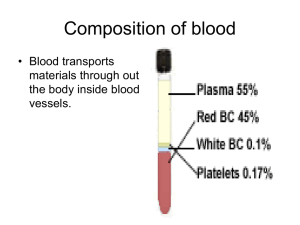
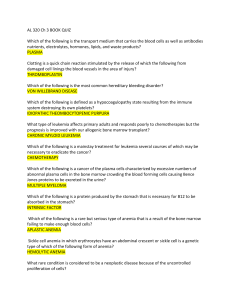
Basic And Cardiovascular Physiology Body Fluid (Blood) Blood is a specialized connective tissue, extracellular body fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. Properties of blood: Volume Color : 7-8% of total body weight. : Arterial blood is bright red due to oxy-hemoglobin but venous blood is dark red due to carboxy- hemoglobin Normal reaction: Slightly alkaline, PH depends on food habits of animal (average PH =7.36-7.45) Taste : Salty Specific gravity: Depends on species animal (average 1.052-1.06) Viscosity : 4.5 times more viscous than water. Osmotic pressure: Average 25mm of Hg. Osmolarity : Average 290-310 mosm/l. Composition of blood: Blood Formed element/cellular element (30-45%) Plasma (55-70%) Solid (8-9%) R.B.C/Erythrocyte W.B.C/Leukocyte Platelets/Thrombocytes Granulocyte Neutrophil Eosinophil Water (91-92) Agranulocyte Basophil Lymphocyte T- Lymphocyte Monocyte B-Lymphocyte Basic And Cardiovascular Physiology Functions of blood Blood performs many important functions within the body including: • Supply of oxygen to tissues (bound to hemoglobin, which is carried in red cells) • Supply of nutrients such as glucose, amino acids, and fatty acids (dissolved in the blood or bound to plasma proteins (e.g., blood lipids)) • Removal of waste such as carbon dioxide, urea, and lactic acid • Immunological functions, including circulation of white blood cells, and detection of foreign material by antibodies • Coagulation, which is one part of the body's self-repair mechanism (blood clotting after an open wound in order to stop bleeding) • Messenger functions, including the transport of hormones and the signaling of tissue damage • Regulation of body pH • Regulation of core body temperature • Hydraulic functions: The restriction of blood flow can also be used in specialized tissues to cause engorgement, resulting in an erection of that tissue; examples are the erectile tissue in the penis and clitoris. Another example of a hydraulic function is the jumping spider, in which blood forced into the legs under pressure causes them to straighten for a powerful jump, without the need for bulky muscular legs . Serum: After coagulation of whole blood the fluid portion is called serum. Plasma: Before coagulation of whole blood the fluid portion is called Plasma. Differences between Plasma & serum Plasma Before coagulation of whole blood the fluid portion is called plasma Fibrinogen present Will clot again/may coagulate Contain different types of cell Serum After coagulation of whole blood the fluid portion is called serum Fibrinogen absent Will not clot again Contain no cell except few Anticoagulant: An agent that prevents or delays blood coagulation. It is used for storing whole blood. 1. 2. 3. 4. 5. Herodin Heparin (0.2mg per ml of blood) Sodium citrate solution Na, K, NH4 salts of oxalate & fluorides EDTA(Ethylene diamine tetra acetic acid) Basic And Cardiovascular Physiology The formation of blood cells Which path is taken is regulated by • The need for more of that type of blood cell which is, in turn, controlled by appropriate cytokines and/or hormones. For example, Interleukin-7 (IL-7) is the major cytokine in stimulating bone marrow stem cells to start down the "lymphoid" path leading to the various lymphocytes (mostly B cells and T cells). Some of the cytokines that drive the differentiation of the "myeloid" leukocytes are • • • Erythropoietin (EPO), produced by the kidneys, enhances the production of red blood cells (RBCs). Thrombopoietin (TPO), assisted by Interleukin-11 (IL-11), stimulates the production of megakaryocytes. Their fragmentation produces platelets. Granulocyte-macrophage colony-stimulating factor (GM-CSF), o Under the influence of granulocyte colony-stimulating factor (G-CSF), they differentiate into neutrophils. o Further stimulated by interleukin-5 (IL-5) they develop into eosinophils. o Interleukin-3 (IL-3) participates in the differentiation of most of the white blood cells but plays a particularly prominent role in the formation of basophils (responsible for some allergies). Basic And Cardiovascular Physiology o Stimulated by macrophage colony-stimulating factor (M-CSF) the granulocyte/macrophage progenitor cells differentiate into monocytes, macrophages, and dendritic cells (DCs). Red Blood Cells (erythrocytes) Shape and size: Biconcave (dog), discoid (ruminant) Diameter : Average 7.8 µm. Volume : 90-95 cubic µm. Color : Red due to containing hemoglobin Composition : Water-65% and solids-35%. Nucleus : no nucleated in mammalian but in camels, reptiles, avis is nucleated. Life span : 120 days. They live about 120 days and then are ingested by phagocyte cells in the liver and spleen. Most of the iron in their hemoglobin is reclaimed for reuse. The remainder of the heme portion of the molecule is degraded into bile pigments and excreted by the liver. Some 3 million RBCs die and are scavenged by the liver each second. Function 1. Red blood cells are responsible for the transport of oxygen and carbon dioxide. 2. It helps to acid- base balance through the buffering action of hemoglobin. 3. It maintains viscosity of blood. 4. It maintains iron balance through special permeability of its membrane. 5. R. B. C is responsible for blood group reactions. Erythropoiesis Erythropoiesis is the process by which red blood cells (erythrocytes) are produced under normal physiological condition. Types of Erythropoiesis 1. Mesoblastic Erythropoiesis: In the early fetus, erythropoiesis takes place in the mesodermal cells of the yolk sac. 2. Hepatic erythropoiesis: By the third or fourth month of fetus, erythropoiesis moves to the spleen and liver. 3. Myeloid erythropoiesis: After seven months of fetus, erythropoiesis occurs in the bone marrow. Increased level of physical activity can cause an increase in erythropoiesis. However, in humans with certain diseases and in some animals, erythropoiesis also occurs outside the bone marrow, within the spleen or liver. This is termed extramedullary erythropoiesis. The bone marrow of essentially all the bones produces RBCs until a person is around five years old. The tibia and femur cease to be important sites of hematopoiesis by about age Basic And Cardiovascular Physiology 25; the vertebrae, sternum, pelvis and ribs, and cranial bones continue to produce red blood cells throughout life. Predisposing factor of erythropoisis Hypoxemia Extensic factor (vit B12) Intensic factor (mucopeptide) Stimulates kidney & liver REF (Renal erythropoieting factor) Globulin ESF (erythrocyte stimulating factor) Bone marrow Erythrocyte Genesis Stem cell in the bone marrow Hemocytoblast Basophilic erythroblast Polychromatophilic erythroblast Normoblast Reticulocyte Erythrocyte Basic And Cardiovascular Physiology Factors affecting the erythropoisis 1. Tissue oxygenation and role of erythropoietin Any condition causing decrease of O2 transport to tissues, stimulate kidney to secrete erythropoietin that stimulate bone marrow to produce red blood cells; increase in red blood cells formation. Examples: High altitudes, Increased demand for oxygen – Athletes, Loss of RBCs – Haemorrhage, Cardio-pulmonary disease – Prolonged heart failure and chronic asthma 2. Healthy bone marrow: Bone marrow is the only site for RBCs production. Destruction by irradiation, chemicals, drugs or bacterial toxins – Lead to deficiency of all blood cells; Aplastic anaemia 3. Healthy liver: Liver is site of Formation of globin portion of haemoglobin. Formation of 10% of erythropoietin. Storage of iron and Vitamin B12. All plasma proteins are produced in liver except gamma (γ) 4. Hormones: Thyroid hormones, androgens and corticoids stimulate erythropoiesis by promoting tissue metabolism 5. Nutritional factors: Cells of bone marrow are of the most rapidly growing and reproducing cells Affected by nutritional state of the person. Nutrients that most important for formation and maturation of red blood cells are: a) Protein: Animal proteins (High biological value protein) Present in liver, kidney and muscles Greater in production of haemoglobin than other proteins. Contain essential amino acids that are neither stored nor formed in body. b) Minerals (Iron, cooper, cobalt): Cofactors in haemoglobin synthesis. Cobalt is a part of vitamin B12 – Stimulating erythropoietin secretion from kidneys. c) Vitamins (B12, folic acid): All vitamins are needed for erythropoiesis. Vitamin B12 and folic acid are mainly needed for final maturation of RBCs because bone marrow cells are among the most rapidly growing and reproducing cells of the body. Vitamin B12 and folic acid are essential for synthesis of DNA. Deficiency of vitamin B12 and folic acid causes diminished DNA synthesis, lead to nuclear maturation failure and division of bone marrow cells. Isotonic solution: Having equal pressure.85% NaCl+H2O - RBC Hypotonic solution: A solution of lower osmotic pressure than another.H2O +5% NaCl Hypertonic solution: A solution of higher osmotic pressure than another. Pure water Basic And Cardiovascular Physiology Hemoglobin Hemoglobin (the red pigment of blood) is the iron-containing oxygen-transport metalloprotein in the red blood cells of all vertebrates.The mammalian hemoglobin molecule can bind (carry) up to four oxygen molecules. Synthesis Hemoglobin (Hb) is synthesized in a complex series of steps. Production of Hb continues in the cell throughout its early development from the proerythroblast to the reticulocyte in the bone marrow. Step-1: Acetic acid is changed into succinyl-CoA in the Kerb’s cycle and then two molecules of succinyl-CoA combined with two molecules of glycin to form a pyrole molecule. HC CH HC CH NH (Pyrole) Step-2: Four pyrole molecules united to form protoporphyrin compound. Step-3: Protoporpyrin combined with iron (Fe) to form heme. This heme compound synthesized from the mitochondria. Step-4: Free ribosome synthesized the globin(polypeptide). Then four heme molecules united with single molecule of globin to form one molecule of hemoglobin. Fig: Structural formula of heme and its combination with globin to form hemoglobin. Basic And Cardiovascular Physiology Hemoglobin Derivatives Oxyhemoglobin: - Hemoglobin combines with oxygen. Carbohemoglobin:-hemoglobin combines with CO2. Carboxyhemoglobin: -hemoglobin combines with CO. Methemoglobin: -hemoglobin combines with O2 but iron remain in the ferric Fe+++) state & it is stable compound.Oxygen can not be removed by exposing the to a vacuum. Sulphaemoblobin: - hemoglobin combines with hydrogen sulphite. It is a stable compound. Nitric oxide hemoglobin: - hemoglobin combines with nitric oxide instead of oxygen.Found in nitric oxide poisoning. Myoglobin: - Myoglobin or muscle hemoglobin is a true hemoglobin composed of heme and globin. Polycythemia (also known as polycythaemia or polyglobulia) is a disease state in which the proportion of blood volume that is occupied by red blood cells increases. Polycythemia vera (PV, PCV) (also known as erythremia, primary polycythemia and polycythemia rubra vera) is a myeloproliferative blood disorder in which the bone marrow makes too many red blood cells. It may also result in the overproduction of white blood cells and platelets. Destruction process of the RBC’s/ Fate of RBC 1. In the spleen, the components of the old destroyed RBC’s are recycled! 2. Fe => Transferrin => Ferritin. In other words, the iron is stored and saved. 3. The globine is converted back into its amino acids which can be used for building other proteins. 4. The heme is processed in a very special manner: 5. The heme is converted, still in the spleen, first into biliverdin which is then converted into bilirubin. 6. This bilirubin then appears in the blood and is bound to the blood transport protein: albumin. Basic And Cardiovascular Physiology 7. This bilirubin is called “free” or “indirect” bilirubin 8. This free or indirect bilirubin is then transported by the blood to the liver 9. This bilirubin is now called “conjugated” (!) or “direct” bilirubin. Whatever its name, this type of bilirubin is secreted into the bile. 10. The bile flows into the intestine, where the bilirubin is converted, by the intestinal bacteria, into urobilinogen. 11. This urobilinogen is absorbed by the blood and either goes back to the liver (to go back to the bile, to make a loop), or excreted by the kidney (as urobilin) or excreted via the stool (as stercobilin). 12. Important; the stercobilin gives the stool its characteristic brown colour. If you don’t have stercobilin, then the stool becomes pale like clay. This is an important diagnostic tool to discover diseases of the gall bladder or the bile duct! Basic And Cardiovascular Physiology Jaundice: - Jaundice is the presence of hemobilirubin or cholibilirubin or both in the circulating blood characterized by yellowish discoloration of mucous membrane especially on the eyes. Anemia Anemia (also spelled anaemia and anæmia; from Ancient Greek: ἀναιμία anaimia, meaning lack of blood, from ἀν- an-, "not" + αἷμα haima, "blood") is a decrease in number of red blood cells (RBCs) or less than the normal quantity of hemoglobin in the blood. WHO's Hemoglobin thresholds used to define anemia (1 g/dL = 0.6206 mmol/L) Classification Morphological classification of anemia: 1. Normocytic normochromic anemia: RBC and Hb are normal size but anemia due to hemolysis or impaired RBC production. 2. Normocytic hypochromic anemia:Anemia is characterized by normal cell but lack of Hb content. 3. Microcytic hypochromic anemia: the cells are smaller than normal. 4. Macrocytic anemia: They are larger than normal. Causes Broadly, causes of anemia may be classified as 1. Impaired red blood cell (RBC) production, ➢ Disturbance of proliferation and differentiation of stem cells ➢ Disturbance of proliferation and maturation of erythroblasts ➢ Other mechanisms of impaired RBC production 2. Increased RBC destruction (hemolytic anemias), ➢ Intrinsic (intracorpuscular) abnormalities: Hereditary, enzymatic difficiency ➢ Extrinsic (extracorpuscular) abnormalities: Antibody mediated, Mechanical trauma. 3. blood loss ➢ Anemia of prematurity from frequent blood sampling for laboratory testing, combined with insufficient RBC production ➢ Trauma or surgery, causing acute blood loss ➢ Gastrointestinal tract lesions, causing a rather chronic blood loss ➢ Gynecologic disturbances, also generally causing chronic blood loss ➢ From menstruation, mostly among young women 4. Fluid overload (hypervolemia). Basic And Cardiovascular Physiology ➢ General causes of hypervolemia include excessive sodium or fluid intake, sodium or water retention and fluid shift into the intravascular space.[23] ➢ Anemia of pregnancy is induced by blood volume expansion experienced in pregnancy. Types of Anaemia There are several types and classifications of anaemia. This is a condition in which the body lacks the amount of red blood cells to keep up with the body’s demand for oxygen. 1. Iron deficiency anaemia: Iron deficiency anaemia is a condition in which the body has too little iron in the bloodstream. 2. Folic Acid Deficiency Anaemia: This form of anaemia is characterised by a lack of folic acid, one of the B group of vitamins, in the bloodstream. 3. Pernicious anaemia: Pernicious anaemia usually affects people between the ages of 50 and 60 and is a result of a lack of vitamin B12. 4. Aplastic anaemia: Aplastic anaemia is caused by an absence or reduction of red blood cells. This can happen through injury where the blood forming tissue in the bone marrow is destroyed. Because of this, the sufferer is unable to fight infection and is likely to be a heavy bleeder. 5. Sickle Cell Anaemia: This form of anaemia is of a hereditary nature and is a result of an abnormal type of red blood cells. Sickle cell anaemia is a life threatening disease and there is no prevention. 6. Hemolytic anemia: This is due to red blood cells being destroyed faster than the bone marrow can produce new ones. The reason for the premature death of red blood cells may be due to the red blood cells themselves (inherited) or because of outside factors. Underlying causes include blood diseases, autoimmune disorders, and certain medications White Blood Cells (leukocytes) White blood cells Basic And Cardiovascular Physiology • • • • are much less numerous than red (the ratio between the two is around 1:700); have nuclei; participate in protecting the body from infection; Consist of lymphocytes and monocytes with relatively clear cytoplasm, and three types of granulocytes, whose cytoplasm is filled with granules. White blood cells or leukocytes (also spelled leucocytes") are cells of the immune system involved in defending the body against both infectious disease and foreign materials. Five[1] different and diverse types of leukocytes exist, but they are all produced and derived from a multipotent cell in the bone marrow known as a hematopoietic stem cell. Function of Leukocyte 1) Phagocytosis: The cell membrane of WBC can engulf particular matter (Bacteria, Virus etc).The ingestion of particular matter is known as phagocytosis. 2) Antibody formation: B-Lymphocyte produces antibody. 3) Fibroblast formation: lymphocytes may be converted into fibroblast, monocyte. 4) Macrophage formation: Monocyte into tissue is called macrophage. 5) Antihistaminic function: Eosinophil release histamine basophils release histamine, bradikinin, serotonin, and lysozomal enzymes that initiate inflammatory response. 6) Prevents intravascular coagulation: Basophil secret heparin which is a powerful systemic anticoagulant. Fixed leukocytes Some leukocytes migrate into the tissues of the body to take up a permanent residence at that location rather than remaining in the blood. Often these cells have specific names depending upon which tissue they settle in, such as fixed macrophages in the liver, which become known as Kupffer cells. These cells still serve a role in the immune system. • • • • Histiocytes Dendritic cells (Although these will often migrate to local lymph nodes upon ingesting antigens) Mast cells Microglia Genesis Agranulocyte Basic And Cardiovascular Physiology Stem cell Lymphoblast Monoblast Prolymphocyte Promonocyte Lymphocyte Monocyte Granulocytes Stem cell Myeloblast Promyelocyte Early neutrophilomyelocyte Early eosinphilomyelocyte Early basophilomyelocyte neutrophilomyelocyte eosinphilomyelocyte basophilomyelocyte neutrophilometamyelocyte eosinphilomyelocyte basophilomyelocyte eosinphil basophil neutrophil Lymphocytes There are several kinds of lymphocytes (although they all look alike under the microscope), each with different functions to perform. The most common types of lymphocytes are • • B lymphocytes ("B cells"). These are responsible for making antibodies. T lymphocytes ("T cells"). There are several subsets of these: o inflammatory T cells that recruit macrophages and neutrophils to the site of infection or other tissue damage o Cytotoxic T lymphocytes (CTLs) that kill virus-infected and, perhaps, tumor cells o helper T cells that enhance the production of antibodies by B cells Basic And Cardiovascular Physiology Although bone marrow is the ultimate source of lymphocytes, the lymphocytes that will become T cells migrate from the bone marrow to the thymus where they mature. Both B cells and T cells also take up residence in lymph nodes, the spleen and other tissues where they • • • encounter antigens; continue to divide by mitosis; Mature into fully functional cells. Monocytes They originate from spleen & bone marrow. Monocytes leave the blood and become macrophages and one type of dendritic cell. Macrophages are large, phagocytic cells that engulf • foreign material (antigens) that enter the body • dead and dying cells of the body. In all animals 5-6%, chicken 8-10% Life span: Few hours to few days. Neutrophils Neutrophils (show ameboid activity) squeeze through the capillary walls and into infected tissue where they kill the invaders (e.g., bacteria) and then engulf the remnants by phagocytosis. Horse, dog, cat, Human = 55-65% Cow, sheep, goat, chicken=25-35% Eosinophils The number of eosinophils in the blood is normally quite low (0–450/µl). However, their numbers increase sharply in certain diseases, especially infections by parasitic worms. Eosinophils are cytotoxic, releasing the contents of their granules on the invader. Basophils Ordinarily representing less than 1% of the WBCs, their numbers also increase during infection. Basophils leave the blood and accumulate at the site of infection or other inflammation. There they discharge the contents of their granules, releasing a variety of mediators such as: • • • histamine serotonin prostaglandins and leukotrienes Which increase the blood flow to the area and in other ways adds to the inflammatory process. The mediators released by basophils also play an important part in some allergic responses such as Basic And Cardiovascular Physiology • • hay fever and an anaphylactic response to insect stings. Platelets Platelets are small, colorless, round or rod-shaped bodies in the circulating blood of mammals produced from megakaryocytes. Blood normally contains 150,000–400,000 per microliter (µl) or cubic millimeter (mm3). This number is normally maintained by a homeostatic (negative-feedback) mechanism. Function: 1. Platelets initiate blood coagulation. 2. Thromboplastin blood coagulation factor. 3. To prevent hemorrhage when blood vessels are injured. 4. They hasten clot intraction. Life span: About 4 days. If this value should drop much below 20,000/µl, there is a danger of uncontrolled bleeding. Abnormalities of the formed elements Polycitomia-Increase RBC than normal in blood. Anemia- Decrease number of RBC or hemoglobin concentration or both in blood. Jaundice- Increase number of bilirubin. Lymphocytosis- Increase number of lymphocyte. Leukemia- More than 30000 of leukocytes. Cancerous growth. Leukopenia- Decrease number of leukocyte in blood. Neutrophilia- Increase number of neutrophil in blood. Neutropenia- Decrease number of neutrophil in blood. Eosinphilia- Increase number of eosinphil in blood. Eosinopenia- Decrease number of eosinphil in blood. Basophilia- Increase number of basophil in blood. Blood Clotting Basic And Cardiovascular Physiology When blood is shed from blood vessels it loses its fluidity and becomes a semisolid jelly like mass is called clot &the phenomenon of the transformation of fluid blood into a jelly like mass is known as coagulation or clotting of blood. A blood clot consists of • • a plug of platelets enmeshed in a Network of insoluble fibrin molecules. Factors of coagulation Factor І Factor ІІ Factor ІІІ Factor ІV Factor V Factor VІ Factor VІІ Factor VІІІ Factor ІX Factor X Factor XІ Factor XІІ Factor XІІІ Fibrinogen prothrombin Thromboplastin Calcium Proacceterin Acceterin Stable factor or proconvertin Antihemophilic factor(AHF) christmas Stuart factor Plasma thromboplastin antecedent(PTA) Hageman factor Fibrin stabilizing factor(FSF) Initiating the Clotting Process Basic And Cardiovascular Physiology There are two processes that can initiate clotting: • • A very rapid process the socalled extrinsic pathway (upper right) and A slower but larger intrinsic pathway (upper left). The Extrinsic Pathway • • • Damaged cells display a surface protein called tissue factor (TF) Tissue factor binds to activated Factor 7. The TF-7 heterodimer is a protease with two substrates: o Factor 9 and o Factor 10 Basic And Cardiovascular Physiology The Intrinsic Pathway • • • • • Factor 12 (also called the Hageman factor) circulates in the blood. If blood escapes into tissue spaces (e.g., as a result of an injury), contact with collagens in the tissue space activates Factor 12. Activated Factor 12 is a serine protease that activates Factor 11 which, in turn, activates Factor 9 which, in turn, activates Factor 10. The Two Pathways Converge • • Factor 10 — produced by either or, more likely, both pathways — binds and activates Factor 5. This heterodimer is called prothrombinase because it is a protease that converts prothrombin (also known as Factor II) to thrombin. Thrombin has several different activities. Two of them are: o proteolytic cleavage of fibrinogen (aka "Factor I") to form: ▪ soluble molecules of fibrin and a collection of small ▪ fibrinopeptides o activation of Factor 13 which forms covalent bonds between the soluble fibrin molecules converting them into an insoluble meshwork — the clot. Why blood does not clot normally within blood vessel? Ans: Smoothness of blood vessel. Rate of blood flow. Presence of some anticoagulant. Physiological properties of intact vascular endothelium Factors that hasten coagulation Factors that hasten coagulation are➢ ➢ ➢ ➢ Increase temperature Gentile agitation Contact with water wettable surface Adding some hemostatic agents ➢ Application of oxidized cellulose gauge, alum, sodium alginate etc. Factors prevent coagulation are➢ Lower temperature ➢ Preventing contact with water settable surface. Basic And Cardiovascular Physiology ➢ By adding decalcifying agents such as oxalates of sodium, potassium, ammonium & fluoride. ➢ By diluting blood to 20 times its volume. ➢ By adding some biological agents such as – heparin, hirudin, snake venom etc. Packed cell volume The hematocrit (Ht or HCT, British spelling haematocrit), also known as packed cell volume (PCV) or erythrocyte volume fraction (EVF), is the volume percentage (%) of red blood cells in blood. It is normally about 45% for men and 40% for women. It is considered an integral part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count, and platelet count. In mammals, hematocrit is independent of body size. Packed cell volume diagram The packed cell volume (PCV) can be determined by centrifuging heparinized blood in a capillary tube (also known as a microhematocrit tube) at 10,000 RPM for five minutes. This separates the blood into layers. The volume of packed red blood cells divided by the total volume of the blood sample gives the PCV. Because a tube is used, this can be calculated by measuring the lengths of the layers. One unit of packed red blood cells will elevate the hematocrit by about 3%. Elevated ➢ Dengue fever, ➢ Polycythemia vera (pv), ➢ Myeloproliferative disorder ➢ Chronic obstructive pulmonary disease (copd) ➢ Dehydrated, ➢ Capillary leak syndrome also leads to abnormally high hematocrit counts, because of the episodic leakage of plasma out of the circulatory system. Basic And Cardiovascular Physiology Lowered ➢ hemorrhage. ➢ anemia Groups of individuals at risk for developing anemia include: • infants without adequate iron intake • children going through a rapid growth spurt, during which the iron available cannot keep up with the demands for a growing red cell mass • women in childbearing years with an greater need for iron because of blood loss during menstruation • pregnant women, in whom the growing fetus creates a high demand for iron • patients with chronic kidney disease, as their kidneys no longer secrete sufficient levels of the hormone erythropoietin, which stimulates red blood cell production by the bone marrow Erythrocyte sedimentation rate The erythrocyte sedimentation rate (ESR), also called a sedimentation rate or Westergren ESR, is the rate at which red blood cells sediment in a period of one hour. It is a common hematology test, and is a non-specific measure of inflammation. To perform the test, anticoagulated blood is placed in an upright tube, known as a Westergren tube, and the rate at which the red blood cells fall is measured and reported in mm/h. The factors responsible for ESR are as follows➢ Fibrinogen, ➢ Viscosity of blood ➢ Certain products of tissue destruction The ESR is increased in Physiological condition ➢ pregnancy, ➢ Oestrus cycle ➢ Muscular exercise after meals Pathological condition ➢ inflammation, ➢ Anemia or rheumatoid arthritis. ➢ Truma ➢ Tuberculosis ➢ Liver disease The ESR is decreased in ➢ polycythemia, ➢ sickle cell anemia, ➢ Allergic condition ➢ Congestive heart failure. The basal ESR is slightly higher in females. Basic And Cardiovascular Physiology Hemagglutination Hemagglutination, or haemagglutination, is a specific form of agglutination that involves red blood cells (RBCs). When blood plasma or serum of one animal is mixed with erythrocytes of another animal agglutination of erythrocytes occur. This process is called hemagglutination.This is an antigen and antibody reaction. It has two common uses in the laboratory: blood typing and the quantification of virus dilutions. 1. Blood Typing Blood type can be determined by using antibodies that bind to the A or B blood group in a sample of blood. For example, if antibodies that bind the A blood group are added and agglutination occurs, the blood is either type A or type AB. To determine between type A or type AB, antibodies that bind the B group are added and if agglutination does not occur, the blood is type A. 2. Viral Hemagglutination Assay Many viruses attach to molecules present on the surface of RBCs. A consequence of this is that at certain concentrations, a viral suspension may bind together (agglutinate) the RBCs, thus preventing them from settling out of suspension. Since agglutination is rarely linked to infectivity, attenuated viruses can therefore be used in assays. Cross-matching Cross-matching (or crossmatching) blood, in transfusion medicine, refers to the testing that is performed prior to a blood transfusion in order to determine if the donor's blood is compatible with the blood of an intended recipient, or to identify matches for organ transplants. Cross-matching is usually performed only after other, less complex tests have not excluded compatibility. Blood compatibility has many aspects, and is determined not only by the blood types (O, A, B, AB), but also by blood factors, (Rh, Kell, etc.). Cross-matching is done by a certified laboratory technologist, in a laboratory. It can be done electronically, with a computer database, or serologically. Simpler tests may be used to determine blood type (only), or to screen for antibodies (only). (indirect Coombs test). Veterinarians also administer transfusions to other animals. Various species require different levels of testing to ensure a compatible match. For example, cats have 3 known blood types, cattle have 11, dogs have 12, pigs 16 and horses have 34. However, in many species (especially horses and dogs), cross matching is not required before the first transfusion, as antibodies against non-self cell surface antigens are not expressed constitutively - i.e. the animal has to be sensitized before it will mount an immune response against the transfused blood. Blood transfusion: Placement of whole blood from one individual to another is called blood transfusion. Basic And Cardiovascular Physiology Purpose: Blood transfusion is primarily to restore the blood volume after severe hemorrhage or in the compensate for an insufficient supply of RBC in various anemias. Blood typing The common technology of blood typing is ABO blood typing. In this method groups of human beings Blood group-A Blood group-B Blood group-AB Blood group-O Blood group-Rh Blood types are mainly based on antigen (agglutinogen) content of erythrocytes May be shown as bellowBlood group A B AB O Presence of agglutinogen in erythrocytes A B A&B No Presence of agglutinin in the serum Anti B Anti A No Anti A & Anti B Basic and Cardiovascular Physiology