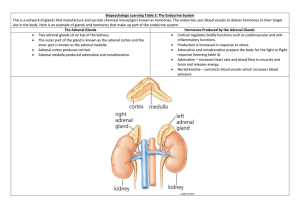
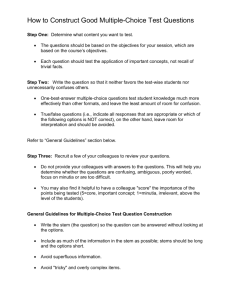
Curriculum in Urology Adrenal Tumours .................................. L. Jarolima,*, J. Brezab, H. Wunderlichc  valu 84, 15006 Prague 5, Czech Republic Department of Urology, Charles University, V U Department of Urology, Derer's University Hospital, Bratislava, Slovak Republic c Department of Urology, Friedrick Schiller University, Jena, Germany a b Abstract Benign or malignant tumours within the adrenal glands can give rise to of a number of hypersecretion syndromes dependent on where the tumour is located. These include oversecretion of aldosterone (Conn syndrome), cortisol (Cushing syndrome) or androgens (androgenital syndrome) and adrenaline or noradrenaline (pheochromocytoma). It is very dif®cult to distinguish benign and malignant adrenocortical tumours. However, a number of criteria can be applied, including size; benign tumours of the adrenal cortex are generally smaller than malignant tumours. Benign tumours tend to be homogeneous in cross-section compared with heterogeneous malignant tumours. The presence of distant metastases is an absolute indication of malignancy. * Corresponding author. Tel. 420-22443-4804; Fax: 420-22443-4820. E-mail address: ladislav.jarolim@lfmotol.cuni.cz (L. Jarolim). Open adrenalectomy remains still a safe and effective surgical technique for treatment of complicated and recurrent adrenal tumours. However, in experienced hands, laparoscopic adrenalectomy is a safe and minimally invasive surgical technique with a short hospitalization stay and minimal complication rate. Generally, adrenocortical carcinomas are curable only when they are small and localized. Adjuvant treatment regimes for more advanced adrenocortical carcinoma involves the chemotherapeutic agent mitotane, while conventional multiagent chemotherapy still needs to be evaluated in randomized trials. Physiology and pathophysiology of the adrenal glands Adrenal physiology Each adrenal gland consists of the cortex and the medulla, and under normal circumstances the mass is of the order of 0302-2838/02/$ ± see front matter # 2002 Elsevier Science B.V. All rights reserved. PII: S 0 3 0 2 - 2 8 3 8 ( 0 2 ) 0 0 3 6 5 - 2 Eur Urol 2003;43 (Curric Urol I±X) I * 3±7 g. With regard to aetiology, morphology and function, these two regions of the gland act as entirely distinct organs. Three zones can be identi®ed within the adrenal cortex: the zona glomerulosa, the zona fasciculate and the zona reticularis. The main products of the peripheral zone of the cortex, the zona glomerulosa, are mineralocorticoids (mainly aldosterone), while secretion of glucorticoids (mainly cortisol) predominates in the zona fasciculata and the sex steroids (androgens, progesterone and oestrogens) are secreted by the inner most zone, the zona reticularis. The function of the zona glomerulosa is under the control of the rennin±aldosterone system, whereas glucorticoid and androgen production is controlled mainly by hypophyseal adrenocorticotropic hormone (ACTH). ACTH secretion exhibits a diurnal rhythm, with highest levels at 6 am and lowest levels at 10 pm, which correlates with the oscillating pattern of cortisol plasma levels. A common precursor of steroidal hormones of the adrenal cortex is cholesterol; these hormones are metabolised by the liver and the metabolites are secreted by the kidneys. The arterial blood supply (Fig. 1) to the adrenal glands consists of the: superior adrenal artery (from the inferior phrenic artery), medial adrenal artery (from the abdominal aorta), II * inferior adrenal artery (from the renal artery). The venal blood supply (Fig. 1) is more complicated depending on which side the gland is located. In the case of the right gland, the right adrenal vein is short and empties into the inferior vena cava; the left adrenal vein is longer and thicker and empties into the left renal vein. In addition, there are multiple smaller veins. Mineralocorticoids. Mineralocorticoids, in particular aldosterone, control the volume and ion content of the extracellular and intracellular fluids. Aldosterone stimulates reabsorption of sodium and increases secretion of K into urine. An excess of aldosterone causes a rise of the extracellular fluid, hypertension, hypokaliaemia and metabolic alkalosis. Glucocorticoids. Glucocorticoids are of vital importance and have numerous effects on the metabolism of saccharides (cortisol increases gluconeogenesis), proteins (catabolic effect, increasing proteolysis and leading to a loss of the muscular mass, skin thinning, osteoporosis) and lipids. Glucocorticoids influence the immune system and have anti-inflammatory and immunosuppressive effects. Due to the effect of cortisol, the blood inflow and glomerular filtration increase in the kidneys. Glucocorticoids cross the blood±brain Fig. 1. Adrenal blood supply. Eur Urol 2003;43 (Curric Urol I±X) Jarolim/Breza/Wunderlich barrier and directly affect the metabolism of the brain. Adrenal androgens. Adrenal androgens are converted into active hormones (testosterone and dihydrotestosterone) and exhibit anabolical effects, unlike the catabolic effect of glucocortocoids. In males, the adrenal glands contribute to the daily production of testosterone by about 100 mg per day, while the testicles produce about 7000 mg of testosterone a day. In females, the adrenal glands produce roughly 50% of circulating testosterone. Hypersecretion syndromes Depending on which zona of the adrenal cortex is involved in tumour growth (benign or malignant) one of four hypersecretion syndromes may be displayed clinically. The pathoanatomical ®nding on the adrenal glands has the same basic variants: bilateral hyperplasia of the adrenal cortex, adrenocortical adenoma, or adrenocortical carcinoma. Primary hyperaldosteronism (Conn syndrome). Conn syndrome results from overproduction of aldosterone by the cells of zona glomerulosa. It occurs in adult patients, with women affected twice as frequently as men. In approximately 80% of cases, the cause is benign adrenocortical adenoma (Fig. 2) and in 20% of cases by bilateral hyperplasia of the adrenal cortex; very rarely the syndrome is due to an adrenocortical carcinoma. The symptoms of the Conn syndrome include muscular weakness, headache, polydipsia and polyuria, arterial hypertension, hypocalaemia, metabolic alkalosis and low plasma rennin levels. Cushing syndrome. Cushing syndrome is a complex phenomenon caused by hypersecretion of cortisol. It has a typical symptomatology, including: trunk obesity, plethora and moon-shaped face, purple striae on the belly, breasts and thighs, hirsutism, acne, sexual malfunction, arterial hypertension, hyperglycaemia and osteoporosis. Cushing syndrome can be classified into five categories. The central form is typified by bilateral diffuse hyperplasia of the adrenal cortex and hyperproduction of cortisol due to permanently increased ACTH secretion. Paraneoplastic Cushing syndrome has the same aetiopathology; the only difference is that ACTH is produced by ACTH-producing tumours and not by the hypophysis. Macronodular hyperplasia of the adrenal cortex independent of ACTH is characterized by the presence of large nodules in the adrenal cortex and concomitant bilateral hyperplasia of the adrenal cortex Fig. 2. Conn's syndrome caused by small benign adenoma of the adrenal cortex. Adrenal Tumours Eur Urol 2003;43 (Curric Urol I±X) III * Fig. 3. Macronodular hyperplasia of the adrenal cortex in Cushing's syndrome characterized by large nodules in the adrenal cortex and concomitant bilateral hyperplasia of the adrenal cortex. (Fig. 3). About 20±30% of all cases of the Cushing syndrome are the peripheral type caused by a benign or malignant tumour of the adrenal cortex, be (Fig. 4). In pubertal girls, Cushing syndrome is always a consequence of this form of tumour. The fifth form is iatrogenic type and is typically seen in patients receiving large doses of corticosteroids as in organ transplantation. IV * Adrenogenital syndrome. Adrenogenital syndrome is nearly always caused by a tumour within the zona reticularis, which produces excessive amounts of androgens or oestrogens and sometimes also cortisol. Approximately 50% of cases are in children and adolescents. At postpubertal age, the adrenogenital syndrome is far more frequent in females than in males. Fig. 4. Peripheral type of Cushing syndrome caused by a malignant tumour of the adrenal cortex. Eur Urol 2003;43 (Curric Urol I±X) Jarolim/Breza/Wunderlich Overproduction of androgens in women leads to virilisation manifesting itself through hirsutism, breast atrophy, oligomenorrhagia and clitoridomegalia. In boys, overproduction of androgens results in pubertas praecox, while in adult men the adrenogenital syndrome virtually cannot be detected. Overproduction of oestrogens causes feminization of adult men, which may manifests itself through gynaecomasty, atrophy of the testicles and decreased libido. In prepubertal girls, the consequence of overproduction of oestrogens by a tumour of the adrenal gland is precocious puberty. The ®rst subjective symptom of adrenocortical carcinoma is pain, which may be of the blunt persistent type caused by the pressure of the tumour on the neighbouring organs or by of in®ltration into the nerve bundles. Another, less frequent type of pain is severe abdominal pain due to acute bleeding into the tumour or from a rupture of the adrenocortical carcinoma. A relatively large group of adrenocortical tumours (around 15%) comprises the socalled adrenal gland incidentalomas. These are asymptomatic and hormonally inactive tumours, which are found incidentally by sonographic or radiological examination of the abdominal organs. Myelipoma. Myelipoma is not a true neoplasia of the adrenal gland, but rather a metaplasia. It arises from both the adrenal cortex and the adrenal medulla and is completely benign, with no symptomatology. As such, it is usually detected incidentally or when it reaches excessive size, causing pain. It consists of lipid cells and haematopoietic cells. It is again totally benign and never occurs before puberty. Adrenomedullar tumours The adrenal medulla is part of the sympathico-adrenal system and is composed of chromo®nic cells, which are in principle neurons without efferent ®bres. Theses cells produce catecholamines, the principal ones being adrenaline and noradrenaline, which in¯uence the regulation of numerous physiological and metabolic Adrenal Tumours functions. The most signi®cant disease of the adrenal medulla is pheochromocytoma, which causes the ®fth adrenal hypersecretion syndrome (adrenaline or noradrenaline). If the tumour arises from extra-adrenal chroma®ne cells, it is referred to as an extra-adrenal pheochromocytoma or paraganglioma. In 80±90% of cases, the pheochromocytoma occurs as a solitary tumour and is considered to be an acquired disease. In 10% of cases, it occurs extra-adrenally, in 10% of cases, bilaterally (sometimes as part of familial multiple endocrine neoplasia syndrome MEN2A and MEN2B), and in 10% of cases, it has histological features of malignancy. A pathognomic sign of the pheochromocytoma is paroxysmal hypertension appearing in approximately 50% of patients. Diagnosis of adrenal lesions The diagnosis of adrenal lesions involves the taking of a patient medical history and the physical examination in the ®rst instance, followed by laboratory tests aimed at proving overproduction of hormones of the adrenal cortex and hypophysis, their metabolites and main stimulators of their biosynthesis (ACTH, renin). Laboratory tests. To evaluate the disorder of the secretion of corticoids, the level of cortisol in plasma is assessed. It changes in a broad physiological range (100±650 nmol/ l) and exhibits a circadian rhythm. Free cortisol in urine is a sensitive indicator of the concentration of free cortisol in plasma; values range between 70 and 170 nmol per day and rise markedly with Cushing syndrome. Further examinations are stimulation tests (ACTH tests, metopirone test, corticoliberin test) and inhibition tests (dexamethason test). To evaluate the secretion of mineralocorticoids, the assessment of aldosterone in plasma and urine, plasma renin activity and concentration of angiotensin II are used. To evaluate the secretion of androgens, plasma values of androstendione and dehydroandrostendione, free testosterone and 17-ketosteroid in urine are assessed. With regard to pheochromocytoma, the detection of >100 nmol per 24 h adrenaline Eur Urol 2003;43 (Curric Urol I±X) V * and >500 nmol per 24 h noradrenaline in urine is diagnostic. Imaging techniques. A series of imaging techniques of the adrenal glands may be employed if biochemical and hormonal abnormalities are detected. At present the method of choice is computed tomography (CT), in particular, spiral CT, which can detect tumours as small as 0.5 cm in diameter. The application of contrast during CT examination allows an assessment of the vascularity of the tumour. Magnetic resonance imaging (MRI) allows the adrenal glands to be visualized in numerous planes. Additionally, paramagnetic contrast substances can be used, which makes it possible to resolve solid tumours from cystic formations and to ascertain the vascularity of the tumour. In clinical practice, if a tumour of the adrenal glands is proven by CT and MRI, usually no further visualizing examinations are needed before surgery. In selected cases, angiography may be performed as it provides information on the vascular supply of the tumour as well as information useful for surgical decisions. Large palpable masses in right upper quadrant have been detected with this technique. Adrenalectomy VI * Adrenalectomy is indicated for syndromes of hyperfunction of either the adrenal cortex or the medulla caused by a tumour or cortical hypertrophy (with the exception of congenital adrenal hyperplasia), or for adrenal tumours >3 cm in diameter with no hormonal activity where malignancy is suspected. Good surgical results can be expected if certain rules are adhered to. Correct pre-operative diagnosis is essential, with con®rmation of the exact form of the hypersecretion and its lateralization. If the macroscopic changes on the adrenal glands are not too signi®cant, the surgeon must work in an operative ®eld with high visibility and haemostasis must be optimal in order to differentiate minor aberrations in the physiological anatomical Eur Urol 2003;43 (Curric Urol I±X) relationships. In addition, pre- and postoperative care should allow the avoidance or rapid action to be taken in the case of a critical state due to the removal of a hormonal hyperfunction [8]. Surgical approach The choice of incision site is made dependent on: the size of the lesion; the type of disease; patient habitus; and the experience and preference of the surgeon. The surgical technique chosen is dependent of the vascularisation of the adrenal gland. The lateral approach is used with smaller tumours (<5 cm). The posterior approach goes direct to the adrenal gland, but does not allow widening of the ®eld in case of complications; this approach through the 10th intercostals space is used infrequently. The thoracoabdominal approach is used for very large tumours, particularly those on the right side, and is through the eighth intercostal space. The drawback with this incision technique is that the pleural cavity has to be opened and it is used mostly on the right side. Transperitoneal approach. The transperitoneal incision is used for large tumours, especially malignancies or pheochromocytomas due to the possibility of multifocality (10% of cases). This approach can be used in bilateral hyperplasias and in some patients with Cushing's syndrome who have extreme osteoporosis with multiple fractures, this is the only one possible. Sufficient time must be allowed with this technique because the approach to the adrenal glands is not direct. There are a number of transperitoneal approaches, including middle laparotomy, which has the advantage of simplicity and little bleeding and being suitable in bilateral disease. One disadvantage is the high post-operative rate of hernias. Other approaches include the subcostal incision (suited to large tumours), the transabdominal or Chevron incision. This is a bilateral subcostal incision, which gives wide access to both adrenal glands; it is not necessary to extend the incision of the contralateral side in the case of unilateral disease. Jarolim/Breza/Wunderlich Right adrenalectomy. For adrenalectomy on the right, the posterior peritoneum is cut just under the liver and the duodenum freed. Gerot's fascia is opened and the incision continued along the inferior vena cava superiorly, taking care not to cause injury to it (a Satinsky clamp should be used in such cases of injury). During a right adrenalectomy, one or two suprarenal arteries and veins are ligated, followed by the small medial veins and arteries and then the central adrenal vein. Left adrenalectomy. For adrenalectomy on the left, after making the incisions as for the right side, the phrenocolic ligament is cut and the descending colon mobilized medially. The inferior mesenteric vein is ligated and the ligament of Treitz cut in the case of a large tumour. At the lower edge of the pancreas, the posterior peritoneum is cut and Gerot's fascia opened. For the left adrenalectomy, the inferior adrenal vein is ligated followed by the inferior adrenal artery and the central adrenal vein. Finally, the superior adrenal vein and artery (sometimes several branches from the inferior phrenic vein and artery are present) are ligated, as well as the group of medial arteries and veins. Laparoscopic adrenalectomy. Laparoscopic adrenalectomy has been developed in recent years and is an ideal approach for smaller tumours, particularly those located in the left. The technique may involve a retroperitoneal approach using tissue dilation and this is the most common technique. The major advantage of the laparoscopic technique is comfortable recovery with a shorter period of hospitalisation; transfusion requirements are less and there are fewer perioperative complications with trained staff [4]. Laproscopic adrenalectomy is indicated for any adrenal mass in the case of: Hormone-inactive mass. Hormone-active solid mass. Recurrent central forms of Cushing's syndrome. The procedure is contraindicated in patients with: Adrenal Tumours Hernias following abdominal operations. Severe obesity. Concurrent significant intraperitoneal tumours. Coagulopathy. Serious ischaemic heart or bronchopneumonic disease. Advanced pregnancy. In terms of anaesthesia, minimal use should be made of nitrous oxide due to the risk of overdistension. The patient should also be catheterised. For right side adrenalectomy, the patient is placed in the lumbotomic position. The liver is folded cranio-medially and suf®cient diathermy of ligamentum triangulare conducted. The vena cava should be suf®ciently exposed and a careful dissection conducted between the adrenal gland and the inferior vena cava. Careful coagulation of smaller vessels with the monopolar scissors as well as bipolar forceps is applied. The thick central adrenal vein is isolated and clipped without any diathermy. For left side adrenalectomy the patient is placed in the same position as for the right side. To proceed, lateral freeing of the colon is conducted followed by the freeing of the spleen and pancreas and then careful dissection along the splenic vein. The renal vein is localized and the incoming main adrenal vein is isolated and freed of all connecting tissue and clipped. When cutting the adrenal vein no diathermy is applied. Smaller vessels including arteries are diathermed by bipolar forceps. The freed adrenal gland is pushed out using a collecting bag, which is introduced through one of the ports and removed through the abdominal wall. Comparative studies have demonstrated the advantages of the laparoscopic approach compared with traditional open approaches. These include a more rapid recovery, shorter hospitalisation and fewer complications. Partial adrenalectomy. An adrenal-sparing technique was introduced in 1985 by Linehan. It can be applied to patients with von Hippel-Lindau disease who have developed multiple bilateral adrenal pheochromocytoma. The partial adrenalectomy Eur Urol 2003;43 (Curric Urol I±X) VII * technique can preserve normal adrenal function and avoid the morbidity associated with medical adrenal replacement [5±7]. Pre- and post-operative preparation. Preand post-operative preparation of the patient is important. For those patients treated for hypercortisolism and patients undergoing bilateral adrenalectomy cortisol substitution should be applied consisting of 100 mg during surgery and 100 mg at 6 h intervals for the first day. Parenteral administration of cortisol is followed by peroral substitution in descending dosage from 50 to 30 mg per day divided in two dosages (morning 30± 20 mg; midday 20±10 mg). For patients with pheochromocytoma or conditions involving over production of catecholamine the situation is more complicated. There is a potential danger from flooding of the system with catecholamines during tumour manipulation, resulting in a very rapid increase in blood pressure. Consequently, attempts should be made to dissect and ligate the central suprarenal vein; fentolamine (Regitine) should be applied in the case of a rapid blood pressure rise. Dispensarization after surgery for pheochromocytoma is necessary, with measurement of urinary metabolites of catecholamines. Anaesthesia in these patients also has to be modified; the use of atropine in the pre-medication is not advised. Halothane and curare should not be used, whereas methoxyflurane, succinylcholine and nitrous oxide are considered suitable. Lidocaine may be applied in the event of arrhythmias during surgery. VIII * Pre- and post-operative complications. The most serious complication during adrenalectomy is damage to the inferior vena cava. Using the lateral approach it is possible to open the pleural cavity giving rise to a pneumothorax. In right sided adrenalectomy, there is a further danger of damage to the duodenum, liver, hepatic veins, pancreas, stomach, spleen and renal hilus; in the case of the latter, a nephrectomy may sometimes be required. Blood pressure fluctuations Eur Urol 2003;43 (Curric Urol I±X) during pheochromocytoma are an impor± tant complication and have been discussed above. With regard to post-operative complications, poor healing may occur in patients with hypercorticolism. In these patients, it is necessary to remove cutaneous stitches after the 14th day or even later. There is also a tendency towards wound infection in patients with steroidal diabetes and hypoglycaemia is possible in patients treated for pheochromocytoma. Haematoma infection requiring drainage is common after the removal of large tumours with a large residual cavity. Intestinal adhesions and problems with peristalsis and ileus are also potential post-operative complications. Adrenocortical carcinoma Demographics Small asymptomatic adrenocortical nodes with an average size of 2±2.5 cm are found relatively often at autopsy, however, actual adrenocortical tumours, benign or malignant, are rare in clinical practice. Adrenocortical carcinomas occur mostly in the ®rst decade of life as well as the fourth and ®fth decades, and are slightly more common in women. Abnormalities of the adrenal morphology (masses larger than one cm in diameter) are found incidentally in approximately 1% of all patients undergoing abdominal CT. As many as 2% of all autopsies show adenomatous changes of the adrenal glands and up to 38% of patients with primary extra-adrenal malignancies have adrenal metastases at the time of autopsy. Adrenocortical masses are among the most common tumours in humans. However, only a small proportion of these tumours cause endocrine diseases such as primary hyperaldosteronism, hypercortizism, hyperandrogenism and/or hyperoestrogenism. Adrenocortical carcinoma is a rare tumour with an incidence of 0.5±2% of adenomas of the adrenal gland per year. Adrenal cortical tumours producing excessive levels of steroid hormones have an estimated incidence of approximately 4 per million people per year and Jarolim/Breza/Wunderlich are represented in 50% of the cases each by adenomas and carcinomas. In a review of about 87 series containing 1891 patients with adrenocortical carcinoma, Wooten and King [1] found a slight female predominance (4:3); the incidence of left adrenal tumours was 52.8% and bilateral tumours occurred in 2.4% of patients. Of the carcinomas detected, 59.3% were functional lesions; female patients developed functional tumours more often than male patients. Patients with untreated adrenocortical carcinoma have a very poor prognosis; the mean survival time being only 3 months. Overall, 5-year survival in treated patients ranges from 16 to 43%. Aetiology The aetiology of adrenocortical carcinoma is unknown, although one opinion is that it arises de novo from the adrenal cortex. Another view is that the carcinomas develop from hyperplastic nodules in the adrenal gland. Alterations in intercellular communication, local production of growth factors and cytokines, and aberrant expression of ectopic receptors on adrenal tumour cells have been implicated in adrenal cell growth, hyperplasia, tumour formation and autonomous hormone production. Neoplastic transformation of the tissue of the adrenal cortex may also be caused by chronic excessive stimulation of ACTH. Genetic aberrations and chromosomal abnormalities, including several chromosomal loci (loss of heterozygosity on chromosomes l1p, 13q and 17p) and the genes coding for p53, p57 and insulinlike growth factor II, have been reported in adrenal tumours and may be important in pathogenesis. Classification and symptoms Adrenocortical carcinoma has been classi®ed as either functional (75%) or nonfunctional (25%) tumours. Functional carcinomas are classi®ed according to whether they produce an excess of corticosteriod, sex hormone(s), or mineralocorticoid. Excess production of corticosteroid, androgen and oestrogen occurs more frequently than mineralocorticoid excess. In Adrenal Tumours Table 1. The TNM staging system for adrenocortical carcinomas Stage Criteria I II III IV <5 cm; confined to adrenal gland >5 cm; confined to adrenal gland Local invasion or positive lymph nodes Local invasion and positive lymph nodes or distant metastases contrast to adult tumours, over 95% of paediatric tumours are functional and are frequently associated with congenital abnormalities and secondary tumours. Staging The TNM system is used for staging of adrenocortical carcinomas (Table 1). Approximately 60% of carcinomas diagnosed are stage IV, with only 2% being stage I. Unfortunately, many of the carcinomas, in particular the non-functional type, have a large tumour size. Metastases in adrenocortical carcinoma are common, with the most common sites being liver, lung and lymph nodes; other less frequent sites are bone, omentum and diaphragm (Table 2). Identification of malignant adrenocortical tumours It is very dif®cult to distinguish benign and malignant adrenocortical tumours. Even in well-differentiated tumours, many of them simultaneously exhibit morphological characteristics of both benign and malignant tissues of the adrenal cortex. However, a number of criteria can be applied, including size; benign tumours of the adrenal cortex are generally smaller than malignant tumours. Benign tumours tend to be homogeneous in cross-section compared with heterogeneous malignant Table 2. Location of metastatic disease in adrenocortical carcinoma [3] Site of metastases Frequency (%) Liver Lung Lymph nodes Bone Omentum/peritoneum Diaphragm Others 47 43 25 15 9 6 26 Eur Urol 2003;43 (Curric Urol I±X) IX * tumours. On CT, benign adrenocortical adenomas are a uniformly yellow, dark red or even black colour on cross-section, depending on fat and lipofuscin content of the cells. In contrast, adrenocortical carcinomas, which on cross-section have a lobar nature, are non-uniform with regions of necroses and bleeding. This is apparent through different tissue colours, from yellow, whitish and red to brown and dark. Nevertheless, the presence of distant metastases are the absolute indication of malignancy. Treatment Surgical treatment has been described above. In terms of chemotherapy for the disease, the most commonly used agent is mitotane, which causes necroses after being taken up by the adrenal glands. The speci®c cytotoxic activity of mitotane on the adrenal glands has lead to its use in both primary and adjuvant therapy settings. Response rates of 14±35% have been reported from a number of trials. Survival rates of 13% after 2 years have been reported by Venkatesh et al. [2], however, signi®cantly longer survival bene®ts were possible when mitotane serum blood levels were maintained above 14 mg/l. Mitotane therapy has been associated with signi®cant toxicity. Gastrointestinal symptoms include nausea and anorexia, while neuromuscular toxicity includes lethargy, dizziness, somnolence and depression. Almost all patients on this mitotane therapy will experience adrenal insuf®ciency and steroid replacement should be routinely used. Fludrocortisone acetate should be given at an initial dose of 0.1 mg three times per week, adjusted to 0.1 mg per day according to serum electrolytes and weight gain. Other therapeutic regimens that have been evaluated include the cisplatin and etosposide combination and suramin. However, none have proved as effective as mitotane. Follow-up Recurrences and metastases in adrenocortical carcinoma are common and occur in 85% of patients after complete resection. In the follow-up, careful histories and physical examination as well as CT of the abdomen and chest X-ray should be performed four times each year for the ®rst 2 years and thereafter twice each year. Patients with an elevated serum level of dehydroepiandrosterone can be followed with this marker. Patients with a tumour producing elevated levels of urinary corticosteroids should have their urine checked every 3±6 months. A rise of urinary steroid levels often signals a recurrence ahead of symptom appearance, clinical ®ndings or ®ndings in radiological examinations. References [1] Wooten MD, King DK. Adrenal cortical carcinoma. Cancer 1993;72:3145±55. [2] Venkatesh S, Hickey RC, Sellin RV, Fernandez JF, Samaan NA. Adrenal cortical carcinoma. Cancer 1989;64:765±9. [3] Pommier RF, Brennan MF. An eleven-year experience with adrenocortical carcinoma. Surgery 1992;112: 963±71. [4] Fahlenkamp D, Rassweiler J, Fornara P, Frede T, Loening S. Complication of laparoscopic procedures in urology: experience with 2407 procedures at four German centers. J Urol 1999;62:765±71. [5] de Graaf JS, Lips CJ, Rutter JE, van Vroonhoven TJ. Subtotal adrenalectomy for phaeochromocytoma in multiple endocrine neoplasia type 2A. Eur J Surg 1999; 165(6):535±8. [6] Edstrom E, Grondal S, Norstrom F, et al. Long-term experience after subtotal adrenalectomy for multiple endocrine neoplasia type IIa. Eur J Surg 1999;165(5): 431±5. [7] Walther MM, Herring J, Choyke PL, Linehan WM. Laparoscopic partial adrenalectomy in patients with hereditary forms of pheochromocytoma. J Urol 2000; 164(1):14±7. [8] Jossart GH, Burpee SE, Gagner M. Surgery of the adrenal glands. Endocrinol Metab Clin North Am 2000;29:57±68. X * Eur Urol 2003;43 (Curric Urol I±X) Jarolim/Breza/Wunderlich