Heart Anatomy & Physiology: Cardiac Function & ACS Overview
advertisement

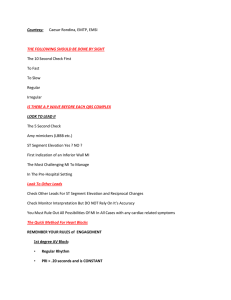
Anatomy 4 chambers: ▪ Atria (2) ▪ Ventricle (2) 4 Valves: ▪ Semilunar: Aortic, pulmonic ▪ Atrioventricular: Tricuspid, Bicuspid/Mitral Remember: Stenosis – is a narrowing of valves Regurgitation – is the process (backflow of blood) Murmur – is the symptom (assessment) Coverings (epicardium): Pericardium ▪ Fibrous ▪ Serous (parietal, pericardial cavity, visceral) Myocardium Endocardium Major Veins ▪ Inferior & Superior Vena Cava (unoxygenated) ▪ 4 Pulmonary Veins (oxygenated) Major Arteries ▪ Pulmonary arteries (unoxygenated) ▪ Aorta (oxygenated) Physiology Action – Potential The brief reversal of electric polarization (positive and negative) of the membrane of a nerve cell (neuron) or muscle cell (ex: cardiac). In the neuron an action potential produces the nerve impulse, and in the muscle cell it produces the contraction required for all movement. Action-Potential to Heart: 1. Cardiac Pacemaker Cells action-potential 2. Cardiac Myocyte action-potential Depolarization During depolarization, the membrane potential rapidly shifts from negative to positive polarity. For this rapid change to take place within the interior of the cell, several events must occur along the plasma membrane of the cell such as sodium influx into the cell. Repolarization Is a stage of an action potential in which the cell experiences a decrease of voltage (negative polarity) This phase occurs after the cell reaches its highest voltage from depolarization. Electrolytes: Determine action potential in the cell membrane Sodium (Na+) Extracellular Potassium (K+) Intracellular Calcium (Ca++) Extracellular Remember: ▪ It is important to know cardiac action potential to understand knowledge involving cardiac pharmacology. It is influenced by innervation of the Autonomic Nervous System (Sympathetic and Parasympathetic). However, it can initiate and generate its own (automaticity) thru its specialized pacemaker cells. ▪ Action potential activity within the heart can be recorded to produce an electrocardiogram (EKG). Autonomic Innervation The autonomic nervous system plays a key role in regulating changes in the cardiovascular system and its adaptation to various human body functions. The sympathetic arm of the autonomic nervous system is associated with the fight and flight response, while the parasympathetic division is responsible for the restorative effects on heart rate, blood pressure, and contractility. How? Sympathetic Nerves: Binding of catecholamines (e.g. norepinephrine, epinephrine) to adrenergic receptors in the heart (Beta 1) Cholinergic Nerve (Vagus): Binding of acetylcholine to muscarinic/cholinergic receptors in the heart (M2) Cardiac Conduction system Cells in the cardiac conduction system can generate electrical impulses and then distribute the signal throughout your heart. While all cells in your heart can conduct electricity, the cells in this system conduct it at very specific speeds. This is how different parts of your heartbeat at just the right time. The parts of the cardiac conduction system are (in order, starting where electricity is generated): ▪ ▪ ▪ ▪ ▪ The sinoatrial (SA) node. The atrioventricular (AV) node. The Bundle of His. Bundle branches. Purkinje fibers. Cardiac output: Cardiac output (CO) is the amount of blood the heart pumps in 1 minute, and it is dependent on the heart rate, contractility, preload, and afterload. Normal CO: 4-8 liters per minute, depending on the person’s size. Basically, total blood volume circulates to heart in 1 full minute as a cardiac output (CO) Remember: Cardiac output Cardiac Output is just simply what you want from heart to produce in order to nourish nutrients and O2 in each body system. Persistent decrease CO means abnormal heart and subsequent problem to brain, kidneys, heart, liver tissues, etc. Cardiac CO: Heart Rate (HR) x Stroke Volume Heart Rate (HR): Heart rate is the speed of the heartbeat measured by the number of contractions (beats) of the heart per minute (bpm) propagated by conduction system. Stroke Volume (SV): Volume of blood pumped by the ventricles with each heartbeat. Approximately 70 ml. Preload: aka “Filling Pressure”. Is the pressure that stretches the right or left ventricle during relaxation or before it contracts to produce cardiac output. Afterload: is a pressure against which the heart must overcome to eject blood during contraction. Ex: aortic pressure Illustration: Ejection fraction: The measurement of the percentage of blood leaving the heart each time it contracts. EF= SV X 100% EDV Example: CHF (Systolic vs diastolic heart failure) Blood Pressure: Is the pressure of the blood in the circulatory system (Heart and Blood vessels), often measured for diagnosis since it is closely related to the force and rate of the heart (Cardiac Output) and the diameter and elasticity of the arterial walls (Vascular resistance). 120/80 mm Hg are considered within the normal range. Systolic vs. Diastolic Blood Pressure: The first number, called systolic blood pressure, measures the pressure in your arteries related to heart activity (Cardiac output) The second number, called diastolic blood pressure, measures the pressure in your arteries (Vascular resistance) when the heart rests. Mean arterial pressure (MAP): The average pressure in your arteries throughout one cardiac cycle, which includes the series of events that happen every time your heart beats. What is a normal MAP? In general, most people need a MAP of at least 60 mmHg or greater to ensure enough blood flow to vital organs, such as the heart, brain, and kidneys. Consider anything between 70- and 100-mm Hg to be normal. A MAP in this range indicates that there’s enough consistent pressure in your arteries to deliver blood throughout your body. What is a high MAP? A high MAP is anything over 100 mm Hg, indicates that there’s a lot of pressure in the arteries. This can eventually lead to blood clots or damage to the heart muscle, which must work a lot harder. Associated conditions are MI, kidney failure and heart failure. What is a low MAP? Anything under 60 mm Hg is usually considered a low MAP. It indicates that your blood may not be reaching your major organs. Without blood and nutrients, the tissue of these organs begins to fail, leading to permanent organ damage. They include septic shock and other forms of circulatory shock. Formula: Illustration: Blood pressure Heart sounds: S1, S2, S3, S4 Acute Coronary Syndrome (ACS) Acute coronary syndrome (ACS) encompasses a range of cardiac events, including stable angina, unstable angina & acute myocardial infarction (with or without ST segment elevation). Clients with ACS require immediate treatment. ACS is a sequelae of coronary artery disease (CAD). Assessing a patient with ACS: Risk Factors of CAD: ▪ Hereditary/Familial, Age, Gender ▪ Hyperlipidemia (Atherosclerosis) ▪ Hypertension (Arteriosclerosis) ▪ Diabetes Mellitus ▪ Smoking History of present illness: ▪ Presence of Chest Pain (Angina) Characteristics: ✓ Substernal ✓ Relieved by Nitrates ✓ On exertion 3/3: Typical Angina 2/3: Atypical 0/3: non-Angina Associated signs and symptoms: ▪ Shortness of breathing ▪ Nausea/vomiting ▪ Dizziness/Syncope ▪ Lightheadedness ▪ Anxiety ▪ Sweating (diaphoresis) ▪ Fatigue A cardiac chest pain (angina) or discomfort, often described as aching, pressure, tightness or burning. Pain may spread from the chest to the shoulders, arms, upper abdomen, back, neck or jaw. ▪ Cool clammy skin Note: If the patient is complaining of chest pain, it is important to determine what causes the symptom. A chest pain can be for instance, pleuritic, positional, or upon touch (tender) Ruling out (approach to chest pain) Skin Wounds, burns, herpes zoster etc. Subcutaneous Cellulitis, abscess Sprain, strain, rhabdomyolysis, costochondritis (most common cause of chest pain in ER) Pleuritic (Upon Breathing): Pleurisy, Pulmonary embolism, Pulmonary Tumor, Pneumothorax, Pneumonia Musculoskeletal Pleural Space Pericardium Positional & pleuritic: pericarditis, myocarditis Heart Ischemic: Acute coronary syndrome Esophagus Epigastric: GERD, Esophagitis, GI ulcers Trachea Tracheitis Aorta Aortic dissection (chest pain with tearing sensation in the back), thoracic aortic aneurysm (tenderness) if ruptures, may radiate in the back downwards. Note: Always remember that ACS is a result of CAD that overtime results from the risk factors mentioned. It will cause the buildup of fatty deposits (plaques) in and on the walls of coronary arteries, the blood vessels delivering oxygen and nutrients to heart muscles. When a plaque deposit ruptures or splits, a blood clot forms. This clot blocks the flow of blood to heart muscles. When the supply of oxygen and nutrient to cells is too low (ischemia), cells of the myocardium can be injured and eventually die if no prompt treatment is done. The death of cells resulting in damage to muscle tissues is a severe type of ACS known as myocardial infarction. Differentiating ACS Differentiating ACS Asymptomatic CAD Stable angina Unstable angina NSTEMI STEMI Chest Pain On exertion On rest On rest On rest On rest Relief With rest With nitrates With nitrates With nitrates (-) (-) (-) (-)/(+) ST depression With nitrates ST elevation (-) (-) (-) (+) (+) <50% Upto 70% Upto 90% Upto 90% Upto 100% EKG (ST changes) Cardiac Markers Occlusion Asymptomatic CAD and Stable Angina: Stable plaque with no platelets and coagulation involved Unstable angina and non-ST elevation MI (NSTEMI): Unstable plaque with platelet aggregation involved; results to subendocardial injury ST elevation MI (NSTEMI): Unstable plaque with platelet aggregation and coagulation involved results to transmural injury EKG Changes: Cardiac Markers In order rising: Myoglobin: Troponin: CPK: AST: LDH: 0 - 85 ng/ml < 0.6 ng/ml (most specific & most sensitive) 12 - 70 U/ML (m) 10 - 55 U/ml (f) 10 - 50 IU/L 100 - 190 U/L Algorithm: Considering the patient is having chest pain, risk factors of CAD, history of present illness, associated signs and symptoms 1 EKG If ST elevation Stat Heart Catheterization 2 Cardiac Markers: Troponin CK-MB If Troponin (+) Urgent Heart Catheterization If Troponin (-) and EKG (-) CK-MB can be (+) but not cannot be a specific indicator of ACS If 1-2 vessels involved: Stenting (Percutaneous coronary intervention: PCI) If 3 or more: CABG Serial Monitoring: Q6 hours X 2 more If negative (-) Stress Test and Echo (evaluation) or outpatient work up Heart catheterization is a procedure in which a thin, flexible tube (catheter) is guided through a blood vessel to the heart to diagnose or treat certain heart conditions (PCI or stenting) Remember: Door-to-balloon is a time (1-1.5 hours) measurement in the treatment STEMI. The interval starts with the patient's arrival in the ER and ends when a catheter guidewire crosses the culprit lesion in the cardiac cath lab. If Stress test (+) Remember: If no access to heart catheterization, may do thrombolysis. However, patient will be at highest risk for bleeding Routine Heart Catheterization Stress Test: (Non-Pharmacologic) Heart Catheterization: Percutaneous Coronary Intervention (PCI)/ Balloon angioplasty: Inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery. Angioplasty is often combined with the permanent placement of a small wire mesh tube called a stent to help prop the artery open and decrease its chance of narrowing again. PCI is an interventional type of heart catheterization. Preparation: ▪ Check dye allergy ▪ Check for intake of Metformin ▪ Check for intake of antiplatelets ▪ Check BUN, creatinine ▪ NPO 6-8 hours Risk: ▪ Re-narrowing of artery ▪ Blood clots ▪ Bleeding ▪ Heart attack ▪ Coronary artery damage. ▪ Acute Kidney Disease ▪ Stroke ▪ Arrhythmias Remember: Check BUN, creatinine, and intake of metformin (anti diabetic) to patients receiving contrast dye. Kidney primarily excretes these materials Metformin: Withheld until 48 hrs. after procedure). Induces toxic accumulation of lactic acid. Aggravates renal failure Standard Management: Pharmacology (MONA-BASH-C) Understanding Hemostasis/Clot formation vs AntiHemostatic (Antiplatelet, Anticoagulants, Thrombolytics/Fibrinolytics): Hemostasis involves three major steps: ▪ Vasoconstriction ▪ Platelet Plug (primary hemostasis) ▪ Blood coagulation (secondary hemostasis): Involves Clotting Factors (CF) until the formation of Fibrin (non-water soluble) Coagulation Cascade Extrinsic Pathway Intrinsic Pathway Common Pathway PTT Physiologic anti-clot mechanisms: ▪ Antithrombin mainly inhibits thrombin by binding to heparin like molecule ▪ Protein C pathway degrades CF5, CF8 ▪ Tissues factor and Protein S inhibit extrinsic pathway ▪ Tissue Plasminogen activator breaks down plasminogen to form plasmin which degrades fibrin. (D-dimer is the biproduct) Vit K dependent PT/INR Antiplatelets: Bleeding risk LOW ▪ Prevents formation of new clots ▪ Prevent further increase in size of existing clots Example: ▪ Aspirin (ASA) ▪ Clopidogrel ▪ Abciximab ▪ Eptifibatide ▪ Tirofiban ▪ Cilostazol ▪ Dipyridamole ▪ Prasugrel ▪ Ticlopidine ▪ Ticagrelor Remember: NCLEX Tips ▪ Check for signs of bleeding ▪ Monitor platelet count Hold medication if <50,000 Inform HCP if <150,000 ▪ Monitor HGB, hold if <7 g/dl ▪ Activated charcoal for ASA toxicity ▪ Hyperventilation (Respiratory Alkalosis is a sign of ASA toxicity Anticoagulants: Bleeding risk MODERATE ▪ Prevents formation of new clots ▪ Prevent further increase in size of existing clots Heparin ▪ Enhances antithrombin activity ▪ Unfractionated (IV): Inhibits CF2, CF10 ▪ Low molecular weight/LMW (SQ): Inhibits CF10 Example: Enoxaparin Fondaparinux Remember: NCLEX Tips ▪ Check for signs of bleeding ▪ Monitor platelet count Hold medication if <50,000 Or if less than 50% of baseline (HIT) ▪ Monitor HGB, hold if <7 g/dl ▪ Check for PTT only for Unfractionated (IV) heparin (not > 70 sec: bleeding risk), LMWH does not need checking of PTT ▪ No massage to SQ injection site ▪ No Fondaparinux within 6 hours post operative patients with spinal anesthesia ▪ Generally, not given with other blood thinners (antiplatelets) unless prescribed by HCP. Heparin is not given with other oral anticoagulants like apixaban, rivaroxaban and the likes due to high bleeding risk. ▪ Heparin antidote: Protamine Sulfate Heparin-induced thrombocytopenia (HIT): Is a serious complication of taking heparin. With HIT, your immune system causes your platelets to clot in the presence of heparin, resulting in your platelet levels dropping. Without treatment, the clotting puts you at risk of developing life-threatening blood clots. HIT usually happens from 5 days to 2 weeks after first dose of heparin. It can cause DVT, PE and less often ACS and CVA. Treatment Options for HIT are blood thinners that rarely cause HIT like Fondaparinux (SQ), Argatroban (IV), Dabigatran (PO) Warfarin ▪ Vitamin K inhibitor ▪ Anticoagulant of choice to patients with ESRD ▪ Anticoagulant of choice to patients with valvular disease ▪ Takes effect usually up to 5 days Remember: NCLEX Tips ▪ Check for signs of bleeding ▪ Monitor HGB, hold if <7 g/dl ▪ Check for INR (not > 3.5 sec: bleeding risk) ▪ Consistent intake of green leafy vegetables (rich in Vit K). It does not need to be increased or decreased. ▪ Antibiotics can affect Vit K due to its effect to intestinal bacteria. ▪ Can be given with Heparin (bridging) until therapeutic INR level is achieved usually up to 5 days ▪ Warfarin antidote: Vitamin K Remember: Anticoagulation Therapy Heparin (IV Drip) PTT: 25 – 35 sec (less sensitive) (1.5 – 2X is therapeutic) Risk for Bleeding: > 70 secs Warfarin (Coumadin): INR: 0.9 - 1.18 (Up to 3X is therapeutic) Risk for Bleeding: > 3.5 secs Direct Acting Oral Anticoagulants: Apixaban (PO), Rivaroxaban (PO), Edoxaban (PO) ▪ Inhibits CF10, non-Vitamin K inhibitor ▪ Anticoagulant of choice to patients without ESRD ▪ Anticoagulant of choice to patients without valvular disease ▪ Takes effect immediately ▪ Alternate to Warfarin ▪ Lower risk of bleeding than warfarin Argatroban (IV), Bivalerudin (IV), Dabigatran (PO) ▪ Inhibits CF2, non-Vitamin K inhibitor ▪ Takes effect immediately ▪ Alternate to Heparin Remember: NCLEX Tips Note: No need for too many blood works as compared to Heparin ▪ Check for signs of bleeding ▪ Monitor renal function (BUN and creatinine) ▪ Do not give with any forms of heparin together (higher risk for bleeding) Thrombolytics/Fibrinolytics/Tissue Plasminogen Activator (TPA): Bleeding risk HIGH ▪ Dissolves clots (Fibrinolysis) by catalyzing the conversion of plasminogen to plasmin, the primary enzyme involved in dissolving blood clots. ▪ This treatment is used in facilities without an interventional cardiac catheterization laboratory or when one is too far away to transfer the client safely. Alteplase ▪ Intravenous (IV): 1 hour ▪ Catheter assisted: up to 72 hours ▪ Most often used fibrinolytic in the treatment of acute coronary syndrome (ACS), pulmonary embolism (PE), and acute stroke (CVA) ▪ Non antigenic, therefore seldom associated with any allergic reactions compared to Streptokinase (produced from streptococcus) Remember: NCLEX Tips ▪ Check for signs of bleeding ▪ Do not give with other blood thinners ▪ No IM and SQ injections, No ABG blood draws ▪ Given in a compressible site in case of bleeding. Not given central line (non-compressible) Contraindications: ▪ Prior intracranial hemorrhage ▪ Arteriovenous malformation (AVM): aneurysms ▪ Ischemic CVA within 3 mos. ▪ Suspected aortic dissection ▪ Active bleeding ▪ BP >180/110 (may indicate hemorrhagic CVA) ▪ Recent surgery in 2 weeks ▪ Significant head trauma within 3 mos. General signs of bleeding: ▪ Intracranial hemorrhage: Headache, altered mental status, decrease LOC ▪ Epistaxis ▪ Gum bleeding ▪ GIB: Abdominal pain/discomfort, Upper GI: coffee ground emesis, hematemesis; Lower GI: black tarry stool, hematochezia ▪ Hemoptysis ▪ Petechiae, easy bruising (hematoma), purpura, Note: easy bruising is expected to a patient getting blood thinners. Bruising accompanied by other forms of bleeding like epistaxis, hematuria and GIB must be investigated (inform HCP). Bruises in unusual places such as back, abdomen and upper thighs may be concerning because most people don’t frequently bump those body parts (inform HCP). ▪ Hematuria ▪ Vaginal bleeding Remember: Hypovolemic shock The symptoms include: ▪ Anxiety, confusion ▪ Low or no urine output ▪ Pale skin ▪ Tachycardia ▪ Low Blood pressure ▪ Dyspnea ▪ Weak pulse ▪ Clammy skin ▪ Decrease O2 saturation General Patient Teachings: Blood Thinners ▪ Monitor for signs of bleeding ▪ Monitor blood works for specific blood thinners ▪ Combination of some blood thinners must be prescribed by physician. ▪ Antiplatelet and anticoagulants should be stopped at least 5-7 days prior to the surgery to reduce the chance of intraoperative and postoperative bleeding or consult prescribing physician. ▪ Avoid EGOS (Risk for bleeding) E: Vitamin E G: (4Gs: Herbal Remedies) Ginkgo biloba Ginger Garlic Ginseng O: Omega 3 S: St. John’s Wort ▪ ▪ ▪ ▪ ▪ No contact sports Prevent constipation (increase fiber and oral fluid intake) Prevent trauma resulting from falls Avoid rigorous toothbrushing, flossing Avoid use of razors Infective Endocarditis Risk: Preexistent disorders Prosthetic valves Cong. heart defects Rheumatic heart disease Intravenous drug use Causative Agents: ▪ Streptococcus viridans (most common but not virulent) ▪ Staph aureus (common and virulent) ▪ Staph epidermidis Remember: Inflammatory type of Endocarditis is called Libman Sacks Endocarditis: related to SLE. Remember: High risk groups with prosthetic valves for example should have antibiotics before dental procedures. ▪ ▪ ▪ ▪ Splinter hemorrhages: Thin, red to reddish-brown lines of blood under the nails due to product of Ag-Ab complexes forming emboli. It runs in the direction of nail growth. Janeway lesion: non-tender, small erythematous or hemorrhagic macular lesions indicative of infective endocarditis also due to Ag-Ab complexes. Osler’s nodes: Painful, red, raised lesions on the hands and feet caused by immune deposition from Ag-Ab complexes. Roth spots: Retinal hemorrhages with white or pale centers due dysfunction of the retinal capillaries from Ag-Ab complexes or inflammatory reactions. Myocarditis Causative Agents: ▪ Coxackie virus ▪ Parasitic/protozoal (Trypanoma cruzi): Severe case “Chagas disease” needs heart transplant Pericarditis Remember: Anatomy Pericardial cavity: < 50 ml fluid: normal > 50 ml fluid: abnormal (Pericardial effusion) > 150 ml fluid: cardiac tamponade Causes: ▪ Idiopathic ▪ Coxackie virus ▪ Dressler’s syndrome (Post AMI) ▪ Uremia (Urea irritates pericardium) Classic sign: ▪ Chest pain on lying (relieved by sitting up) ▪ Pericardial friction rub Treatment of choice: ▪ Pericardiocentesis Complication: Cardiac Tamponade Beck’s Triad ▪ Narrowed pulse pressure (Hypotension) ▪ Muffled/distant heart sound ▪ Distended neck veins Rheumatic Heart Disease (RHD) Rheumatic fever: An inflammatory disease (autoimmune) that can involve the heart, joints, skin or brain. These diseases are closely associated with one another. (e.g. Rheumatoid arthritis, rheumatic heart disease, scarlet fever, impetigo, pharyngitis) and are usually triggered by Streptococcal infections (group A beta-hemolytic streptococcus, aka GABHS) Remember: Diagnostic criteria ▪ Acronym JONES (major criteria) CAFÉ PAL (minor criteria) ▪ Throat cultures for (+) GABHS, elevate Anti- streptolysin titer Kawasaki disease (Mucocutaneous lymph node syndrome) Kawasaki disease (KD): Is a systemic vasculitis of childhood that presents with ≥5 days of fever, nonexudative conjunctivitis, lymphadenopathy, mucositis, hand and foot swelling, and a rash. Diagnosis: CRASH & Burn 4/5 of the given criteria + Fever ≥5 days Treatment: IV Immunoglobulin along with aspirin is the recommended initial treatment for Kawasaki disease, with the primary goal of coronary disease prevention. Remember: IVIG creates high plasma oncotic pressure, and signs of fluid overload and pulmonary edema develop if it is given in large quantities. Therefore, the child should be monitored for symptoms of CHF Congestive Heart Failure (CHF) Remember: Anatomy and physiology is the key Right sided: Resistance to right side d/t failure causes backflow to both large veins (vena cavas). Excess fluids pool in GI tract, liver, extremities (U/L) Left sided: Resistance to left side d/t failure causes backflow to lungs through pulmonary veins. Excess fluids cause pulmonary edema. Assessing a patient with CHF: Causes of CHF: Note: Etiology does not change the manner of treatment in CHF ▪ ▪ ▪ ▪ ▪ ▪ ▪ Cor Pulmonale (Chronic lung disorders) Pulmonary hypertension Pulmonary stenosis Acute coronary syndrome Cardiomyopathy Aortic stenosis Hypertension Right CHF signs and symptoms: ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Jugular vein distention (JDV) Headache Syncope Dizziness Swelling in legs and feet (peripheral edema) Weight gain Abdominal discomfort Nausea/vomiting Hepatosplenomegaly Ascites Remember: Instruct the patient to seek immediate care if gaining 2 or more pounds in 1 day or 5 or more pounds in 1 week Left CHF signs and symptoms: ▪ Shortness of breathing on exertion ▪ Orthopnea ▪ Paroxysmal nocturnal dyspnea Pulmonary edema ▪ Crackles “wet lungs” ▪ Hypoxemia ▪ Pink frothy sputum ▪ Shortness of breathing even at rest Remember: Sudden shortness of breath, irregular heartbeat, or chest pain are signs of CHF exacerbation, therefore a priority and needs immediate care. Acute Exacerbation: Consider patient is manifesting sudden shortness of breath, irregular heartbeat, or chest pain ▪ Chest X-Ray ▪ BNP (B-Type Natriuretic Peptide ▪ EKG ▪ Cardiac markers (CK-MB, Troponin) (+) CHF ▪ Chest X-Ray (+) Infiltrates ▪ Elevated BNP (+) ACS: Ischemic CHF ▪ EKG: (+) STEMI ▪ Troponins (+) Remember: Normal BNP <125 pg/mL (0 - 74 YO) <450 pg/mL (75 - 99 YO) Brain (or b-type) natriuretic peptide (BNP) is secreted in response to ventricular stretch and wall tension when cardiac filling pressures are elevated. The BNP level is used to differentiate dyspnea of heart failure from dyspnea of noncardiac etiology. Remember: It is important to evaluate or rule out acute coronary syndrome. Majority of CHF is caused by CAD-Acute coronary syndrome. EKG and cardiac markers most specifically troponin are gold standards. If determined, additional treatment approach is necessary such as MONABASH and heart catheterization. PCI (stenting) if needed. Remember: Echocardiography confirms and distinguishes between 2 types of CHF namely diastolic (filling failure) from systolic (pump failure) by checking ejection fraction. Remember: Ejection Fraction (EF) A normal EF is 50-70%. A measurement under 40% may be evidence of CHF or cardiomyopathy and may indicate severity and may need a long term management such Implantable Cardioverter Defibrillator (ICD) to prevent serious arrhythmias Pharmacologic treatment: According to classification Class 1: No restrictions to activity Class 2: Mild SOB on exertion (slight limitation) Class 3: SOB on ADL (marked limitation) Class 4: SOB at rest 1 2 3 4 Remember: Patient with Class 4 CHF may be on hospice status that needs palliative care. Inotropes are indicated as a palliative treatment. Home infusion of milrinone through a central line is becoming more common as a palliative measure for endstage heart failure. It requires venous access a PICC line as the medication is a vesicant and can cause extravasation if infused through a peripheral IV. Monitor the central line insertion site for infection, ensure infusion pump, monitor daily weights. Helpful Mnemonics: UNLOAD FAST Low Na diet: Remember: Diuretics Potassium Sparing (SEAT): ▪ Spironolactone ▪ Eplerenone ▪ Amiloride ▪ Triamterene Potassium Wasting (BF): ▪ Bumetanide ▪ Furosemide DASH (Diet Approach to Stop HTN) ▪ All foods high in sodium (>400 mg/serving) should be avoided. ▪ Do not add salt or seasonings containing sodium when preparing meals ▪ Do not use table salt ▪ Avoid high-sodium foods (e.g., canned soups, processed meats, cheese, frozen meals) ▪ Limit milk products to 2 cups daily Venous thromboembolism (VTE) Deep vein thrombosis vs Pulmonary embolism DVT occurs when a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs. Pulmonary embolism (PE) is a DVT that breaks loose and travels through the bloodstream to the lung vasculature. Death from PE is often attributed to a missed diagnosis. Early identification of risk factors can have a positive effect on client outcome. Assessing a patient with VTE: (DVT and PE) Causes of DVT: Virchow’s Triad Immobile conditions such as brain trauma, major surgeries, long flights, or drive of >3-4hrs, etc. Smoking, IV catheterization, hypertension, chronic inflammation, sepsis Genetic predisposition (coagulation disorders) Cancer, contraceptives, pregnancy, nephrotic syndrome, etc. Signs and symptoms of DVT: Remember: A 2 cm increase in size, larger than the other extremity is a significant finding. It may be a sign of DVT along with other manifestations. A measuring tape is a necessary equipment in suspecting DVT. Diagnostic evaluation of DVT: Duplex ultrasonography is the standard imaging test to diagnose DVT. D-dimer blood test: Measures a substance in the blood that is released when a clot breaks up. Indicated for suspicion of DVT. D-dimer is the degradation biproduct of fibrin after exposed to plasmin. Normal levels 220 to 500 ng/mL. Note: If D-Dimer is elevated or DVT is detected, the following diagnostic exam is indicated to check for presence of PE. Computed tomographic angiography (CTA): A special type of X-ray test that includes injection of contrast material (dye) into a vein. This test can provide images of the blood vessels in the lungs. Standard imaging test to diagnose PE. Note: If CTA is not available and contraindications are observed may do V/Q scan Ventilation-perfusion (V/Q) scan: A specialized test that uses a radioactive substance to show the parts of the lungs that are getting 02 (ventilation scan) and getting blood flow (perfusion scan). Used when CTA is not available or when contraindicated. Pulmonary angiography: Special type of X-ray test that requires insertion of a large catheter to femoral vein & into the pulmonary arteries, followed by injection of contrast dye through the catheter. Most accurate test to diagnose PE but requires time and safe precautions are observed due to its invasiveness. Signs and symptoms of PE: Signs and symptoms: ▪ Shortness of breath (SOB)/ Dyspnea ▪ Pleuritic chest pain on inspiration or coughing ▪ Tachycardia ▪ Tachypnea ▪ Hypoxemia ▪ Apprehension, anxiety ▪ Syncope ▪ Cough ▪ Diaphoresis ▪ Cold clammy skin ▪ Fever (rare sign of severe PE) ▪ Hypotension (sign of impending circulatory failure) Mechanism: Preventing VTE (DVT and PE): VTE PROPHYLAXIS/ TREATMENT Pharmacologic Mechanical Unfractionated Heparin (IV Drip) Graduated compression stocking/ted hose Low molecular weight heparin (LMWH): SQ Intermittent pneumatic compression device Oral anticoagulants (Vit K antagonist, Direct Acting) IVC filter Thrombolytics Thrombectomy/ Embolectomy Remember: Heparin Dosing and indication Most central lines require IV heparin flushes to maintain patency and prevent clotting by using single-dose vials of 2– 3 mL of 10 units/mL or 100 units/ml. A dose of 1000–10,000 units is given for cases of thromboembolism. Remember: LMWH (Enoxaparin) Comes in a prefilled syringe. To ensure complete medication delivery, the air bubble should not be expelled prior to injection. ▪ Right or left side of abdomen, 2 inches from umbilicus ▪ Insert the needle at a 90-degree angle into a pinched-up area of skin. ▪ Discourage the client from rubbing the site. Anti-embolism stockings: Anti-embolism stockings improve blood circulation in the leg veins by applying graduated compression. When fitted properly and worn consistently, the stockings decrease VTE risk. The stockings should not be rolled down, folded down, cut, or altered in any way. If stockings are not fitted and worn correctly, venous return can be impeded. Intermittent pneumatic compression device or sequential compression device (SCD): A mechanical prophylactic treatment to reduce the incidence of VTE by enhancing the blood flow in the deep veins of the legs, thereby reducing venous stasis. SCD utilize sleeves with separated areas or pockets of inflation, which works to squeeze on the appendage in a “milking action.” The most distal areas will initially inflate, and the subsequent pockets will follow in the same manner. An inferior vena cava filter: A device that is inserted percutaneously, via the femoral vein. The filter traps blood clots (embolus from DVT) from lower extremity and prevents them from causing PE. Prescribed when clients have recurrent emboli or anticoagulation is contraindicated. Clients should report any metallic implants (e.g., vascular filters/coils) to the health care team prior to radiologic imaging. Surgical or catheter embolectomy: Performed in patients with massive pulmonary embolism. Embolectomy is used for patients with persisting shock despite supportive care and who have an absolute contraindication for thrombolytics Thrombectomy: Involves removal of the clot in a patient with DVT. Spectrum of PE: Overview D/C Home Signs/Symptoms Right Heart Strain Hypotension/VS LMWH – Oral anticoagulants (Vit K antagonist, Direct Acting) Asymptomatic None None Stable LMWH – Oral anticoagulants (Vit K antagonist, Direct Acting) Symptomatic Yes None Stable Medical Unit Heparin (IV drip) - LMWH – Oral anticoagulants Sub-massive Yes Massive Stable Thrombolytics or Thrombectomy if with chronic right heart strain Yes ICU Yes Yes Unstable EKG Interpretation Steps 1. Identify PQRST 2. Determine PR Interval, QRS complex (time) 3. Check rhythm 4. Determine heart rate 1. Identify PQRST 2. Determine PR Interval, QRS complex (time) Normal values: PR Interval: 0.12-0.20 secs Abnormal: ≥ 0.24 secs QRS comp: 0.6-0.12 secs Abnormal: > 0.12 secs Example: PR: QRS: 3. Check rhythm. What is a regular rhythm? What is irregular rhythm? Remember: Checking rhythms is important in counting the heart rate. One cycle of PQRST represents the other in a regular rhythm. In contrast, one cycle may not represent the other in an irregular rhythm. Regular rhythm: Irregular rhythm: Common regular rhythm (R-R Intervals): ▪ Sinus Rhythm ▪ Sinus Tachycardia ▪ Sinus Bradycardia ▪ Supraventricular Tachycardia(SVT) ▪ Atrial Flutter (variable) ▪ 3rd degree AV block (CHB) Common irregular rhythm (R-R Intervals): ▪ Premature Atrial Contractions ▪ (PACs) ▪ Premature Ventricular Contractions (PVCs) ▪ Atrial Fibrillation ▪ 2nd degree AV block (Type 1) 4. Determine the heart rate. 1. Six (6) seconds strip method: Applicable for both regular and irregular rhythm. Count the number of QRS complexes over a 6 second interval. Multiply by 10 to determine heart rate. 10 R waves or QRS complexes in a 6 second strip in a regular rhythm multiply by 10 is 100 bpm. 10 QRS X 10 = 100 bpm 5 R waves or QRS complexes in a 6 second strip in an irregular rhythm multiply by 10 is 50 bpm. 5 QRS X 10 = 50 bpm 2. 1,500 method: Applicable ONLY for regular rhythm. Since R-R intervals are all the same or constant in all cycles, one R-R represents the other. Determine the heart rate by counting the number of smallest boxes between R-R. (Most accurate in calculating HR) Smallest boxes: 1500 mm/min ÷ 15 = 100 bpm Note: 1mm = 1 smallest box 1 sec = 25 smallest boxes 60 sec (1 min) = 1,500 smallest boxes (1,500 mm) Overview of Common Arrhythmias: Common Arrhythmias: 1. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 2. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 3. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: Types: 4. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 5. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 6. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 7. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: Types: 8. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: Types: 9. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: 10. PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: PQRST P wave: PR Interval: QRS complex: Rhythm: Rate: Interpretation: How to distinguish types of AVB? PR ≥ 0.24 secs Consistent PR Inconsistent PR 1° AVB 2° AVB (II) 2° AVB (I) 3° AVB 1P:1QRS ≥2P:1QRS Irregular Rhythm Regular Rhythm Management of arrhythmias: continued 1. Sinus Bradycardia 2. Sinus Tachycardia 3. Atrial fibrillation, Atrial Flutter 4. SVT 5. PVC 6. Ventricular Tachycardia, Ventricular Fibrillation 7. AV Blocks