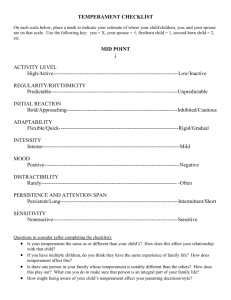
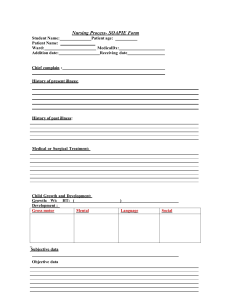
Socio-Demographic Details CP: No: Name: Age: DOB Date of evaluation: Place of residence: Educational Status Address: Source of referral: Information gathered from: a) b) Reliability and Adequacy of information: Identification marks of the patients 1. 2. Presenting Complaints History of Present Illness c) Sex: History of Past Illness (Medical / Psychiatric / Neurological) Family History Diagnosis : Personal History Significant Prenatal History Significant perinatal factors. Developmental History Motor Development: Language Development: Self Help Skills Social Relationships: Peer relationship – a) Special friends: b) Groups: c) Solitary Play: d) Co-operative play: e) Imaginative Play: Quality of peer relationships f) Cordial: g) Confiding: h) Distant: Parenting (Mention Father and Mother Separately) i) Permissive, Restrictive, Accommodating: ii) Communication: iii) Criticism, hostility, rejection: iv)Encouraging, Supportive, nourishing: Any other relevant information Behavior problems Schooling history: Habits interests and talents Sexual history Physical Status: General Temperament and Personality Attributes Activity level. Rhythmicity (Regularity) of biological functions: Approach or avoidance: Adaptability: Threshold of responsiveness: Intensity of reaction. Quality of mood. Distractibility Persistence Qualitative Analysis: Easy /Difficult / Slow to Warm temperament. Psychological Evaluation Mental Status Examination Initial Observation Attention and Concentration Activity Level Motor behavior Speech and language Ability Cognitive functions (Orientation, Memory, General fund of information and General intelligence) Mood and affect Thought processes Perception Child’s version of the problem 3 wish test Tasks given to the child (Specify) and comments thereon Any other observation or comments such as play room observation.