Basic EKG Interpretation: A Cardiology Presentation
advertisement

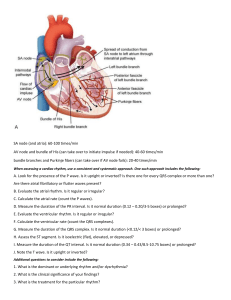
Basic EKG Interpretation MELISSA EMERY BSN, RN SPRING 2025 LEVEL 1 Learning Objectives 1. Discuss the cardiac conduction and electrical rhythm of the heart 2. Analyze elements of an ECG strip: ventricular and arterial rate & rhythm, QRS complex and shape; QRS duration, P-wave, P-wave shape, and PR interval 3. Analyze an ECG rhythm strip to identify normal sinus rhythm as well as common or lifethreatening dysrhythmias 4. Identify medications, treatments, and client monitoring needed to prevent, treat, or reverse cardiac dysrhythmias 5. Discuss implantable pacemakers, the purpose, and clients who are likely to need them. 6. Identify patient teaching needs for self-management and self-care with a pacemaker 7. Differentiate between defibrillation and cardioversion, when it should be used, and complications following these procedures 8. Identify nursing care and management for clients who require telemetry or continuous ECG monitoring. Electrical Cardiac Conduction Electrode Placement for ECG ▪ Found on the ECG is the ECG waveform (PQRST complex) and small/large boxes. ▪ First, the ECG strip paper is made up of small boxes that are contained within large squares. Each box represents a measurement of time. Each small square represents 0.04 seconds of time ▪ Each large square has 5 small squares in it so it represents 0.20 seconds Explanation ▪ Remember each tiny box =0.04 seconds ▪ Looking horizontally …along time…..It takes 5 of those to make the bigger box inside the bold lines ▪ So…5 x 0.04=0.20 seconds ▪ 5 of those larger boxes=1 second Another look at Normal PQRST Complex Normal Characteristics of Each Part of the PQRST Complex ▪ P-wave: One p-wave should be present and in front of every QRS complex, be upright and round, not flat Measurement should be less than 0.12 seconds (no more than 3 squares) ▪ PR interval normal range is 0.12-0.20 seconds (beginning of P wave to beginning of QRS) ▪ QRS complex: should be behind every p wave, should not be very wide or narrow, and measures no more than 0.12 seconds. Start of the Q wave and end at the S wave. ▪ ST segment is identified as isoelectric, or above or below isoelectric line ▪ QT interval normal range is 0.32-0.40 seconds ▪ TP interval is isoelectric period ▪ PP interval signifies atrial rhythm and rate ▪ RR interval signifies ventricular rate and rhythm Analyzing the ECG Rhythm Strip ▪ Determine ventricular rate ▪ Determine ventricular rhythm ▪ Determine QRS duration ▪ Determine whether QRS duration is consistent ▪ Identify QRS shape ▪ Identify P waves, is there a P in front of every QRS? ▪ Identify P wave shape ▪ Determine atrial rate ▪ Determine atrial rhythm Or… ▪ What is the ventricular RATE? ▪ (# of R-R intervals in 6 sec. x 10= ventricular rate in bpm) SA 60-100 bpm AV 40-60 bpm Ventricular 30-40 bpm ▪ Is the RHYTHM regular or irregular? Additionally, measure P-R Interval, measure QRS duration ▪ Check the RELATIONSHIP Is there a p wave for every QRS? (are the atria communicating with the ventricles?) Are they evenly spaced? Analyze this! Sinus Rhythms ▪ Impulse originates ▪ at the _________ ▪ Rate is__-___bpm Normal Sinus Rhythm ▪ Ventricular Rate 60-100 BPM ▪ Rhythm regular (PQRST complexes evenly spaced) ▪ The rhythm originates in the SA node and follows the normal pathway of conduction, resulting in atrial and ventricular depolarization. ▪ Treatment- when associated with a pulse, no treatment required. Sinus Bradycardia ▪ Rate < 60 bpm ▪ Rhythm regular ▪ Causes: Normal in conditioned athletes. ▪ May be due to increased vagal tone (as seen with vomiting and/or straining on stool), or hypothermia. ▪ May be seen after MI or pts. on digitalis, beta-blockers, quinidine, or calcium channel blockers. ▪ S/S: May be asymptomatic. ▪ If decreased CO occurs as a result of slow HR, may result in fatigue, syncope, lightheadedness, hypotension, SOA ▪ Tx: Treat only symptomatic bradycardias. (atropine, transcutaneous pacing) Sinus Bradycardia Sinus Tachycardia ▪ Rate >100 BPM ▪ Rhythm regular ▪ Causes: Normal response to increased oxygen demand due to fever, pain, anxiety, hypoxia, CHF, fright, stress, etc... ▪ S/S: May be asymptomatic. Possible angina due to increased myocardial oxygen demand. ▪ Can be associated with physiological and psychologic stressors such as exercise, fever, pain, hypotension, hypovolemia, anemia, hypoxia, MI, HF, anxiety, fever. ▪ It can also be an effect of drugs such as epinephrine, Norepinephrine (levophed), Atropine, Caffeine. ▪ Tx: directed at correcting the underlying cause. O2 Tx may be beneficial. Sinus Tachycardia (>100 bpm) Dysrhythmias/Arrhythmias ▪ Abnormal change in HR, heart rhythm, or both ▪ Normally electrical impulses make the heart contract ▪ Any disruption of the electrical impulse’s pathway can produce an arrhythmia ▪ Rhythms are named according to site of origin of the impulse and the mechanism of formation or conduction involved. ▪ ex: an impulse that originates in the Sinoatrial Node (SA) node is a Sinus Rhythm ▪ If…that rhythm has an increased rate is ……Sinus Tachycardia Sinus Arrhythmia Premature Atrial Complexes (PACs) ▪ Rate will depend on the underlying rhythm, and the premature beat will interrupt the regularity of the underlying rhythm. ▪ Causes: CHF, MI, pulmonary embolism, dig toxicity, hypokalemia, hypomagnesemia. ▪ S/S: c/o “skip” or occasional “palpitations” if PACs are frequent or may be unaware of their occurrence. ▪ Tx: Usually doesn’t require tx if infrequent, however frequent PAC’s may initiate episodes of A-fib or A-flutter. Premature Atrial Complexes (PACs) Atrial Fibrillation (or A Fib) ▪ Atrial rate can’t be measured because it’s too chaotic, (Chaos between the QRS complexes but ventricular rate is variable. Rhythm is usually very irregular.) ▪ Causes- significance depends on the ventricular rate. The more rapid the ventricular rate, the more serious the dysrhythmia. May be due to ischemic heart disease, hypoxia, pulmonary embolism, mitral or tricuspid valve disease, MI, dig or quinidine toxicity. ▪ S/S- May be asymptomatic. May sense palpitations, lightheadedness or weakness. Usually, a pulse deficit noted. ▪ Tx- Depends on presentation. If stable, calcium channel blockers or beta-blockers to control ventricular rate. If serious s/s present due to rapid ventricular rate, synchronized cardioversion. If sustained, these pts. need anticoagulant tx (warfarin) to prevent mitral thrombi. Atrial Fibrillation ▪ Atrial fibrillation with a ventricular rate < 100 can be called “A-fib with controlled ventricular response” ▪ A-fib with a ventricular rate > 100 is considered uncontrolled A-fib. Can be called “A-fib with rapid ventricular response” (or RVR) A Fib Video Atrial Flutter ▪ Sawtooth appearance ▪ Ventricular rate variable- determined by AV blockade ▪ Same causes, S/S, and Tx as A-Fib. ▪ A-fib with rate <100 bpm considered controlled ventricular response ▪ A-fib with rate > 100 bpm considered Accelerated ventricular response Atrial Flutter Video Ventricular Dysrhythmias ▪ Impulse originates ▪ at the _________ ▪ Rate is__-___bpm Premature Ventricular Complexes (PVC) ▪ Rate will depend on the underlying rhythm, and the premature beat will interrupt the regularity of the underlying rhythm. ▪ Cause- Can occur in healthy persons with apparently normal hearts and with no apparent cause. May also occur because of hypoxia, an increase in catecholamines, acid-base imbalance, electrolyte imbalance, dig toxicity, ischemia, MI, CHF, excessive caffeine, tobacco, or alcohol use. Premature Ventricular Complexes (PVC) (cont.) ▪ S/S- may be asymptomatic or c/o skipped beats. If PVC’s are frequent, signs of decreased CO may be present. ▪ Tx- dependent on the cause, s/s, and clinical situation. If occurring with MI, should be directed at assuring adequate O2, relief of pain, and rapid identification and correction of electrolyte imbalances. Premature Ventricular Contractions (PVCs) ▪ Wide and bizarre QRS (>0.12 sec.) ▪ Occur with an underlying rhythm, ex: NSR with PVCs Ventricular Tachycardia (or… V Tach of VT) Ventricular Tachycardia ▪ Atrial rate not discernible, ventricular rate 100-250 BPM. Ventricular rhythm essentially regular. QRS is wide and bizarre. ▪ Causes- myocardial irritability due to MI, CAD, CHF, hypoxia. May also be caused by toxicity from dig. ▪ S/S- If conscious, pt. may c/o palpitations or SOB. Loss of consciousness may occur. (esp. if VT is prolonged or sustained). ▪ Tx- pt. stable w/pulse Amiodarone, Adenosine, Oxygen, IV access, (may quickly go unstable) pt. pulseless treat as VF (both are shockable rhythms). Ventricular Fibrillation ( or…V Fib or VF) ▪ Rate can NOT be determined ▪ No pattern or regularity ▪ Causes- MI, untreated VT, hypothermia, electrolyte imbalance, electrocution, hypoxia, dying heart. ▪ Life threatening!!! ▪ S/S- pulseless, apneic ▪ Rhythm is rapid and chaotic ▪ Tx- Defibrillation, CPR Shockable Rhythms Cardioversion and Defibrillation ▪ Delivery of electrical current to depolarize a critical mass of myocardial cells. (When cells repolarize, the SA node is usually able to recapture its role as pacemaker of the heart.) ▪ Cardioversion involves use of “timed” electrical current to terminate a tachydysrhythmia. (Synch “on”) ▪ Defibrillation is used in emergency situations as treatment for ventricular fibrillation and pulseless VT (Synch “off”) Placement of Defib Paddles Asystole ▪ Ventricular rate indiscernible, but may see some atrial activity ▪ No rhythm present ▪ Causes- extensive myocardial damage, ventricular aneurysm, acute respiratory failure. ▪ S/S- pulseless, apneic ▪ Tx- CPR, IV, consider possible causes, and meds. NOT a Shockable Rhythm Pattern of deterioration….. For VF/pVT: For Asystole/PEA: ▪ - High quality CPR ▪ Biphasic: Manufacturer recommendation (eg, initial dose of 120-200 J); if unknown, use maximum available. Second and subsequent doses should be equivalent, and higher doses may be considered. • Monophasic: 360 J ▪ - Give Epinephrine 1 mg every 3-5 minutes, followed by a 10-20 mL flush of NS/LR ▪ - May give Amiodarone First Dose 300 mg IV/IO bolus. ▪ Second Dose: 150 mg ▪ - May give Lidocaine 1-1.5 mg/kg IV/IO bolus First dose: 1-1.5 mg/kg. ▪ Second dose: 0.5-0.75 mg/kg. ▪ - High quality CPR ▪ - Give Epinephrine 1 mg every 3-5 minutes, followed by a flush of 10-20 mL NS/LR ▪ - Correct possible causes (H/Ts) ▪ Hypovolemia ▪ Hypoxia • Hydrogen ion (acidosis)• Hypo/hyperkalemia • Hypothermia • Tension pneumothorax • Tamponade, cardiac • Toxins • Thrombosis, pulmonary • Thrombosis, coronary Pacemakers ▪ Pacemaker- an electronic device that delivers an electrical stimulus to the heart to depolarize the myocardium. ▪ Used for slower-than-normal impulse formation, or to control some tachycardias,or for advanced heart failure ▪ May be permanent or Temporary Pacemaker Video Review Questions References ▪ Harding, M., Kwong, J., Hagler, D., Roberts, D., Reinisch, C., & Lewis, S. M. (2020). Lewis's medical-surgical nursing: Assessment and management of clinical problems. Elsevier. ▪ Algorithms. cpr.heart.org. (n.d.). Retrieved February 4, 2023, from https://cpr.heart.org/en/resuscitation-science/cpr-and-eccguidelines/algorithms