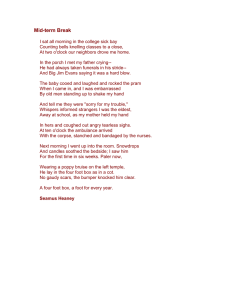
Musculoskeletal Science and Practice xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Musculoskeletal Science and Practice journal homepage: www.elsevier.com/locate/msksp Technical and measurement report Reliability of Foot Posture Index individual and total scores for adults and older adults Mariana R.C. Aquinoa, Bruna S. Avelara, Paula L. Silvab, Juliana M. Ocarinoa, Renan A. Resendea,∗ a Universidade Federal de Minas Gerais, School of Physical Education, Physical Therapy and Occupational Therapy, Department of Physical Therapy, Avenida Antônio Carlos, 6627, Campus Pampulha, Pampulha, 31270-901, Belo Horizonte, MG, Brazil b University of Cincinatti, Department of Psychology, 2600 Clifton Ave, Cincinnati, OH 45220, United States A R T I C L E I N F O A B S T R A C T Keywords: Foot posture Pronation Supination Elderly Background: Previous studies have suggested that the Foot Posture Index (FPI-6) is valid and reliable to evaluate foot posture of adults and children. However, studies with adults had some important limitations. In addition, it is not clear if FPI-6 is reliable for older adults. Variations in foot structure, such as edema, bone callosity and bunions, are more frequent in older adults, which may compromise FPI-6 reliability for this population. Objectives: To investigate test-retest and inter-rater reliability of FPI-6 total and individual scores for the assessment of foot posture of adults and older adults. Methods: Twenty-one adults and 19 older adults participated in this study. The examiners performed FPI-6 on two days of data collection. We used Cohen Weighted Kappa and Intraclass Correlation Coefficient for categorical and continuous variables, respectively. Results: For adults, FPI-6 scores demonstrated test-retest reliability varying from fair to substantial and interrater reliability varying from fair to almost perfect. For older adults, FPI-6 scores demonstrated test-retest reliability varying from not reliable to moderate and inter-rater reliability varying from fair to almost perfect. The examiners demonstrated more than 80% of agreement in all FPI-6 scores for adults and older adults. Conclusions: The relatively low reliability in light of this high level of agreement suggest that the current version of FPI-6 can be a useful tool to assess foot posture for adults and should be further examined. On the other hand, FPI-6 should be cautiously used for older adults. 1. Introduction The Foot Posture Index (FPI-6) was designed to be quick and reliable to evaluate foot posture (Redmond et al., 2006). FPI-6 has six items that are used to quantify and to classify foot posture (Redmond, 2005). Unlike other instruments, FPI-6 encompasses most of the foot segments and the three planes of motion (Redmond et al., 2006). In addition, FPI6 data have stronger association with foot kinematics than other methods, suggesting that FPI-6 provides a more complete description of foot posture (Redmond et al., 2006). FPI-6 is validated for healthy individuals aged between 18 and 57 years (Redmond, 2005). However, studies that evaluated its inter-rater and test-retest reliability had conflicting results, with reliability variously reported as poor (Terada et al., 2014), moderate (Cornwall et al., 2008; Menz and Munteanu, 2005) and good (Lee et al., 2015; Morrison and Ferrari, 2009) reliability levels. This controversy may be explained by methodological limitations, such as concomitant assessment of both feet (Morrison and Ferrari, 2009), short time between the test and retest data collections (Cornwall et al., 2008; Evans et al., 2012; Terada et al., 2014), and inappropriate statistical methods (Evans et al., 2012). In addition, only one study included older adults (Menz and Munteanu, 2005). Variations in foot structure, such as edema, bone callosity and bunions, are more frequent in older adults (Shibuya et al., 2011), which may compromise FPI-6 reliability for this population. In addition, previous studies only evaluated reliability of FPI-6 total score (Caina et al., 2007; Cornwall et al., 2008; Evans et al., 2012; Terada et al., 2014; Menz and Munteanu, 2005). Considering that the sum of different scores on each item of FPI-6 may result on the same total score, it is not clear if each aspect of foot posture can be reliably assessed. This study evaluated the test-retest and the inter-rater reliability of FPI-6 total and individual scores for the assessment of foot posture of adults and older adults. ∗ Corresponding author. Universidade Federal de Minas Gerais, Pampulha, Avenida Antônio Carlos, 6627, School of Physical Education, Physical Therapy and Occupational Therapy, Department of Physical Therapy, 31270-901, Belo Horizonte, MG, Brazil. E-mail addresses: marircaquino@gmail.com (M.R.C. Aquino), avelar.bruna@gmail.com (B.S. Avelar), paulalanna@gmail.com (P.L. Silva), julianaocarino@gmail.com (J.M. Ocarino), renan.aresende@gmail.com (R.A. Resende). https://doi.org/10.1016/j.msksp.2018.02.002 Received 27 October 2017; Received in revised form 29 January 2018; Accepted 3 February 2018 2468-7812/ © 2018 Elsevier Ltd. All rights reserved. Please cite this article as: Aquino, M.R.C., Musculoskeletal Science and Practice (2018), https://doi.org/10.1016/j.msksp.2018.02.002 Musculoskeletal Science and Practice xxx (xxxx) xxx–xxx M.R.C. Aquino et al. 2. Methods 2.4. Statistical analysis 2.1. Participants FPI-6 total score was categorized in neutral (total score between 0 and 5), pronated (between 6 and 9), extremely pronated (higher than 9), supinated (between −1 and −4) and extremely supinated (lower than −4) (Redmond, 2005). We used Cohen's Weighted Kappa (Kw) with linear calculation to evaluate FPI-6 inter-rater and test-retest reliability (Viera and Garrett, 2005). We performed Kw for each FPI-6 item and for the total FPI-6 score. We used the StatsDirect software, version 3, to perform Kw analysis, using α = 0.05. The Kw values were interpreted as follows: slight, Kw between 0.01 and 0.20; fair, Kw between 0.21 and 0.40; moderate, Kw between 0.41 and 0.60; substantial, Kw between 0.61 and 0.80; and almost perfect, Kw between 0.81 and 1.0 (Viera and Garrett, 2005). In addition, we reported the observed percentage agreement. In order to allow comparisons with previous studies, we computed Intraclass Correlation Coefficient (ICC) for FPI-6 total raw score (i.e. not categorized) using SPSS (SPSS Inc., Chicago, USA). Sample size was determined considering an expected observed agreement of 0.8, chance agreement of 0.2 and relative error of 40%, resulting in a sample size of 17 participants for each group (Gwet, 2012). Individuals with age between 20 and 87 years participated in this study. They were divided in two age groups (WHO, 2010): adults (18–64 years), and older adults (above 65 years). The inclusion criteria were: (i) being able to remain in orthostatic position; (ii) no history of injury or surgery to the lower limbs in the past six months; (iii) no structural deformities of the lower limbs, as equinovarus foot, hammer toes and claw toes. The exclusion criteria were: (i) injuries between the test and the retest; (ii) not showing up for the retest. Participants signed a consent form approved by the university's Ethical Research Committee (CAAE: 58492216.0.0000). 2.2. Foot Posture Index (FPI-6) 3. Results FPI-6 is a clinical tool that classifies foot posture according to six items (Redmond, 2005): (i) palpation of the head of the talus; (ii) curvatures above and below the lateral malleolus; (iii) position of the calcaneus in the frontal plane; (iv) prominence in the talonavicular joint; (v) the medial longitudinal arch's congruence; and (vi) abduction/adduction of the forefoot on the rearfoot. Each item is scored from −2 to 2, resulting in a total score of −12 to 12. Negative values indicate supinated foot posture and positive values indicate pronated foot posture. The detailed description of FPI-6 can be found elsewhere (Redmond, 2005). 3.1. Participants Twenty-one adults (four men and seventeen women), with an average age, mass, and height of 26.90 years (SD 10.01), 62.16 kg (SD 14.15), and 1.64 m (SD 0.08), respectively, participated in this study resulting in 42 feet assessments. In addition, 19 older adults (two men and seventeen women), with an average age, mass, and height of 73.53 years (SD 7.87), 68.62 kg (SD 16.83), and 1.61 m (SD 0.73), respectively, participated in this study – resulting in 38 feet assessments. Two examiners were recruited: Examiner 1 was an undergrad physiotherapy student and Examiner 2 was a physiotherapist with five years of clinical practice. 2.3. Procedures The examiners used FPI-6 in 30 feet before data collection (Redmond, 2005). During this training period, they could communicate with each other for familiarization with FPI-6. The participant stood on a step, with the arms by the side and looking straight ahead. Following FPI-6 guidelines (Redmond, 2005), the examiners were not allowed to see the participant's contralateral foot during the evaluation of foot posture (Fig. 1). Each FPI-6 item was independently evaluated and scored by each examiner in separate sheets. First, the examiners evaluated the left foot, and then, the right foot. In order to evaluate testretest reliability, both examiners repeated data collection on the same participant 7–15 days after the first day of data collection. The examiners were blinded to each other and to their own data. Both feet were considered for analyses. 3.2. Adults FPI-6 test-retest reliability, for adults, is reported in Table 1. FPI-6 total score demonstrated test-retest reliability varying between moderate and substantial. In addition, FPI-6 total-score demonstrated testretest ICC of 0.66 (confidence interval (CI) of 95%, 0.45–0.80) and 0.69 (CI95%, 0.49–0.82) for the Examiner 1 and 2, respectively. The six items of FPI-6 demonstrated reliability varying from fair to substantial. FPI-6 inter-rater reliability, for adults, is reported in Table 2. The FPI-6 total score demonstrated inter-rater reliability varying between moderate and substantial. In addition, the FPI-6 total-score demonstrated inter-rater ICC of 0.79 (CI95%, 0.64–0.88). The six items of FPI6 demonstrated inter-rater reliability varying from fair to almost perfect. Fig. 1. Participant standing posture during data collection of the left foot. A) Posterior view. B) Anterior view. 2 Musculoskeletal Science and Practice xxx (xxxx) xxx–xxx M.R.C. Aquino et al. Table 1 FPI-6 test-retest reliability for adults. Variable Examiner 1 (Kw) Observed Agreement Examiner 1 (%) Examiner 2 (Kw) Observed Agreement Examiner 2 (%) Total FPI-6 Item 1: PHT Item 2: CLM Item 3: CFP Item 4: PTN Item 5: MAC Item 6: ABD/ADD Mean (SD) 0.48 0.44 0.53 0.37 0.58 0.43 0.56 0.48 (0.07) 88.89 92.86 88.1 81.75 84.52 82.14 85.71 86.28 (3.97) 0.65 0.39 0.52 0.43 0.36 0.76 0.57 0.52 (0.14) 88.10 78.57 85.71 83.33 73.81 92.86 91.67 83.53 (6.5) Kw – Weighted Kappa; Total FPI-6 – Foot Posture Index total score; PHT – palpation of the head of the talus; CLM – curvatures above and below the lateral malleolus; CFP – position of the calcaneus in the frontal plane; PTN – prominence in the talonavicular joint; MAC – medial longitudinal arch's congruence; ABD/ADD – abduction/adduction of the forefoot on the rearfoot; SD - standard deviation. Table 2 FPI-6 inter-rater reliability for adults in both days of data collection. Table 4 FPI-6 inter-rater reliability for the older adults on both days of data collection. Variable Day 1 (Kw) Observed Agreement Day 1 (%) Day 2 (Kw) Observed Agreement Day 2 (%) Variable Day 1 (Kw) Observed Agreement Day 1 (%) Day 2 (Kw) Observed Agreement Day 2 (%) Total FPI-6 Item 1: PHT Item 2: CLM Item 3: CFP Item 4: PTN Item 5: MAC Item 6: ABD/ ADD Mean (SD) 0.63 0.36 0.75 0.37 0.46 0.84 0.54 92.06 91.27 92.86 80.16 77.38 95.24 88.10 0.57 0.36 0.53 0.30 0.48 0.59 0.45 85.71 89.29 87.50 80.16 78.57 86.90 84.52 0.41 0.31 0.55 0.38 0.25 0.42 0.47 88.16 84.21 87.50 83.55 79.80 85.96 85.09 0.33 0.45 0.83 0.45 0.26 0.54 0.53 82.89 94.74 95.39 87.50 81.58 86.84 85.96 0.56 (0.18) 88.15 (0.07) 0.47 (0.11) 84.66 (0.04) Total FPI-6 Item 1: PHT Item 2: CLM Item 3: CFP Item 4: PTN Item 5: MAC Item 6: ABD/ ADD Mean (SD) 0.40 (0.10) 84.89 (0.03) 0.48 (0.18) 87.84 (0.05) Kw – Weighted Kappa; Total FPI-6 – Foot Posture Index total score; PHT – palpation of the head of the talus; CLM – curvatures above and below the lateral malleolus; CFP – position of the calcaneus in the frontal plane; PTN – prominence in the talonavicular joint; MAC – medial longitudinal arch's congruence; ABD/ADD – abduction/adduction of the forefoot on the rearfoot; SD - standard deviation. Kw – Weighted Kappa; Total FPI-6 – Foot Posture Index total score; PHT – palpation of the head of the talus; CLM – curvatures above and below the lateral malleolus; CFP – position of the calcaneus in the frontal plane; PTN – prominence in the talonavicular joint; MAC – medial longitudinal arch's congruence; ABD/ADD – abduction/adduction of the forefoot on the rearfoot; SD - standard deviation. 3.3. Older adults 4. Discussion FPI-6 test-retest reliability, for older adults, is reported in Table 3. The FPI-6 total score demonstrated test-retest reliability varying between not reliable and fair. In addition, the FPI-6 total score demonstrated test-retest ICC of 0.41 (CI95%, 0.11–0.64) for Examiner 2 and was not reliable for Examiner 1. The six items of FPI-6 demonstrated test-retest reliability varying from not reliable to moderate. FPI-6 inter-rater reliability, for older adults, is reported in Table 4. The FPI-6 total score demonstrated moderate inter-rater reliability. In addition, the FPI-6 total-score demonstrated inter-rater ICC of 0.69 (CI95%, 0.47–0.82). The six items of FPI-6 demonstrated inter-rater reliability varying from fair to almost perfect. FPI-6 scores demonstrated test-retest reliability varying from fair to substantial and inter-rater reliability varying from fair to almost perfect for adults. For older adults, FPI-6 scores demonstrated test-retest reliability varying from not reliable to moderate, and inter-rater reliability varying from fair to almost perfect. The low reliability demonstrated by some of FPI-6 scores might be explained by the limitations in FPI-6 manual, by the number of available scores for each item and by the low variability of foot postures in the older adults sample. FPI-6 total score demonstrated test-retest reliability varying from moderate to substantial and from not reliable to fair for the adults and older adults, respectively. Moreover, the six items of FPI-6 demonstrated test-retest reliability varying from fair to substantial, and from not reliable to moderate for adults and older adults, respectively. These Table 3 FPI-6 test-retest reliability for older adults. Variable Total FPI-6 Item 1: PHT Item 2: CLM Item 3: CFP Item 4: PTN Item 5: MAC Item 6: ABD/ADD Mean (SD) Examiner 1 (Kw) 0.28 0.42 0.45 0.47 0.34 0.35 0.44 0.39 (0.07) Observed Agreement Examiner 1 (%) Examiner 2 (Kw) a 84.21 92.11 84.87 86.84 84.21 85.09 83.33 85.81 (0.03) 0.04 0.14a 0.51 0.31 0.33 0.35 0.31 0.28 (0.15) Observed Agreement Examiner 2 (%) 76.32 90.79 86.84 82.89 82.46 82.46 80.70 83.20 (0.04) a No significant. Kw – Weighted Kappa; Total FPI-6 – Foot Posture Index total score; PHT – palpation of the head of the talus; CLM – curvatures above and below the lateral malleolus; CFP – position of the calcaneus in the frontal plane; PTN – prominence in the talonavicular joint; MAC – medial longitudinal arch's congruence; ABD/ADD – abduction/adduction of the forefoot on the rearfoot; SD - standard deviation. 3 Musculoskeletal Science and Practice xxx (xxxx) xxx–xxx M.R.C. Aquino et al. varying from not reliable to almost perfect for adults and older adults. The low reliability levels of some of FPI-6 scores may be explained by limitations in FPI-6 manual, by the number of available scores for each item and by the low variability of foot postures in the older adults sample. Notably, examiners demonstrated more than 80% agreement in all FPI-6 scores. The relatively low reliability in light of this high level of agreement suggest that the current version of FPI-6 can be a useful tool to assess foot posture for adults and should be further examined. On the other hand, FPI-6 should be cautiously used for older adults. results demonstrate that, in general, the FPI-6 does not have high reliability levels, especially for older adults. This may be explained by some limitations in the FPI-6's manual. For example, FPI-6 manual does not show example figures of intermediate scores. In addition, for item 4, the manual figure shows a foot part that is not exactly the talonavicular joint region (Redmond, 2005), which may explain why item 4 had the lowest inter-rater reliability, for both days and age groups. Future studies could examine if improvements in the identified aspects of the manual would lead to increased reliability of the FPI-6. The low test-retest reliability levels may also be explained by the low variability in our older adults sample, since it increased the expected agreement due to chance and reduced Kw values (Viera and Garrett, 2005) even with high levels of observed agreement. It is possible that using a healthy sample contributed to the low variability of foot postures. Notably, however, the low variability in FPI-6 scores observed in our study is not an isolated finding (see for instance Cornwall et al., 2008; Terada et al., 2014; McLaughlin et al., 2016; Morrison and Ferrari, 2009; Teyhen et al., 2011). This consistently low variability across many studies is likely related to consistently low frequency in particular extreme scores (e.g., extremely supinated foot posture), suggesting that the number of FPI-6 categories might be excessive. The general lower reliability of the FPI-6 for older adults in comparison to adults may be explained by the difficulty, reported by examiners, to visualize bony structures in the former. The presence of calluses, bunions and edema are more common in this age group (Shibuya et al., 2011), which made it difficult to rate some items. This rationale is supported by the fact that, for older adults, the item that involved palpation in addition to visual observation (i.e. item 2) demonstrated the highest reliability. However, the influence of foot variations on FPI-6 reliability is only speculative at this point. In comparison to previous studies, this study demonstrated lower test-retest (ICC = 0.69) and similar inter-rater (ICC = 0.79) reliability of the FPI-6 total score for adults. Cornwall et al. (2008), for example, reported high test-retest reliability for young adults (ICC = 0.93), and moderate inter-rater reliability (ICC = 0.70). However, they only had 15 min of interval between the test and the retest, which likely increased the contribution of memory effects. For older adults, Menz and Munteanu (2005) demonstrated higher test-retest reliability (ICC = 0.61) than the present study (ICC = 0.41). The higher level of experience of the examiner in that study may help to explain these different findings. It should be noted that previous studies only evaluated FPI-6 total score. Different scores in individual items may result in the same total score. Thus, it is not clear if the examiners of these previous studies were reliable in the FPI-6 individual items. Most of our sample were female. Therefore, these results should only be cautiously applied for men (Menz, 2004). In addition, the variability in foot postures for adults and older adults were 0.63 and 0.46 (Allaj, 2017), respectively, suggesting that lower variability might have compromised reliability for older adults. Future studies with larger sample size and including older adults with symptomatic feet might increase variability and consequently improve FPI-6 reliability for this population. Acknowledgements We are thankful to the State of Minas Gerais Funding Agency FAPEMIG [grant number APQ-01139- 15] and to the Funding Program for Recently Hired Professors of the Universidade Federal de Minas Gerais for their financial support. Finally, we are thankful to the Terceira Idade Program of the Universidade Federal de Minas Gerais for their support during data collection. References Allaj, E., 2017. Two simple measures of variability for categorical data. J. Appl. Stat. 1–20. http://dx.doi.org/10.1080/02664763.2017.1380787. Caina, L.E., Nicholson, L.L., Roger, D., Adams, J.B., 2007. Foot morphology and foot/ ankle injury in indoor football. J. Sci. Med. Sport 10, 311–319. http://dx.doi.org/10. 1016/j.jsams.2006.07.012. Cornwall, M.W., McPoil, T.G., Lebec, M., Vicenzino, B., Wilson, J., 2008. Reliability of the modified foot posture index. J. Am. Podiatr. Med. Assoc. 98, 7–13. http://dx.doi.org/ 10.7547/0980007. Evans, A.M., Rome, K., Peet, L., 2012. The foot posture index, ankle lunge test, Beighton scale and the lower limb assessment score in healthy children: a reliability study. J. Foot Ankle Res. 5, 1. http://dx.doi.org/10.1186/1757-1146-5-1. Gwet, K.L., 2012. Handbook of Inter-rater Reliability. pp. 121–139. Lee, Jong Dae, Mi Kim, Young, Kim, Kyung, Hyun Koh, Da, Su Choi, Myeong, HJL, 2015. Reliability of the foot posture index (FPI-6) for assessment of stroke patients. J. Kor. Phys. Ther. 27, 311–314. http://dx.doi.org/10.18857/jkpt.2015.27.5.311. McLaughlin, P., Vaughan, B., Shanahan, J., Martin, J., Linger, G., 2016. Inexperienced examiners and the foot posture index: a reliability study. Man. Ther. 26, 238–240. http://dx.doi.org/10.1016/j.math.2016.06.009. Menz, H.B., 2004. Two feet, or one person? Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot 14, 2–5. http://dx.doi.org/10.1016/ S0958-2592(03)00047-6. Menz, H.B., Munteanu, S.E., 2005. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J. Orthop. Sports Phys. Ther. 35, 479–486. http://dx.doi.org/10.2519/jospt.2006.0201. Morrison, S.C., Ferrari, J., 2009. Inter-rater reliability of the Foot Posture Index (FPI-6) in the assessment of the paediatric foot. J. Foot Ankle Res. 2, 26. http://dx.doi.org/10. 1186/1757-1146-2-26. Redmond, A., 2005. The Foot Posture Index - Easy Quantification of Standing Foot Posture - Six Item Version FPI-6-User Guide and Manual. pp. 1–19 United Kingdom. Redmond, A.C., Crosbie, J., Ouvrier, R.A., 2006. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin. Biomech. 21, 89–98. http://dx.doi.org/10.1016/j.clinbiomech.2005.08.002. Shibuya, Naohiro, Jupiter, Daniel C., Ciliberti Jr., Louis J., VanBuren, Vincent, JLF, 2011. Prevalence of podiatric medical problems in veterans versus nonveterans. J. Am. Podiatr. Med. Assoc. 101, 323–330. http://dx.doi.org/10.7547/1010323. Terada, Masafumi, Wittwer, Ara M., PAG, 2014. Intra-rater and inter-rater reliability of the five image-based criteria of the foot posture Index-6. Int. J. Sports Phys. Ther. 9, 187–194. Teyhen, D.S., Stoltenberg, B.E., Eckard, T.G., Doyle, P.M., Boland, D.M., Feldtmann, J.J., et al., 2011. Static foot posture associated with dynamic plantar pressure parameters. J. Orthop. Sports Phys. Ther. 41, 100–107. http://dx.doi.org/10.2519/jospt.2011. 3412. Viera, A.J., Garrett, J.M., 2005. Understanding interobserver agreement: the Kappa statistic. Fam. Med. 37, 360–363. WHO, 2010. Global recommendations on physical activity for health. Geneva World Heal Organ 60. 5. Conclusions FPI-6 scores demonstrated test-retest and inter-rater reliability 4