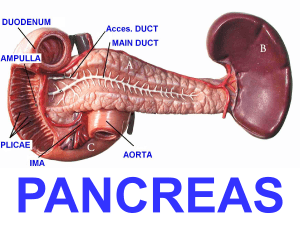
ACUTE AND CHRONIC PANCREATITIS TERM 2: SESSION 11 - NUR149 THE PANCREAS • It is a gland about six inches long, located in the upper abdomen, across the back of the belly, behind the stomach. • Has two functions: endocrine and exocrine. • Composed of scattered islets of Langerhans (endocrine function) FUNCTIONS OF THE PANCREAS EXOCRINE FUNCTION: ENDOCRINE FUNCTION: • Secretion of pancreatic enzymes into the • Islets of Langerhans which composed alpha (20%) GI tract through the pancreatic duct. secretes glucagon, beta (90%) secretes insulin, • Enzymes high in protein and electrolytes. • Alkaline due to high concentration of sodium bicarbonate. • This neutralizes stomach acids in the duodenum. • Enzymes are amylase (aids in carbohydrate digestions, trypsin aids in protein digestions, lipase for fats. delta cells (5%) secrete somatostatin • Glucagon – glycogen synthesis (stored glucose); stimulates fats and proteins for conversion in liver for additional glucose (Gluconeogenesis) • Insulin – lowers glucose and promotes glucose storage • Somatostatin –growth inhibiting hormone and insulin and glucagon inhibitor CONTROL OF CARBOHYDRATES METABOLISM • Glucose is formed through metabolism of ingested carbohydrates and also by gluconeogenesis (fats - lipogenesis and protein). • It usually stored in liver, muscles and other tissues for future use. • Normal glucose levels: 100mg/dl (5.5 mmol/L). • Insulin moderates the glucose level in the bloodstream • Increased glucose levels are due to glucagon, epinephrine, adrenocorticosteroids, growth hormone, and thyroid hormone. PANCREATITIS Inflammation of the pancreas ACUTE PANCREATITIS ● Acute inflammation of the pancreas. ● Most common in middle-aged men and women ● Considered to be a medical emergency ● Autodigestion of the pancreas ● A mild, self-limited disorder to a severe, rapidly fatal disease that does not respond to any treatment . ● Mild acute pancreatitis = edema & inflammation confined in the pancreas PATHOPHYSIOLOGY CLINICAL MANIFESTATIONS ● Severe abdominal pain (due to distention of the pancreas, peritoneal irritation, and obstruction of the biliary tract) ● Abdominal guarding and rigid or board-like abdomen (ominous sign of peritonitis) ● Bruising in the flank (Grey Turner’s spots) or umbilicus region (Cullen’s sign ● Bowel sounds may be decreased or absent. ● Paralytic ileus may occur and causes marked abdominal distension. ● Shock (hemorrhage in the pancreas), toxemia from activated pancreatic enzymes and hypovolemia due to massive fluid shift into the retroperitoneal space COMPLICATIONS LOCAL COMPLICATIONS SYSTEMIC COMPLICATIONS ● ● Pseudocyst – accumulation of fluid, pancreatic enzymes, tissue debris, ● Pulmonary (pleural effusion, atelectasis, pneumonia, and ARDS) and inflammatory exudates ● Cardiovascular (hypotension) surrounded by a wall. ● Tetany (due to hypocalcemia) Abscess – collection of pus due extensive necrosis in the pancreas. Requires immediate surgical drainage to prevent sepsis. ASSESSMENT ● Increased serum amylase and lipase levels ● Elevated urinary amylase levels ● Elevated WBC ● Hypocalcemia ● Hyperglycemia and glucosuria ● Elevated serum bilirubin ● Hematocrit and hemoglobin levels MEDICAL MANAGEMENT ● NPO ● Enteral/parenteral nutrition ● Nasogastric suction for nausea and vomiting to decrease painful abdominal distension and paralytic ileus. ● Histamine-2 (H2) antagonists & proton pump inhibitor. ● Analgesia ● Antiemetics DIAGNOSTIC TESTS & SURGICAL MANAGEMENT ● X-ray studies of the abdomen ● Laparotomy and chest ● Pancreatectomy ● Ultrasound ● Contrast-enhanced CT-scan ● Paracentesis ● ERCP to determine if the pancreas is resolving NURSING MANAGEMENT ● Relieve pain and discomfort ● Improve breathing pattern ● Improve nutritional status ● Maintain skin integrity ● Promote home and community-based care CHRONIC PANCREATITIS ● An inflammatory disorder characterized by progressive destruction of the pancreas. ● Cells are replaced by fibrous tissue with repeated attacks of pancreatitis pressure within the pancreas increases. The result is obstruction of the pancreatic and common bile ducts and the duodenum. ● There is atrophy of the epithelium of the ducts, inflammation, and destruction of the secreting cells of the pancreas. RISK FACTORS/CAUSES ● Alcohol consumption and malnutrition (major cause) ○ Excessive and prolonged consumption of alcohol ○ Long-term consumption – hypersecretion of protein causing protein plugs and calculi ○ Alcohol has direct toxic effect on the pancreatic cells ● Age 37 to 40 ● Smoking CLINICAL MANIFESTATIONS ● Recurrent attack of severe upper abdominal and back pain with vomiting. ○ Opioids in large doses produces no relief ○ Disease progression aggravates the pain more ● Some chronic pancreatic patients do not experience any pain. ● Weight loss (major problem) will trigger another attack. ● Malabsorption occurs late, stool becomes frequent, frothy, and foul-smelling due to impaired fat digestion (steatorrhea) ● Calcifications occurs due to disease progression, calcium stones form within the ducts. ASSESSMENT AND DIAGNOSTIC FINDIGNS ● Endoscopic retrograde cholangiopancreatography (ERCP) ● Magnetic resonances imaging, CT scans, and Ultrasound ● Glucose tolerance test (evaluates islet of Langerhans cell function, increase level of glucose – diabetes with pancreatitis) ● Increased serum amylase levels ● Steatorrhea SURGICAL MANAGEMENT ● Pancreaticojejunostomy (Rouxen- Y surgery) ● Whipple resection (Pancreaticoduodenectomy) ● Beger or Frey operations ● ○ Remove most of the head of the pancreas except for a shell of pancreatic tissue posteriorly. ○ Provide permanent pain relief and avoid endocrine and exocrine insufficiency. Distal pancreatectomy (Endoscopic & laparoscopic) Note: Patients who undergo surgery for chronic pancreatitis may experience weight gain and improved nutritional status. However, morbidity and mortality after these surgical procedures are high because of the poor physical condition of the patient before surgery and the concomitant presence of cirrhosis. Even after undergoing these surgical procedures, the patient is likely to continue to have pain and impaired digestion secondary to pancreatitis, unless alcohol is avoided completely. THANK YOU FOR LISTENING!