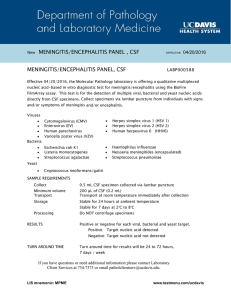
Quiz 3 DeliriumAcute, generally reversible altered state of consciousness with episodic confusion. May be caused by substance abuse, infection, metabolic/electrolyte derangement. DementiaSlow (mostly), progressive decrease in intellectual function without change in consciousness. (Most) are chronic and largely irreversible. Reversible causes: B12/Thiamine, thyroid, infection, tumor, trauma Most common reversible- depression, alcohol dependence, norm pres hydrocep. B12 = megaloblastic anemia / hypersegmented neutrophils, homocysteine Check TSH, B12, RPR Irreversible: Alzheimer, vascular, FTLD/Pick, Parkinson dementia, lewy body, Creutzfeld-Jakob disease Frontal lobe- Impairments of judgement, abstract reasoning, strategic planning, emotional restraint, control of appetite, and continence. Medial temporal lobe, hippocampus, amygdala, limbic systemLeads to disorders of memory and hallucinations. Parietal lobeImpairment of visuospatial skills and integration of sensory inputs leading to sensory agnosias and apraxias. Occipital lobeFailure of visual sensory systems. Temporal neocortexReceptive dysphasia and automatisms. Alzheimer’s disease: Most common type of neurodegenerative dementia. Abnormal deposition of proteins form amyloid plaques and tau tangles. Hyperphosphorylated tau forms crosslinked paired helical filaments. Some have genetic associations (ApoE-4, Presenilin, APP) APP gene on Chr 21 increases risk for patients w/ Down’s syndrome. The insidious progression eventually inhibits ability to perform ADLs. Early episodic memory loss is followed by language, behavioral, and visuospatial deficits. CT/MRI shows medial temporal (hippocampal) and parietal atrophy. Vascular dementia: “Multi-infarct dementia” 2nd most common type of dementia. Caused by ischemic events (multiple lacunar strokes, chronic cerebrovascular disease). Smoking, HTN, DM, lipidemia, CAD, age are all risk factors. Step-wise or progressive decline in cognitive function. Executive dysfunction and focal neurologic deficits may be present. CT/MRI shows multiple infarcts of basal ganglia / periventricular white matter. Rare disease- CADASIL- cerebral autosomal dominant angiopathy subcortical infarcts and leukoencephalopathy, associated w/ NOTCH3 Frontotemporal dementia: “Pick’s Disease” Abnormal amounts or forms of Tau and TDP-43 proteins in the frontal and temporal lobes. Frontal and temporal lobe degeneration; atrophy on CT/MRI Gradual onset, w/ early changes in personality (changes first) and behavior. Onset is often < 65 years old. Two subtypesBehavioral variant FTD- Inappropriate/impulsive behavior, obsession, inattentiveness Primary progressive aphasia- early language deficits Round intraneuronal inclusions of phosphorylated Tau/Pick bodies or ubiquitinated TDP43 Lewy Body dementia: (Parkinsonism AT or AFTER onset of dementia) Abnormal deposits of alpha-synuclein protein called Lewy Bodies. Characterized by dementia w/ a triad of symptoms: Fluctuations in attention and level of arousal Visual hallucinations Parkinsonism #1 risk factor is age Can also have visuospatial/executive dysfunction, as well as REM sleep behavior disorder. Histology shows Lewy bodies (eosinophilic inclusions) primarily in the cortex. Parkinson’s Disease: (without dementia) Neurodegeneration of dopaminergic neurons in substantia nigra. Most cases are idiopathic, rare genetic forms exist. Histology shows alpha-synuclein Lewy bodies (eosinophilic inclusions). Tetrad of presentation is resting tremor, rigidity, bradykinesia, postural instability Motor systems begin unilaterally and progress asymmetrically. Commonly have a shuffling gait and decreased arm swing. Can also have depression, dementia, and REM sleep behavior disorder. Secondary causes include: Drug-induced (antipsychotics, metoclopramide) Cerebrovascular disease Parkinson-plus syndromes Progressive supranuclear palsy, multiple systems atrophy, corticobasal syndrome, Dementia w/ lewy bodies. Huntington Disease: Autosomal dominant, neurodegenerative disorder from CAG repeats in Huntingtin gene on chromosome 4. Number of CAG repeats expand in each generation, with earlier onset and increased disease severity. Onset is usually from 20-50 years of age Patients have Chorea (involuntary dance-like movements) WITH neuropsychiatric symptoms such as personality change, dementia, depression, aggression, psychosis. Some may also experience slowed/absent saccades (eye movements designed to shift the fovea to the object of visual interest), and weight loss. Ensure safe mental status, then do genetic testing and brain imaging CT/MRI shows atrophy of striatum, especially the caudate, w/ enlarged lateral ventricles Creutzfeldt-Jakob Disease: Subacute, rapidly progressive dementia (weeks to months). May have startle myoclonus, ataxia, other movement disorders. Accumulation of infectious prions in the brain (normal prion transforms into beta pleated form which is protease resistant and transmissible). Usually sporadic or acquired from infected beef or surgical instruments. Histology shows spongiform degeneration of cortex w/ accumulated protein, neuronal loss, and astrocytic proliferation. Normal Pressure Hydrocephalus: A potentially treatable form of dementia that is thought to arise from impaired reabsorption of CSF; most commonly affects elderly. Clinical triad is wet, wacky, wobbly (incontinence, magnetic gait, dementia). CT or MRI shows ventriculomegaly out of proportion to parenchymal atrophy. LP has normal opening pressure and can lead to symptom improvement. ______________________________________________________________________ ______________ Cerebellum- does not initiate movement; it contributes to coordination, precision, and accurate timing. AkathisiaAn urgent need to move that is associated w/ patients being treated w/ dopamine receptor blocking agents (DRBA) and patients w/ restless leg syndrome. Can be from Parkinson’s, TBI, or encephalitis. DRBAs: Haloperidol, metoclopramide, risperidone, aripiprazole, etc. TCAs and SSRIs Calcium channel blockers There are 2 distinctive forms of DRBA-induced Akathisia: acute and tardive. Tardive akathisia has late-appearing motor restlessness such as repeated leg-crossing, weight-shifting, or stepping in place. It can be focal or generalized and is often refractory to treatment. Acute akathisia most commonly develops w/ medication changes, and typically lasts less than 6 months. 1st-line treatments include beta-blockers like propranolol. High doses of B6 can help. Benzos are rarely used. Restless leg syndrome: Historical diagnosis more often than physical exam. Dx requires the following: urgency to move legs, unpleasant sensations, relief w/ movement, worsening at night, cannot be attributed to another condition. Associated w/ iron deficiency, chronic kidney disease, thyroid, depression, fibromyalgia, DM, RA, peripheral neuropathy, pregnancy, dialysis, Parkinson’s. Can be a genetic syndrome. Anti-depressants, caffeine, nicotine, and alcohol can make it worse. Try non-drug treatments first. Medical treatments include iron, magnesium, dopamine agonists (Ropinirole, pramipexole, ritigotine patch), anti-seizure (gabapentin enacarbil, gabapentin and pregabalin [for neuropathy]), benzos (clonazepam). Asterixis: Extension of wrists causes a flapping motion from myoclonic lapses in tonic muscles. Can also test by having pt supine with knees bent and feet flat, leaving the knees to fall to the side. Negative myoclonus of the lower limbs at the hip joints may be repetitively observed. Unilateral- focal brain lesion Bilateral- metabolic or drugs (alcohol usually, but sometimes Phenytoin) Hepatic encephalopathy from inability to convert ammonia urea Sometimes benzos, salicylates, barbs, valproate, lithium, gabapentin, metoclopramide. Can also be a result of kidney failure and azotemia ( nitrogen in blood), Wilson’s disease, hypercapnia. Limit alcohol, try laxatives to remove toxins. Tx for Wilson’s is drugs that prevent copper absorption. Athetosis: Inability to maintain a single position in the fingers and toes, tongue, or any part of the body due to a failure of the striatum to suppress unwanted muscle activity d/t a lesion in the Basal Ganglia. Results in a slow snake-like writhing movement particularly in the fingers. Symptoms worsen w/ attempts to control them or improve posture. Can be caused by postnatal hypoxia, head trauma, and perinatal kernicterus; also hepatic encephalopathy and Wilson disease. Treatment focuses on underlying causes. Sometimes anti-dopamine agents or botox injections are used. Hemiballismus: results from neuronal damage in the subthalamic nucleus. Presents w/ violent movements of unilateral arms and legs. Usually lasts 6 to 8 weeks. Most commonly caused by lacunar strokes; can be from anything else that affects the basal ganglia (TBI, ALS, AVM, CA, HIV, demyelination). Treat w/ anti-dopaminergic drugs (risperidone, haloperidol, etc.), benzos (clonazepam), anti-seizure drugs (topiramate), or tetrabenazine. Could also perform posteroventral pallidotomy or administer intrathecal baclofen. Huntington’s Disease: Is a dominant defect, meaning anybody who inherits it will develop the disease. Major loss of medium spiny neurons in the striatum leading to an inability to prevent parts of the body from moving unintentionally. This genetic condition is caused by repeating CAG in HTT gene on chromosome 4, which results in atrophy (ex vacuo ventriculomegaly) of the caudate and putamen losing Ach and GABA. This results in dopamine, GABA, and ACH in the brain; also neuronal death via NMDA-R binding and glutamate excitotoxicity. Patients will develop chorea which are sudden, jerky movements d/t lesions in the basal ganglia. These movements can be random, unpredictable, or continuous. Additional symptoms include athetosis, aggression, depression, and dementia. Symptom onset is between age 20 and 50. There is no cure or way to stop the progression. Symptomatic treatment is all we have: antidepressants, mood stabilizers, and meds attempt to reduce involuntary movements. Syndenham chorea (acute rheumatic fever) in pediatrics: Children with post-streptococcal rheumatic fever can develop chorea w/ tongue darting and milkmaid’s sign (grip w/ wrist flicking) 1-6 weeks after infection. Symptoms usually resolve within 3 weeks-6 months. This affects girls more than boys, and usually ages 515. Autoantibodies attack primarily the basal ganglia, but also the joints, kidneys, and heart. Treatment includes secondary prevention w/ long-term Abx, dopamine-receptor blockers to suppress the chorea, and sometimes short-term immune therapies. Dystonia: Sustained, involuntary muscle contractions that need to be differentiated from tics and athetosis. Often presents w/ writer’s cramp, blepharospasm, and torticollis. Symptoms include one or more repeated postures, persistent or intermittent contractions, abnormal repetitive movements, asymmetrical posture. Can involve one muscle group or multiple. Symptoms may worsen if they try to control muscle movement. Can be caused by CO or hypoxia, infections, heavy metal poisoning. Can also be a symptom of another disorder such as Parkinson’s, Huntington’s, Wilson’s, TBI, birth injury, stroke, or brain tumor. Treat w/ therapy, OMT, or surgery (DBS preferred). *Dystonia w/ Torticollis is treated w/ Botox, or Carbidopa-Levodopa, Trihexyphenidyl and benztropine, Tetrabenazine, deutetrabenazine, diazepam, clonazepam, and baclofen. Myoclonus: Sudden, brief uncontrolled muscle movement or hiccups. It is most commonly d/t a disturbance of the brain or spinal cord, more rarely from injury to peripheral nerves. This can occur by itself or as a result of MS, epilepsy, parkinson’s, alzheimer’s, or creutzfeld-jakobs. Additionally, drug intoxication, metabolic disorders, or hypoxia can cause myoclonus. Positive myoclonus is muscle contraction, negative myoclonus is muscle relaxation. Treat w/ tranquilizers or anti-convulsants. Botox or DBS may be helpful. Tremors: Intention- (rubral, cerebellar, course)Rhythmic, oscillatory, high amplitude tremor during purposeful movement that is d/t cerebellar dysfunction which affects fine motor skills. Can be caused by psych, drugs, CVA, DAI, MS, toxic/metabolic, Wilson’s. Treat the underlying condition, or try botox, Keppra, cannabis, or DBS. EssentialMOST COMMON movement disorder, often genetic. High frequency tremor with sustained posture (ex- outstretched arms). Many patients self-treat w/ alcohol. Treat w/ beta blockers, anti-seizure drugs (primidone, gabapentin, topiramate), benzos (clonazepam), or Botox, therapy, DBS, focused ultrasound. RestingUncontrolled movement of distal appendages, mostly in hands. Tremor alleviates w/ purposeful movement. It is d/t a substantia nigra lesion, which can be caused by neuroleptics, metoclopramide, phenothiazines, Wilson’s, Parkinson’s. Treat underlying cause, medications, surgery. ______________________________________________________________________ ______________ Parkinson’s substantia nigra Hemiballismus contralateral subthalamic nucleus Tremor cerebellum Huntington’s chorea striatum In the basal ganglia, most of the neurons use GABA and inhibit their targets. Their targets may be inhibitory by default; if an inhibitor inhibits an inhibitor, the result is excitatory. Inputs from the cortex and thalamus to the striatum and subthalamic nucleus are glutamatergic, but the outputs from the striatum, pallidum, and substantia nigra pars reticulata all use GABA. Dopamine is used by the projection from the substantia nigra pars compacta to the dorsal striatum and also in the analogous projection from the ventral tegmental area to the ventral striatum (nucleus accumbens). Acetylcholine is used by several external inputs to the striatum. The striatum is made of the caudate nucleus, putamen, and nucleus accumbens, which are all considered input nuclei. Output nuclei send basal ganglia information to the thalamus and consist of the internal globus pallidus (GPi), and the substantia nigra pars reticulata (SNr) Intrinsic nuclei are located between the input and output nuclei, and consist of the external globus pallidus (GPe), the subthalamic nucleus (STN), and the substantia nigra pars compacta (SNc). Parkinson’s disease: Major loss of dopaminergic cells in the substantia nigra pars compacta. Histology shows Lewy bodies composed of a-synuclein (intracellular eosinophilic inclusions). MPTP is a contaminant in illegal drugs that is toxic to the SN and may contribute to the disease. Genetic mutations as a cause do exist but are very rare. Gradual loss of the ability to initiate movement. It has combined hypo and hyper kinetic symptoms that include pill rolling tremor, cogwheel rigidity, akinesia/bradykinesia, postural instability, shuffling gait, and small handwriting. Complications include difficulty thinking, depression, eating/swallowing trouble, sleep disturbance, constipation, anosmia, fatigue, pain, sexual dysfunction, and bladder dysfunction. Treatments include Carbidopa-Levodopa (most effective), dopamine agonists that mimic dopamine, and MAO-B inhibitors (prevent breakdown of dopamine in the brain). Amantadine provides short term relief in early stages and can be combined with levodopa in late stages. COMT inhibitors prolong the effect of levodopa by preventing its breakdown. Anticholinergics like benztropine may be used. DBS has shown good results. *Huntington’s disease: Is a dominant defect, meaning anybody who inherits it will develop the disease. Major loss of medium spiny neurons in the striatum leading to an inability to prevent parts of the body from moving unintentionally. This genetic condition is caused by repeating CAG in HTT gene on chromosome 4, which results in atrophy (ex vacuo ventriculomegaly) of the caudate and putamen losing Ach and GABA. This results in dopamine, GABA, and ACH in the brain; also neuronal death via NMDA-R binding and glutamate excitotoxicity. Patients will develop chorea which are sudden, jerky movements d/t lesions in the basal ganglia. These movements can be random, unpredictable, or continuous. Additional symptoms include athetosis, aggression, depression, and dementia. Symptom onset is between age 20 and 50. There is no cure or way to stop the progression. Symptomatic treatment is all we have: antidepressants, mood stabilizers, and meds attempt to reduce involuntary movements. *Syndenham chorea (acute rheumatic fever) in pediatrics: Children with post-streptococcal rheumatic fever can develop chorea w/ tongue darting and milkmaid’s sign (grip w/ wrist flicking) 1-6 weeks after infection. Symptoms usually resolve within 3 weeks-6 months. This affects girls more than boys, and usually ages 515. Autoantibodies attack primarily the basal ganglia, but also the joints, kidneys, and heart. Treatment includes secondary prevention w/ long-term Abx, dopamine-receptor blockers to suppress the chorea, and sometimes short-term immune therapies. *Wilson’s disease: Caused by mutations of the ATP7B gene which is important to control removal of copper from the liver to the bile to be excreted via the intestines. Patients may become confused and have various disorders ranging from depression to schizophrenia, leading to personality and behavioral changes. Within three years they will develop Kayser-Fleischer rings in the corneas which are brown/yellow. In females, menstruation may cease or never start. Miscarriages and infertility are common. Neurologic symptoms may include tremor, difficulty speaking and swallowing, lack of coordination, spasticity, and muscle rigidity. Other signs include renal stones, renal tubular damage, arthritis, osteoporosis, and osteophyte formation in joints. *Serum blood will have ceruloplasmin Urine will have copper. Tourette’s disease: Sudden, rapid, repetitive, unwanted movements or sounds called tics. Most cases are caused by a combination of gene variations and environmental factors. Twin studies suggest that it is an inherited disorder, and may be linked to genes SLITRK1, NRXN1, CNTN6. Males are more likely to have tics, females are more likely to have OCD symptoms. To diagnose, must have both motor and vocal tics for at least 1 year, w/ onset prior to age 18. Imaging can be performed to rule out other causes. Simple tics are sudden and brief and involve a limited number of muscle groups. Complex tics are distinct, coordinated patterns involving several muscle groups. The most common Tourette’s comorbidities are ADHD, OCD, anxiety, learning disabilities, behavioral problems, sleep disruption, social skill deficits, and sensory processing issues. Treatments include medications that block dopamine, alpha agonists, stimulants to lessen ADHD, antidepressants, behavioral treatments, and psychotherapy. ______________________________________________________________________ ______________ Delirium- abrupt onset of reduced orientation characterized by a fluctuating course, PLUS an additional disturbance that can include inattention, disorganized thinking, and altered LOC, language, visuospatial ability, perception, sleep, emotional, hyper/hypo activity. “Waxing & waning” = delirium. It is transient, and usually reversible. Dx is via clinical judgement; it is often a medical emergency. Labs and imaging MAY reveal an organic cause. It can be caused by drugs, electrolytes, “lack” of drugs, infection, reduced sensory input, intracranial process, urology or GI, or myocardial/pulmonary problem. AVOID anticholinergic drugs if patients are at high risk of delirium. Medications that are NOT recommended to prevent delirium include Haldol, atypical antipsychotics, dexmedetomidine, statins, and ketamine. Delirium triage scale has two components: Do they have an altered LOC? Can they spell LUNCH backwards w/o making more than 1 mistake? Dementia- A gradual (usually) neurodegenerative process; attention affected much later. risk if APO-E-E4, female, old, HTN, DM, trauma, lipids, homocysteine. Patients often have “anosognosia” inability to recognize their disorder. Aducanumab may slow progression by reducing amyloid plaque in the brain. Mild cognitive impairment is 1-2 SD from normal on formal cognitive testing. Dementia is > or = to 2 SD from normal on formal cognitive testing. Cannot be d/t delirium or another mental disorder (depression/schizo, etc.) Degenerative: Alzheimer’s, Frontotemporal, Lewy body, Huntington, CTE, prion, MS, ALS, Wilson Frontotemporal has circumscribed atrophy, pick bodies, early personality change Lewy body dementia comes w/ early visual hallucinations Vascular: Vascular dementia, cognitive impairment Lesions on CT/MRI in white and gray matter, stepwise Other: Neoplasm/paraneoplastic, metabolic, psychiatric, NPH, NOS, SLE, Syphilis, vitamins Other meds to Tx/prevent dementia: Cholinesterase inhibitors- donepezil, rivastigmine, galantamine NMDA antagonists- memantine None of these are useful for mild cognitive impairment. Antipsychotic meds for hallucinations, delusions, agitation: *Black box warning for risk of CVA Haldol- risk of tardive dyskinesia Risperidone- extrapyramidal symptoms Olanzapine- metabolic effects (DM), otherwise well tolerated Quetiapine- sedation, transient orthostasis Other meds for hallucinations, delusions, agitation: *Not FDA approved for this Anti-depressants- sertraline Anticonvulsants- valproate, carbamazepine Beta blockers- propranolol Anxiolytics- clonazepam, lorazepam *Benzos can cause excess sedation, unsteady gait, confusion, and paradoxical agitation. Meds to Tx sleep disturbances: Trazodone- caution in men (giant unwanted erections that last too long) Quetiapine- if insomnia is accompanied w/ agitation AVOID zolpidem ______________________________________________________________________ ______________ Parkonsonism: Movement disorders that result from degeneration of substantia nigra; indirect pathway becomes overactive w/ increase of glutamatergic activity. GABA and Dopamine are inhibited, Acetylcholine is stimulated. Parkinsonism can be drug-induced (DIP): Antipsychotics (D2 antagonists) and antiemetics If you stop these drugs that cause the DIP PD symptoms diminish within 6 months. Damage from DIP is more symmetric than Parkinson’s disease. MPTP (Synthetic heroin derived from meperidine) is oxidized to pyridinium ion (MPP+) resulting in neuronal death in hours to days. The PD symptoms that result from this are irreversible. Dopaminergic neurons will continue to generate for years even after stopping the use of synthetic heroin. Dopamine precursorsLevodopa can enter the brain via L-amino acid transporters, where they are decarboxylated to dopamine. It is more effective in early-stage PD. Benefits decline after a few years of use. If given alone, it is decarboxylated in the periphery and absorbed in the small intestine Only 1-3% will reach the brain. ADRs when given alone: - N/V, anorexia, arrhythmias, hypotension (d/t peripheral metabolism) -L-dopa-induced dyskinesias (choreoathetosis of face and distal extremities) If severe, tx w/ Amantadine and Clozapine -“Off periods” may have marked akinesia- rescue w/ Apomorphine SubQ -Behavioral/psych disorders, punding (complex, repetitive, non-goal-oriented activity) Drug Interactions: -HTN crisis may occur if given w/ non-selective MAOIs (MAO-A inhib) or sympathomimetics -Avoid taking antiemetics (can worsen PD) -Pyridoxine (Vit B6) increases the peripheral breakdown of L-dopa -Antipsychotic drugs that block dopamine receptors (Can use atypical antipsychotics instead- like Clozapine) Contraindications: Patients w/ psychosis, closed-angle glaucoma, cardiac disease, active GI bleeding, hx/suspected melanoma DOPA decarboxylase inhibitors (DDCIs)Carbidopa is a peripheral dopa-decarboxylase inhibitor that does NOT cross the BBB. Combining Levodopa and Carbidopa together peripheral metabolism of L-dopa, which the plasma level of L-dopa more is able to get to the brain, and you can lower the daily dose of L-dopa needed to achieve the desired effects. Immediate release formulations- Dhivy, Parcopa Controlled/Extended release- Sinemet, Rytary Implanted pump- Duopa Inhalation powder- Inbrija Inhibition of dopa-decarboxylase leads to compensatory activation of COMT (CatecholO-methyltransferase), which converts L-dopa to 3-OMD (3-O-methyldopa), which causes a poor therapeutic response to the L-dopa; this is because 3-OMD competes for the same active carrier that is needed for L-dopa absorption and distribution across the BBB. The solution is to administer a selective COMT inhibitor. COMT-inhibitors (Catechol-O-methyltransferase inhibitors)Entacapone is the preferred because it does not cross the BBB, and it does not cause acute hepatic failure like Tolcapone does. -Triple combination therapy (Stalevo) is a formulation of Levodopa, Carbidopa, and Entacapone, which results in greater symptomatic benefit than carbidopa-levodopa alone. ADRs: -Earlier and more frequent dyskinesia -N/V/D, dizziness, drowsiness, headache, dry mouth MAO-B inhibitorsSelegiline is a selective and irreversible MAO-B inhibitor that slows that biotransformation of dopamine. Used as an adjuvant to enhance and prolong the effect of L-dopa. Rasagiline is a selective and irreversible MAO-B inhibitor that is 5x more potent than Selegiline in preventing DIP. It is used early as monotherapy for patients w/ mild PD symptoms. It can be used as an adjuvant w/ carbidopa-levodopa. Safinamide is a selective and irreversible MAO-B inhibitor used to decrease off-period fluctuations. It is used as an adjuvant w/ carbidopa-levodopa to reduce fluctuations. ADRs and Contraindications for ALL of the above listed MAOIs: -Do not take any other MAOIs when taking 1 of these 3 drugs -High doses also inhibit MAO-A -L-dopa w/ a combined inhibitor can cause HTN crisis d/t peripheral NE -TCAs or SSRIs can cause serotonin syndrome -May cause insomnia (metabolites include amphetamine) -Confusion, dyskinesia, psychiatric toxicity, hallucinations -Do not take dextromethorphan or ANY OTC cold-medicine Dopamine receptor agonistsThese act directly on postsynaptic dopamine receptors and are 1st-line therapy in younger patients w/ less severe PD. They may delay the need to use levodopa in early PD, and may decrease the necessary dose of levodopa in advanced PD. When used in patients who are taking L-dopa, it helps to control fluctuations and prevent adverse effects in those who are becoming tolerant to L-dopa. *In patients who have never responded to L-dopa, these drugs typically do not work. Pramipexole targets the D3 receptor and can be monotherapy for mild PD or an adjuvant to treat L-dopa fluctuations. May be neuroprotective. Ropinirole targets the D2 receptor and can be monotherapy for mild PD or an adjuvant to treat L-dopa fluctuations. Rotigotine targets the D3 receptor and is well-tolerated, and available as a skin patch. ADRs and Contraindications: -GI effects and bleeding ulcers -CV arrhythmias, valvulopathy, vasospasm, hypotension, peripheral edema -Dyskinesias -Mental disturbances, poor impulse control -Dopamine agonist withdrawal syndrome if abruptly stop taking -Sleep attacks (pramipexole/ropinirole) -Do NOT take if hx of psychotic illness, recent MI, or active GI bleeding Apomorphine is potent and broad-spectrum dopamine agonist, targeting D1, D2S, D2L, D3, D4, D5. It must be given SubQ or SL d/t extremely high phase-2 first-pass metabolism. It is very lipophilic and concentrates highly in the brain. It is used as a rescue-agent for patients experiencing on/off fluctuations and akinesia during chronic levodopa therapy. Doses must be administered at least 2 hours apart. ADRs and Contraindications: -N/V/D (can pretreat w/ antiemetics), constipation -Dyskinesias, drowsiness, insomnia, chest pain, sweating, hypotension, syncope -Mental or behavioral disturbances -Do not take if patient is taking Serotonin 5-HT3 antagonists I HAVE QUESTIONS ABOUT THIS…. Basically…. Yes, use antiemetics… but make sure they are not 5-HT3 antagonists. AnticholinergicsBenztropine and Trihexyphenidyl block muscarinic acetylcholine receptors. Used as an adjuvant for patients on L-dopa or dopamine agonists who still have tremors. Can be used as monotherapy for patients under 70 who have little or no bradykinesia or gait issues and have only tremors and rigidity. They have a lower efficacy than L-dopa; are designed to correct the imbalance in dopamine/acetylcholine activity. They help tremor and rigidity, but not bradykinesia. ADRs and Contraindications: -Urinary retention, impaired sweating, blurred vision, tachycardia, dyskinesias -Increased intraocular pressure -Xerostomia/dry mouth -Nausea and constipation (interferes w/ peristalsis) -Do not give to patient with: Cognitive impairment, prostatic hyperplasia, pyloric stenosis, tachycardia, tardive dyskinesia Antiviral agent Amantadine is an antiviral agent w/ weak anti-parkinsonism properties. It potentiates dopaminergic functions by influencing the synthesis, release, or reuptake of dopamine. It is an antagonist of adenosine A2A receptors and NMDA-type glutamate receptors. Available as immediate-release Symmetrel, or extended-release Gocovri or Osmolex. It is used in patients w/ advanced PD taking L-dopa to decrease dyskinesias, or as short-term monotherapy for mild PD to reduce bradykinesia, rigidity, and tremor. ADRs and Contraindications: -Restlessness, behavioral, depression, sleep, confusion -Peripheral edema without cardiac, hepatic, or renal disease -Livedo reticularis (blood vessel spasms that cause mottling of the skin) -Do not use in patients w/ hx of seizure, heart failure, or renal disease Alzheimer’s: Accumulation of amyloid beta protein plaques, formation of neurofibrillary tangles, loss of cortical neurons (cholinergic). Acetylcholinesterase inhibitorsBreak down acetylcholine into acetic acid and choline improves cholinergic transmission. The following drugs are more selective for AChE in the CNS than in the PNS. Donepezil (nothing mentioned in lecture about this, other than ADR listed below). Galantamine augments the action of acetylcholine on nicotinic receptors in the CNS. Rivastigmine is the only AChE inhibitor available as a skin patch, and it has no interaction with drugs that alter activity of CYP450 enzymes. ADRs and Contraindications: -GI -Bradycardia and hypotension -Sleep disturbances and vivid dreams (mostly w/ donepezil) -Do not use if patient has known bradycardia or cardiac conduction disease NMDA receptor antagonistsN-methyl-D-Aspartate is an excitatory glutamate receptor that allows calcium into neurons too much of this can be neurotoxic; causes neurodegeneration and apoptosis. Memantine is an uncompetitive NMDA antagonist used for moderate to severe Alzheimer’s which blocks the receptor and decreases calcium influx. It is used as combination therapy with an AChE inhibitor (donepezil + memantine). ADRs and Contraindications: Headache, dizziness, drowsiness, constipation, HTN, SOB Monoclonal antibodiesmAbs target the aggregated Amyloid beta proteins in the brain. Decreasing amyloid beta reduces the rate of disease progression and slows cognitive and functional decline. Lecanemab is covered by medicare and has been shown to reduce amyloid plaque. It is given IV, but patients are monitored for ADRs. Donanemab was recently approved and is also given IV. ADRs and Contraindications: -Brain bleeds -Amyloid related imaging abnormalities (ARIA) Amyotrophic Lateral Sclerosis: Progressive degeneration of motor neurons, resulting in inability to initiate or control muscle movement. 90% of cases are spontaneous, 10% is familial. Average life expectancy is 2 to 5 years from diagnosis. Death occurs from respiratory failure or complications from immobility. Riluzole inhibits release of glutamate, blocks NMDA receptors and Na+ channels which is thought to protect (neuroprotective) motor neurons from glutamate-induced excitotoxicity. It prolongs the time before patients require respiratory support and may extend life for a few months. Edaravone is a free-radical scavenger that reduces oxidative stress. It slows functional deterioration in early ALS. It is available IV or oral. Tofersen is an antisense oligonucleotide that binds mutated SOD1 mRNA, preventing toxic SOD1 proteins from being made. This drug is for ALS associated w/ a mutation in superoxide dismutase 1 (SOD1-ALS) which is found in 20% of familial ALS cases. This mutant gene causes protein misfolding which aggregates within motor neurons and astrocytes. It is available as an intrathecal injection. Baclofen is a GABAB receptor agonist that is a muscle relaxant and antispasmodic that acts on spinal cord nerves and decreases the frequency and severity of muscle spasms. Gabapentin is an antiepileptic that modulates the glutamatergic system and is used to slow decline in muscle strength. Huntington’s disease: It is an autosomal dominant inherited disorder characterized by chorea and dementia which affects movements, cognition, and mental health. It also caused rhythmic movements of the tongue and face, as well as mental deterioration. Chorea is a result of imbalanced dopamine, Ach, and GABA overreaction of dopaminergic neurotransmission. Average life expectancy is 15-18 years. Death results from progressive respiratory depression. Dopamine receptor blockers (phenothiazines) and other antipsychotics can produce improvement in motor function and psychosis. Drugs that deplete central monoamines (reserpine) can alleviate chorea. Tetrabenazine was the 1st drug approved to treat HD. It is a synaptic vesicular amine transport inhibitor that reversibly binds the human vesicular monoamine transporter type 2 (VMAT2), resulting in decreased uptake of monoamines into synaptic vesicles; it suppresses chorea. ADRs and Contraindications: -Adjust dose for poor metabolizers or rapid metabolizers -Can cause drowsiness, depression, nausea, anxiety/agitation Haloperidol, fluphenazine, olanzapine are D2 receptor blockers that can suppress movements by modulating dopamine function. Deutetrabenazine is a selective inhibitor of VMAT2 that modulates dopamine stores. It is as effective as tetrabenazine and has fewer side effects. It is metabolized by CYP2D6. ADRs and Contraindications: - Adjust dose for poor metabolizers or rapid metabolizers -Agitation, restlessness, parkinsonism, sedation, dry mouth, diarrhea, insomnia, fatigue -QT prolongation -Do not use if on MAOIs, reserpine, tetrabenazine -Do not use if severely depressed or suicidal ______________________________________________________________________ ______________ CNS Infections I, II, III Normal CSF values Opening pressure 15mmHg or 150-200mmH2O WBC 0-5, Protein < 40, Glucose 40-70 Part 1- Acute Meningitis How does it spread? There are no lymphatics in the brain… so it must be hematogenous (blood), or colonization (usually via respiratory tract). It must be able to cross the BBB Choroid plexus is more permeable than the rest of the CNS vasculature Some follow endothelial cells Can be direct contiguous following head trauma, sinusitis, or otitis media Can be neural route via peripheral nerves (rabies) or olfactory (HSV1/N fowleri) Can be via direct implantation from neurosurgery or medical devices Acute septic = bacterial Symptoms in hours-days neutrophils in CSF (neutrophilic pleocytosis) Aseptic = usually viral Symptoms in hours-days mononuclear cells in CSF (lymphocytic pleocytosis) Chronic = fungal or TB Insidious onset of several weeks Chronic, granulomatous inflammatory disease mononuclear cells in CSF Usually from mycobacterium, fungi, or parasites Patient is often immunocompromised Bacterial: Mycobacterium tuberculosis, Treponema pallidum (neurosyphilis), Fungal: Cryptococcus neoformans Meningitis: inflammation of the meninges from infectious or non-infectious cause. Encephalitis: inflammation of the brain parenchyma w/ altered LOC, seizures, confusion Usually viral Meningoencephalitis: Both meningeal and encephalitic symptoms Viral, bacterial, or parasitic Common causes of meningitis: Less than 1 month oldBacterial: GBS (most common), Listeria, Ecoli K1 Viral: HSV-2, HSV-1 1-23 months oldBacterial: S pneumo, N meningitidis, H influenzae, GBS, Ecoli K1 Viral: Enteroviruses, Arboviruses, HIV (early upon infection) 2-50 years oldBacterial: S pneumo, N meningitidis Viral: Enteroviruses, Arboviruses, HIV (early upon infection) Over 50 years oldBacterial: S pneumo, N meningitidis, Listeria, Ecoli, Klebsiella, Pseudomonas Viral: Enteroviruses, Arboviruses, HIV (early upon infection) Case: 10-month-old female to ER w/ fever, lethargy, recent cold. Immunizations not UTD. Temp 40C, HR 130. Nuchal rigidity, + Kernig and Brudzinski. No focal deficits. WBC 3,000 w/ 98% neutrophils, CSF opening 300, Protein 160, Glucose 15 *10-month-old unvaccinated, given above info bacterial via nasopharynx Empiric therapy = Vanco + Ceftriaxone Management of Acute Septic Meningitis in childrenSuspicion LP and cultures empiric Abx redirect therapy based on results If LP contraindicated: blood cultures empiric Abx CT if negative, do LP continue based on results < 1 month old: Most common pathogensViruses, GBS (most common), Ecoli, Listeria monocytogenes Empiric therapyAmpicillin + cefotaxime, Ampicillin + aminoglycoside (Ex: gentamicin) 1-23 months old: Most common pathogensViruses, Pneumococci, N meningitidis, GBS, Ecoli K1, H influenzae Empiric therapyVancomycin + 3rd gen cephalosporin (ceftriaxone) 2-50 years oldMost common pathogensViruses, Pneumococci, N meningitidis Empiric therapyVancomycin + 3rd gen cephalosporin (ceftriaxone) Over 50 years oldMost common pathogensViruses, Pneumococci, N meningitidis, Listeria monocytogenes, Klebsiella, Ecoli Empiric therapyVancomycin + 3rd gen cephalosporin (ceftriaxone) + Ampicillin Not testable right now- but understand why dexamethasone is added to tx plan. Know which pathogens can be cultured on the following media: Blood agar Chocolate agar Thayer Martin agar Mueller-Hinton agar Know the uses for India ink, PCR/rtPCR, latex agglutination Streptococcus pneumoniae: *Gram + diplococci, catalase negative, alpha hemolytic, encapsulated, secretes pneumolysin to enter tissue and evade phagocytosis. *Widespread Abx resistance *Is a leading cause of pneumonia, meningitis, sepsis CAN use penicillin if you identify that it is a non-resistant strain; otherwise Vanco + 3rd generation cephalosporin. Grows on blood agar, or brain-heart infusion Case: 10-month-old female to ER w/ fever, lethargy, recent cold. Immunizations not UTD. Temp 40C, HR 130. Nuchal rigidity, + Kernig and Brudzinski. No focal deficits. CSF stain shows Gram- coccobacilli that does not grow on blood agar, except as satellite colonies around S aureus (b/c S aureus is B-hemolytic and breaks RBCs). Tiny colonies grew on chocolate agar which provides factors X and V. Also grew on Thayer Martin. Dx: Haemophilus influenzae B which is encapsulated and Gram- w/ LPS Tx: 3rd generation cephalosporin This infection could likely have been prevented w/ an HiB conjugate vaccine Polysaccharide-only vaccine only stimulates short-lived IgM w/o memory Conjugate vaccines stimulate IgG and B memory cells Grows best on chocolate agar Case: Gram-, encapsulated, oxidase-positive, aerobic diplococcus- N meningitidis Most important serotypes: A, B, C, Y, W-135 IgA protease breaks down mucosal IgA, capsule evades phagocytosis, LPS is an endotoxin, Pillin proteins allow colonization to nasopharyngeal epithelium. This can result in severe sepsis w/ DIC petechial rash that progresses to a pupuric rash (bleeding into skin). LPS and LOS result in activation of cytokines, complement, coag cascade Fever, perfusion, hypotension, death Most commonly on Chocolate agar or Mueller-Hinton agar, but also on Thayer Martin. Fermentation of glucose and maltose, but not sucrose. Oxidase positive Tx w/ penicillin, alternatively ceftriaxone or cefotaxime Close contacts should be prophylactically tx w/ rifampin or cipro. GBS (S agalactiae): Gram+ cocci, beta hemolytic, may need CAMP test for detection. Frequently colonized female GI/GU tract. Most common cause of neonatal bacterial meningitis. Blood agar Listeria monocytogenes: Gram+ rods, beta hemolytic, can grow in cold temperatures (refrigerators/meat/cheese) Can cause meningitis in pregnant women, neonates, elderly, immune patients. Mueller-Hinton agar E.coli: Gram- bacilli, aerobic Is a common cause of neonatal meningitis, BUT NOT the most common. Case: 2-week-old girl w/ 1 day of irritability, fever, vomiting, anorexia becoming lethargic. Illness was preceded by 2 days of respiratory illness. Temp 39C, conjunctival injection, bulging fontanelle, erythema of posterior pharynx. This age group is most commonly GBS, but it could be listeria, Ecoli, viral (HSV2 etc)…. You analyze her CSF and it shows WBC 350 w/ 75% lymphocytes and normal glucose. PCR suggests Echovirus type 11, which is an Enterovirus (Echo, coxsackie, polio, etc.). Enteroviruses cause 85% of viral meningitis. Part 2- Acute Encephalitis and Myelitis Encephalitis: inflammation of the brain parenchyma w/ altered LOC, seizures, confusion Usually viral Mild to profound lethargy, confusion, somnolence, seizure, coma, hallucinations, agitation, personality changes, behavioral disorders. May have neurologic signs such as ataxia, hemiparesis, myoclonic jerks, cranial nerve deficits. Encephalitis + meningitis = meningoencephalitis Encephalitis + myelitis = encephalomyelitis Myelitis = spinal cord inflammation w/ limb weakness Most common causes of encephalitis: HSV-1, Arboviruses, Enteroviruses Less common causes in immune-competent: N fowleri, Rabies Causes in immune-compromised: Toxoplasma, HIV, JCV Types of encephalitis: Acute- most often viral Subacute (insidious)- HIV, JCV, Toxoplasma Post infectious- immunologic (rare, often demyelinating; Ex: subacute sclerosing panencephalitis) Slow- Prion HIV most commonly affects the temporal lobe. CSF findings include pleocytosis, w/ protein and glucose similar to viral meningitis. Viral-specific IgM may be found (Arboviruses)- use PCR/rtPCR. Case: 9 yom, fever w/ right sided headache. Swam in farm pond 3 days ago. Following day became drowsy w/ stiff neck. LP suggested meningoencephalitis. Mobile amoebas were seen on wet mount of CSF. Became unresponsive 2 days later. CT showed lesion in right frontal lobe and diffuse edema. Child died. N fowleri found at autopsy. N fowleri is an amoeba that lives in fresh water that causes rapidly progressive, fatal meningoencephalitis. There is NO approved treatment, although amphotericin has shown some limited success. Case: 60 yof brought to ER after a seizure. 2-day hx of fever and 1-day hx of lethargy. PE shows nuchal rigidity. Seizure suggests encephalitis, nuchal rigidity suggests meningitis. Patient was dx w/ encephalitis and admitted. Blood cultures obtained, empiric therapy Acyclovir was initiated (always do this when thinking encephalitis d/t HSV1/2, VZV). MRI and CT revealed no masses. MRI did reveal temporal lobe lesion, CSF showed lymphocytic pleocytosis, normal glucose. PCR revealed HSV-1 DNA. *HSV-2 is more associated w/ meningitis *HSV-1 is more associated w/ encephalitis *VZV causes post-herpetic neuralgia HSV-1 is the most common cause of fatal, sporadic encephalitis; despite occurring yearround and not having any age, sex, or immunosuppression risks associated w/ it. Symptoms begin in hours to days; fever, headache, behavioral changes, and seizures are the most common. The virus ascends the olfactory or trigeminal nerve to the brain, replicates, and causes necrosis of brain parenchyma. It is best diagnosed by PCR of CSF. Treatment is acyclovir; 70% mortality if untreated. Arbovirus from mosquitos usually presents as meningoencephalitis, however West Nile causes encephalomyelitis (myelitis component includes severe muscle weakness) (West Nile is the most common arbovirus in the USA). Eastern equine encephalitis virus is rare, but it is the worst (mortality 70% in the elderly). St Louis encephalitis virus also causes meningoencephalitis; the dead-end host is ONLY HUMANS, instead of both humans and horses like the others. LaCrosse virus “California encephalitis” usually causes mild symptoms, except in children- it causes seizures; also, the reservoir is rodents instead of birds. Case: 10 yom to ER w/ 2-day hx of fever and headache. Diagnosed w/ non-specific viral illness and sent home. Came back 2 days later w/ fever, paresthesia of the right scalp and arm, dysphagia, disorientation, and ataxia. Admitted for encephalitis. CSF WBC 226, glucose 69. IgG and IgM for Arboviruses were negative, PCR for HSV-1 and rtPCR for Enteroviruses were negative. rtPCR for Rabies was positive. Over the next 10 days he deteriorated and died. Major rabies reservoirs in wildlife in USA: Bats, raccoons, skunks, fox Domestic animals not usually involved d/t vaccination. Domestic animals internationally are much more commonly infected d/t lack of vaccines. Africa India Asia Usually rabid dogs Before death: rtPCR of CSF, antibodies in CSF, antigen detection in nerve endings of skin biopsy After death: Rabies antigen or RNA in brain, presence of negri bodies Rabies prophylaxis/treatment: Day 0- immune globulin in 1 site, active vaccine in another site Days 3, 7, 14- active vaccine Myelitis: Inflammation of the spinal cord, w/ flaccid limb weakness similar to poliomyelitis. Has been associated with Enteroviruses, especially Enterovirus D68, but West Nile can also cause myelitis. Case: 10 yom w/ asthma to ER w/ 3-day hx of fever, sore throat, cough , dyspnea. Rapid strep was negative. The following day he developed left arm weakness that progressed to his right arm, then both legs. 2 days later he was unable to walk. He was admitted for myelitis. Respiratory, stool, and CSF samples were analyzed via PCR and cultureEnterovirus D68 was isolated from his respiratory secretions. It is transmitted via respiratory droplets, replicates in respiratory tract, enters blood after alveoli, viremic spread to spinal cord either directly OR retrograde via motor neurons. E-D68 causes severe respiratory illness in asthma patients. Flaccid myelitis occurs rapidly in hours to days, typically in children around 6 years old. Weakness can spread to respiratory muscles and trunk. Treatment is supportive care +/- intubation, there is no vaccine. Part 3- Chronic, Opportunistic, Prior Infections Cryptococcus neoformans, HIV, JCV, Toxoplasma gondii Immune-suppressed patients are most at risk for “opportunistic” infections. Transplant, cancer, steroids, anti-TNF, taking anything that ends in “mab/umab”, HIV/AIDS Case: 42 yof w/ leukemia has worsening headache, N/V for the past week. Didn’t come to ER at first thinking it was just from cancer drugs. Then brought to ER by spouse for confusion and lethargy. CSF exam shows slightly decreased glucose, 10 mononuclear cells. Yeast were seen w/ India ink stain. Dx was made w/ latex agglutination test: C neoformans C neoformans is a monomorphic yeast that makes a thick polysaccharide capsule once inhaled (virulence factor), then it evades phagocytosis. It replicates in meninges, stimulates inflammation increasing ICP symptoms of meningitis. It is found in the soil or in pigeon shit. It does not spread person-to-person. It is best detected by latex agglutination test of antigen in serum or CSF, or by using India ink stain. It can alternatively be grown on Sabouraud’s agar or brain-heart infusion. Treatment includes Amphotericin B and Flucytosine. Case: 62 yom being treated w/ natalizumab for relapsing MS is brought to the clinic by his wife who reports progressive vision loss and confusion over the past 6 weeks. He has become increasingly forgetful. Over the past week he has experienced progressive weakness on his right side. CSF was normal. PCR of CSF found DNA of JC virus. These “umab” drugs can suppress cytokines and their receptors, inhibiting the processes involved in normal inflammatory responses. Natalizumab binds to VCAM-1 and prevents T-cells from entering the CNS, which can allow JC virus that is latent in most people’s kidneys and lymphoid tissue to reactivate and result in Progressive Multifocal Leukoencephalopathy. The reactivated virus replicates in oligodendrocytes in the brain of T-cell-depressed people, causing demyelination and enlarged atypical astrocytes. This results in an insidious onset of focal symptoms including cognitive and motor impairment, behavioral, speech, and visual changes. Diagnosis is made by PCR of CSF. There is currently not any FDA approved treatment. In HIV patients, you can adjust their anti-retroviral medications if their T-cell count is low and their viral load is high. Case: 65 yom w/ AIDS for 30 years has been well-controlled on his regimen, which has kept his T-cells acceptable and his viral load low. Despite that, his cognition has declined, his memory is failing, his speech is less fluent, he is depressed, and his gait has become unsteady. He is eventually diagnosed w/ HIV associated neurocognitive disorder (HAND). HAND is defined as impaired cognition + loss of two other abilities. Imaging and histology will show diffuse cortical atrophy, cortical neuronal loss w/ multinucleated cells. Aggressive anti-viral therapy has shown reversal of symptoms in some patients. Case: 60 yom brought to ER by family w/ 5-day hx of confusion and paranoia. He was previously hospitalized for Pneumocystis pneumonia, severe shingles, and recurrent thrush. HIV test is positive, CD4 count is 75, MRI shows scattered ring-enhancing lesions which are associated w/ lymphoma, toxoplasmosis, and cryptococcus. PCR of his CSF detected T gondii DNA; treatment was initiated w/ Pyrimethamine + Sulfadiazine (they both inhibit folate synthesis) After treatment w/ these drugs, “rescue” them w/ Leukovorin to save their bone marrow. Despite that, he died 3 days later. Autopsy showed edematous brain w/ hemorrhagic necrosis and tissue cysts. T gondii is a protozoan parasite found in meat and cat boxes. Infection follows ingestion of an oocyst or tissue cyst. The replicative form is a tachyzoite that spreads throughout the body. Tachyzoite replication and innate inflammatory response leads to neuronal damage and apoptosis in the brain. Toxoplasmic encephalitis, w/ or w/o focal CNS lesion is usually subacute in onset, and presents w/ AMS, seizures, weakness, cranial nerve disturbances, sensory abnormalities, cerebellar dysfunction, meningismus, movement disorders, and neuropsychiatric manifestations (paranoia). Prevention in patients w/ T-cell count below 200: TMP/SMX Case: 37 yom to ER w/ facial palsy for a few hours, and 36 hours of severe headache, photosensitivity, and neck stiffness. Also has fever w/ back and leg pain. Back pain radiates down left leg w/ accompanied leg weakness for a few days. LP shows 160 mononuclear cells, normal glucose. He works at a wildlife refuge in PA and is frequently bitten by ticks. CSF and serum finds antibody to B burgdorferi. He is diagnosed w/ Lyme neuroborrleiosis and stated on Doxycycline. B burgdorferi is a corkscrew shaped spirochete that is flagellated. It does not gram stain, but does have a gram-negative cell wall structure. They are extracellular and avoid opsonization and phagocytosis. Mouse is reservoir. Classic triad is aseptic meningitis, cranial neuritis (esp. facial nerve palsy), and peripheral neuropathy/radiculitis. Definitive diagnosis is made with serology to find antibodies in CSF and serum. Case: Al Capone had tertiary syphilis and had early dementia w/ mental and physical decline. Syphilis is caused by Treponema pallidum which is sexually transmitted. It is a spiralshaped, extracellular spirochete that quickly spreads through the body by secreting hyaluronidase to avoid phagocytosis. It causes marked inflammation d/t LPS. It does not gram stain but has a gram-negative cell wall. It cannot be cultured. Diagnosis is made w/ serology and dark-field microscopy. Treatment is penicillin. Case: 22 yom hospitalized w/ confusion, hallucinations, bradykinesia, and myoclonus. 1-month earlier his family noticed spasticity and difficulty w/ memory. Several months prior to that he developed personality changes, depression, and anxiety. Lab tests revealed a prion disease called Creutzfeldt-Jakob (vCJD). Prions are proteinaceous infectious particles that can arise spontaneously within cells and spread between cells in the same host. It can also spread from one host to another. Infectious prions have NO detectable nucleic acid, they are highly resistant to heat and disinfecting agents, and are resistant to protease degradation. Their unique conformation is a result of misfolding into beta-pleated sheets instead of helices. Prion diseases are sometimes called transmissible spongiform encephalopathies. These diseases are progressive and fatal. They have long incubation periods. Brains have scrapie-associated fibrils w/ vacuolization and astrocytosis, without any immune or inflammatory response. Animals- Scrapie (sheep), Bovine spongiform encephalopathy (cows), chronic wasting disease (deer and elk). Humans- Creutzfeld-Jacob disease (CJD), Variant CJD (vCJD). In humans, these diseases were mostly sporadic and seen in patients over 60 years old. They would have insidious onset of memory loss, decreased cognition, personality changes, myoclonus, and ataxia. CSF findings are normal, autopsy shows spongiform brain. There is no treatment, all you can do is die. ______________________________________________________________________ ______________