair distribution & fat
distribution).
• Genital examination: exclude penile abnormalities such as Peyronie’s disease.
4.
Investigations
I.
Laboratory investigations:
Such as random blood sugar, lipid profile, serum prolactin & Total testosterone.
II.
Intracorporal injection (ICI) test:
• Principle: to test the response of penile tissue to vasoactive substances.
4
•
•
Vasoactive substances: such as prostaglandin E1, papaverine Hcl and phentolamine.
Normal response: Rigid erection (E5) within 10 min and persists for 30-60 min.
Nocturnal penile tumescence (NPT) monitoring:
a. To differentiate between psychogenic and organic ED.
b. Device: Rigiscan.
Penile color Doppler ultrasonography: to exclude arterial insufficiency.
Cavernosometry and cavernosograghy: to exclude venous leakage.
III.
IV.
V.
5. Treatment:
• Treatment of the underlying systemic cause
Such as DM or hypertension.
• Sex therapy:
• Principles: reduce anxiety, increase desire and improve sexual
performance.
• Indication: psychogenic ED.
•
Medical treatment:
I. Selective phosphodiesterase 5 (PDE5) inhibitors:
The selective PDE5 inhibitors play an important role in the treatment of
themajority of patients with ED.
- Mechanism of action: act by selective inhibition of PDE5, which is cGMPspecific and responsible for the degradation of cGMP in the corpus
cavernosum.
- Types:
o Sildenafil citrate (25-100 mg),
o Tadalafil (5-20 mg),
o Vardenafil (10-20 mg)
o Avanafil (50-200 mg).
- Contraindication: Patients on nitrate therapy.
II. Non-selective phosphodiesterase inhibitors: such as pentoxifylline
III. Transdermal therapy: such as nitroglycerine, or Papaverine gel.
IV. Intraurethral therapy: such as PGE1 pellets.
V. Intracorporal injection (ICI) of vasoactive substance: such as papverine,
phentolamine & PGE1.
VI. Vacuum constriction device (VCD): They produce penile engorgement by
applying vacuum device to a tube placed over the penis, then a rubber
constriction ring is placed around the base of the penis to maintain engorgement.
• Surgical treatment: Penile prosthesis can be used in severe cases of ED after failure of
other lines of treatment.
5
Ejaculatory Disorders5,6
Physiology of ejaculation
Normal ejaculation is composed of two phases; emission and expulsion.
1- Emission phase
Emission is the first phase of ejaculation characterized by passage of seminal
fluid from the prostate, seminal vesicles, and vas deferens into the posterior
urethra. It occurs concomitant with contraction of the internal urethral sphincter
which closes the bladder neck and prevents retrograde passage of semen into the
bladder. All organs participating in the emission phase receive dense autonomic
innervations (sympathetic and parasympathetic) that originate from pelvic plexus.
2- Expulsion phase
Expulsion is passage of seminal fluid from the posterior urethra to the
external urethral meatus. Expulsion is a spinal cord reflex and depends on
contractions of the pelvic floor muscles in addition to bulbospongiosus and
ischiocavernosus muscles. These contractions occur rhythmically at 0.8 second
intervals. The expulsion phase is associated with orgasm (intense pleasurable
feeling).
Premature ejaculation
Premature ejaculation (PE) is defined as the ejaculation that always or
nearly always occurs prior to or within about 1 minute of vaginal penetration in
primary (lifelong) PE or within 3 minutes or less in secondary (acquired) PE, and
is associated with negative personal consequences, such as distress, frustration,
and/or the avoidance of sexual contact.
Prevalence
Premature ejaculation (PE) is the most common sexual dysfunction in men, with
prevalence rates reaching up to 75%.
Types of PE
Primary (lifelong) PE: affects men who had never attained ejaculatory
control.
2. Secondary (acquired) PE: occurs after a period of normal ejaculatory control.
1.
Etio-pathogenesis of PE
1. Psychogenic factors
• Anxiety.
• Low frequency of sexual activity.
• Early sexual experience.
2. Biological factors
• Genetic predisposition: accounts for around 30% of PE cases
• Neurobiological theory: 5-hydroxytryptamine receptor dysfunction.
6
•
Penile sensitivity: due to a greater sensitivity of the penis to direct
stimulation.
•
Endocrinal diseases: such as diabetes mellitus or thyroid dysfunction.
•
Urological diseases: such as chronic prostatitis or prostate-vesiculitis.
•
Neurological diseases: such as multiple sclerosis and peripheral
neuropathies.
•
Drug-induced PE: such as amphetamine, cocaine, and dopaminergic drug.
•
Other sexual dysfunctions: such as erectile dysfunction.
Treatment of PE
1. Pharmacologic therapy: selective serotonin reuptake inhibitors (SSRIs)
antidepressants such as dapoxetine.
2. Behavioral therapy: such as start-stop technique.
7
References
1. Saleh R, Abu El-Hamd M, Abdel-Karim M, Abdelrahman H. Evaluation of
pubertal onset and characteristics in Egyptian boys: A cross-sectional
study. Andrologia. 2019 Mar;51(2):e13192. doi: 10.1111/and.13192. Epub
2018 Nov 8. PMID: 30411390.
2. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in
boys. Arch Dis Child. 1970 Feb;45(239):13-23.
3. Shindel AW, Lue TF. Medical and Surgical Therapy of Erectile
Dysfunction. 2022 Jul 17. In: Feingold KR, Anawalt B, Blackman MR,
Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K,
Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M,
Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R,
New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA,
Trence DL, Wilson DP, editors. Endotext [Internet]. South Dartmouth (MA):
MDText.com, Inc.; 2000–. PMID: 25905163.
4. Sooriyamoorthy T, Leslie SW. Erectile Dysfunction. 2022 Nov 28. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
PMID: 32965924.
5. Saleh R, Majzoub A, Abu El-Hamd M. An update on the treatment of
premature ejaculation: A systematic review. Arab J Urol. 2021 Aug
4;19(3):281-302. doi: 10.1080/2090598X.2021.1943273. PMID: 34552780;
PMCID: PMC8451625.
6. El-Hamd MA, Saleh R, Majzoub A. Premature ejaculation: an update on
definition and pathophysiology. Asian J Androl. 2019 Sep-Oct;21(5):425432. doi: 10.4103/aja.aja_122_18. PMID: 30860082; PMCID: PMC6732885.
8
INTRODUCTION TO ANDROLOGY
Anatomy of the male genital system
Testis
The testes are ovoid organs suspended by the spermatic cord inside the
scrotum. Each testis is about 4.5 cm length, 2.5 cm width and 2 cm in its
anteroposterior diameter. The volume of each testis ranges from 15-25 ml
and the weight is about 15-25 gm.
The testis is surrounded by a thick white outer capsule composed of 3 layers:
The inner tunica vasculosa, tunica albuginea and the outer tunica vaginalis.
The testis is divided by septa into about 250 lobules. Each of these lobules
contains 1-4 seminiferous tubules.
The seminiferous tubules have a central lumen and contain 2 types of cells :
Sertoli cells and spermatogenic cells with an outer thin basement membrane
surrounding by a fibrous tunica propria. The interstitial tissue in between the
seminiferous tubules is composed of blood vessels, lymphatics and
macrophages.
Functions of the testis
- Steroidogenesis ( testosterone production ) by leydig cells.
- Spermatogenesis.
Epididymis
It rests on the superior and posterolateral surfaces of the testis .The efferent
ductules arise from the rete testis, join together to form the epididymis which
is a single highly convoluted duct about 5-6 meters in length .It is divided
into 3 segments : Head ( caput) ,body( corpus) and tail ( cauda). three parts:
head (upper part), body (middle part) and tail (lower part). It transports
sperms from the testis to the vas deferens and acts as a site of sperm
maturation and storage.
1
Vas deferens
It is a muscular tube of about 45 cm length and 2.5 mm diameter. It begins as
a continuation of the lower end of the epididymal duct and ends by uniting
with the duct of the seminal vesicle to form the ejaculatory duct.
Seminal vesicles
They are 2 distinct lobulated structures, each of them measures about 4-6 cm
in length and 1 cm in width, lying lateral to vas deferens on the posterior
surface of the bladder base .They are not felt on PR examination unless they
are inflamed or obstructed .
Ejaculatory ducts
They are paired structures which are approximately 2 cm in length and
formed by the union of the ampulla of the vas deferens and the duct of the
seminal vesicle. Ejaculatory ducts terminate in the posterior wall of the
prostatic urethra at the verumontanum.
Prostate
The Prostate resembles a chest-nut in shape and size about 8 gm in weight. It
measures approximately 3 cm from the apex to the base and 3.5 cm across
the base. It is partly glandular; partly muscular organ which surrounds the
beginning of urethera .It is situated in the pelvic cavity behind the pubic arch
and in front of the ampulla of the rectum . It is perforated by the ejaculatory
duct and the urethra. It is divided into 2 lateral lobes and a median lobe. Its
acini open directly in the posterior urethra at the prostatic sulcus. It is
enclosed within 2 capsules; true anatomic fibro-muscular capsule and false
capsule formed by the surrounding compressed pelvic fascia.
2
MALE INFERTILITY
Fertility refers to the capability to conceive or induce a pregnancy.
Fecundity refers to the proba bility of producing a live birth arising from a given
menstrual cycle.
Infertility is the term used when a couple fails to induce a pregnancy within 1
year of regular unprotected intercourse.
Primary infertility defines the condition when no pregnancy at all has been
achieved.
Secondary infertility means no further pregnancies have occurred. The term
infertile can be applied to both men and women.
Incidence
- 15-20% of couples are unable to conceive within one year.
- 30% male factor, 40 % female factor, 20% combined male and
female factors and 10% idiopathic.
Causes of male infertility:
І. Pretesticular causes (endocrinal infertility)
A. Hypothalamic causes:
1. Kallmann’s syndrome (Gn RH deficiency).
2. Hypothalamic tumours.
B. Pituitary causes:
1. Hypopituitarism.
2. Prolactinoma.
Π. Testicular causes
A. Chromosomal and genetic disorders:
1. Klinefelter's syndrome (47XXY).
2. Y- chromosome Microdeletions.
3
B. Non genetic disorders:
1. Varicocele.
2. Cryptorchidism.
3. Testicular torsion.
4. Spermatogenic arrest.
5. Sertoli cell only syndrome.
6. Immotile cilia syndrome.
Ш. Post -testicular causes
A. Obstructive infertility:
1. Epididymal obstruction.
2. Vasal obstruction.
3. Ejaculatory duct obstruction.
4. Congenital bilateral absent vas.
B. Coital infertility:
Sever forms of erectile dysfunction or penile curvature that interfere
intravaginal semen deposition.
C. Ejaculatory infertility:
1. Retrograde ejaculation.
2. Anejaculation.
3. Anorgasmia.
IV. Miscellaneous
1. Infectious causes: Prostatitis, epididymitis.
2. Immunological infertility.
3. Neoplastic causes: Testicular tumours.
4. Medical causes and systemic diseases: Liver diseases and renal failure.
5. Drugs: Chemotherapy, anti-androgens and anabolics.
4
6. Environmental causes: Pollutions and insecticides.
Investigations of male infertility
1. Semen analysis:
The corner stone for infertile male assessment.
The main normal semen parameters include ( WHO,2010):
* Abstinence period: 3-5 days (range 2-7 days)
* Method of collection: Masturbation.
* Volume: 1.5ml (1.4-1.7)
* Liquefaction time: Within 15-60 minutes.
* Consistency: The length of the thread should not exceed 2 cm.
* Appearance: Characteristic color and odour.
* PH: Alkaline (7.2-7.8).
* Sperm concentration: 15million /ml (12-16/ ml)
* Total sperm count: 39 million /ejaculate (33- 46)
* Sperm motility:
- Progressive motility (PR %): 32% (31-34)
- Total motility (PR+NP %): 40% (38-42)
* Sperm Vitality: 58 (55-63)
* Sperm morphology: normal sperm forms: 4% (3-4)
* White blood cells (pus cells): less than 1 million / ml.
* Red blood cells: absent.
* Agglutination: should be less than 10%.
Recently WHO, 2021 published The main normal semen parameters as:
* Volume: 1.4ml (1.3-1.5)
5
* Sperm concentration: 16million /ml (15-18/ ml)
* Total sperm count: 39 million /ejaculate (35- 40)
* Sperm motility:
- Progressive motility (PR %): 42% (40-43)
- Total motility (PR+NP %): 40% (38-42)
- Non Progressive motility (NP %): 1% (1-1)
- Immotile Spermatozoa (IM) : 20 ( 19-20)
* Sperm Vitality: 54 (50-56)
* Sperm morphology: normal sperm forms: 4% (3.9-4)
Definitions of semen abnormalities
Normozoospermia: total number (or concentration, depending on outcome
reported) of spermatozoa, and percentages of progressively motile (PR) and
morphologically.
Azoospermia: no spermatozoa in the ejaculate (given as the limit of quantifi cation
for the assessment method employed) .
Cryptozoospermia: spermatozoa absent from fresh preparations but observed in a
centrifuged pellet.
Oligozoospermia: total number (or concentration, depending on outcome
reported) of spermatozoa below the lower reference limit.
Asthenozoospermia: percentage of progressively motile (PR) spermatozoa below
the lower reference limit.
Teratozoospermia: percentage of morphologically normal spermatozoa below the
lower reference limit.
Oligoasthenozoospermia: total number (or concentration, depending on outcome
reported) ofspermatozoa, and percentage of progressively motile (PR)
spermatozoa, below the lower reference limits.
Oligoteratozoospermia: total number (or concentration, depending on outcome
reported) of spermatozoa, and percentage of morphologically normal spermatozoa,
6
below the lower reference limits
Asthenoteratozoospermia: percentages of both progressively motile (PR) and
morphologically normal spermatozoa below the lower reference limits.
Oligoasthenoteratozoospermia: total number (or concentration, depending on
outcome reported) of spermatozoa, and percentages of both progressively motile
(PR) and morphologically normal spermatozoa, below the lower reference limits.
Necrozoospermia: low percentage of live, and high percentage of immotile,
spermatozoa in the ejaculate.
Haemospermia (haematospermia): presence of erythrocytes in the ejaculate.
leukospermia (leukocytospermia, pyospermia): presence of leukocytes in the
ejaculate above the threshold value ( Pus cells more than 1 million / ml).
2. Hormonal assay for FSH, LH, testosterone and prolactin.
3. Scrotal ultrasonography to detect varicocele.
4. Trans-rectal ultrasonography, to study the prostate, seminal vesicles
and ejaculatory ducts.
5. Chromosomal study, to detect chromosomal abnormalities as in
Klinefelter's syndrome.
6. Sperm DNA fragmentation.
7. CT and MRI for undescended testis.
Treatment of male infertility
І. Medical Treatment
- Treatment of hypogonadotrophic hypogonadism : Replacement therapy
by FSH and LH.
- Treatment of hyperprolactinemia : Bromocriptine.
- Treatment of infection: Antibiotics e.g. Doxycycline, Quinolone.
- Treatment of immunological infertility: Corticosteroids.
- Treatment of systemic causes: Hypothyroidism and liver diseases.
7
- Non-specific treatment: Antioxidants, anti- estrogens e.g. Clomiphene
citrate and tamoxifen , aromatase inhibitors e.g. letrizole and
mucolytics e.g. ambroxole.
II. Surgical Treatment
1. Varicocelectomy for the varicocele.
2. Epididymovasostomy for epididymal obstruction.
3. Trans- urethral resection for veruomontanum (TUR-Veru) in
ejaculatory duct obstruction.
III. Assisted Reproductive Technologies (ART)
1. Artificial insemination using husband's semen (AIH).
2. In Vitro Fertilization (IVF).
3. Intracytoplasmic sperm injection (1CSI).
Varicocele
Varicocele is an abnormal dilatation of veins of the pampiniform
plexus of veins draining the testis (dilatation, thickening and
tortuosity).
Varicocele is the most common and correctable cause of male
infertility.
Varicocele is more common on the left side than the right side.
There is a predominance for left varicocele due to: The left testicular
vein is approximately 8-10 cm longer and left testicular vein drains at
right angle into the left renal vein while the right testicular vein drains
obliquely into the inferior vena cava.
Theories of varicocele impact on testicular function are : Heat ,
metabolites accumulation , elevated oxidative stress and epididymal
8
dysfunction .
Clinical grades
- Grade 1: Palpable during Valsalva’s manoeuvre.
- Grade 2: Palpable at rest, but not visible.
- Grade 3: Visible and palpable at rest.
- Subclinical: Not palpable or visible at rest or during Valsalva’s
manoeuvre , but demonstrable by Duplex examination .
Diagnosis: Scrotal duplex.
Treatment: Varicocelectomy.
Klinefelter's syndrome (47XXY)
It is a chromosomal disorder that leads to disturbed chromosomal
sex and primary testicular failure.
It is the most common chromosomal disorders in infertility and
most common cause of hypogonadism .
The patients are tall with gynecomastia , small firm testes , and ill
developed secondary sexual characters .
The semen is azoospermic.
Chromosomal study (karyotyping) : shows 47XXY.
Treatment
- Androgen replacement therapy.
- Infertility problem can be solved in some patients who have
spermatogenic foci by TESE and ICS
9
Assisted Reproductive Technologies (ART)
Definition:
Treatments or procedures that include the handling of human egg, sperm or
embryo for the purpose of establishing a pregnancy.
Methods of ART:
1- Artificial insemination
2- In Vitro Fertilization ( IVF)
3- Intracytoplasmic sperm injection (1CSI)
1- Artificial insemination:
A. Intravaginal insemination.
B. Intracervical insemination.
C. Intrauterine insemination (IUI).
D. Intratubal insemination.
Indications:
1. Slight deficiency in the number or motility of sperms.
2. Female cervical factors.
3. Unexplained infertility.
2- In Vitro Fertilization ( IVF):
The first successful IVF case was in 1978 when a British woman
delivered a baby called Louise Brown.
Indications:
1. Men with low sperm count, weak motility and /or abnormal morphology.
2. Women with blocked fallopian tubes.
10
3. Ovulation problems.
4. Unexplained infertility.
3- Intracytoplasmic sperm injection (1CSI):
It is the most common used ART procedure nowadays.
Indications:
- Severe oligo ,astheno and /or teratozoospermia.
- Azoospermia:
In cases of obstructive azoospermia, sperms are retrieved by
Testicular Sperm Aspiration (TESA) or Percutaneous Epididymal
Sperm Aspiration (PESA).
In cases of non-obstructive azoospermia, sperms might be retrieved by
Microsurgical Testicular Sperm Extraction (Micro TESE).
- Women with blocked fallopian tubes.
- Ovulation problems.
- Immune infertility.
- Unexplained infertility.
- Failed IUI trials.
Complications of ART:
- Miscarriage (15%).
- Multiple gestation pregnancies (25%).
- Ectopic pregnancy (2-5%).
- Increased the risk of prematurity and C/S.
11
References:
1. Eberhard Nieschlag , Hermann M. Behre and Susan Nieschlag.
Andrology- Male Reproductive Health and Dysfunction ,Springer Heidelberg
Dordrecht London New York 3rd Edition.2010.
2. Kamal Abdel-Hafez and Staff Members of Dermatology , Venereology
and Andrology Department , Faculty of Medicine , Assiut University.
Essentials of Dermatology , Venereology and Andrology, 7th Edition.20182019. Deposit number in the Egyptian National
manual for the
Library:15996/2001.
3. World Health Organization 2010 .WHO laboratory manual for the
examination and processing of human semen - 5th ed. 2010
4. World Health Organization 2021 .WHO laboratory manual for the
examination and processing of human semen - 6th ed. 2010
12