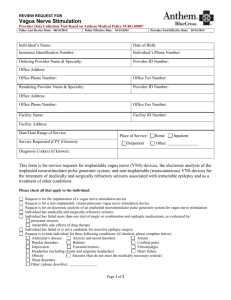
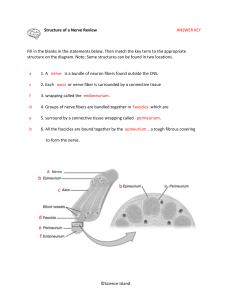
The Vagus Nerve’s Mysterious Role in Mental Health Untangled The healing potential of the brain’s most interconnected nerve intrigues researchers By Jena Pincott edited by Madhusree Mukerjee Investigators have long known that activating the vagus with mild electrical pulses can treat some conditions. In 1997 the U.S. Food and Drug Administration approved a vagus nerve stimulation (VNS) device that can be surgically implanted under the collarbone and linked to a wire wrapped around the nerve. It is widely used to treat cases of epilepsy that do not respond to drugs. In 2005 the FDA certified a similar device for treatment-resistant depression, and the agency approved yet another one in 2021 to speed up recovery from stroke. Gadgets that stimulate the vagus nerve from outside the body, such as at the outer ear or neck, have been cleared in many countries, including the U.S., to treat obesity, pain and migraines. Signaling confidence in the potential of VNS, the National Institutes of Health Common Fund launched a $250-million initiative in 2015 with a second phase in 2022. The program, called SPARC (for Stimulating Peripheral Activity to Relieve Conditions), seeks to map the nerve’s individual fibers and circuits and to illuminate their functions. Scientists hope it will enable them to refine existing treatments and find new therapies for other conditions, ranging from inflammatory bowel disease to long COVID. Clinical trials are underway on so-called transcutaneous VNS (tVNS) devices, which are easier to use because they access the vagus from outside the skin, or cutaneous barrier. These tools potentially could be used to treat rheumatoid arthritis, migraine, lupus and chronic fatigue syndrome— and that’s just a partial list. “A truly revolutionary idea can take 20 to 40 years before it’s thoroughly adopted,” says neurosurgeon Kevin J. Tracey of the Feinstein Institutes for Medical Research in Manhasset, N.Y., “at which point everyone says how we needed that all along.” The vagus vine’s power may be partly mythical, and the research on it is by no means conclusive or clear. But some scientists say it offers hope for millions suffering from complex, hard-to-treat conditions. In 1664 English neuroanatomist Thomas Willis named the longest of the brain’s nerves the vagus, Latin for “wandering.” “We call it the vagus nerve, singular, but there are actually two, one on each side of your body,” Tracey says. Each side has up to 100,000 fibers, and each fiber contributes to a specific function: heart rate, breathing, immunity, gut contractions that help to digest food, even speech. About 80 percent of vagal nerve fibers are afferent, reporting to the brain about the state of the body; the rest are efferent, carrying instructions down from the brain. British physiologist Walter Holbrook Gaskell demonstrated in the late 19th century that afferent signals tend to excite, whereas efferent ones quiet. Concussions Are Remarkably Common and Can Cause Long-Term Problems The first person to zap the vagus with an electric current, using something like a tuning fork pressed against the neck, was American neurologist James Leonard Corning in the 1880s. He was trying to reduce blood flow to the brain to cure epilepsy, but his idea failed. A century later, however, neuroscientist Jacob Zabara of Temple University in Philadelphia found that directly applying an electrical signal to the nerve in a canine could disrupt irregular brain activity, thereby reducing seizures. In 1988 neurologist James Kiffin Penry and neurosurgeon William Bell became the first to implant a VNS device into a human to treat epilepsy. When the vagus nerve brings news of dangerous inflammation in the body, the brain sends down signals to soothe it. The VNS device currently used for epilepsy, which delivers a pulse every few minutes, is a direct descendant of Zabara’s invention. A pivotal study demonstrated that it cut the frequency of seizures by 45 percent on average after a year. It is believed to work mainly by stimulating the afferent fibers, the ones leading up to the brain. The treatment had a remarkable side effect: over time it made people happier. Their mood lightened even if they still had frequent seizures. According to Tracey, when doctors told these patients they could remove the implant, many of them replied, “No, leave it in. It makes me feel good.” This anecdotal evidence prompted the device maker to begin marketing its vagus nerve stimulator as an innovative treatment for depression. The accidental discovery excited a wave of research to figure out exactly how the vagus nerve impacts mood—a wave that has yet to crest. Scientists now know that the vine carries information about heart rate, digestion and, more broadly, the state of the body to many of the brain regions implicated in psychiatric illness. These afferent signals first reach the brain stem’s hub, the nucleus tractus solitarius, which sorts them and passes them on. One recipient is the amygdala, which helps us process emotions, especially fear, anxiety and stress. Another is the hypothalamus, involved in the release of stress hormones such as cortisol. A third is the ventral tegmental area, which plays a central role in our experience of pleasure, motivation and reward. Crucially, the downward signals of the vagus help the body regulate some of its inner activity, such as heart rate, to maintain internal equilibrium. When we encounter a threat, “fight-or-flight” hormones raise our heart rate and blood pressure while curbing activity in the gut and intestines. The vagus nerve detects these changes and reports them to the brain, providing real-time feedback. It also facilitates fine-tuning. When stress signals become excessive, the brain sends messages down the vagus to activate the countervailing “rest-and-digest” system. The vine releases the neurotransmitter acetylcholine at its root tips—in the heart, reducing heart rate and blood pressure, and in the stomach, improving digestion. The system relaxes. A second serendipitous finding, in the late 1990s, showed that the vagus nerve can do much more than calm the body. Researchers in Tracey’s laboratory were studying a drug to reduce inflammation in the brain. Some inflammation is protective, such as the swelling and redness around a wasp sting that show the immune system is dealing with the venom. But inflammation from an overactive immune system can damage tissues. When the body senses an injury or infection, cells in the spleen release signaling molecules called proinflammatory cytokines into the bloodstream to activate the immune response at the site. If cytokines circulate continuously for months or years—from stress, chronic infection or autoimmune disease—inflammation can cause insidious harm. To test their anti-inflammatory drug, the researchers injected mice with a toxin that triggered an immune reaction. But there was a mix-up: instead of injecting the toxin into the brain, a member of the lab injected the mice in the abdomen, causing systemic inflammation. Much to Tracey’s surprise, the anti-inflammatory drug they subsequently delivered into the brain reduced the inflammation in the body. How did that happen? The blood-brain barrier should have prevented the drug from leaving the brain. “We literally talked about this for months,” Tracey recalls. It turned out that the vagus nerve had carried the drug’s signal from the brain deep into the body. https://www.scientificamerican.com/article/how-the-vagus-nerve-could-influence-physical-and-mentalhealth/