Copy of Omnibus Health Guidelines for Adults Version 2023
advertisement

Disclaimer: The Omnibus Health Guidelines (OHG) are based on best available local and international literature at the time they are written. Evidence is dynamic and continuously evolving, hence, the contents may not accurately reflect evidence which are newly-generated and/or published after the OHG release. The provisions of the OHG are intended to assist target users for implementation and decision-making. When used in patient encounters, they should be interpreted based on the patient’s individual circumstances and applied with sound clinical judgment. Clinicians are expected to maintain discretion and exercise due diligence while upholding the patient’s best interests in the utilization of the OHG. Guidelines should not be interpreted as strict rules on which legal action may be based, nor should they be the sole basis for evaluating insurance claims. Suggested Citation: Department of Health. (2023). The Omnibus Health Guidelines for Adults 20-59 years old ver 2023. Manila, Philippines: Department of Health. Feedback: Contact the Disease Prevention and Control Bureau - Evidence Generation and Management Division at egmd@doh.gov.ph. Editorial Team OHG Technical Team Dr. Mel Anthony Acuavera Dr. Diana Jean Vasquez Dr. Marijuzca Nicolas Dr. Timothy John Bautista Dr. Joy Valerie Catameo Dr. Neil Benjamin Kho Mr. Gerald John Paz Ms. Mita Lourdes Angela Santiago Support Team Dr. Jan Derek Junio Mr. Dan Louie Renz Tating Mr. Angelo Timothy Dawa Mr. Miguel Gaston Agcaoili Ms. Chelsea Danica Bercasio Design and Lay-out Artist Dr. Zashka Alexis Gomez Editor Dr. Ruth Divine Agustin Back to Table of Contents OHG for Adults ver. 2023 | 2 Table of Contents Table of Contents.........................................................................................................................................................................3 Abbreviations and Acronyms.......................................................................................................................................................5 Foreword...................................................................................................................................................................................... 7 Acknowledgements..................................................................................................................................................................... 8 About the Omnibus Health Guidelines (OHG)..............................................................................................................................10 Rationale.............................................................................................................................................................................10 Objectives........................................................................................................................................................................... 10 Development and Update Process...................................................................................................................................... 11 Target Users, Applications, and Uses................................................................................................................................. 11 Expansion Plans..................................................................................................................................................................12 Feedback Process...............................................................................................................................................................12 Section Guide......................................................................................................................................................................13 PART I:.........................................................................................................................................................................................19 The General Wellness and Preventive Measures Section:........................................................................................................ 20 General Principles..............................................................................................................................................................20 Self-care..............................................................................................................................................................................21 Household Care.................................................................................................................................................................. 25 The Supportive Care, First Aid Measures, and Basic Emergency Care Section:...................................................................... 32 General Principles.............................................................................................................................................................. 32 Self-monitoring and Self-testing.......................................................................................................................................32 Supportive Therapies and Symptomatic Relief.................................................................................................................33 First-aid and Basic Emergency Care................................................................................................................................. 34 The General History and Physical Examination Section:...........................................................................................................41 General Principles............................................................................................................................................................... 41 Screening for Red Flags.....................................................................................................................................................42 History Taking.................................................................................................................................................................... 42 Physical Examination.........................................................................................................................................................44 The Screening Services Section:.............................................................................................................................................. 50 General Principles of Screening........................................................................................................................................ 50 Screening Services............................................................................................................................................................. 51 The Immunization Services Section:........................................................................................................................................ 65 General Principles.............................................................................................................................................................. 65 Vaccines for Adults............................................................................................................................................................ 65 Monitoring and Management of Adverse Effects Following Immunization (AEFI)............................................................ 69 The Sexual and Reproductive Health Section:.......................................................................................................................... 72 General Principles.............................................................................................................................................................. 72 Family Planning Services................................................................................................................................................... 72 Assessment of Pregnancy..................................................................................................................................................76 Maternal Health Services................................................................................................................................................... 77 The Diagnosis of Common Conditions in Primary Care Summary Section.............................................................................. 85 General Principles of Diagnosis......................................................................................................................................... 85 Diagnostic Tests in Primary Care...................................................................................................................................... 85 The Treatment of Common Conditions in Primary Care Summary Section............................................................................ 101 General Principles............................................................................................................................................................. 101 Treatment Options in Primary Care.................................................................................................................................. 101 PART II:...................................................................................................................................................................................... 119 Non- Communicable Diseases................................................................................................................................................. 120 Acute Myeloid Leukemia....................................................................................................................................................121 Asthma.............................................................................................................................................................................. 124 Chronic Obstructive Pulmonary Disease......................................................................................................................... 130 Diabetes Mellitus...............................................................................................................................................................135 Dyslipidemia......................................................................................................................................................................142 Generalized Anxiety Disorder........................................................................................................................................... 146 Hepatocellular Carcinoma................................................................................................................................................ 150 Hypertension.....................................................................................................................................................................153 Major Depressive Disorder................................................................................................................................................160 Methamphetamine Use Disorder......................................................................................................................................165 Infectious Diseases.................................................................................................................................................................. 170 Community Acquired Pneumonia (CAP)............................................................................................................................ 171 Coronavirus Disease (COVID-19)....................................................................................................................................... 175 Dengue.............................................................................................................................................................................. 184 Human Immunodeficiency Virus - Acquired Immunodeficiency Syndrome (HIV AIDS).................................................. 188 Infectious Diarrhea........................................................................................................................................................... 194 Leptospirosis.................................................................................................................................................................... 198 Tinea Infection................................................................................................................................................................. 202 Tuberculosis, Pulmonary................................................................................................................................................. 205 National Practice Guidelines Program Products..................................................................................................................... 214 Omnibus Health Guidelines ver. 2023 | 4 Abbreviations and Acronyms AAFP - American Academy of Family Physicians AAO - American Academy of Ophthalmology AAP - American Academy of Pediatrics AAPD - American Academy of Pediatric Dentistry ACOG - American College of Obstetricians and Gynecologists ACC - American College of Cardiology ACP - American College of Physicians ACS - American Cancer Society ADA - American Diabetes Association ADAA - Anxiety and Depression Association of America ADeA - Australian Dental Association AEFI - Adverse Events Following Immunization AGDHAC - Australian Government Department of Health and Aged Care AHA - American Heart Association AO - Administrative Order APA - American Psychiatric Association ARC - American Red Cross ASCVD - Atherosclerotic Cardiovascular Disease ASSIST - Alcohol, Smoking, and Substance Involvement Screening Test ATS - American Thoracic Society AUDIT - Alcohol Use Disorders Identification Test COE - Council of Europe COPD - Chronic Obstructive Pulmonary Disease CSEP - Canadian Society for Exercise Physiology DBM - Department of Budget and Management DDB - Dangerous Drugs Board DHHS - Department of Health and Human Services DVA - Department of Veteran Affairs DENR - Department of Environment and Natural Resources DM - Department Memorandum DO - Department Order DOH - Department of Health DOLE - Department of Labor and Employment ESC - European Society of Cardiology EREID - Emerging and Re-emerging Infectious Diseases FNRI - Food and Nutrition Research Institute FSRH - Faculty of Sexual and Reproductive Healthcare GAD - Generalized Anxiety Disorder GBD - Global Burden of Disease GINA - Global Initiative for Asthma GOLD - Global Initiative for Chronic Lung Disease GSIS - Government Service Insurance System IADT - International Association of Dental Traumatology Omnibus Health Guidelines ver. 2023 | 5 Abbreviations and Acronyms ICE - Institute of Clinical Epidemiology ICRC - International Committee for the Red Cross IDF - International Diabetes Federation IDSA - Infectious Diseases Society of America IDST - Infectious Disease Society of Taiwan IHME - Institute of Health Metrics and Evaluation ISH -International Society of Hypertension JMC - Joint Memorandum Circular JRRMMC - Jose R. Reyes Memorial Medical Center LA - Labor Advisory MOH - Ministry of Health NCEP - National Cholesterol Education Program NICE - National Institute for Health and Care Excellence NIH - National Institutes of Health NTP-MOP - National Tuberculosis Program-Manual of Procedures ORS - Oral Rehydration Salts PCCP - Philippine College of Chest Physicians PCS - Philippine Cancer Society PD - Presidential Decree PHEX - Philippine Guidelines on Periodic Health Examination PHILPEN - Philippine Package of Essential Noncommunicable Disease Interventions PLAS - Philippine Lipid and Atherosclerosis Society PNDF - Philippine National Drug Formulary PPA - Philippine Psychiatric Association PSH - Philippine Society of Hypertension PSMID - Philippine Society for Microbiology and Infectious Diseases RA - Republic Act RACGP - Royal Australian College of General Practitioners RANZCP - Royal Australian and New Zealand College of Psychiatrists SSS - Social Security System UN- United Nations UP - University of the Philippines UK NICE - United Kingdom National Institute for Health and Care Excellence US CDC - United States Centers for Disease Prevention and Control US DVA - United States Department of Veterans Affairs US FDA - United States Food and Drug Administration USPSTF - United States Preventive Services Task Force WHO - World Health Organization Omnibus Health Guidelines ver. 2023 | 6 Foreword The passage of the Republic Act (RA) No. 11223 or the Universal Healthcare Act in 2018 ushered in multiple innovations and reforms within the health sector, with the recognition that inherent to the achievement of true universal health care (UHC) is the strengthening of primary care complemented by the development of functional and integrated healthcare provider networks (HCPN). The Department of Health, through the Disease Prevention and Control Bureau (DPCB), led the development and updating of the Omnibus Health Guidelines (OHG), which is a major policy initiative to ensure the delivery of safe, effective, and person-centered services to all Filipinos of various life stages, with main focus on primary care strengthening (Administrative Order 2022-0018). By consolidating and defining evidence-based service delivery standards using a lifestage approach, the OHG serves as a guide to ensure that every Filipino is offered the best possible care at each opportunity. The OHG embodies what we envision for primary care - “initial-contact, accessible, continuous, comprehensive and coordinated care that is accessible at the time of need including a range of services for all presenting conditions, and the ability to coordinate referrals to other health care providers in the health care delivery system, when necessary”, as defined in the UHC Act. The principles of health promotion, set in the Health Promotion Strategy Framework, along with services encompassing prevention, such as screening and immunization, diagnosis, treatment, rehabilitation, and palliation, and referrals, are enumerated in the OHG. As a scientifically robust and comprehensive reference, the OHG contains links to relevant laws, policies, local and international high-quality clinical practice guidelines (CPGs), manuals, clinician support tools, and other materials, to facilitate well-informed decision-making for various users, such as primary care providers, managers of various settings, and local governments . Because the contents of the OHG are evidence-informed and updated with the standards of care also developed by our local medical societies, the OHG promotes communication and collaboration between primary care providers and specialists - a critical step in the realization of UHC. Further, new health technologies identified in the OHG serve as triggers for initiating processes that enable health financing, including inclusion in the benefit packages of PhilHealth, and health technology assessments by the Health Technology Assessment Council (HTAC). It is my fervent hope that the OHG will be widely disseminated and utilized by clinicians and our partners in health, to help us realize UHC and our DOH 8-point Agenda, in particular - Ligtas, dekalidad, at mapagkalingang serbisyo para sa bawat Pilipino - dahil bawat buhay mahalaga. TEODORO J. HERBOSA, MD Secretary, Department of Health Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 7 Acknowledgements The development and updating of the Omnibus Health Guidelines were made possible through the concerted efforts, commitment, and expertise of the personnel of various Divisions of the Disease Prevention and Control Bureau, headed by the Division Chiefs Dr. Manuel Vallesteros, Dr. Raffy Deray, Dr. Jan Aurelle Llevado, and Dr. Ruth Divine Agustin, overseen by Dir. Maria Elizabeth Caluag and Dir. Jose Gerard Belimac, and led by Dir. Razel Nikka Hao, under the guidance of Assistant Secretary Beverly Lorraine Ho, and Public Health Services Team Undersecretary Maria Rosario Singh-Vergeire. We thank our stakeholders and target users who participated in our surveys and key informant interviews and provided critical feedback for the improvement of the OHG. We also thank our various development partners who dedicated their time and expertise to review the technical contents of the OHG. We acknowledge the invaluable contributions of the members of the DOH Lifestage Technical Working Group (LTWG), including Dr. Noel Espallardo and Dr. Cheridine Oro-Josef of the Philippine Academy of Family Physicians, Dr. Ma. Encarnita Limpin, Dr. Diana Payawal, Dr. Imelda Mateo, Dr. Maaliddin Biruar, and Dr. Dax Ronald Librado of the Philippine College of Physicians, Dr. Domingo S. Bongala, Jr., Dr. Rex Madrigal, Dr. Jorge Concepcion, and Dr. Alejandro Dizon of the Philippine College of Surgeons, Dr. Gil Gonzalez, Dr. Mikaela Erlinda Martinez-Bucu, and Dr. Suzette Munoz of the Philippine Obstetrical and Gynecological Society, Dr. Jeremy Cordero and Dr. Dianne Marie De Jesus of the Philippine College of Emergency Medicine, and Dr. Maria Ysabella Someros and Dr. Larimer Hugo of the Philippine Psychiatric Association. We give our special thanks to the various representatives of the Centers for Health Development and the Ministry of Health - Bangsamoro Autonomous Region in Muslim Mindanao for giving their constructive comments and inputs in various consultation fora for the improvement of the OHG and the development of the Roll-out Guide. We are also grateful to the personnel of the various DOH Central Office Bureaus who gave crucial inputs to improve the OHG. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 8 We acknowledge the following medical societies whose members dedicated their time and expertise to the development and updating of the Omnibus Health Guidelines for Adults. Philippine Academy of Family Physicians (PAFP) Philippine College of Physicians (PCP) Philippine College of Surgeons (PCS) Philippine Obstetrical and Gynecological Society (POGS) Philippine College of Emergency Medicine (PCEM) Philippine Psychiatric Association (PPA) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 9 About the Omnibus Health Guidelines (OHG) Rationale In the past decades, the Department of Health (DOH) issued numerous policies on medical and public health programs and health services that were usually disseminated and carried out using a fragmented, vertical and programmatic manner. The roll-out of the Universal Health Care (UHC) Act called for a shift from this towards a more integrative approach in terms of policy, planning, and health service delivery, with emphasis on the central role of primary care in the achievement of UHC. The UHC Act also paved the way to strengthening the health sector’s appreciation and use of evidence-based standards of care by mandating the DOH to ensure the safety and quality of health services, to “set standards for clinical care through the development, appraisal, and use of clinical practice guidelines in cooperation with professional societies and the academe” (Section 27.c), and to ensure “evidence-informed sectoral policy and planning for UHC” (Section 31). To achieve these, the DOH institutionalized the Expanded National Practice Guidelines Program (NPGP) through Administrative Order (AO) No. 2023-0002, which elucidates a comprehensive framework for the development, appraisal, and implementation of evidence-informed guidelines. In conjunction, the Department issued Administrative Order No. 2022-0018, establishing the Omnibus Health Guidelines as the overarching policy reference for the fulfillment of relevant mandates of the UHC by 1) setting standards of care primarily through the utilization of quality-appraised Clinical Practice Guidelines (CPGs), complemented by other evidence-informed references, 2) facilitating the achievement of technical integration and guiding the functional and efficient linking of services across different levels of care and settings, and 3) upholding primary care-oriented and people-centered care using a life course approach to service delivery. The achievement of UHC, as envisioned in the UHC Act, is the telos of the Omnibus Health Guidelines (OHG), with primary care strengthening as the medium. By identifying what safe, effective, person-centered quality care is for various life stages, the OHG is able to facilitate the achievement of UHC and contribute to the fulfillment of the DOH 8-point agenda, in particular, Agenda 2: ”Ligtas, dekalidad, at mapagkalingang serbisyo” para sa bawat Pilipino”. Objectives The OHG aims to provide comprehensive guidance for an integrated and consolidated approach to health service delivery for various life stages (Child, Adolescent, Adults, Elderly), across the continuum of care– from health promotion, prevention, screening, diagnosis, treatment, rehabilitation, to palliation– in various settings and levels of care (AO No. 2022-0018). Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 10 Development and Update Process The development and updating of the Omnibus Health Guidelines consists of the following general processes: ● ● ● ● Rational priority setting and selection of topic updates based on the DOH 8-point agenda, burden of disease, presence of emerging quality and new evidence, presence of practice variation, and stakeholder feedback; Scoping, review, and appraisal, when applicable, of various references containing standards of care/service delivery standards, including DOH-approved CPGs, international CPGs and guidance documents, DOH policies, and other relevant laws and policies; Synthesis and translation of CPG recommendations and other standards from quality-appraised sources to key provisions in the OHG to create comprehensive guidance across the entire spectrum of care– encompassing health promotion, prevention, screening, diagnosis, treatment, rehabilitation, palliation, and referrals; and Vetting of the technical validity of the updated provisions by the Lifestage Technical Working Group (LTWG), accompanied by multiple consultations with various stakeholders and target users. Target Users, Applications, and Uses The target users of the OHG are the following: ● Clinicians and primary care providers, including physicians, nurses, midwives, and Barangay Health Workers (BHWs), can use the OHG as the main reference for service delivery including the clinical consults, diagnosis, treatment, supportive care and palliation, and referral-enhancing patient care and streamlining workflows; ● Primary care managers, especially those in national government institutions, local governments, and settings-based managers for schools, workplaces, and establishments, can use the OHG as the main reference for strategic planning, management, operations, and resource allocation– aiding in identifying investment needs, gaps, priorities for quality assurance and systems strengthening; ● Health Program Managers can use the OHG as the main reference for designing interventions to meet health outcome targets for more efficient and effective integration of program strategies and provision of quality services; ● The Philippine Health Insurance Corporation (PhilHealth) can use the OHG as a policy basis for development of benefit packages for quality and cost-effective service delivery; ● The Health Technology Assessment Council (HTAC) can use the OHG as a policy basis for identifying priority health technologies for HTA; and ● Other partners of the health sector such as development and humanitarian partners, civil society organizations, and the academe, may also refer to the OHG for the uses listed above, as relevant to their respective roles and functions, in addition to developing and implementing activities related to capacity-building and curriculum enhancement. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 11 Expansion Plans To strengthen and enable our primary care providers to deliver safe, effective, high-quality, and person-centered care, in accordance with the UHC Act, the OHG shall be regularly updated every 3 years, or as frequently as necessary (AO No. 2022-0018). This is to ensure that the OHG contains standards of care supported by the best available and most current evidence and is responsive to the need for guidance for the multitude of conditions encountered in primary care. Annually, the DOH, through Disease Prevention and Control Bureau - Evidence Generation and Management Division (DPCB - EGMD), shall conduct surveys and stakeholder consultations to determine priority topics for updating, obtain feedback for quality improvement, and assess the awareness and utilization of the OHG. Further, to facilitate the implementation and utilization of target users, implementation tools (e.g., clinician support tools) shall be developed and disseminated and implementation, monitoring, and evaluation strategies shall be carried out, following the provisions of AO 2023-0018 and AO 2022-0002. A User Guide shall be developed to facilitate ease of use for the different cadres and managers in primary care. Feedback Process Interested parties or individuals may provide feedback on the OHG in two ways: ● Submit comments and feedback on the contents of the OHG anytime by accomplishing this feedback form; and/or ● Participate in annual surveys or stakeholder consultations. The call to participate in surveys and consultations shall be released through Department Circulars. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 12 Section Guide Figure 1. OHG Navigation Map The 2023 update of the OHG seeks to facilitate a user-friendly and intuitive experience. The version 2023 OHG update is divided into two main parts with multiple sections. The navigation map of the updated OHG is shown in Figure 1. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 13 Part I: General Primary Care is intended to consolidate the health service delivery standards regarding general primary care and is not disease-specific. The Sections in Part I should be used to provide care for all individuals consulting at primary care, whether they are healthy or symptomatic. Part I is comprised of the following: ● General Wellness and Preventive Measures ○ This section contains provisions for Self-care and Household care. Multiple cadres of primary care providers, including BHWs, midwives, nurses, and physicians, can use this as reference in educating adults about general promotive and preventive actions to maintain health and well-being. ● Supportive Care, First Aid Measures, and Basic Emergency Care ○ This section contains provisions on Self-monitoring and Self-testing, Supportive Therapies and Symptomatic Relief, and First-aid and Basic Emergency Care. These provisions can be used to educate individuals about health-seeking behaviors, self-care, and home care for simple conditions. ● General History and Physical Examination ○ This section contains provisions and information that can be used during the actual clinical encounter, including what to ask during the interview and what to look for during physical examination. Red flags are enumerated to identify conditions necessitating immediate attention and referral. Normal findings or values are provided to ensure clinicians are able to distinguish between normal and pathological findings. ● Screening Services ○ This section contains provisions on the screening services that should be offered to eligible groups of adults, based on the latest available evidence. This section is divided into PE-based screening, questionnaire-based screening, and laboratory or imaging-based screening. ● Immunization Services ○ This section contains provisions on the vaccines that should be offered to eligible adults, based on the latest available evidence. Provisions on the monitoring and Management of Adverse Effects Following immunization (AEFI) are also enumerated. ● Sexual and Reproductive Health Services ○ This section contains provisions on sexual and reproductive health services, including family planning and pre-natal and post-natal services. ● Diagnostic Tests in Primary Care: Summary ○ This section consolidates the diagnostic tests for common or high-burden conditions that should be made available or offered in primary care, in order to be able to deliver comprehensive care at initial contact. ● Treatment Options in Primary Care: Summary ○ This section consolidates the medications that should be made available or offered in primary care, in order to be able to deliver comprehensive care at initial contact. Part II: Specific Guidance for Common and High-Burden Diseases in Adults is intended to provide the relevant disease-specific, evidence-based standards of care, ranging from screening to basic emergency care, for patients presenting with signs and symptoms of diseases commonly encountered in primary care. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 14 These standards mainly focus on what needs to be performed, offered, or administered in the primary care context. The diseases are grouped into two sets: Non-communicable Diseases (NCDs) and Infectious Diseases (IDs). Each set contains diseases/conditions arranged in alphabetical order for ease of use. As the OHG is updated, this list will be continuously expanded in order to comprehensively cover the wide range of acute and chronic conditions encountered in primary care. ● Non-Communicable Diseases ○ Acute Myeloid Leukemia ○ Asthma ○ Chronic Obstructive Pulmonary Disease ○ Diabetes Mellitus ○ Dyslipidemia ○ Generalized Anxiety Disorder ○ Hepatocellular Carcinoma ○ Hypertension ○ Major Depressive Disorder ○ Methamphetamine Use Disorder ● Infectious Diseases ○ Community Acquired Pneumonia ○ COVID-19 ○ Dengue ○ Human Immunodeficiency Virus- Acquired Immunodeficiency Syndrome (HIV-AIDS) ○ Infectious Diarrhea ○ Leptospirosis ○ Tinea Infection ○ Tuberculosis, Pulmonary Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 15 What is the OHG? The OHG serves as the overarching policy reference containing consolidated best available evidence-based standards of care across various life stages and various settings. (AO No. 2022-0018, AO No. 2023-0002). The current focus of the OHG is strengthening primary care by consolidating primary care service delivery standards. When is the OHG used? Users of the OHG may consult the document at any point in clinical or public health practice, when in need of guidance on the continuum of care– from health promotion, prevention, screening, diagnosis, treatment, rehabilitation, to palliation and referral. What is the OHG used for? Since the OHG details the “WHATs” of health care provision, the document can be used as a reference for: health service delivery; resource mapping; strategic planning; project/program monitoring; technical and organizational capacity building; and health curriculum enhancement. Who is the OHG for? The OHG can be used as a reference by primary care providers, public health managers, other national government agencies, development and humanitarian partners, civil society organizations, research and academia, students, and patients and their families and communities. How is the OHG made? The OHG development and update process begins with rational priority setting, followed by scoping, review, and appraisal of evidence-based references. Recommendations or statements from these references are plotted into a continuum-of-care matrix until the entire spectrum of care is completed. These are then synthesized and translated into key provisions in the OHG. Finally, the OHG contents are vetted by the Lifestage Technical Working Group alongside various stakeholders and target users. Only after undergoing this sequential process does the DPCB release the OHG for public use. Am I required to follow the guidelines listed in the OHG when treating my patients? What if the test/treatment/intervention is not available where I am? The OHG consolidates best available evidence on standards of care, so following guidelines detailed under the OHG would be aligned with best practices. However, not all settings have the capacity to accommodate specific cases nor are required resources available at all times. Further, because the OHG is updated regularly, the newest safe and efficacious interventions (e.g., medications, tests) are already included but may still be undergoing necessary processes for financing, procurement, and inclusion in the Philippine National Formulary (PNF). There may also be unique characteristics of individuals that make the provisions inapplicable. In these circumstances, healthcare professionals and other stakeholders can do any of these suggested courses of actions, should the need arise: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 16 For clinicians: ● Clinicians are advised to exercise due diligence when applying the provisions of the OHG to their practice. The practice of medicine remains an art and a science. Hence, clinical decision-making, taking into account the patient’s characteristics, values, and preferences, should be paramount; ● Clinicians can be guided by the strength of recommendation for each statement made apparent by the tags placed after each statement (ie. strong or weak/conditional recommendation), and the differences in the strength of language used for each statement (ie. stronger, more active language for strong recommendations vs. weaker, more passive language for weak recommendations); ● Reference hyperlinks are also available for each guideline statement for instances that need deeper investigation on the appropriateness of the provisions to particular cases; and ● Clinicians can be guided by the referral provisions of the OHG to refer patients to a higher/lower level of care. For public health managers and key decision makers: ● The OHG can be used as a reference for scoping/resource mapping, needs assessment, strategic planning, and monitoring and evaluation on the roll-out of different health programs. For non-health professionals/general public: ● Consult with a licensed healthcare professional/team for any health concern. I want to contribute further updates on guidelines stated in the OHG. Where can I submit these? The OHG is updated every three (3) years or as frequently as needed. To submit suggestions for updates/ amendments, accomplish and submit the feedback form. I have other questions about the OHG. Where can I send my queries/concerns? For other inquiries and concerns, you may contact the DPCB - Evidence Generation and Management Division at egmd@doh.gov.ph. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 17 Category Format What changed? The updated format now contains two major parts: General Primary Care and Specific Guidance. Certain texts are clickable and hyperlinked to related sections or to reference documents or relevant tools, forms, or materials. Content The content has been updated to reflect evidence-based standards of care for the key priority programs of the Department of Health, including: Immunization, Reproductive Health, Tuberculosis (TB), HIV-AIDS, Neglected Tropical Diseases and Emerging and Re-Emerging Infectious Disease (EREID), Mental Health, and NCDs. Specific guidance on certain common and high-burden conditions have also been provided, with a brief description of the condition, an overview table, details on signs and symptoms, and enumeration of the evidence-based standards in the spectrum of care, including screening, diagnosis, treatment, palliation/rehabilitation (if applicable), and referral. Recommendations from DOH-approved CPGs, other high-quality international CPGs, and other guidance documents are integrated in various parts of this updated version. The strength of recommendation from the source CPG is indicated (e.g., strong/recommended, weak/conditional) when available, and the actual reference CPGs are indicated and hyperlinked for easier access. Users of CPGs may refer to Figure 1 when interpreting and applying recommendations from CPGs. References in-text are numbered in superscripts and hyperlinked to the source document. A reference list is placed at the end of each section, with references numbered sequentially according to the order of in-text citation, and with relevant hyperlinks. Figure 1. Guide in Interpreting CPG Recommendations Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 18 PART I: General Primary Care This part provides a consolidation of general primary care standards, including preventive and self-care measures for individuals and their households, screening services, immunization services, sexual and reproductive health services, and a general overview of the diagnostic services and therapeutic options that should be offered and/or made available at the primary care level. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 19 The General Wellness and Preventive Measures Section: aims to provide guidance to primary care providers on the advice that can be given to adults and their households about general health and wellness and preventive measures, including healthy lifestyle and self-care practices, household practices, home investments, and community activities. Health is defined by the World Health Organization (WHO) as a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. 1 Further, the WHO defines a related term, “well-being”, as “a positive state experienced by individuals and societies… [which] encompasses quality of life and the ability of people and societies to contribute to the world with a sense of meaning and purpose” 1. To achieve health and well-being and not merely the absence, cure, or control of diseases, a holistic approach anchored on primary healthcare (PHC) is necessary. The OHG contributes to this goal by enumerating health promotion and preventive interventions that can be delivered and taught in primary care, resulting in the betterment of the health and empowerment of individuals, families, and communities. The Republic of the Philippines, as a Member State of the United Nations (UN), is in adherence with the stipulations of the Universal Declaration of Human Rights and the UN Statement of Common Understanding on Human Rights-Based Approaches to Development Cooperation and Programming, which elaborated how human rights standards and principles should be placed in practice and programming guidelines. 2,3 Stipulated in Article 25 of the Universal Declaration of Human Rights is “The Right to Adequate Standard of Living/Basic Needs” which states: “1) Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond his control; 2) Motherhood and childhood are entitled to special care and assistance. All children, whether born in or out of wedlock, shall enjoy the same social protection.” 2 In delivering any healthcare service, providers are reminded to place prime importance on the principles of Article 25, alongside championing other human rights. Should patients require care and/or social services outside of clinical care, providers are advised to attend to their health needs and refer them to the appropriate government agencies to receive other social services/support needed. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 20 General Principles ● ● ● ● Preventive strategies are classified into the following: ○ Primordial prevention: preventing the development of risk factors for disease (e.g., strategies that modify the upstream determinants of chronic diseases such as eating patterns, physical activity, environmental and social determinants of health, usually through legislation or public policies); ○ Primary prevention: preventing the development of disease in individuals who already have one or more risk factors (e.g., immunizations, pre-exposure and post-exposure prophylaxis for certain infectious diseases, adequate treatment of hypertension and dyslipidemia to prevent ischemic heart disease or stroke); ○ Secondary prevention: detecting disease in asymptomatic individuals to treat it early and prevent its progression (e.g., screening for colorectal cancer or cervical cancer); and ○ Tertiary prevention: minimizing complications, improving quality of life, preventing imminent death in the setting of an acute illness (e.g., thrombolysis in stroke or fluid resuscitation and antibiotic administration in septic shock) or disability (e.g., rehabilitation for stroke or heart attack survivors). Always seek to integrate education about general wellness and preventive measures in each patient encounter. Encourage adults to be aware of their rights, including their right to health, autonomy and self-determination, confidentiality, and informed consent. Encourage adults to be responsible for their health, actively seek medical advice, and be involved in shared decision-making with their respective healthcare providers. Self-care Encourage adults to observe the following healthy practices: ● Dental Care. ○ Perform proper dental care by brushing twice a day using the right amount of fluoridated toothpaste (1000-1500 ppm), which is recommended to be the entire brushing surface of a toothbrush, flossing at least once a day, and avoiding rinsing with water after toothbrushing to optimize the preventive effects of fluoride. 3,4 ○ Visit the dentist regularly for oral prophylaxis and oral examination every 6 months or as advised by the dentist (preferably 3 to 4 months based on caries risk assessment high-risk classification). 3,4 ● Diet and Nutrition. Adhere to a healthy dietary pattern, visually guided by Pinggang Pinoy and characterized by the following: 6, 7 ○ Rich in fruits, vegetables, whole grains, fish, and low-fat dairy products; ○ Fortified with micronutrients; ○ Low in cholesterol and saturated fat, with avoidance of trans fat; Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 21 Self-care Reduced daily salt intake to less than 5 grams per day (equivalent to 2300 mg of sodium and just under 1 teaspoon of table salt per day), with use of iodized table salt preferred; ○ Minimal to no intake of processed foods, canned goods, and “fast foods;” and ○ Minimal to no intake of sugar-sweetened foods and beverages, such as donuts, cookies, sweets, fizzy drinks, and juice with added sugar. Exercise. ○ Perform moderate to vigorous aerobic physical activities, consisting of at least 150 minutes per week of accumulated moderate-intensity physical activity or 75 minutes per week of vigorous-intensity physical activity, unless contraindicated, or as prescribed by a physician.8 ○ Replace sedentary time with age-appropriate physical activity of any intensity (including light intensity), to obtain benefits, such as but not limited to, decreasing the risk of developing hypertension and diabetes, preventing obesity, reducing symptoms of anxiety and depression, improving cognitive health, and decreasing the risk of mortality.8,9,10 Infectious Disease Prevention. Observe protective measures against infectious diseases, such as the following, in line with the Water, Sanitation, and Hygiene (WASH) Strategy : ○ Observe proper personal hygiene: ■ Hand Hygiene. Perform proper handwashing with soap and water. Perform disinfection with alcohol if soap and water are unavailable. ■ Body Hygiene. Bathe with soap and water daily. Use shampoo for hair and scalp care. Avoid sharing personal items such as towels, uniforms, headsets/ earphones, slippers, and shoes, among others. ■ Proper respiratory hygiene and cough etiquette. When sneezing or coughing, cover the mouth and nose or cough/sneeze into the elbow when tissue/covering is not available.11,12 ○ Prevention of communicable diseases based on transmission routes ■ Use the appropriate personal protective equipment (PPEs) (e.g. masks, gloves, etc.) as necessary, according to the recommendations of health authorities. ○ Prevention of food- and water-borne diseases ■ Use safe drinking water. ■ Use a sanitary toilet and avoid open defecation practices. ○ Self-protection measures against mosquito-borne diseases ■ Wear light-colored clothes, long sleeves, and long pants if staying outdoors. ■ Apply insect repellent to prevent mosquito-borne diseases. ■ Use screen doors and windows or insecticide-treated screens/ curtains for doors and windows. ■ Use long-lasting insecticide-treated nets (LLIN) at night in malaria-endemic and high-risk areas. ○ Self-protection measures against soil-transmitted helminths/parasitic diseases/other zoonotic diseases (e.g. leptospirosis) ■ Wear slippers/shoes. ○ ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 22 Self-care Avoid wading in or swimming in and using infested freshwater, which may serve as transmission sites for infectious diseases. ■ Wash legs/ feet with soap and water after wading in flood water. ■ Avoid intake of water from possible contaminated water sources. Injury Prevention. Observe injury prevention measures such as the following: ○ Use sports-appropriate protective gear as necessary to prevent injury from sports-related accidents.13 ○ Observe driving practices that promote road safety and prevent road crash-related injuries including the following: ■ Practice road courtesy at all times as a driver, as a passenger, and as a pedestrian, by being aware of traffic signs and strictly following traffic rules and regulations, in accordance with RA No. 4136: “Land Transportation and Traffic Code”. This involves simple and practical measures such as following traffic light rules, using the pedestrian crossing, overpass, underpass, and sidewalks, giving the right of way to an overtaking vehicle, and driving within the set speed limit, etc. 14,15 ■ Use age-appropriate restraints and protective gear in both non-motor (e.g. bicycles) and motor vehicles, including the use of helmets, seatbelts, goggles, and child restraint systems (CRS), in accordance with RA No. 8750: “Seat Belts Use Act of 1999”, RA No. 10054: “Motorcycle Helmet Act of 2009”, and RA No. 11229: “An Act Providing for the Special Protection of Child Passengers in Motor Vehicles and Appropriating Funds Therefor”. 16, 17, 18 ■ Avoid distracted driving and driving under the influence of alcohol, dangerous drugs, and other similar substances, in accordance with RA No. 8750, RA No. 10054, and RA No. 11229.19, 20 ○ Avoid or prevent fireworks-related injuries through the following, in accordance with RA No. 7183: “An Act Regulating the Sale, Manufacture, Distribution and Use of Firecrackers and Other Pyrotechnic Devices” and its revised 2012 Implementing Rules and Regulations (IRR), and Executive Order (EO) No. 28 series of 2017: “Providing for the Regulation and Control of the Use of Firecrackers and Other Pyrotechnic Devices” 21, 22: ■ Avoid using firecrackers outside the designated fireworks zones. ■ Properly supervise children and adolescents regarding the safe use of fireworks ○ Learn and practice water safety skills, including proper swimming techniques, avoiding underwater hazards, and wearing life jackets whenever aboard boats, ships, and similar water vessels.23 Sun protection. Avoid extreme exposure to the sun by wearing protective sunglasses, hats, and umbrellas, and using sunscreen with Sun Protection Factor (SPF). 24 Weight Management. Maintain a healthy weight and a normal BMI of 18.5-22.9 kg/m2.25,26 Mental Health and Wellness. Engage in the following to promote and protect mental health: ○ Perform meditation, stress management, creative activities, and other relaxation techniques. ■ ● ● ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 23 Self-care ● ● ● ○ Maintain good relationships with family and peers. ○ Participate in health activities of the local community. ○ Keep regular routines. ○ Allocate time for working and time for resting. ○ Make time for recreational or leisure activities. ○ Observe self-care practices and approaches. ○ Develop personal skills and foster supportive environments. ○ Actively seek out mental health information and education. Sleep. Attain good-quality sleep lasting 7-9 hours on a regular basis.9 Substance use avoidance or cessation. Avoid the initiation of or stop the following practices: smoking tobacco or using e-cigarettes (vaping), drinking alcoholic beverages and using illicit substances (e.g. marijuana, methamphetamine/shabu, etc.). Safe and Responsible Sexual and Reproductive Health (SRH) Practices. Observe safe and responsible SRH practices such as the following 27, 28: ○ Practice responsible sexual behavior and safer sex, including abstinence, avoidance of having multiple sexual partners, and using contraceptives properly (e.g. proper use of condoms and water-based lubricants, proper use of contraceptive pills, etc.) to prevent unplanned pregnancy and sexually transmitted infections (STIs). ○ Observe other responsible practices such as but not limited to the following: ■ Assert one’s personal rights, practice healthy sexual development and sexuality, and report any form of online and offline gender-based violence and any form of sexual exploitation to appropriate authorities through proper channels. ■ Assert the importance of consent, body autonomy, and setting and respecting physical and mental boundaries at all times. ■ Respect partner’s rights at all times and maintain a good relationship with one’s own partner. ■ Practice Digital Citizenship Education (DCE), in order to actively, positively, and responsibly engage in both online and offline communities. 29 ■ Avoid online and offline risky behaviors and always personally protect one’s own and other’s online information and observe proper online behavior. 29 ■ Use open communication to relay opinions, interests, preferences, and plans and have a mutual decision and participative discussion. ○ Practice gender-responsive behavior, respect gender rights, and seek information on topics including but not limited to the following: ■ Sexual and reproductive health (SRH) ■ Sexual Orientation and Gender Identity and Expression (SOGIE) ■ Gender-based violence (GBV) ■ Risky/abusive behaviors (towards self and others) to avoid violence and injuries ■ Recognition of abusive behaviors ■ Recognition of the cycle of abuse ■ Psychosocial couple-based prevention program Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 24 Self-care ○ ■ Psychoeducation Be aware of the ban on all formal and informal unions of anyone below 18 years, in accordance with RA No. 11596: “An Act Prohibiting the Practice of Child Marriage and Imposing Penalties for Violations Thereof”. 30 Household Care Encourage adults to observe the following practices in their households: ● Health awareness and health seeking behaviors. Maintain appropriate knowledge and understanding of the specific health needs of each family member, including children, adolescents, older persons, and persons with disabilities, and perform the necessary steps to take care of each other’s physical and mental health, including the following: ○ Actively seek healthcare services from their primary care providers. ○ Ensure enrolment of household members in PhilHealth. ○ Facilitate regular wellness visits or follow-up visits of family members with their healthcare providers. ○ Facilitate access to and observance of preventive measures, including vaccination, and necessary medical tests, medications, or non-pharmacologic treatments. ● Hygiene and Sanitation. Observe sanitary and hygienic practices in the household such as the following: ○ Observe safe and proper food preparation such as keeping food clean, separating raw and cooked food, cooking thoroughly, keeping food at safe temperatures (e.g. refrigerating food below 4℃, freezing food below -18℃), and using safe and clean water and raw materials to avoid spoilage and food poisoning.31 ○ Observe proper personal hygiene. ○ Use sanitary toilets. Abandon open defecation practices. ○ Observe proper waste handling and disposal practices, in compliance with RA No. 9003 “Ecological Solid Waste Management Act of 2000” 32, RA No. 6969 “Toxic Substances and Hazardous and Nuclear Wastes Control Act of 1990” 33, and relevant LGU ordinances, through: ■ Waste segregation according to the following solid waste classification (Table 1) 32,34 : ■ Waste management by: ● Composting of leftover foods, vegetables, peels, etc. ● Recycling or converting items into reusable materials ● Proper disposal of household chemicals, used bulbs, old appliances, batteries and other products containing harmful substances guided by the manufacturer’s instruction manual. ○ Regularly perform cleaning and pest control, including rodent and vermin control Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 25 Household Care Table 1. Solid Waste Classification Classification: Definition/ Examples: Compostable (Nabubulok) includes kitchen waste, vegetable and fruit peelings Recyclable (Nareresiklo/ nabebenta) scrap metal, non-ferrous scrap metals, tin cans, aluminum, glass bottles, plastic bottles, corrugated cardboard, newspaper, office paper Non-recyclable/ Residual (Hindi nabubulok) waste materials that cannot be recycled or decomposed (e.g. used plastic or paper cups, broken glass, food wrappers, plastic bags) Special Waste Household Household waste that requires treatment before disposal, including waste electrical Hazardous waste or electronic equipment, paint cans, thinners, batteries, power banks, etc. Household Disposable masks, gloves, sharps, any other waste of an individual who has an Healthcare waste infectious disease Eliminate all open water reservoirs which may become breeding grounds for mosquitoes in the home environment. ○ Avoid or minimize indoor and outdoor pollution, smoke, and vape emissions and maintain adequate ventilation by: ■ Cessation of smoking and vaping, avoidance of burning garbage and dried leaves, cessation of biomass fuel use, and avoidance of exposure to exhaust from vehicles 35, 36, in accordance with RA No. 8749 “Philippine Clean Air Act”. 37 ■ Ensuring that spaces adjacent to openable windows are free from toxic gases and other pollutants. ■ Using ventilating fans/electric fans when the supply of fresh air is not enough or cannot be supplied by natural ventilation. ■ Ensuring exhaust fans/air extractors are operated continuously in an occupied room. ■ Ensuring that exhaust fans/ air extractors are regularly cleaned and maintained in good condition. ■ Ensuring that household furniture equipment is not blocking the airflow across the rooms and physical barriers that can impede airflow are removed. Nurturing and Supportive Environment. Foster a safe, nurturing, supportive, and respectful household13, in accordance with PD No. 603 through the following 38 : ○ Spend time talking about or processing each other's interests and experiences. ○ Use appropriate words and offer praise to show care to family members. ○ Ensure open communication lines where members feel safe to express their opinions and emotions. ○ Show role model behavior to all household members, especially to children and adolescents, including: ■ Avoiding consumption or use of tobacco, alcohol, or any other substance within the household. ○ ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 26 Household Care Prohibiting children and adolescents from using, purchasing, selling, trading and distributing tobacco products, heated tobacco products and vapor products, alcoholic beverages and illegal substances, among others, in accordance with RA No. 9211 “Tobacco Regulation Act of 2003; RA No. 11467 “The National Internal Revenue Code of 1997, as amended”. 39, 40 ■ Avoiding violence at all times. ○ Encourage members to develop, determine, and express their gender identity, and provide emotional support in a non-discriminatory, gender-affirming, developmentally appropriate, safe, and inclusive household and environment. ○ Show pregnant members affection by offering encouragement to seek professional care, take breaks and naps, and consume healthy food. In addition, offer help in caring for the newborn and encourage and support them to breastfeed during the postnatal period. ○ Discuss crisis situations using honest language to ease anxiety and fear. ○ Seek help from family and peers, mental health service providers (e.g. allied health professionals such as psychologists, psychometricians, or members of the trained to provide mental health services), and other community support groups when negative life events occur (i.e. violence, conflict, parental loss, abuse). ○ Support household members with any existing health conditions by encouraging them to: ■ Keep in touch with family, friends, or people who care for them. ■ Identify people whom they can contact for support anytime. ■ Ensure that they adhere to prescribed medications or non-pharmacologic treatments, including counseling. ■ Follow up with a healthcare provider or support group regularly. Positive Parenting. Use positive approaches when educating children and adolescents about acceptable and unacceptable behavior (e.g. communicating calmly with the child in case of conflict and not resorting to corporal or physical punishment) and perform the following activities, as appropriate: ○ Spend quality ‘one-on-one time’ with children and adolescents to strengthen the relationship, understand their feelings, and talk about their interests, experiences, and plans, and make mutual decisions. ○ Reinforce Digital Citizenship Education (DCE) by developing, following, and routinely revisiting a Family Media Use Plan to limit and monitor social media use.29 ○ Seek advice from experts (e.g. licensed psychologists or psychiatrists) on parenting skills that are appropriate for managing challenging behaviors or behavioral disorders in children and adolescents. Responsible Pet Ownership. Prevent rabies and other zoonotic diseases through responsible pet ownership practices and handling of animals, in coordination with Local Government Units (LGUs), such as the following: ○ Protect and promote the welfare of pets and animals and avoidance of their abuse, maltreatment, cruelty and exploitation, in accordance with RA No. 8485 “Animal Welfare Act of 1998, as amended, and its revised IRR”. 41 ■ ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 27 Household Care Provide pets and animals with food and water that are clean, adequate, and appropriate, and provide shelter or living conditions that are safe and comfortable. 41 ■ Regularly vaccinate pets against rabies and maintain the registration card containing all vaccination-related information for accurate record purposes in accordance with RA No. 9482 “Anti-Rabies Act of 2007”. 42 ■ Prevent pets from roaming the streets or any public place without a leash. 42 ■ Immediately notify within twenty-four (24) hours to concerned officials for investigation or appropriate action for any pet biting incident and for the pet to be placed under the observation of a government or private veterinarian. 42 ■ Bring a bite victim immediately to the nearest clinic or animal bite center. ■ Wash hands with soap and water after touching or handling pets and animals and their surroundings. Safe Use of Household Drugs, Chemicals and Products. Safely manage drugs, chemicals, and other household products in the following manner: ○ Only use products registered and approved by the Department of Trade and Industry (DTI) and the Food and Drug Administration (FDA) (e.g. FDA-notified cosmetic products; FDA-registered household/urban hazardous products (HUHS) including dishwashing soaps, laundry detergents, cleaners and disinfectants; FDA-approved trichloroisocyanuric acid (TCCA) products) , in accordance with RA No. 9711 “Food and Drug Administration Act of 2009". 43 ○ Follow the manufacturer’s instructions and precautions printed on the product label regarding the use, handling, storage, and disposal of household chemicals and products. ○ Use the original containers of potentially dangerous products with their original product labels and avoid transferring them to another container. ○ Do not reuse containers of HUHS and HUPs for food and drinking water storage. ○ Ensure that HUHS not intended for children’s use and household/urban pesticides (HUPs) are stored out of children’s reach and away from places where cross-contamination with food may occur. ○ Keep flammable products well-insulated and out of reach of children and pets. ○ Use appropriate PPE (e.g. gloves) when handling or using chemicals. ○ Ensure that adverse events resulting from intentional or unintentional exposure to cosmetic, TCCA, HUHS and HUP products are reported to the Marketing Authorization Holder and/or FDA and any exposed household member is brought to a healthcare provider for timely and appropriate management. ○ Avoid the use or purchase of mercury-containing devices such as mercury thermometers and mercury sphygmomanometers. Support for Community Programs and Activities. Participate in community programs, health promotion, and disease prevention and control programs or activities, such as the following: ○ Community health clubs based on risk factors or known disease and community support groups (e.g. parenting support groups, caregiver support groups). ■ ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 28 Household Care ○ Various health promotion and disease prevention and control activities such as but not limited to: ■ Mass Drug Administration (MDA) activities for neglected tropical diseases ■ Selective Deworming activities for adults belonging to special populations (e.g. farmers, military, paramilitary personnel, etc), particularly for adults living in Schistosomiasis-endemic areas and adults living in filariasis-endemic provinces; ■ Community oral health programs and activities, including, but not limited to, oral health education and toothbrushing drills, oral health screening, early detection, caries risk assessment, and application of fluoride varnish or silver diamine fluoride. ■ Community activities on emergency preparedness and response, in accordance with RA No. 10121 “Philippine Disaster Risk Reduction and Management Act of 2010”44 and the Manual of Operations on Disaster Risk Reduction and Management in Health in the Province-Wide and City-Wide Health System 45 such as the following: ● Medical and Public Health Component Services and Sample Activities in Response ○ Maternal and Child Health ■ Provide immediate and postpartum care services ■ Coordinate access to human milk banks ○ Prevention and control of Communicable Diseases ■ Practice of isolation ■ Continuously provide the following: ● Insecticide, treated bed nets, and facemask ● Medical prophylaxis ● Anti-tuberculosis drugs ○ Minimum Initial Service Package for Sexual and Reproductive Health ■ Provide emergency birthing kits, hygiene kits, women’s kits, family planning commodities, condoms, anti-retroviral drugs ■ Establish conjugal rooms ■ Counseling services particularly for pregnant adolescents, including their partners ○ Management of injuries ■ Provide trauma kits, first aid kits, other medical supplies ■ Refer patient to higher level facility for the necessary management ○ Control of non-communicable diseases ■ Provide medicine for hypertension, diabetes, etc. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 29 Household Care Provide Tsekap kit (blood pressure apparatus, stethoscope, etc.) to medical team Community activities intended to prevent infectious diseases such as but not limited to: ● “Enhanced 4S Strategy” according to DOH Administrative 2018-0021 for the prevention of dengue and other infectious diseases transmitted by Aedes mosquitoes. 46 ● Rabies and animal bite prevention. ● Preventive chemotherapy for endemic infections including filariasis. ● Active case-finding activities including symptom screening and contact investigation if household or close contact of a person with Tuberculosis disease or any other infectious disease meriting case finding and contact tracing. ● Government immunization initiatives against vaccine-preventable diseases, including routine vaccination and vaccination during public health emergencies (PHE) such as Coronavirus Disease 2019 (COVID-19). Health promotion and advocacy initiatives and capacity development activities from reputable health institutions, academe, and other partner or civil society organizations: Community parenting or caregiving activities and programs, including family development sessions and caregiver well-being sessions. ■ ■ ■ ■ References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. World Health Organisation. Health Promotion Glossary of Terms 2021. www.who.int. Published December 6, 2021. Accessed November 29, 2023. https://www.who.int/publications/i/item/9789240038349 United Nations. Universal Declaration of Human Rights. N.d. Accessed December 9, 2023. https://hrbaportal.org/list-of-human-rights/ United Nations Population Fund. The Human Rights-Based Approach. N.d. Accessed December 9, 2023. https://www.unfpa.org/human-rights-based-approach?fbclid=IwAR2Fz1qVeI4_LD4e58Pu-Mh6LhGP1-EDl7mX2hWBG25mMA54q361bPI RpHw Australian Dental Association. ADA Guidelines for the Use of Fluoride. Published November 20, 2020. Accessed December 13, 2023. https://www.ada.org.au/Fluoride-guidelines-Doc.aspx American Academy of Pediatric Dentistry. Caries-Risk Assessment and Management for Infants, Children, and Adolescents. Published 2022. Accessed December 13, 2023. https://www.aapd.org/globalassets/media/policies_guidelines/bp_cariesriskassessment.pdf Food and Nutrition Research Institute. Pinggang Pinoy. Published August 23, 2016. Accessed December 13, 2023. https://www.fnri.dost.gov.ph/index.php/tools-and-standard/pinggang-pinoy Philippine Lipid and Atherosclerosis Society. Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. Published 2020. Accessed December 13, 2023. https://drive.google.com/file/d/1-_k8Uk9Lct56jT5T8xUcFQZoBAv_z8VL/view WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. https://iris.who.int/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1 Ross R, Chaput JP, Giangregorio LM, et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism. 2020;45(10 (Suppl. 2)):S57-S102. doi:https://doi.org/10.1139/apnm-2020-0467 World Health Organization. Physical Activity. Published 2022. Accessed December 16, 2023. https://www.who.int/news-room/fact-sheets/detail/physical-activity WHO guidelines on tuberculosis infection prevention and control: 2019 update. Geneva: World Health Organization; 2019. https://iris.who.int/bitstream/handle/10665/311259/9789241550512-eng.pdf?sequence=5&isAllowed=y U.S. Centers for Disease Prevention and Control. Coughing and Sneezing. Published October 10, 2023. Accessed December 13, 2023. https://www.cdc.gov/hygiene/personal-hygiene/coughing-sneezing.html#:~:text=To%20help%20stop%20the%20spread,your%20elb ow%2C%20not%20your%20hands Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 30 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. Global Accelerated Action for the Health of Adolescents (AA-HA!): guidance to support country implementation. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO. https://iris.who.int/bitstream/handle/10665/255415/9789241512343-eng.pdf Republic Act No. 4136 “Land Transportation and Traffic Code” Save LIVES - A road safety technical package. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/publications/i/item/save-lives-a-road-safety-technical-package Republic Act No. 8750 “Seat Belts Use Act of 1999” Republic Act No. 10054 “Motorcycle Helmet Act of 2009” Republic Act No. 11229 “An Act Providing for the Special Protection of Child Passengers in Motor Vehicles and Appropriating Funds Thereof” Republic Act No. 10913 “Anti-Distracted Driving Act” Republic Act No. 10586 “Anti-Drunk and Drugged Driving Act of 2013” RA No. 7183 “An Act Regulating the Sale, Manufacture, Distribution and Use of Firecrackers and Other Pyrotechnic Devices” and its revised 2012 Implementing Rules and Regulations (IRR) Executive Order No. 28 series of 2017 “Providing for the Regulation and Control of the Use of Firecrackers and Other Pyrotechnic Devices U.S. Centers for Disease Prevention and Control. Healthy and Safe Swimming Communications Toolkit. Published May 1, 2023. Accessed December 12, 2023. https://www.cdc.gov/healthywater/swimming/safe-swimming-week/toolkit.html American Academy of Pediatrics. Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents (4th Edition). American Academy of Pediatrics; 2017. https://doi.org/10.1542/9781610020237 Philippine Association for the Study of Overweight and Obesity. Know Your BMI Calculator. Published 2020. Accessed December 13, 2023. https://obesity.org.ph/know-your-bmi/ World Health Organization. Obesity: Preventing and Managing the Global Epidemic. World Health Organization; 2000. https://books.google.com.ph/books?id=AvnqOsqv9doC&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=fa lse Republic Act No. 10354 "The Responsible Parenthood and Reproductive Health Act of 2012″ WHO consolidated guideline on self-care interventions for health: sexual and reproductive health and rights. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. https://www.ncbi.nlm.nih.gov/books/NBK544164/pdf/Bookshelf_NBK544164.pdf Council of Europe. Digital Citizenship Education Handbook. Council of Europe; January 2019. https://rm.coe.int/16809382f9 Republic Act No. 11596: “An Act Prohibiting the Practice of Child Marriage and Imposing Penalties for Violations Thereof” U.S. Food and Drug Administration. Refrigerator Thermometers - Cold Facts about Food Safety. Published February 17, 2022. Accessed December 12, 2023. https://www.fda.gov/food/buy-store-serve-safe-food/refrigerator-thermometers-cold-facts-about-food-safety Republic Act No. 9003 “Ecological Solid Waste Management Act of 2000" Republic Act No. 6969 “Toxic Substances and Hazardous and Nuclear Wastes Control Act of 1990" Department of Environment and Natural Resources - Environmental Management Bureau. Waste Segregation Advisory. N.d. Accessed December 16, 2023. https://emb.gov.ph/waste-segregation-advisory/ Global Initiative for Asthma. 2023 GINA Report. Published July 10, 2023. Accessed December 12, 2023. https://ginasthma.org/2023-gina-main-report/ Global Initiative for Chronic Lung Disease. 2024 GOLD Report. Published December 1, 2023. Accessed December 13, 2023 https://goldcopd.org/2024-gold-report/ Republic Act No. 8749 “Philippine Clean Air Act” Presidential Decree No. 603 “The Child and Youth Welfare Code Republic Act No. 9211 “Tobacco Regulation Act of 2003” Republic Act No. 11467 “The National Internal Revenue Code of 1997, as amended” Republic Act No. 8485 “Animal Welfare Act of 1998, as amended, and its revised IRR” Republic Act No. 9482 “Anti-Rabies Act of 2007” Republic Act No. 9711 “Food and Drug Administration Act of 2009" Republic Act No. 10121 “Philippine Disaster Risk Reduction and Management Act of 2010” Department of Health. Manual of Operations on Disaster Risk Reduction and Management in Health in the Province-wide and City-wideHealth System. Published June 2023. Accessed December 12, 2023. https://drive.google.com/file/d/1hPW4YX0DCIC4zJdDt7GUYFh2TIgPG0Ds/view Department of Health. Administrative Order 2018 - 0021. Guidelines for the Nationwide Implementation of the Enhanced 4S-Strategy against Dengue, Chikungunva and Zika. Published July 25, 2018. Accessed December 12, 2023. https://doh.gov.ph/sites/default/files/health_programs/ao2018-0021.pdf Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 31 The Supportive Care, First Aid Measures, and Basic Emergency Care Section: aims to provide guidance on the advice that can be taught to adults and their households about self-monitoring and self-testing, supportive therapies, general first-aid measures, and basic emergency care for lay people. General Principles ● ● ● ● Encourage all asymptomatic adults to seek consultation with their primary care provider at least annually. Encourage all adults experiencing symptoms to consult at the nearest primary care facility or healthcare provider for proper assessment and management. Teach adults how to properly perform self-testing and self-monitoring and how to use appropriate supportive therapies for applicable conditions. Teach adults how to perform first-aid measures and seek basic emergency care as necessary. Self-monitoring and Self-testing Teach adults how to check and monitor their vital signs at home and do home tests or self-tests for certain conditions. ● ● Vital signs ○ Blood Pressure. Home blood pressure monitoring in patients with suspected or confirmed hypertension or for monitoring response to BP-lowering drugs 1-3 or in pregnant patients who are diagnosed with gestational hypertension or preeclampsia 2,3. ○ Pulse rate. Pulse rate determination, if clinically indicated, in patients who experience palpitations, in patients who are suspected or diagnosed with rhythm abnormalities (e.g. atrial fibrillation), or in patients who are maintained on heart-rate lowering drugs (e.g. beta-blockers).1,2,3 ○ Temperature. Temperature monitoring in patients who feel febrile or to monitor response to treatment (e.g. fever lysis) ○ Oxygen saturation. Peripheral oxygen saturation monitoring (SpO2) in patients who are considered suspect, probable, or confirmed COVID-19 cases who are on home isolation, or in patients with cardiopulmonary diseases (such as COPD and pulmonary hypertension) who are on oxygen home therapy. Home tests/maneuvers for certain conditions. ○ Self-monitoring of blood glucose using home glucose meter/glucometer: for diabetic patients, especially if they are on insulin as maintenance medication or are pregnant and have chronic diabetes or gestational diabetes.4 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 32 Self-monitoring and Self-testing ○ ○ ○ ○ Pregnancy testing using home pregnancy kits: for women of reproductive age who are experiencing signs and symptoms such as late menstrual period, breast tenderness, nausea or vomiting, weight change, fatigue, mood changes, changes in eating habits and frequent urination.5 Breast self-awareness: for women to familiarize themselves with the normal appearance and feel of one’s breasts. Immediately consult with a healthcare provider if any change (e.g. pain, a mass, new onset of nipple discharge, or redness) is noticed 6,7. Self-administered COVID-19 antigen testing using FDA-approved kits: for symptomatic individuals, within 7 days from onset of symptoms, especially if the capacity for timely RT-PCR results is limited or not available. 8 HIV Self-testing: for at risk individuals. 9,10 Supportive Therapies and Symptomatic Relief Teach adults how to properly use supportive therapies and symptom-relieving medications, such as the following, when applicable: ● Non-pharmacologic supportive therapies. ○ Adequate rest/sleep ○ Proper diet and nutrition ○ Increased water intake/oral hydration if ill and if without water intake restrictions due to a medical condition (e.g. congestive heart failure, dialysis-requiring chronic kidney disease); ○ Tepid sponge bath for fever ○ Cold compress for contusion ● Non-prescription or over-the counter (OTC) medications. ○ Provide guidance and teach necessary precautions to patients regarding the use of the following common non-prescription/over-the-counter (OTC) medications for symptom relief to avoid underdosing/overdosing, minimize adverse effects, and prevent drug interactions: ■ Antipyretics for fever ● Paracetamol 325 to 650 mg orally or rectally every four to six hours (the maximum total daily dose is 4 g per day).11,12 ■ Analgesics for pain relief (observe caution when using non-steroidal anti-inflammatory drugs (NSAIDs) in patients with kidney disease or gastrointestinal bleeding; avoid in patients with allergies to NSAIDs) ● Paracetamol 325 to 650 mg orally or rectally every four to six hours (the maximum total daily dose is 4 g per day).11,12 ● Oral Ibuprofen 200 mg every 4 to 6 hours as needed; if no relief, may increase to 400 mg every 4 to 6 hours as needed; maximum dose: 1.2 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 33 Supportive Therapies and Symptomatic Relief ■ ■ g/day. Use for >10 days is not recommended unless directed by the healthcare provider.12,13 ● Mefenamic acid 500 mg orally once then 250 mg orally every 6 hours as needed; usually not to exceed 1 week.11, 14 Cold medications for nasal congestion ● Phenylephrine 10 mg orally every 4 hours with a maximum dose of 60 mg per 24 hours15, usually in combination with chlorpheniramine12 and/or paracetamol. Mucolytics or antitussives for cough ● Oral Ambroxol with daily dose of 30 mg to 120 mg taken in 2 to 3 divided doses16 as mucolytic ● Carbocisteine orally with an initial 2,250 mg daily in divided doses, may be decreased to 1,500 mg daily in divided doses when a satisfactory response is obtained17 as mucolytic ● Oral Butamirate as 50 mg tablet, 2 or 3 tabs daily at intervals of 8 or 12 hours 12,18 as antitussive First-aid and Basic Emergency Care Teach adults about the recognition of signs and symptoms needing immediate consultation with a healthcare provider, the proper way of providing first-aid care, and the administration of basic emergency care by trained individuals. ● Signs and symptoms needing immediate consultation. Advice adults to consult at the nearest health facility upon experiencing the following symptoms or conditions, which may be life- and/or limb-threatening: ○ Any of the following signs and symptoms 19,20: ■ Acute neurologic symptoms such as loss of consciousness, altered mental status, dizziness, facial asymmetry, slurring of speech, and new-onset weakness or loss of sensation, seizure, or convulsions ■ Agitated and/or aggressive behavior or suicidal ideation/behavior ■ Acute vision loss ■ Eye injury/foreign body ■ Acute chest pain ■ Acute dental pain ■ Any other severe pain ■ Difficulty in breathing ■ Chest retractions ■ Contractions, pain, or bleeding in late pregnancy ○ Any of the following, accompanied by fever21,22,23: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 34 First-aid and Basic Emergency Care Living in an area where malaria is endemic; History of travel to a malaria endemic area; History of recent malaria infection in the previous months Documented history of Plasmodium vivax infection; History of blood transfusion in the previous month(s) or any dental or surgical procedure ■ Headache ■ Body malaise ■ Myalgia (lower back, arms, and legs) ■ Arthralgia ■ Retro-orbital pain ■ Anorexia ■ Nausea ■ Vomiting ■ Diarrhea ■ Flushed skin ■ Rash (petechial, Hermann's sign) ■ Abdominal pain ■ Open wounds Any of the three cardinal signs of leprosy24 ■ Hypopigmentation of the skin; ■ Thickening of peripheral nerves with loss of sensation; or ■ Positive slit-skin smear upon screening. Any of the following TB signs and symptoms 25,26: ■ At least 2 weeks of cough; ■ Unexplained fever; ■ Night sweats; ■ Unexplained weight loss. Any of the following signs and symptoms of sexually transmitted diseases: ■ Vaginal/penile/anal discharge characterized by: ● presence of foul odor ● persistent pruritus ● burning sensation during urination ● greenish (pus-like) appearance ● painful intercourse (dyspareunia) ● post-coital bleeding ■ Painful or painless genital sores ■ Oral viral and fungal infection (leukoplakia, candidiasis, herpes zoster) Inhalation, ingestion, and/or exposure to harmful substances19 Trauma and associated injuries or symptoms such as the following19,27: ■ ■ ■ ■ ■ ○ ○ ○ ○ ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 35 First-aid and Basic Emergency Care Loss of consciousness, altered mental status, or seizures Difficulty of breathing Bleeding, expanding hematoma, or signs of shock (e.g. pallor, cold extremities) Traumatic dental injuries that result in subluxation, extrusion, lateral luxation, intrusion, avulsion of permanent teeth, and root fracture caused by sporting events, falls, motor vehicle accidents, or interpersonal violence ■ Abdominal pain and/or enlargement ■ Pain or limitation in motion of neck or extremities ■ Burns especially those involving the head and neck, hand, feet or groin area First aid care kit. Encourage all adults and their respective households to prepare and maintain a first-aid kit with the following contents28: ○ First aid manual ○ Plasters, sterile gauze dressings, sterile eye dressings, cotton balls and cotton-tipped swabs, bandages, safety pins, disposable sterile gloves, tweezers, scissors, antiseptic solution, antiseptic cleansing wipes, antiseptic cream, sticky tape, thermometer (preferably digital), painkillers such as paracetamol (or infant paracetamol for children), aspirin (not to be given to children under 16), or ibuprofen, antihistamine cream or tablets, distilled water for cleaning wounds, eyewash, and eye bath; ○ Personal or maintenance medications ○ Epinephrine autoinjector or Epinephrine vial with appropriate syringe for individuals who are at risk of anaphylaxis First aid measures. Teach adults to administer first-aid measures for the following conditions: ○ Animal bites (e.g., dog bites)29 ■ Immediately perform proper wound care, including washing with soap and water. ■ Seek consultation at the nearest DOH - Certified Animal Bite Treatment Center/Animal Bite Center for safe and effective post-exposure anti-rabies vaccination, anti-tetanus vaccination, antibiotics, and health education. ○ Dental Injuries. ■ Rinse avulsed permanent tooth gently in milk, saline, or saliva and take care not to touch the root with fingers. If unable to replant the tooth, place in physiologic storage medium like milk, saliva or saline and seek immediate dental treatment.27 ■ Seek immediate medical attention for uncontrolled or profuse bleeding of a tooth extraction site. ○ Minor closed wounds (e.g., bruise/contusion).30 ■ Apply a cold compress or cold pack to the area for at least 10-20 minutes. ■ Elevate the injured area to a tolerable level to prevent swelling. ○ Minor open wounds (e.g., abrasion, superficial laceration/cuts).30 ■ Apply direct pressure while wearing gloves if there is external bleeding from wound. ■ Rinse with running water then wash with soap and water once the bleeding stops. ■ Apply antibiotic ointment, cream, or gel, as prescribed by a primary care provider. ■ ■ ■ ■ ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 36 First-aid and Basic Emergency Care Cover with a sterile gauze pad or an adhesive bandage. Consult at the nearest health facility if the wound is deep, extensive, persistently bleeding, or at high risk of infection (e.g. puncture wound from a nail). Minor, superficial or first-degree non-chemical burns.30 ■ Stop the burning by removing the person from the source or removing the source from the person. ■ Cool the burned area with cool or cold water (but not direct ice or ice water application) for at least 10 minutes. ■ Avoid removing the cover of the blister to protect the burnt skin. ■ Cover with loose sterile dressing. ■ Apply silver sulfadiazine, as prescribed by a primary care provider, for non-infected burns, if without allergy to sulfonamides and if the medications are available. ■ Consult at the nearest health facility if the burn is deep, extensive, involves critical areas (hands, feet, groin, head, face, circumferential burns), a dirty wound is sustained, there are signs of infection (e.g. fever, purulent discharge) or there is associated difficulty of breathing. Muscle, bone, or joint injuries30: ■ Rest: Limit the use of the injured part. ■ Immobilize: Apply a splint or elastic bandage to limit motion. ■ Apply cold compress to the area for at least 10-20 mins every 6-8 hours in the first 24 hours after injury. ■ Elevate the injured body part to a tolerable level to reduce swelling. ■ Consult at the nearest health facility if any of the following are present: difficulty of breathing, an open fracture, deformity, abnormal movement or inability to move, coldness or numbness, involvement of the head, neck or spine, or the injury is suspected to be significant due to its cause (e.g. fall, vehicular accident). Poisoning and Chemical burns31 ■ Eye exposure. ● Immediately irrigate the affected eye with clear running tap water, occasionally lifting and lowering the lids then seek medical attention. ● Avoid rubbing the eyes. ■ Inhalation. ● Remove the victim from the source of the hazardous substance and bring him/her to an open space with fresh air. ● If the victim vomits, turn him/her to his/her side to avoid choking. ● Seek medical attention immediately. ■ Ingestion. ● Do not induce vomiting. ● Seek medical attention immediately. ■ Skin exposure. ■ ■ ○ ○ ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 37 First-aid and Basic Emergency Care ● ● Inspect and note all areas of the body that came into contact or have been contaminated by the substance, removing the clothes if necessary. Wash or irrigate all contaminated areas with clear running tap water and seek medical attention immediately. Disasters. ■ If trained in Psychological First-Aid (PFA), facilitate and/or coordinate the provision of PFA and other psychosocial services to disaster-affected populations following the key principles of PFA (a sense of safety, calming, a sense of self, and community efficacy, connectedness, and hope, etc.). Safe provision of basic emergency care, cardiopulmonary resuscitation (CPR), and psychosocial assistance. Teach adults to recognize the following emergencies and how to provide help safely: ○ Common emergencies.30,32 ■ Cardiac arrest: sudden loss of consciousness and unresponsiveness and absence or abnormal breathing (e.g. gasping), and absence of pulse. ■ Possible acute stroke: unilateral weakness of face (e.g. drooping), arm, grip or speech disturbance ■ Possible acute coronary syndrome: acute nontraumatic chest pain ■ Respiratory distress: shortness of breath, gasping, rapid shallow breathing, painful or uncomfortable breathing ■ Life-threatening bleeding ■ Shock: drowsiness or altered mental status, excessive thirst, palpitations, difficulty of breathing, weakness, cold extremities, pallor ■ Drowning ■ Vehicular accidents ○ Safe provision of help to emergency victims.32 ■ Seek opportunities to learn or participate in first aid and basic emergency care training, including lay Basic Life Support (BLS), cardiopulmonary resuscitation (CPR), and basic disaster risk reduction and management from qualified experts or trainers. ■ Always check for the safety of the scene to the self before extending help to others. ■ Immediately call for help and activate emergency services upon witnessing any emergency to facilitate the transport of the victim to the nearest healthcare facility. ■ If trained, perform lay BLS on victims in cardiac arrest after ensuring that the scene is safe and calling for help. ○ Help for violence/abuse victims. Advise adults to do the following when encountering or witnessing interpersonal violence or abuse: ■ Immediately call 911 for help. ■ Talk to a friend, a family member, a trusted teacher, a doctor, or a counselor. ○ ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 38 First-aid and Basic Emergency Care ■ ■ Familiarize and access existing referral mechanisms in the locality Collaborate with the Multidisciplinary Team (MDTs) References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. Philippine Society of Hypertension & Philippine Heart Association. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 14, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021-3104. doi:https://doi.org/10.1093/eurheartj/ehy339 International Society of Hypertension. Global Hypertension Practice Guidelines. Hypertension. 75(6), 1334-1357. Published 2020. Accessed December 14, 2023. https://www.ahajournals.org/doi/epub/10.1161/HYPERTENSIONAHA.120.15026 American Diabetes Association. Standards of Medical Care for Diabetes. Published 2022. Accessed December 14, 2023 https://diabetesjournals.org/care/issue/45/Supplement_1 Department of Health. Philippine Clinical Standards Manual on Family Planning. Published 2014. Accessed December 14, 2023. https://platform.who.int/docs/default-source/mca-documents/policy-documents/operational-guidance/PHL-RH-32-01-OPERATIONA LGUIDANCE-2014-eng-Clinical-Standards-Manual-Family-Planning.pdf American College of Obstetricians and Gynecologists. Breast Cancer Risk Assessment and Screening in Average-Risk Women. Published 2017. Accessed December 14, 2023. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/07/breast-cancer-risk-assessment-and-screening-in -average-risk-women Oeffinger KC, Fontham ETH, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk. JAMA. 2015;314(15):1599. doi:https://doi.org/10.1001/jama.2015.12783 Department of Health. Department Memorandum 2022-0033: Guidelines on the Use of Self-Administered Antigen Testing for COVID-19. Published 2022. Accessed December 14, 2023.. https://doh.gov.ph/sites/default/files/health-update/dm2022-0033.pdf World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. Published July 16, 2021. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789240031593 Department of Health. Administrative Order 2022-0035: Guidelines in the Implementation of Differentiated HIV Testing Services.Published August 22, 2022. Accessed December 14, 2023. https://dmas.doh.gov.ph:8083/Rest/GetFile?id=724488 UpToDate. Acetaminophen (paracetamol): Drug information. N.d. Accessed December 14, 2023. https://www.uptodate.com/contents/acetaminophen-paracetamol-drug-information?search=paracetamol%20fever%20adult&sourc e=search_result&selectedTitle=2~150&usage_type=default&display_rank=2 Department of Health. Philippine National Drug Formulary: Essential Medicines List. Published 2008. Accessed December 14, 2023. https://www.fda.gov.ph/wp-content/uploads/2021/03/PNDF-2008.pdf UpToDate. Ibuprofen: Drug information. N.d. Accessed December 14, 2023. https://www.uptodate.com/contents/ibuprofen-drug-information?search=ibuprofen%20pain%20adult&source=search_result&select edTitle=2~150&usage_type=default&display_rank=2# Drugs.Com. Mefenamic acid. N.d. Accessed December 14, 2023. https://www.drugs.com/mtm/mefenamic-acid.html#dosage Drugs.Com. Phenylephrine. N.d. Accessed December 14, 2023. https://www.drugs.com/mtm/phenylephrine.html#dosage Drugs.Com. Ambroxol Hydrochloride. N.d. Accessed December 14, 2023. https://www.drugs.com/ambroxol.html#dosage MIMS. Carbocisteine. N.d. Accessed December 14, 2023. https://www.mims.com/philippines/drug/info/carbocisteine?mtype=generic MIMS. Butamirate. N.d. Accessed December 14, 2023. https://www.mims.com/philippines/drug/info/butamirate Basic emergency care: approach to the acutely ill and injured. Geneva: World Health Organization and the International Committee of the Red Cross 2018. Licence: CC BY-NC-SA 3.0 IGO. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/275635/9789241513081-eng.pdf?sequence=1 U.K. National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management. Published May 01, 2019. Updated April 13, 2022. Accessed December 14, 2023. https://www.nice.org.uk/guidance/ng128 U.S. Centers for Disease Prevention and Control. Definitions of Symptoms for Reportable Illnesses. Published 2017. Accessed December 14, 2023. https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html Department of Health. Clinical Practice Guideline on the Diagnosis, Management and Prevention of Dengue for Adult and Pediatric Filipinos. Published 2023. Accessed December 14, 2023. https://drive.google.com/file/d/1dsYIHm4UibfyP7FyFJeWsRQ5jXMZZNJp/view World Health Organization. Malaria. Published 2023. Accessed December 14, 2023. https://www.who.int/news-room/fact-sheets/detail/malaria World Health Organization. Leprosy. Published 2023. Accessed December 14, 2023. https://www.who.int/news-room/fact-sheets/detail/leprosy University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (Phase 3): Screening for Infectious Diseases. Published October 13, 2023. Accessed December 14, 2023. https://drive.google.com/file/d/1up5YnRyy6S5YpTsGgRoZHo4XDCOSrjR7/view Department of Health. NTP Manual of Procedures, 6th Ed. Published 2021. Accessed December 14, 2023. https://ntp.doh.gov.ph/download/ntp-mop-6th-edition/ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 39 27. 28. 29. 30. 31. 32. Bourguignon C, Cohenca N, Lauridsen E, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dental Traumatology. 2020;36(4). doi:https://doi.org/10.1111/edt.12578 National Health Service (NHS). (2021). What should I keep in my first aid kit? Published April 7, 2021. Accessed December 14, 2023. https://www.nhs.uk/common-health-questions/accidents-first-aid-and-treatments/what-should-i-keep-in-my-first-aid-kit/ Department of Health. Administrative Order 2018-0013: Revised Guidelines on the Management of Rabies Exposures. Published April 16, 2018. Accessed December 14, 2023. https://www.psmid.org/wp-content/uploads/2020/03/CPG-rabies-AO-2018-0013.pdf American Red Cross. First Aid/CPR/AED Participants Manual. Published 2016. Accessed December 14, 2023. http://cdn1.thprd.org/pdfs2/document4085.pdf U.S. Centers for Disease Prevention and Control. First Aid Procedures. Published 2018. Accessed December 14, 2023. https://www.cdc.gov/niosh/npg/firstaid.html Merchant, R. M., Topjian, A. A., Panchal, A. R., Cheng, A., Aziz, K., Berg, K. M., Lavonas, E. J., Magid, D. J., & Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups (2020). Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(16_suppl_2), S337–S357. https://doi.org/10.1161/CIR.0000000000000918 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 40 The General History and Physical Examination Section: aims to provide guidance to the primary care providers on the conduct of a standard comprehensive history-taking and physical examination. Properly conducted history-taking and physical examination documented in a standard medical record are central to accurate diagnosis and management and guide healthcare providers in creating a person-centered care plan that underpins safe, effective, and quality service delivery. Normal and abnormal findings are shown in this section to enhance the acuity of healthcare providers in recognizing signs of diseases or disorders. Integrated into the history and physical examination are important symptoms and signs of diseases and tools used by the priority programs of the Department of Health. General Principles ● ● ● ● Patient autonomy. Respect the patient’s autonomy and act in his/her best interests. Informed consent. Fundamental to each patient-physician encounter is informed consent. Always seek to ensure that the patient thoroughly understands the risks and benefits of any diagnostic maneuver or therapeutic intervention and secure informed consent. Privacy and confidentiality. Always ensure that the patient’s privacy is protected, and confidentiality of patient information is maintained. When laws or policies require reporting of cases to protect the public’s health (e.g., mandatory reporting of notifiable diseases as mandated by RA No. 11332 "Law on Reporting of Communicable Diseases" 1), ensure that measures are followed to maintain data security and confidentiality. Comprehensive health profile for holistic care. Primary care providers should seek to obtain a complete health profile of individuals consulting at primary care through comprehensive history-taking and physical examination. Due to time limitations, resource constraints, or patient-specific factors, a single encounter may not be enough to obtain all the information or perform all the maneuvers. Hence, certain parts of the history-taking and the PE may be done in different encounters, as part of continuing care. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 41 Screening for Red Flags Before proceeding to comprehensive history taking and physical examination, screen the patient for conditions that would necessitate immediate or emergent medical attention, assessment, management, and/or referral to a higher level of care. Screening for red flags to guide the triaging of the patient may be done by any trained member of the healthcare team. Examples of red flags are listed below. ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● Chest pain/ discomfort/ heaviness, either in the center of the chest, radiating to left arm or chest, when climbing up hill or in a hurry, not relieved by rest or medication, and/or lasts over an hour or more; Slurred speech; Facial Asymmetry; Weakness/ Numbness on arm on one side of the body; Not oriented to time, person, place; Seizure or convulsion; Loss/ decreased level of consciousness; Difficulty of breathing; Act of self-harm/ Suicide; Agitated and/or aggressive behavior; Eye injury/ foreign body injury in the eye; or Severe injuries/ signs of abuse Severe or persistent abdominal pain Severe allergic reaction Loss of consciousness Profuse bleeding History Taking Obtain the patient’s history in order in a systematic manner and document the patient’s story accurately in the health record. ● ● Obtain a comprehensive history at the first outpatient consultation to facilitate the completion of an individual’s complete health profile and identify the various risk factors that need to be addressed for preventive health and holistic care. In certain instances, a focused approach instead of extended history-taking may be enough, such as during consults that necessitate urgent or emergent care or during follow-up consults. Primary care providers should adjust the history-taking approach according to the patient’s clinical status and health needs. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 42 History Taking ● Ensure the completion of the health record with the following sections. The standardized Adult Health Examination Form2 can be used to ensure the completeness and accuracy of the health record. ○ Patient Identification. Obtain and record personal information accurately to ensure patient safety and avoid fatal errors. ○ General Survey, Vital Signs, and Anthropometrics. The General Survey is a quick assessment of the patient’s consciousness, coherence, and cardiorespiratory condition. Obtain the vital signs and anthropometrics of the patient (e.g., height, weight, and BMI) to aid in the overall assessment of the patient during the encounter. ○ Chief Complaint. Ask the patient about the main reason for the consult to guide the differential diagnosis. The chief complaint should be the first problem in the problem list. However, since individuals are also encouraged to regularly consult their primary care providers, at least annually, even when they are asymptomatic – in these cases, the chief complaint or reason for consultation can be recorded as a “well visit”, “annual health exam”, or a “general check-up”. ■ History of Present Illness (HPI). This is the most essential part of the diagnostic examination. Ask the patient to describe, quantify, and identify the chronology of their symptoms clearly and how it has affected their current activities of daily living. ○ Past Medical and Surgical History. Ask about an individual’s past medical and surgical history to gain better context and identify pre-existing conditions that may affect their current and future health risks such as the following: ■ Chronic medical illnesses and allergies ■ Prior or current infectious diseases ■ Prior operations ■ Prior and current injuries ■ Prior hospitalizations ○ Obstetric and Gynecologic History (for females). Probe female patients regarding the details of their obstetric and gynecologic history. This would include details on their menstrual history, any previous or present pregnancies, contraceptive use, history of pap smear and/ or cervical cancer screening. The information gathered can help identify whether the patient will need to be referred for any pre- or post- natal care services, or other sexual or reproductive health screening or interventions. ○ Personal and Social History (PSH). Probe details of the personal and social history of the patient, particularly risk factors such as smoking, vaping, alcoholic intake, substance use, dietary intake, physical activity, sexual practices, and mental health risk factors or traumatic life events, and environmental exposures. ○ Family History (FH). Ask about the family history to identify hereditary/genetically linked diseases or risk factors (e.g., certain cancers, cardiovascular diseases, etc.,) or diseases that are transmitted among family members or close household contacts. An accurate Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 43 History Taking ○ ○ family history helps assess risk and can help identify whether an individual will benefit from screening or prophylactic interventions. Preventive Care Services/Immunization. Ask about prior screening tests including dates and results and vaccinations. Review of Systems (ROS). Oftentimes, clinicians are tempted to skip the ROS due to lack of time. However, it is essential to ask for salient symptoms by each system or anatomic region to guide the differential diagnosis and identify any additional problem that might not have been identified in the preceding parts of the history-taking. Record all pertinent positives and pertinent negatives. Physical Examination Perform physical examination in a systematic manner and document the physical findings in the health record (Table 2). ● ● ● ● Be guided by the information gained from the individual’s history in identifying anatomic sites or organ systems that need focused attention or a more thorough examination (e.g., a complaint or a symptom of difficulty of breathing on exertion should prompt a more careful examination of the cardiovascular and pulmonary systems; a complaint of a breast lump should prompt a clinical breast examination). Ensure a professional and empathic approach and respect a patient’s need for modesty. Secure a patient’s informed consent for sensitive physical maneuvers. The standardized Adult Health Examination Form2 can be used to ensure the completeness and accuracy of the health record. Specific sections may be accomplished by the appropriate cadres of healthcare providers in the healthcare care facility or in the primary care provider network. Table 2. Physical Examination for Adults Category Component General Survey Vital signs Blood pressure Method/Device Normal Values/Findings3-10 Inspection Conscious, coherent, not in distress Validated oscillometric upper arm BP device Systolic Blood Pressure: 90-120 mmHg 3-5 Diastolic Blood Pressure: 60-80 mmHg 3-5 Note: Elevated BP on screening physical confirmation that prompts suspicion of Hypertension should be confirmed through repeat office BP Measurement using a validated oscillometric BP device with an appropriately-sized upper arm cuff, according to the Standard BP Measurement Protocol or through Ambulatory BP Monitoring (ABPM)4 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 44 Category Anthropometrics Component Method/Device Normal Values/Findings3-10 Respiratory Rate Inspection 12-20 breaths per minute Heart Rate Auscultation 60-100 beats per minute Temperature Non-mercury thermometer (e.g. digital axillary thermometer, tympanic, or infrared) Oral: 35.8–37.3ºC Axillary: 34.8–36.3ºC Tympanic: 36.1–37.9ºC Rectal: 36.8–38.2ºC Infrared: 36.1-37.2 ºC6 Peripheral Oxygen Saturation (if clinically warranted) Pulse oximeter 95-99% at room air Height Beam Type Adult Weighing Scale (Physician’s Platform Scale) Weight Beam Type Adult Weighing Scale (Physician’s Platform Scale) Waist Circumference Non-extensible/nonstretchable tape measure Females: < 80 cm Males: <90cm Body Mass Index (BMI) Calculation: (weight in kg) (height in m)2 Asia-Pacific Cut-offs 7,8: Underweight <18.5 kg/m2 Normal 18.5-22.9 kg/m2 Overweight 23-24.9 kg/m2 Obese ≥25 kg/m2 Note: In pregnant women, use pre-pregnancy BMI to determine healthy weight gain 9 Skin Head, Eyes, Ears, Neck, and Throat (HEENT) Head Eyes Back to Table of Contents Inspection, Palpation Uniform skin color, no pallor, no jaundice, no rashes or skin lesions, warm to touch, no loss/ decrease in sensation Inspection, Palpation, Auscultation, Otoscopy, Fundoscopy, Oral Examination Normocephalic, no deformities, no depression nor tenderness No lesion, bruises and scaling, no signs of hair loss No masses, ptosis, lesions No discharges, excessive lacrimation No tenderness Pink palpebral conjunctiva, anicteric sclera Pupils are equally reactive to light and accommodation Omnibus Health Guidelines ver. 2023 | 45 Category Component Method/Device Normal Values/Findings3-10 Full extraocular muscle movement Ears No swelling or discharge No tragal tenderness No discoloration, thickening, perforations, lesions and masses Intact gross hearing On otoscopy: No foreign bodies, non-hyperemic external auditory canal, tympanic membrane intact with a good cone of light Nose Symmetrical without deformities Nasal septum at midline Pink nasal mucosa without swelling, bleeding or exudates No tenderness over frontal and maxillary sinuses Throat, including mouth, oral mucosa, and neck Lips are light reddish and moist Oral mucosa is pinkish with no ulcerations Complete dentition, no cavities, no oral or mucosal lesions or ulcerations Gums are pinkish. Tongue midline Palatine tonsils are pinkish without lesions, exudates, erythema, and enlargement Uvula is midline Supple Neck Symmetrical, no limitations in range of motion Trachea is at the midline. No palpable lymph nodes or masses Thyroid gland is barely palpable Normal jugular venous pressure (JVP) No bruit Chest/Lungs Inspection, Palpation, Percussion, Auscultation, Symmetrical chest expansion No inspiratory contraction of the accessory muscles, supraclavicular retraction, or intercostal retractions Normal tactile and vocal fremitus Bronchovesicular breath sounds heard all over the chest Heart Inspection, Palpation, Percussion, Auscultation Adynamic precordium, no precordial bulge Normal/undisplaced Point of Maximal Impulse (PMI) No thrills and heaves Normal S1 and S2 with normal rate and regular rhythm, no murmurs Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 46 Category Component Method/Device Normal Values/Findings3-10 Abdomen Inspection, Auscultation, Percussion, Palpation No discoloration, no visible peristalsis/ pulsation Normoactive bowel sounds Tympanic in all four quadrants No shifting dullness or fluid wave Abdomen is flat, soft and non-tender, no palpable masses Liver edge and spleen non-palpable No costovertebral angle tenderness Extremities Inspection, palpation, auscultation Nails are white with pinkish nail beds. No clubbing No cyanosis, no pallor Extremities are warm, no edema Full and equal pulses on all four extremities, no bruits No joint swelling, no gross deformities, with full range of motion No numbing (intact and equal tactile senses) Normal motor strength on all extremities Inspection, Palpation Mons Pubis and Pubic Hair: clear with normal hair distribution; no nits or lice Vulva: ● Labia majora and minora: symmetrical, smooth to somewhat wrinkled, unbroken, slightly pigmented skin surface; no ecchymosis, excoriation, nodules, swelling, rash, lesions; no swelling, pain, induration or purulent discharge upon palpation ● Multiparous women: majora are separated and minora more prominent Clitoris: approximately 2 cm in length and 0.5 cm in diameter; no lesions Urethral Meatus: slitlike in appearance, midline, no discharge, swelling, and redness, about the size of a pea, should not cause pain and/or result in any urethral discharge upon palpation Vaginal Introitus: pink and moist, patent without bulging ● Nulliparous with intact hymen, vaginal muscle tone tight and strong ● Multiparous: with remaining hymen, vaginal muscle tone diminished ● Normal Vaginal Discharge – white and free of foul odor (some white clumps may be seen—mass clamps of epithelial cells) Perineum: Smooth. Slightly darkened ● Upon Palpation: smooth and firm (homogenous in nulliparous, thinner in parous women) ● Well-healed episiotomy scar is also within normal limits for parous women Female External Genitalia Mons Pubis and Pubic Hair Vulva Clitoris Urethral Meatus Vaginal Introitus Perineum and Anus Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 47 Category Male External Genitalia Component Method/Device General Pubic Region Penis Urethra Scrotum Testes Inguinal Region Inspection, Palpation, Back to Table of Contents Normal Values/Findings3-10 Scrotum: thin loose skin over muscular layer, hairless or with infrequent hair ● Size varies, may appear pendulous ● Skin color - often more deeply pigmented than body skin; often reddened in red-haired individuals ● Sac is divided in half by septum, left scrotal sac may be longer than the right ● Contracts in cold temperature; relaxes in warm temperature ● Rugose surface ● Non-tender, no pitting Testicle: Present in each scrotal sac, ● Equal in size, approximately 4x3x2 cm ● Left testis may normally be lower than the right Mildly sensitive to gentle/moderate compression ● but not tender ● Firm but not hard, smooth, rubbery, ovoid in shape, ● Free from nodules, swelling or bulges Omnibus Health Guidelines ver. 2023 | 48 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Republic Act No. 113332 “Mandatory Reporting of Notifiable Diseases and Health Events of Public Health Concern Act" Department of Health. Health Examination Form for Adults 20 to 59 years old. Published 2023. Accessed December 7, 2023. https://drive.google.com/file/d/1IzYtn7lnG5_pSWN7MO46N0TRu62Wy4Om/view Unger et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension, 75(6), 1334-1357. PMID: 32370572. 10.1161/HYPERTENSIONAHA.120.15026. 2020. https://www.ahajournals.org/doi/epub/10.1161/HYPERTENSIONAHA.120.15026 Philippine Society of Hypertension & Philippine Heart Association. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 14, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021-3104. doi:https://doi.org/10.1093/eurheartj/ehy339 Lapum JL, Verkuyl M, Garcia W, St-Amant O, Tan A. Vital Sign Measurement across the Lifespan - 1st Canadian Edition.; 2018. https://pressbooks.library.torontomu.ca/vitalsign/ Philippine Association for the Study of Overweight and Obesity. Know Your BMI Calculator. Published 2020. Accessed December 13, 2023. https://obesity.org.ph/know-your-bmi/ World Health Organization. Obesity: Preventing and Managing the Global Epidemic. World Health Organization; 2000. https://books.google.com.ph/books?id=AvnqOsqv9doC&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=fa lse US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Behavioral Counseling Interventions for Healthy Weight and Weight Gain in Pregnancy: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(20):2087-2093. https://doi:10.1001/jama.2021.6949 Bickley, L. S., Szilagyi, P. G., & Hoffman, R. M. Bates' guide to physical examination and history taking. 12th ed. Wolters Kluwer; 2017 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 49 The Screening Services Section: aims to provide guidance to primary care providers on the appropriate screening services for adults. Screening services are essential in the provision of preventive health services and are intended to “identify people in an apparently healthy population who are at higher risk of a health problem or a condition, so that an early treatment or intervention can be offered”1. General Principles of Screening ● ● ● Screening is a form of secondary prevention - it allows early detection of a disease to improve the chances for positive health outcomes Screening is different from early diagnosis: in screening, testing is offered to asymptomatic individuals while in early diagnosis, testing is done to detect disease in symptomatic individuals. Primary care managers and providers are encouraged to utilize the Wilson and Jungner’s principles of screening1 when planning, developing, financing, or implementing screening programs anchored on evidence-based screening interventions: ○ The condition should be an important health problem. ○ There should be an accepted treatment for patients with recognized disease. ○ Facilities for diagnosis and treatment should be available. ○ There should be a recognizable latent or early symptomatic phase. ○ There should be a suitable test or examination. ○ The test should be acceptable to the population. ○ The natural history of the condition, including development from latent to declared disease, should be adequately understood. ○ There should be an agreed policy on whom to treat as patients. ○ The cost of case-finding (including a diagnosis and treatment of patients diagnosed) should be economically balanced in relation to possible expenditure on medical care as a whole. ○ Case-finding should be a continuous process and not a “once and for all” project. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 50 Screening Services ● ● ● ● ● ● Offer screening services to all eligible adults. Select the appropriate screening tests individualized to a patient’s risk profile. Screening questionnaires can be used to screen certain conditions during the actual patient encounter in the primary care clinic (Table 3). Some screening maneuvers are already integrated in the routine physical examination (e.g., screening for hypertension by BP measurement at every clinic visit, screening for obesity by measurement of anthropometrics) but additional screening maneuvers may be performed depending on the risk profile of the patient (Table 4). Other screening tests or procedures may necessitate referral to an appropriate facility or performance by a qualified/trained health personnel if the test/procedure is not available within the primary care clinic (Table 5). Ensure that a care cascade, including a functional referral system within the healthcare provider network (HCPN) is in place for continuity of care after screening. Table 3. Screening Tools/ Questionnaires Conditions being Screened Alcohol use (unhealthy alcohol use) Screening Tool/Questionnaire Strength of Recommendation (if available) and Reference Guideline Alcohol Use Disorders Identification Test (AUDIT) Tool Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) Tool2 Strong (PHEX 1 2021) 3 PhilPEN Risk Factor Assessment PhilPEN 201219 Anxiety Generalized Anxiety Disorder-7 (GAD-7) Scale4 Strong (PHEX 2021)5 Cardiovascular Disease Risk ASCVD Risk Calculator6 2020 ISH Global Hypertension Practice Guidelines7 WHO Cardiovascular Disease (CVD) Risk Screening and Assessment Tool WHO 20208 Chronic Obstructive Pulmonary Disease (COPD) (among patients with symptoms) COPD Diagnostic Questionnaire COPD Population Screener Lung Function Questionnaire CAPTURE Screening Tool Weak (2023 Philippine Clinical Practice Guidelines for the Management of COPD)9 Dental Caries Caries Risk Assessment UK Department of Health and Social Care 202110 Depression Patient Health Questionnaire 9 (PHQ-9) for HCWs11 (CES-D) for Caregivers and Ill Adults Strong (PHEX 2021)5 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 51 Conditions being Screened Screening Tool/Questionnaire Strength of Recommendation (if available) and Reference Guideline (GDS-15) for Older Adults12 High-risk Sexual Behavior Sexual Risk Survey Safe Sex Behavior Questionnaire(SSBQ) Sexual Health Practices Self-Efficacy Scale Sexual Health Practices Self-Efficacy Scale Condom use errors/ Problem survey (CUES) Correct Condom Use Self Efficacy Scale (CCUSS) UCLA Multidimensional Condom Attitudes Scale (MCAS) Hypersexual Behavior Inventory (HBI) Hypersexual Disorder Screening Inventory (HDSI) Weak (PHEX 1 2021) 3 Mental, Neurologic and Behavioral Disorders; Psychiatric Emergencies Directed Assessment at Primary Care according to WHO mhGAP Intervention Guide – Version 2.0 WHO 201613 Musculoskeletal Disease Gait, Arms, Legs, and Spine (GALS) locomotor screening Weak (PHEX 2023)14 Nicotine Dependencies in Current Smokers Fagerstrom Test IA (evidence obtained from systematic review of relevant randomized controlled trials; there is good evidence to support the recommendation) (2014 PCCP Philippine Clinical Practice Guidelines on Diagnosis and Treatment of Tobacco Use and Dependence) 15 Obesity Body Mass Index (BMI) Waist Circumference (WC) Waist-Hip Ratio (WHR) Strong (for BMI) Weak (for WC) Weak (for WHR) (PHEX 3 2023)16 Physical Inactivity Physical Activity Vital Sign (PAVS) Questionnaire Strong (PHEX 2023)14 Substance Use Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) Tool Strong (PHEX 2021)5 Suicide Columbia-Suicide Severity Rating Scale (C-SSRS) 2017 PPA Consensus Treatment Guidelines on Major Depressive Disorder17 Tobacco Use Screen during history-taking Strong (for screening) (PHEX 2021)5 Grade A (USPSTF 2021) 18 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 52 Conditions being Screened Work-related Musculoskeletal Disorders Screening Tool/Questionnaire Strength of Recommendation (if available) and Reference Guideline PhilPEN Risk Factor Assessment PhilPEN 201219 Rapid Upper Limb Assessment (RULA) Rapid Entire Body Assessment (REBA) Weak (PHEX 2023)14 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 53 Table 4. Screening Maneuvers in PE Conditions being Screened Eligible Population Screening Maneuver Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings Breast Cancer All women 50 to 69 years old Biennial Clinical Breast Examination (CBE) Strong (PHEX 2021)20 CBE: No nipple discharge, no retractions, symmetric, no dimpling, no palpable mass or nodules (findings should be correlated with the physiologic changes associated with the menstrual cycle) CBE: Nipple discharge, nipple retraction, asymmetry, dimpling, pain, palpable mass or nodules (Note: findings should be correlated with the physiologic changes associated with the menstrual cycle) Cataract Adults with risk factors (e.g. hypertension, diabetes, ocular trauma, obesity) Visual acuity testing Weak (AAO 2021)21 VA 20/20 Clear lens32 If VA is 20/40 -20/100 with or without improvement in pinhole or if if VA is 20/200 or worse For near vision, if <J4 using Jaeger chart Lens opacity Comprehensive Eye Evaluation Adults aged 40 who do not have risk factors for eye disease External examination Visual acuity testing using far and near vision charts (e.g. Snellen’s Chart, Sloan, HOTV for literate LEA symbols for illiterate; Jaeger or similar near vision chart)] Visual fields by confrontation Weak (AAO 2020) 22 VA 20/20 or J1, no visual cuts,pupils are equally reactive to light and accommodation, full Extraocular muscle (EOM) range of motion; no masses, ptosis, lesions; no discharges, excessive lacrimation; no tenderness; pink palpebral conjunctiva, anicteric sclera32 Decreased visual acuity, visual field cuts, asymmetric pupils, limited EOM range of motion, masses, discharge, redness, or tenderness Pupillary function (e.g., size Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 54 Conditions being Screened Eligible Population Screening Maneuver Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings and response to light, relative afferent pupillary defect) Ocular alignment and motility (e.g., cover/uncover test, alternate cover test, ductions and versions) Fundoscopy People Living with HIV with symptoms of CMV retinitis Dental Infection Asymptomatic adults Annual visual inspection Strong (PHEX 2023) 23 Visual inspection: normal Visual Inspection: swollen gums, apparent bleeding, tooth decay Diabetic retinopathy Adults with type 1 or type 2 diabetes mellitus Fundoscopy within 5 years after the onset of diabetes (for type 1) or at the time of the diabetes diagnosis (for type 2) B (ADA 2022)24 No arterial narrowing 32 Cotton wool spots, microaneurysm, intraretinal hemorrhages, macular edema, neovascularization, etc. Familial Hypercholesterolemia Asymptomatic adults Screening for family history of premature cardiovascular disease (e.g. myocardial infarction, ischemic stroke, peripheral arterial disease or sudden cardiac death before the age of 55 years in males and 65 in females) and stigmata through physical Strong (PHEX 2021)25 PE: Normal PE: corneal arcus in those aged 45 years or younger, tendon xanthoma, xanthelasma Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 55 Conditions being Screened Eligible Population Screening Maneuver Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings examination Hypertensive retinopathy Adults with grade 2 or 3 hypertension Fundoscopy Class I (ESC 2018) 26 No arterial narrowing, hemorrhages or exudates 32 Arteriolar constriction, arteriovenous nicking, flame-shaped hemorrhages, cotton wool spots, yellow hard exudates, optic disk edema Glaucoma Adults with family history of glaucoma,type 2 diabetes mellitus, myopia, elevated intraocular pressure (IOP) Visual acuity testing Weak (AAO 2020)27,28,29 No visual field cuts Visual field cuts Clear optic disk margins Increased optic disk to cup ratio Normal intraocular pressure (IOP): 12-21 mmHg Elevated intraocular pressure Normal findings Discoloration, masses, persistent nodule or ulcer, which may be red or white patches, swelling or persistent sores, lump in the neck area Fundoscopy IOP measurement Oral Cancer Adults aged 35 years and older who are smokers and/or alcohol drinkers Back to Table of Contents Visual and tactile inspection once every 3 years by trained health workers Strong (PHEX 2021) 20 Closed angle Omnibus Health Guidelines ver. 2023 | 56 Table 5. Screening Laboratory Tests and Procedures Conditions being Screened Eligible Population Screening Test to be Offered at Primary Care Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings Asymptomatic Bacteriuria Apparently healthy pregnant women Urine Culture Weak (PHEX 2023)23 Urine Culture: negative Urine Culture: positive for specific organism/s Breast Cancer All women 50 to 69 years old Mammography every 1 to 2 years Strong (PHEX 2021)20 Mammography: negative (BIRADS Category I) Mammography: BI-RADS Category 2-6 (findings may be benign or malignant) Cervical Cancer Women aged 30 to 65 years old Every 3 years with cervical cytology alone or every 5 years with high-risk HPV testing alone Strong (PHEX 2021)20 Cytology/Pap Smear: negative (normal) Cytology/Pap Smear: positive (abnormal) HPV testing: negative HPV testing: positive VIA: negative / no acetowhite area VIA: positive / with acetowhite areas OR Every 5 years with high-risk HPV testing in combination with cytology (co-testing) OR Every 3 years using visual inspection with acetic acid, as an alternative to Pap smear, among Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 57 Conditions being Screened Eligible Population Screening Test to be Offered at Primary Care Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings asymptomatic women Chlamydia and Gonorrhea Adults high risk for Chlamydia and Gonorrhea (e.g. men with HIV infection, non-monogamous relationship without condom use, age<25 years with 2 or more sexual partners in the past year, sex partner with active or previous STI, with previous or coexisting STI, douching within the past year, commercial sex workers, cervical ectopy) Nucleic Acid Amplification Test (NAAT) Strong (PHEX 2023)23 NAAT: negative NAAT: positive Colorectal Cancer Adults 50 years old and above Annual Fecal Occult Blood Test (FOBT) or Fecal Immunohistochemical Test (FIT), followed by colonoscopy Strong (PHEX 2021)20 FOBT or FIT: negative FOBT or FIT: positive Colonoscopy: normal Colonoscopy: polyps, masses, precancerous growths, cancer Adults aged 40 years and above, or younger if with risk factors (e.g. adults 20-39 years old with CVD risk of 10% and above OR who are overweight or obese OR who have 1 or more additional risk factors for diabetes) Fasting Blood Sugar (FBS) Strong (FBS) (PHEX 2023)16 Weak (HbA1c) (PHEX 2023)16 FBS: <100 mg/dL or <5.6 mmol/L Pre-diabetes ● FBS: 100-125 mg/dL or 5.6-6.9 mmol/L ● HbA1c: 5.7-6.4% Asymptomatic adults 40 to 75 Lipid Profile (must Diabetes Mellitus Dyslipidemia Back to Table of Contents HbA1c HbA1c: ≤5.6% Diabetes: ● FBS: ⋝126 mg/dl or ⋝7 mmol/L ● HbA1c: ⋝6.5% Conditional (PHEX 1 Lipid Profile: Lipid Profile: Omnibus Health Guidelines ver. 2023 | 58 Conditions being Screened Gastric Cancer Hepatitis B Eligible Population Screening Test to be Offered at Primary Care Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings years old with one or more CV risk factors (e.g. DM, HTN, Smoking Hx) include Total Cholesterol, LDL Cholesterol, HDL Cholesterol, Triglycerides) 2021)3 ● Optimal LDL cholesterol: <100mg/dL ● Near optimal LDL cholesterol:100 to 129mg/dL ● HDL cholesterol: >60mg/dL ● Total Cholesterol: <200mg/dL ● Triglycerides: <150mg/dL ● Total cholesterol ≥ 200 mg/dL ● LDL cholesterol ≥130 mg/dL ● HDL Cholesterol <40 mg/dL in men or <50 mg/dL in women ● Triglycerides ≥150 mg/dL Adults at risk for gastric cancer (e.g. age >40y/o, FHx of Gastric Ca, precancerous lesion, Hx of H. pylori infection, Obesity, Hx of smoking, Hx of high consumption of salted food) Upper Endoscopy Weak (PHEX 2021)20 Upper Endoscopy: normal Upper Endoscopy: masses,ulcerations, precancerous growths, cancer All adults in highly endemic areas Rapid or laboratory based HBsAg OR Upper GI Series: normal Upper Gastrointestinal Series Anti-HBs (will also help determine who needs to get Hepatitis B vaccine boosters) Hepatitis C Adults high risk for Hepatitis C (e.g. people who use injection Back to Table of Contents Serum anti-HCV Upper GI Series: masses, tumors, tissue changes 2021 Clinical Practice Guidelines for the Management of Hepatitis B in the Philippines30 Rapid or laboratory based HBsAg: negative/non-reactive Rapid HBsAg: positive/reactive Strong (PHEX 2023)23 Serum anti-HCV: non-reactive Serum anti-HCV: reactive Omnibus Health Guidelines ver. 2023 | 59 Conditions being Screened Eligible Population Screening Test to be Offered at Primary Care Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings Patients at risk to develop HCC may include patients with chronic hepatitis B or C infection, heavy and prolonged alcohol consumption, cirrhosis, diabetes, non-alcoholic fatty liver disease, and inherited metabolic diseases Liver Ultrasound with alpha-fetoprotein test every 6 months Strong (PHEX 2021)20 Liver Ultrasound: normal Liver Ultrasound: enlargement, masses, fatty liver, cirrhosis Human Immunodeficiency Virus Adults high risk for HIV (e.g. key populations including adolescents, high-risk individuals who have not been tested recently, partners, infants and children of people living with HIV, patients showing signs and symptoms consistent with AIDS defining illness, patients with sexually transmitted infections, patients with Hepatitis B and C, patients with undernutrition not responsive to interventions, all confirmed tuberculosis patients, and all pregnant women regardless of risk; key population: MSM, people in prisons and other closed settings, people who inject drugs, sex workers, and transgender men and women) Rapid diagnostic test Hypertension All adults Office BP drugs or PWID) Hepatocellular Carcinoma Back to Table of Contents AFP: level between 10ng/mL to 20ng/mL AFP: elevated AFP Strong (PHEX 2023)23 RDT: non-reactive RDT: reactive Strong (for screening) Normal BP: BP: ⋝140/90mmHg 3,31 Omnibus Health Guidelines ver. 2023 | 60 Conditions being Screened Eligible Population Screening Test to be Offered at Primary Care Strength of Recommendation (if available) and Reference Guideline Normal Results measurements using standardized BP measurement protocol at every clinic visit (PHEX 1 2021)3 <120/80mmHg PSH 202031 Borderline BP: 120-139/80-89mmHg Abnormal Findings ISH 20207 Latent Tuberculosis Adults high risk for TB infection (e.g. close contacts) Tuberculin Skin Test (TST) or Interferon-gamma Release Assay (IGRA) Weak (PHEX 2023)23 TST or IGRA: negative TST or IGRA: positive Lung Cancer Adults high risk for lung cancer (e.g. age of more than 50 years old with history of smoking, family history of lung cancer) Annual low-dose CT scan Weak (PHEX 2021)20 Low-dose CT scan: negative Low dose CT: masses (suspicious spots or nodules) Nutritional Anemia Asymptomatic adults Hemoglobin (Hgb) and Red Blood Cell (RBC) parameters Strong (PHEX 3 2023)16 Hgb: >13.5 g/dl (men) >12.0 g/dl (women) Hgb: <13.5 g/dl (men) <12.0 g/dl (women) Hct: 42-52% (men) 37-47% (women) Hct: above/below normal MCV: 80-100fL MCH: 27-31 pg Syphilis Adults high risk for Syphilis (e.g. HIV-positive men, men having sex with men, unprotected sex, Back to Table of Contents Rapid Plasma Reagin (RPR) or Venereal Disease Research Strong (PHEX 2023)23 RPR: negative/non-reactive VDRL: negative MCV: above/below normal MCH: above/below normal RPR: positive/reactive VDRL: positive Omnibus Health Guidelines ver. 2023 | 61 Conditions being Screened Eligible Population Screening Test to be Offered at Primary Care persons living with HIV (PLHIV), sexual contact with known case of syphilis, commercial sex workers, sexual contact with persons from countries or communities with high prevalence of syphilis and syphilis-related morbidity, prior syphilis, born to a person diagnosed with syphilis in pregnancy, multiple sexual partners, and history of sex in conjunction with illicit drug use) Laboratory (VDRL) tests every 6 to 12 months Back to Table of Contents Strength of Recommendation (if available) and Reference Guideline Normal Results Abnormal Findings Omnibus Health Guidelines ver. 2023 | 62 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. World Health Organization. Screening programmes: a short-guide. Increase effectiveness, maximize benefits and minimize harm. Copenhagen: WHO Regional Office for Europe. Published 2020. Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/330829/9789289054782-eng.pdf World Health Organization. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). Published 2010. Accessed December 14, 2023. https://www.who.int/publications/i/item/978924159938-2 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX) Phase 1. Published 2021. Accessed December 14, 2023. https://drive.google.com/drive/folders/1UXFurxj0dLH1J-Ua1KmrYaTuky7pON8Z Spitzer R., MDMD CALC. GAD-7 (General Anxiety Disorder-7) Scale. N.d. 2001. Accessed December 14, 2023. https://www.mdcalc.com/calc/1727/gad7-general-anxiety-disorder7 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Mental Health and Addiction. Published 2021. Accessed December 14, 2023. https://drive.google.com/file/d/1Nq-QO0UYMh0MiLWeKmO8CSdcuZyFdlbg/view American College of Cardiology. ASCVD Risk Estimator Plus. n.d. Accessed December 14, 2023. https://tools.acc.org/ascvd-risk-estimator-plus/#!/calculate/estimate/ Unger et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension, 75(6), 1334-1357. PMID: 32370572. 10.1161/HYPERTENSIONAHA.120.15026. 2020. https://www.ahajournals.org/doi/epub/10.1161/HYPERTENSIONAHA.120.15026 World Health Organization. HEARTS Technical Package for Cardiovascular Disease Management in Primary Health Care: Risk-based CVD Management. Geneva: World Health Organization. Published 2020. Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/333221/9789240001367-eng.pdf?sequence=1 Lung Center of the Philippines & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guidelines for the Management of Chronic Obstructive Pulmonary Disease. Published 2023. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/1kAx4VZrlqH3AQkQ-E35TSQLg7Z6wQud1 U.K. Department of Health and Social Care. Delivering better oral health: an evidence-based toolkit for prevention. Chapter 4: Dental Caries. Updated November 09, 2021. Accessed December 14, 2023. https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention/chapter-4-d ental-caries U.S. National Institutes of Health. The Patient Health Questionnaire 9 - Overview. Published 2001. Accessed December 14, 2023. https://coepes.nih.gov/sites/default/files/2020-12/PHQ-9%20depression%20scale.pdf Agency for Healthcare Research and Quality.Geriatric Depression Scale (Short Form). N.d. Accessed December 14, 2023. https://integrationacademy.ahrq.gov/sites/default/files/2020-07/Update_Geriatric_Depression_Scale-15.pdf World Health Organization. mhGAP Intervention Guide Mental Health Gap Action Programme for mental, neurological and substance use disorders in non-specialized health settings Version 2.0. World Health Organization. Published 2016. Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/250239/9789241549790-eng.pdf?sequence=1 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Musculoskeletal Disorders. Published 2023. Accessed December 14, 2023. https://drive.google.com/file/d/1p557JgrPgx9O9tI2NnSK-ha19KoECra1/view Philippine College of Chest Physicians. Philippine Clinical Practice Guidelines: Diagnosis and Treatment of Tobacco Use and Dependence.Published 2014. Accessed December 14, 2023, https://www.apsresp.org/pdf/esap/esap-201408-lectures/cs-5-3.pdf University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination Phase (PHEX) Phase 3: Task Force on Renal, Metabolic, Nutrition, and Endocrine Disorders. Published Published 2023. Accessed December 14, 2023. https://drive.google.com/file/d/1jViG7Whi45tBVHADBKraV06mUnpKvnNS/view Philippine Psychiatric Association. Consensus Treatment Guidelines on Major Depressive Disorder in Adults. Published 2017. Accessed December 14, 2023. https://drive.google.com/drive/u/1/folders/1iykz29ZFbnkufon3eSCKndbQfTs1TCnw U.S. Preventive Services Task Force. Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions. Published 2021. Accessed December 14, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling -and-interventions Department of Health. Implementing Guidelines on the Institutionalization of Philippine Package of Essential NCD Interventions (PHIL PEN) on the Integrated Management of Hypertension and Diabetes for Primary Health Care Facilities. Published December 4, 2012. Accessed December 14, 2023. https://dmas.doh.gov.ph:8083/Rest/GetFile?id=336917 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Neoplastic Diseases. Published 2021. Accessed December 14, 2023. https://drive.google.com/file/d/1oMATzGvpulZZrarfVktgVJzNt_7eavH4/view American Academy of Ophthalmology. Cataract in the Adult Eye Preferred Practice Pattern. Published 2021. Accessed December 14, 2023. https://www.aaojournal.org/action/showPdf?pii=S0161-6420%2821%2900750-8 American Academy of Ophthalmology. Comprehensive Adult Medical Eye Evaluation Preferred Practice Pattern. Published 2020. Accessed December 14, 2023. https://www.aaojournal.org/action/showPdf?pii=S0161-6420%2820%2931026-5 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX) Phase 3: Screening for Infectious Diseases. Published 2023. https://drive.google.com/file/d/1up5YnRyy6S5YpTsGgRoZHo4XDCOSrjR7/view American Diabetes Association. Retinopathy, Neuropathy, and Foot Care: Standards of Medical Care in Diabetes. Published 2022. Accessed December 14, 2023. https://diabetesjournals.org/care/article/45/Supplement_1/S185/138917/12-Retinopathy-Neuropathy-and-Foot-Care-Standards?sea rchresult=1 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Cardiovascular Disease. Published 2021. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 63 26. 27. 28. 29. 30. 31. 32. https://drive.google.com/file/d/1LyjMZhD0hAh2DJI6ta-IUPEDZacI8yow/view Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021-3104. doi:https://doi.org/10.1093/eurheartj/ehy339 American Academy of Ophthalmology. Primary Open-Angle Glaucoma Suspect Preferred Practice Pattern. Published 2020. Accessed December 14, 2023. https://www.aaojournal.org/action/showPdf?pii=S0161-6420%2820%2931025-3 American Academy of Ophthalmology. Primary Open-Angle Glaucoma Preferred Practice Pattern. Published 2020. Accessed December 14, 2023 https://www.aaojournal.org/action/showPdf?pii=S0161-6420%2820%2931024-1 American Academy of Ophthalmology. Primary Angle Closure Preferred Practice Pattern. Published 2020. Accessed December 14, 2023 https://www.aaojournal.org/action/showPdf?pii=S0161-6420%2820%2931023-X Department of Health. Clinical Practice Guidelines for the Management of Hepatitis B in the Philippines.Published 2021. Accessed December 14, 2023. https://drive.google.com/drive/folders/16PonztbznskCZhLpf1ro58ECYihNFOxP Philippine Society of Hypertension & Philippine Heart Association. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 14, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view Bickley, L. S., Szilagyi, P. G., & Hoffman, R. M. Bates' guide to physical examination and history taking. 12th ed. Wolters Kluwer; 2017 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 64 The Immunization Services Section: aims to provide guidance to primary care providers on the appropriate immunization services for adults. Routine immunization services not only protect individuals but the population at large. Vaccines are central to the prevention of diseases of public health importance and age- and sex-appropriate vaccines should be offered to eligible adults at every opportunity. General Principles ● ● ● ● ● Observe patient-centered care, with respect for the patient’s autonomy and right to self-determination, privacy and confidentiality, and informed consent. Engage in a shared decision-making process when selecting the vaccines appropriate to the patient’s health profile and risks. Acknowledge the concerns of individuals about vaccination and immediately address misconceptions and vaccine hesitancy in a clear and respectful manner. Provide accurate information about the benefits and risks of each vaccine, including adverse events following immunization (AEFI) and clearly explain how the benefits outweigh the risks. Share accurate scientific information about vaccines from verified sources. Ensure that vaccine counseling and vaccination are part of regular clinical care and emphasize the importance of keeping vaccinations up to date. Vaccines for Adults ● ● Offer vaccination services to all eligible adults (Table 6). Encourage adults to maintain and safely keep updated immunization records. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 65 Table 6. Recommended Vaccines for Adults Eligible Population Vaccine Strength of Recommendation (if available) and Reference Guideline Apparently Healthy Adults All adults with complete primary series of tetanus Tetanus toxoid-containing vaccine Strong (PHEX, 2023)1 All adults with unknown tetanus vaccination status Primary series: Tdap followed by any tetanus toxoid-containing vaccine Weak (PHEX, 2021)2 18 to 26 - year old females Human papillomavirus vaccine Strong (PHEX, 2021)2 (every 10 years) (unvaccinated or incomplete primary series) 18 to 26 - year old males Weak (PHEX, 2021)2 (unvaccinated or incomplete primary series) 18 to 64 years old Hepatitis B vaccine Strong (DOH, 2021)3 (as catch-up for those with no serological evidence of immunity) COVID-19 Vaccine Strong (PSMID, 2023)4 Inactivated Influenza vaccine Weak (PHEX, 2021)2 Pneumococcal Conjugate Vaccine - 13 valent Weak (PHEX, 2021)2 Typhoid Vi polysaccharide intramuscular vaccine Weak (PHEX, 2021)2 Hepatitis A vaccination Weak (PHEX, 2023)1 (2-dose; 0,6 months) Japanese encephalitis virus vaccine Weak (PHEX, 2023; PSMID, 2018)1,5 Measles-containing vaccine Weak (PHEX, 2023)1 (for non-pregnant or unvaccinated) ≥ 50 years old, for prevention of herpes zoster infection Adjuvanted recombinant zoster virus vaccine Strong (PSMID, 2018)5 Adults with Medical/ Special Conditions or Special Circumstances Asplenia Haemophilus influenzae b vaccine (anatomical or functional) Bronchial asthma, COPD, and cardiovascular disease Weak (PHEX, 2023; PSMID, 2018)1,5 Influenza vaccine Strong (PSMID, 2018)5 Varicella vaccine Strong (PSMID, 2018)5 Weak (PSMID, 2018)5 Strong (PSMID, 2018)5 (for the prevention influenza-related respiratory infections and hospitalizations) Cancer End-stage renal disease Healthcare Workers (for those without a history of varicella infection) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 66 Eligible Population Vaccine Strength of Recommendation (if available) and Reference Guideline Hepatitis B vaccine Strong (PSMID, 2018)5 (including medical students) Other high risk population for Hepatitis B infection: A. Persons deprived of liberty (PDLs) B. Drug users C. Patients with chronic renal failure At risk for Meningococcal disease: A. Individuals living in close quarters/proximity B. Asplenic patients C. Microbiologists (increased exposure) Persons living with HIV Inactivated Influenza Vaccine Rabies vaccines: 1. Direct carers of rabies patients 2. HCWs involved in rabies control 3. Personnel in rabies diagnostic laboratories Hepatitis B vaccine Weak (PHEX, 2021)2 Weak (PHEX, 2023)1 Meningococcal MenACWY vaccine Weak (PHEX, 2023)1 *meningococcal MenB vaccine may be given to young adults in crowded dormitories Hepatitis B vaccine Influenza Vaccine (administer inactivated vaccines regardless of CD4 count) Pregnant women Strong (PSMID, 2018)5 Hepatitis B Strong (PSMID, 2018)5 Strong (PSMID, 2018)5 ;(US CDC, 2023)6 Strong (DOH, 2021)3 (for pregnant with no serological evidence of immunity) Traveler to a Cholera-endemic area With stable medical comorbidities and are at risk for severe infection With comorbidities or Back to Table of Contents COVID-19 Inactivated Influenza Vaccine If complete with primary series containing tetanus toxoid: Any tetanus toxoid-containing vaccines If with unknown status or incomplete primary series: adjuvanted tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) followed by any tetanus toxoid-containing vaccines If with high-risk exposure to cholera (e.g., outbreak or travel to an endemic area): Oral cholera vaccine If at risk for Hepatitis A during pregnancy, may offer Hepatitis A Oral cholera vaccine Weak, (PSMID, 2023)4 Weak (PHEX, 2023)1 Weak (PHEX, 2021)2 COVID-19 Strong, (PSMID, 2023)4 Pneumococcal vaccine (None, unknown vaccination Recommended (US CDC, Weak (PHEX, 2021)2 Weak (PSMID, 2018)5 Recommended (PSMID, 2018)5; (US CDC, 2020)7 Strong (PHEX, 2023)1 Omnibus Health Guidelines ver. 2023 | 67 Eligible Population Vaccine immunocompromising conditions: status, received PCV7 at any age): ● Chronic renal failure congenital or acquired asplenia ● Congenital or acquired immunodeficiency (including B-[humoral] or T-lymphocyte deficiency, complement deficiencies [particularly C1, C2, C3, and C4 deficiencies], and phagocytic disorders [excluding chronic granulomatous disease]) ● Generalized malignancy ● HIVinfection ● Hodgkin disease ● Iatrogenic immunosuppression (including disease requiring treatment with immunosuppressive drugs such as long-term systemic corticosteroids and radiation therapy) ● Leukemia ● Lymphoma ● Multiple myeloma ● Nephrotic syndrome ● Sickle cell disease and other hemoglobinopathies ● Solid organ transplant (excludes persons with a hematopoietic stem cell transplant) Option 1: Single-dose PCV20 Option 2: Single-dose PCV15 followed by a single-dose of PPSV23 after ≥8 weeks As pre-exposure prophylaxis for other at-risk adult population (PSMID, 2018)5: 1. Individuals directly involved in rabies control 2. Pet owners and household members 3. Animal handlers 4. Field workers such as dog vaccinators/catchers 5. Veterinarians and veterinary students 6. Spelunkers Rabies Vaccine Back to Table of Contents Strength of Recommendation (if available) and Reference Guideline 2023)8 Weak (PHEX, 2023)1 Omnibus Health Guidelines ver. 2023 | 68 Monitoring and Management of Adverse Effects Following Immunization (AEFI) Ensure systems are in place to monitor and address AEFI, such as the following: ● ● ● ● ● ● Observe all adult vaccine clients for 15 minutes post vaccination to prevent secondary injury associated with syncope.9 Inform clients for vaccination about the difference between a reaction related to the vaccine and an adverse event which can have other causes (DOH Administrative Order 2023-0007)10. Offer paracetamol to adults presenting with fever or headache after vaccination and/or localized reactions such as pain, soreness, redness, itching, swelling, or burning at the injection site for 1 - 2 days.11,12 Ensure integrated health service approach for AEFI response that covers the clinical management, navigation, referral, and communication, according to the updated AEFI management pathways12 and clinical guidelines. Report all adverse events following immunization (AEFI) of newly introduced vaccines regardless of severity, that are suspected to be associated with the vaccine using the appropriate reporting platform upon collection of the minimum required case details (DOH Administrative Order 2023-0007)10. Report AEFIs for vaccines under the NIP or those with established vaccine safety profiles using the appropriate reporting platform as long as no other clear cause has been identified and the causal link to vaccine has not been established. Immediately notifiable AEFIs are the following (DOH Administrative Order 2023-0007)10: ○ Acute flaccid paralysis (vaccine-associated paralytic poliomyelitis) ○ Anaphylactoid reaction (acute hypersensitivity reaction) ○ Anaphylaxis ○ Arthralgia ○ Brachial neuritis ○ Disseminated BCG infections ○ Encephalopathy ○ Hypotonic - hyporesponsive episode (HHE or shock-collapse) ○ Injection site abscess ○ Lymphadenitis (simple and/or suppurative) ○ Osteitis or osteomyelitis ○ Persistent inconsolable screaming ○ Seizures ○ Sepsis ○ Severe local reaction ○ Thrombocytopenia ○ Toxic shock syndrome (TSS) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 69 Monitoring and Management of Adverse Effects Following Immunization (AEFI) ● ● Refer all adults presenting with an anaphylactic reaction after receiving a vaccine dose to an allergy specialist for clearance to determine if the vaccine client shall proceed with their next scheduled vaccinations. Advise vaccine recipients to report to the National Adverse Events Following Immunization Committee in case of AEFI (Contact number: 8651-7800, local 2930). Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 70 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Adult Immunization. Published 2023. Accessed December 16, 2023. https://drive.google.com/file/d/1q5m5uxA-zY_MHgBO2S9EW_AoK3x3qr0L/view University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Immunization for Adults. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/15bZXoiltUJxGMlp5wgOMxI70tY6PTplE/view Department of Health. Clinical Practice Guidelines for the Management of Hepatitis B in the Philippines. Published 2021. Accessed December 16, 2023. https://drive.google.com/drive/folders/16PonztbznskCZhLpf1ro58ECYihNFOxP Philippine Society for Microbiology and Infectious Diseases. Philippine COVID-19 Living Recommendations. Published 2023. Accessed December 14, 2023. https://www.psmid.org/philippine-covid-19-living-recommendations-3/ Philippine Society for Microbiology and Infectious Diseases. Philippine Clinical Practice Guidelines for Adult Immunization. Makati: Zurbano Publishing and Printing Corp. Published 2018. Accessed December 14, 2023. https://drive.google.com/file/d/1pdl986x5sLNzSCBwRGC9HNBAvgGHl06N/view U.S. Centers for Disease Control and Prevention. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2023–24 Influenza Season. Published 2023. Accessed December 14, 2023. https://www.cdc.gov/mmwr/volumes/72/rr/rr7202a1.htm U.S. Centers for Disease Control and Prevention. Prevention of Hepatitis A Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices.Published 2020. Accessed December 14, 2023. https://www.cdc.gov/mmwr/volumes/69/rr/rr6905a1.htm U.S. Centers for Disease Control and Prevention. Pneumococcal Vaccine for Adults Aged ≥19 Years: Recommendations of the Advisory Committee on Immunization Practices, United States. Published 2023. Accessed December 14, 2023. https://www.cdc.gov/mmwr/volumes/72/rr/pdfs/rr7203a1-H.pdf U.S. Centers for Disease Control and Prevention. Vaccine Recommendations and Guidelines of the ACIP. Published 2022. Accessed December 14, 2023. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/adverse-reactions.html Australian Government Department of Health and Aged Care. Common side effects following immunisation for vaccines used in the National Immunisation Program schedule. Australian Immunisation Handbook. Published 2023. Accessed December 14, 2023. https://immunisationhandbook.health.gov.au/resources/tables/table-common-side-effects-following-immunisation-for-vaccines-u sed-in-the-national-immunisation-program-schedule Department of Health. Adverse Events Following Immunization (AEFI): A Manual of Procedure for Surveillance and Response to AEFI. National Epidemiology Center. Published 2014. Accessed December 14, 2023. https://drive.google.com/file/d/1aV_prtVB1xyuC8HwfY-EIdrOri9nfUQc/view Department of Health. Interim AEFI Management Pathways for Healthcare Providers, Version 4. Published 2021. Accessed DEcember 14, 2023. https://drive.google.com/file/d/1xqsv-vP4zz2zsg-6y5NjuESzBlF7fhez/view Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 71 The Sexual and Reproductive Health Section: aims to provide guidance on the services that should be offered at the primary care level in order to uphold the right of individuals to sexual and reproductive health to achieve a state of complete physical, mental and social well-being. This section encompasses standards of care in sexual and reproductive health, including family planning and maternal health. General Principles ● ● ● Respect the right to autonomy and self-determination of all individuals. Offer family planning to all eligible couples and individuals. ○ Family planning refers to a program which enables couples and individuals to decide freely and responsibly the number and spacing of their children and to have the information and means to do so, and to have access to a full range of safe, affordable, effective, non-abortifacient modern natural and artificial methods of planning pregnancy1. ■ The State shall promote and provide information and access, without bias, to all methods of family planning, including effective natural and modern methods which have been proven medically safe, legal, non-abortifacient, and effective in accordance with scientific and evidence-based medical research standards1 . ■ Discuss the benefits and harms of different FP methods and select the best method through participatory decision-making. Offer maternal health services, including antenatal care, intrapartum care, and post-natal care to all pregnant women and girls. ○ Antenatal care (ANC) is the care provided by skilled health-care professionals to pregnant women and adolescent girls in order to ensure the best health conditions for both mother and baby during pregnancy. The components of ANC include: risk identification, prevention and management of pregnancy-related or concurrent diseases, and health education and health promotion. ■ ANC reduces maternal and perinatal morbidity and mortality both directly, through detection and treatment of pregnancy-related complications, and indirectly, through the identification of women and girls at increased risk of developing complications during labor and delivery, thus ensuring referral to an appropriate level of care.2 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 72 Family Planning ● ● ● Offer contraception to women until they reach menopause.3 Determine the appropriate family planning methods through taking the family, menstrual, contraceptive and sexual history. (Strong recommendation, UK-NICE)4 ○ Women who meet the following criteria after a thorough menstrual and sexual history and assessment of pregnancy risk can be reasonably excluded from a consideration of pregnancy 5: ■ is ≤7 days after the start of normal menses ■ has not had sexual intercourse since the start of last normal menses. ■ has been correctly and consistently using a reliable method of contraception ■ is ≤7 days after spontaneous or induced abortion ■ is within 4 weeks postpartum ■ is fully or nearly fully breastfeeding of no interval of more than 4-6 hours between breastfeeds (exclusively breastfeeding or the vast majority [≥85%] of feeds are breastfeeds), amenorrheic, and <6 months postpartum ○ Offer a urine pregnancy testing to confirm pregnancy among women who do not fulfill these criteria prior to initiating any form of contraception. Select the appropriate family planning method after shared decision making between the patient or the couple, and the primary care provider1,6. The different family planning methods include the following6. The WHO Contraception Tool7 may be used a reference and teaching material for recommending safe, and effective methods: ○ Medical Eligibility Criteria (MEC) refers to the medical conditions or characteristics related to the safety and efficacy of the contraceptive. Categories range from 1 to 4, weighing benefits and risks in using the contraceptive6. ○ Combined hormonal contraceptives6 (CHC) (e.g. combined oral contraceptive pills, combined injectable contraceptive, combined contraceptive patches and rings) ■ Provide to women (Medical Eligibility Criteria Category 1): ● from age of menarche through 40 years of age ● > 42 days postpartum ● with varicose veins ● Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) ● Women living with HIV taking any nucleoside reverse transcriptase inhibitor (NRTI), newer non nucleoside reverse transcriptase inhibitors (NNRTI) containing etravirine and rilpivirine, or raltegravir ■ Consider for (MEC Category 2): ● Breastfeeding women ≥ 6 months postpartum ● ≥ 21 days to 42 days postpartum without other risk factors for venous thromboembolism ● with superficial venous thrombosis ● with known dyslipidemias without other known cardiovascular risk factors Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 73 Family Planning Women with HIV using NNRTIs containing efavirenz Women using protease inhibitors (e.g. ritonavir and antiretrovirals boosted with ritonavir) Progestogen-only containing contraceptives (POC)6 [e.g. progestogen-only pills, implants [e.g levonorgestrel (LNG) (e.g. Sino-Implant (II) or etonogestrel (ETG)], and injectables ■ Provide to breastfeeding women who are (MEC Category 1): ● ≥ 6 weeks to < 6 months months postpartum ● ≥ 6 months postpartum ● Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) ● Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) ● Women living with HIV taking any nucleoside reverse transcriptase inhibitors ● Women living with HIV newer NNRTIs containing etravirine and rilpivirine ● Women living with HIV taking raltegravir ■ Consider for (MEC Category 2): ● breastfeeding women who are < 6 weeks postpartum ● Women living with HIV using NNRTIs containing efavirenz ● Women using protease inhibitors (e.g. ritonavir and ARVs boosted with ritonavir) Depot medroxyprogesterone acetate6 (intramuscular or subcutaneous). Provide for (MEC Category 1): ● Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) ● Women taking any nucleoside reverse transcriptase inhibitor ● Women living with HIV using protease inhibitors (e.g. ritonavir and ARVs boosted with ritonavir) ● Women living with HIV using NNRTIs containing efavirenz or newer NNRTIs containing etravirine and rilpivirine ● Women living with HIV taking raltegravir Intrauterine device (IUD)6 ■ Levonorgestrel-releasing intrauterine device (LNG-IUD): ● Provide to (MEC Category 1): ○ breastfeeding women who are ≥ 4 weeks postpartum ○ Women living with HIV taking newer NNRTIs containing etravirine and rilpivirine ○ Women living with HIV taking raltegravir ● Consider for (MEC Category 2): ● ● ○ ○ ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 74 Family Planning breastfeeding women who are < 48 hours postpartum Women at increased risk of STIs Women living with asymptomatic or mild HIV clinical disease (WHO stage 1 or 2) ○ Women living with HIV taking the following antiretrovirals, provided their HIV clinical disease is asymptomatic or mild (WHO Stage 1 or 2) ■ protease inhibitors ■ NRTI ■ NNRTIs containing either efavirenz ■ Raltegravir ■ Copper-bearing IUD (Cu-IUD) ● Consider for women at increased risk of STIs (MEC Category 2)6 ● Consider use until menopause when inserted at age 40 or over3 Progesterone-releasing vaginal ring6 ■ Provide to (MEC Category 1): ● actively breastfeeding women and are ≥ 4 weeks postpartum ● women living with HIV taking newer NNRTIs containing etravirine and rilpivirine ● women living with HIV taking raltegravir Barrier method and other pericoital contraceptives 8 ■ Offer condoms to all male and female adults, provided that they have no severe allergic reaction to latex rubber. ■ Offer spermicides to all women, provided that they are not at high risk for HIV infection or have HIV infection ■ Offer diaphragms to all women six weeks after giving birth or undergoing second-trimester spontaneous abortion, not at high risk for HIV infection, or have no allergic reaction to latex rubber ■ Offer cervical caps for women who are not undergoing treatment for cervical precancer or cancer. Sterilization methods ■ Offer counseling on the permanency of sterilization and the availability of highly effective, long-acting, reversible methods of contraception. for adults considering permanent sterilization methods (e.g. vasectomy, tubal ligation)5 Natural family planning methods for eligible women.8 ■ Fertility awareness-based methods ● Consider the following methods among adults who are 1) able to comply with FAB method requirements, and 2) abstain from sexual intercourse or use barrier methods on fertile days9 : ○ Calendar-based method (e.g. Standards Days Method) ○ ○ ○ ○ ○ ○ ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 75 Family Planning Symptoms-based methods (e.g Cervical mucus or ovulation method, basal body temperature, Two-Day Method, and symptothermal method) ■ Consider lactational amenorrhea method among postpartum women who meet all of the following criteria: ● menstruation has not returned. ● the baby is fully or nearly fully breastfed and is fed often, day and night, and ● the baby is less than 6 months old. Monitoring for adverse effects. ○ Obtain blood pressure measurements taken before initiation of contraceptives (strong recommendation)6 ○ Offer the following examinations and tests prior to the initiation of hormonal contraceptives, as appropriate: ■ BMI, Clinical breast examination, bimanual examination and cervical inspection ■ Hemoglobin, glucose, lipids, liver enzymes ■ Thrombogenic mutations ■ Cervical cancer screening ■ HIV screening Referral for management of adverse effects ○ Refer women with current venous thromboembolism who are in need of hormonal contraception while being treated to a specialist (Strong recommendation)4 ○ Recognize signs and symptoms of venous thromboembolism (e.g., deep venous thrombosis, pulmonary embolism) and refer to higher level of care. ○ ● ● Assessment of Pregnancy ● ● Signs and symptoms of possible pregnancy. Suspect pregnancy in a women of reproductive age presenting with signs and symptoms of possible pregnancy such as the following10: ○ Late, missed, or absent menstrual period; ○ Breast tenderness ○ Nausea or vomiting ○ Sudden or excessive weight change ○ Fatigue ○ Mood changes ○ Changes in eating habits ○ Frequent urination History Taking. Perform comprehensive history taking, including the history of present illness, past medical history, family history, personal, social and occupational history, in order to identify Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 76 Assessment of Pregnancy ● ● ● risk factors such as the following: risk factors from personal, social, and occupational history, ovulatory and menstrual irregularity, dysmenorrhea, gestational diabetes, hypertension in pregnancy, preeclampsia, and other obstetric and/or gynecologic conditions. Advise women who are sexually active and experiencing signs and symptoms of early pregnancy to perform pregnancy testing using FDA approved urine home pregnancy kits and encourage them to consult a healthcare professional for confirmation and appropriate medical advice. Gold Standard for confirmation of pregnancy. Request for an early pregnancy ultrasound before 24 weeks of gestation to ensure an intrauterine pregnancy, and to establish gestational age with certainty. ○ One ultrasound scan before 24 weeks of gestation (early ultrasound) is recommended for pregnant women to estimate gestational age, improve detection of fetal anomalies and multiple pregnancies, reduce induction of labor for post-term pregnancy, and improve a woman’s pregnancy experience. (Recommended)10 Advise pregnant women on birth preparedness and complication readiness interventions (e.g. schedule of appointments, what happens at different appointments, stages of pregnancy).11 (Strong recommendation)10 Maternal Health Services ● Antenatal Care. Perform the following for each antenatal check-up: ○ Ensure quality antenatal care including the minimum of eight antenatal contacts (i.e. active connection between a pregnant woman and a health-care provider) according to the following schedule, and/or referral to a hospital for specialist care, if necessary (Recommended)10: ■ First contact at 12 weeks; ■ Second and third contact at 20 and 26 weeks age of gestation (AOG), respectively; ■ Subsequent third trimester contacts at 30, 34, 36, 38, and 40 weeks AOG; and ■ Return for delivery if still have not given birth at 41 weeks AOG; ○ Complete general and obstetrical examination, including 10,11,: ■ vital signs ■ weight gain based on pre-pregnant weight ■ oral health check-up and prophylaxis ■ screening for cigarette smoking, alcohol use, substance abuse, psychosocial risk factors, depression and exposure to violence, HIV and syphilis ■ assessment of significant signs and symptoms ○ Classify women according to low-risk pregnancy and high-risk pregnancy11 ○ Assist in developing a written Birth Plan and modify as necessary12 ○ Provide information and instructions on the signs of labor12 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 77 ○ ○ ○ ○ ○ ○ Provide information on how to modify or have a healthy lifestyle (diet, exercise).11,12 Teach pregnant women about proper diet and nutrition during pregnancy using Pinggang Pinoy. Manage according to identified risks and health concerns11 Discuss and give information on how to contact the health system for non-urgent advice and/or urgent concerns, such as pain and bleeding11,10. Give information on what screening programmes to do (such as blood tests, ultrasound) and explain the importance of such screening tests.10,11, Give advice regarding use of nutritional supplements such as: ■ Daily oral iron and folic acid supplementation with 30 mg to 60 mg of elemental iron and 400 mcg (0.4 mg) of folic acid (Recommended).13 ■ Offer calcium supplementation (1.5–2.0 g oral elemental calcium) for pregnant women to reduce the risk of pre- eclampsia. (Context-specific recommendation).2 ■ Consider giving high dose of iron supplements to mothers in populations where anemia is a public health concern to prevent maternal anemia (Recommended)13 ■ Consider giving Multiple Micronutrient Supplementation (MMS) over Iron-Folic Acid (IFA) supplements to mothers depending on the assessment and advice of the physician (Context-specific recommendation). 13 Provide the following nutritional services for each antenatal checkup ■ Counseling on healthy eating and physical activity during pregnancy. (Recommended).2 ■ Women will be more likely to achieve and maintain a healthy weight before, during and after pregnancy if they could14: ➢ eat fiber-rich foods such as oats, beans, peas, lentils, grains, seeds, fruit and vegetables, as well as whole grain bread and brown rice and pasta ➢ eat at least five portions of a variety of fruit and vegetables each day, in place of foods higher in fat and calories ➢ eat a low-fat diet and avoid increasing their fat and/or calorie intake ➢ eat as little as possible of fried food; drinks and confectionery high in added sugars (such as cakes, pastries and fizzy drinks); and other food high in fat and sugar (such as some take-away and fast foods) ➢ eat breakfast ➢ watch the portion size of meals and snacks, and how often they are eating ➢ balanced, healthy diet Provide advice on the following maternal exercises for each antenatal check up: ■ Aerobic physical activity and strength-conditioning exercise aimed at maintaining a good level of fitness throughout pregnancy, without trying to reach peak fitness level or train for athletic competition.10 ■ Choose activities with minimal risk of loss of balance and fetal trauma such as10: ➢ Walking ➢ Cycling ➢ Swimming Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 78 ● ● ● ● ● ➢ Aerobics ➢ Others: take the stairs instead of the lift or taking a walk at lunchtime, minimize sedentary activities ○ Offer additional testing and services appropriate to the trimester of pregnancy (Table 7). Intrapartum care. Deliver the appropriate intrapartum and neonatal care during labor and delivery (Table 8). Postpartum care. Deliver postpartum care as follows (Table 9): ○ Advise all postpartum women to consult the nearest health center and seek postnatal and newborn care of at least four postnatal visits scheduled as follows15: ○ Within 24 hours of birth or before discharge (weak recommendation)15; ○ On postpartum day 3 (strong recommendation)15; ○ Between postpartum days 7-14 (strong recommendation)15; and ○ Six weeks after birth (strong recommendation, WHO 2013)15. ● Provide the following services during postpartum visits15: ■ Counseling and support for exclusive breastfeeding at each postnatal contact (Strong recommendation)15 ■ Offer basic mental health and psychosocial support from a primary care provider and obtain a referral for evaluation and management by mental health professionals if experiencing symptoms of postpartum depression (Weak recommendation)15. ■ Offer advise on (Consensus statement)15: ➢ proper hygiene including perineal, hand and oral hygiene ➢ birth spacing and family planning including postpartum contraception, safer sex including use of condoms. ➢ nutrition Provide counseling regarding the benefits of birth spacing for the mother’s and the baby’s health. It is recommended to wait until the youngest child is at least 2 years old before trying to become pregnant again. Educate the postpartum mother about the following: ○ If not fully or nearly fully breastfeeding, mothers may become pregnant as soon as 4 to 6 weeks after childbirth ○ If fully or nearly fully breastfeeding, mothers may become pregnant as soon as 6 months postpartum. ○ For maximum protection, a woman should not wait until the return of monthly bleeding to start a contraceptive method.8 Provide information regarding family planning after delivery.8 ○ Reproductive goals (desire and timing) ○ Contraceptives ○ Medical issues or comorbidities Provide the following nutritional services and physical activity after delivery.15 ○ In the settings where gestational anemia is of public health concern, consider giving oral iron supplementation, either alone or in combination with folic acid supplementation, to postpartum women for 6–12 weeks following childbirth to reduce the risk of anemia. ○ Offer regular physical activity throughout the postpartum period by doing at least 150 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 79 ○ minutes of physical activity throughout the week. Replace sedentary time with physical activity of any intensity (including light intensity) to provide health benefits. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 80 Table 7. Summary of Antenatal Services in Primary Care First Trimester Provide Mother and Child Book and health information 10,11 Assess for the following: ● ● ● ● ● ● Nutritional assessment (Recommended11) Syndromic assessment for HIV and syphilis (Recommended)10 Diabetes mellitus risk factor evaluation (Recommended)10 Tobacco and substance use (Recommended)10 Intimate partner violence (Recommended)10 Compute for BMI11 Request the following tests: ● Blood typing11 ● Ultrasound at 12 weeks AOG to determine gestational age, detect multiple pregnancy (Recommended)11 Consider requesting for the following tests as appropriate: ● Complete blood count/Hgb count (Context-specific recommendation)10 screening ● Tuberculosis (Context-specific recommendation)10 ● Test for hepatitis B10,11 ● Midstream urine culture (gold standard) or midstream urine Gram staining (if culture is not available) for asymptomatic bacteriuria at 12 weeks AOG (Context-specific recommendation)10 Second Trimester Request and/or refer to an appropriate health facility to undergo the following tests, as necessary: ● ● ● ● ● ● Screen for gestational hypertension as early as the 20th week AOG11 HIV screening (if the status is still unknown) 16 Urinalysis (Recommended)10 Ultrasound before 24 weeks AOG to confirm normal anatomy, fetal growth and presentation and sex of the baby10 75g-OGTT for gestational diabetes at 24-28 weeks AOG10 Routine retinal assessment for those with pre-existing diabetes mellitus17 Third Trimester Request HIV screening (for those with negative initial HIV tests who are at increased risk of acquiring HIV) (Evidence A)18 Consider requesting for the following tests as appropriate (Context-specific recommendation)10: ● ● ● Midstream urine culture or midstream urine Gram staining for asymptomatic bacteriuria at 34 weeks AOG Complete blood count/Hgb count and/or Blood/RH group at 36 weeks Viral load testing for pregnant women with HIV on ART Consider requesting for the following tests as appropriate: (Context-specific recommendation)10 ● Complete blood count/Hgb count at 26 weeks ● Midstream urine culture or midstream urine Gram staining for asymptomatic bacteriuria at 26 weeks AOG Provide information on benefits of birth spacing, contraceptive options and initiation in the postpartum period.8 Offer the following preventive measures (Context-specific recommendation)10: ● Preventive antihelminthic treatment at 20 weeks AOG for women living in endemic areas** **Areas with greater than 20% prevalence of infection with any soil-transmitted helminths Refer to a CEmONC (comprehensive emergency obstetric and newborn care) provider hospital as necessary. ● Offer IPTp from 36 weeks AOG in malaria-endemic areas* IPTp from 20 - 30 weeks AOG in malaria-endemic areas* Provide information on benefits of birth spacing, contraceptive options and initiation in the postpartum period.8 Offer the following preventive measures (Context- Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 81 specific recommendation)10 Pre-exposure prophylaxis for HIV prevention at 12 weeks AOG ● Intermittent preventive treatment in pregnancy (IPTp) starting at 13 weeks AOG* *Administer in areas with moderate to high transmission of malaria ● Provide information on benefits of birth spacing, contraceptive options and initiation in the postpartum period.8 Provide counseling on infant feeding options if HIV infection is present. Table 8. Summary of Intrapartum Services in Primary Care Essential Newborn Care Intrapartum Care General ● ● Provide effective communication (Recommended)19 ○ use simple and culturally acceptable methods Provide respectful maternal care (Recommended)19 ○ organize and provide maternal care to all women in a manner that maintains their Back to Table of Contents Active phase of the first stage of labor ● Provide information regarding the duration of the first stage of labor (latent and active)19 ○ active first stage (from 5 cm until full cervical dilatation) usually does not extend beyond 12 hours in first labors, and usually does not extend beyond 10 hours in Second stage of labor ● ● Encourage to do proper method of pushing (Recommended)19 ○ support to follow their own urge to push. Inform regarding techniques for preventing perineal trauma to reduce perineal trauma and facilitate spontaneous birth (based on women’s preference and available Third stage of labor ● Give Prophylactic uterotonics (Recommended)19 ○ The use of uterotonics for the prevention of postpartum hemorrhage (PPH) during the third stage of labor is recommended for all births. ○ Oxytocin (10 IU, IM/IV) is the recommended uterotonic drug for the prevention of PPH)-. Step by Step Intervention Step 1. Immediate drying additional stimulation20 and For newly born babies who do not breathe spontaneously after thorough drying should be stimulated by rubbing the back 2–3 times before clamping the cord and initiating positive pressure ventilation. (Weak recommendation). Step 2. Skin-to-skin contact in the first hour of life (Strong recommendation)20 Omnibus Health Guidelines ver. 2023 | 82 ● dignity, privacy and confidentiality, ensures freedom from harm and mistreatment, and enables informed choice and continuous support during labor and childbirth Allow companion during labor and childbirth (Recommended)19 ● ● ● Back to Table of Contents subsequent labors (Recommended) Assess fetal well-being on labor admission19 ○ Auscultate using a Doppler ultrasound device or Pinard fetal stethoscope (Recommended) Do digital vaginal examination (Recommended)19 ○ Digital vaginal examination at intervals of four hours is recommended for routine assessment of active first stage of labor in low-risk women. Provide relaxation techniques, including progressive muscle relaxation, breathing, music, mindfulness and other techniques, are recommended for healthy pregnant women requesting pain relief during labor, depending on a woman’s preferences. (WHO, 201819) ● technique) (Recommended)19 ○ perineal massage ○ warm compresses ○ “hands on” guarding of the perineum For women with or without epidural analgesia, encourage the adoption of a birth position of the individual woman’s choice, including upright positions (Recommended)19 If oxytocin is unavailable, the use of other injectable uterotonics (if appropriate, ergometrine/ methylergometrine, or the fixed drug combination of oxytocin and ergometrine) or oral misoprostol (600 μg) is recommended. May do controlled cord traction (CCT) , if the care provider and the parturient woman regard a small reduction in blood loss and a small reduction in the duration of the third stage of labor (Recommended)19 ○ ● Newborns without complications should be kept in skin-to-skin contact with their mothers during the first hour after birth to prevent hypothermia and promote breastfeeding. Step 3. Delayed Cord clamping (Strong recommendation)20 Late cord clamping (performed after 1 to 3 minutes after birth) is recommended for all births while initiating simultaneous essential newborn care. Step 4. Non Separation from the mother and initiation of breastfeeding (Strong recommendation)20 All newborns, including low-birth-weight babies who are able to breastfeed, should be put to the breast as soon as possible after birth when they are clinically stable, and the mother and baby are ready. Give Vitamin K prophylaxis (Strong recommendation)20 All newborns should be given 1 mg of vitamin K intramuscularly (IM) after birth Omnibus Health Guidelines ver. 2023 | 83 Postnatal Care Table 9. Summary of Postnatal Services in Primary Care Immediate Postpartum Care (after 24 hours)15 ● ● ● ● ● ● Regular assessment for vaginal bleeding, uterine tone, fundal height and vital signs: blood pressure, heart rate, body temperature, respiratory rate (Consensus statement): ○ Every 15 minutes for the first 2 hours ○ Every hour for the next 2 hours ○ Every 6 hours thereafter until discharge. Nutrition Counseling (Consensus statement) Lactation management services to support breastfeeding initiation and exclusive breastfeeding (Strong recommendation) Recognition of danger signs among newborns (Strong recommendation): ○ Stopped feeding well ○ History of convulsions ○ Fast breathing (breathing rate >60 per minute) ○ Severe chest in-drawing ○ No spontaneous movement ○ Fever (temperature >37.5 °C) ○ Low body temperature (temperature <35.5 °C) ○ Any jaundice in the first 24 hours of life, or yellow palms and soles at any age. ART and cotrimoxazole prophylaxis for HIV-exposed infants early infant diagnosis for HIV-exposed infants Back to Table of Contents Day 3 and each subsequent check-ups between day 7 and 14, 6 weeks after birth15 ● ● ● ● ● Assess general well-being (Consensus statement): ○ Micturition and urinary incontinence, bowel function, healing of any perineal wound, headache, fatigue, back pain, perineal pain, breast pain, uterine tenderness, and lochia. Assess breastfeeding progress and maternal nutrition (Consensus statement) Check emotional well-being and resolution of postpartum depression at 10 - 14 days after birth (Consensus statement) Observe risks, sign and symptoms of domestic abuse (Consensus statement) Offer iron and folic acid supplementation for at least three months (Weak recommendation) Omnibus Health Guidelines ver. 2023 | 84 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Republic Act No. 10354 “The Responsible Parenthood and Reproductive Health Act of 2012″ World Health Organization. WHO Recommendations on Maternal Health. Geneva: WHO. Published 2017. Accessed November 2023. https://iris.who.int/bitstream/handle/10665/259268/WHO-MCA-17.10-eng.pdf?sequence=1 Faculty of Sexual and Reproductive Healthcare. FSRH Clinical Guideline: Contraception for Women Aged over 40 Years. Published 2023. Accessed December 14, 2023. https://www.fsrh.org/documents/fsrh-guidance-contraception-for-women-aged-over-40-years-2017/ U.K. National Institute for Health and Care Excellence. Long-acting reversible contraception. Published 2019. Accessed December 14, 2023. https://www.nice.org.uk/guidance/cg30/chapter/Recommendations U.S. Centers for Disease Control and Prevention. U.S. Selected Practice Recommendations for Contraceptive Use. Morbidity and Mortality Weekly Report. Published 2016. Accessed December 14, 2023. https://www.cdc.gov/mmwr/volumes/65/rr/pdfs/rr6504.pdf World Health Organization. Medical eligibility criteria for contraceptive use, 5th Edition. Published 2015. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789241549158 World Health Organization. New App for WHO’s Medical eligibility criteria for contraceptive use. Published 2019. Accessed December 14, 2023. https://www.who.int/news/item/29-08-2019-new-app-for-who-s-medical-eligibility-criteria-for-contraceptive-use World Health Organization. Family Planning: A Global Handbook for Providers. Published 2022. Accessed December 14, 2023. https://fphandbook.org/sites/default/files/WHO-JHU-FPHandbook-2022Ed-v221115a.pdf UpToDate. Fertility awareness-based methods of pregnancy prevention. Published 2023. Accessed December 14, 2023. https://www.uptodate.com/contents/fertility-awareness-based-methods-of-pregnancy-prevention?search=family%20planning%20 barrier%20method&source=search_result&selectedTitle=7~150&usage_type=default&display_rank=7# World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Published 2016. Accessed November 2023. https://iris.who.int/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1 U. K. National Institute for Health and Care Excellence. Antenatal Care. Published 2021. Accessed November 2023. https://www.nice.org.uk/guidance/ng201/resources/antenatal-care-pdf-66143709695941 U. K. National Institute for Health and Care Excellence. Intrapartum Care. Published 2023. Accessed December 14, 2023. https://www.nice.org.uk/guidance/ng235/chapter/Recommendations#antenatal-education-about-labour World Health Organization. WHO antenatal care recommendations for a positive pregnancy experience - Nutritional interventions update: Multiple micronutrient supplements during pregnancy. Published 2020 Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/333561/9789240007789-eng.pdf?sequence=1 U. K. National Institute for Health and Care Excellence. Weight management before, during and after pregnancy. Published 2010. Accessed December 14, 2023. https://www.nice.org.uk/guidance/ph27/resources/weight-management-before-during-and-after-pregnancy-pdf-1996242046405 World Health Organization. WHO recommendations on Postnatal care of the mother and newborn. Published 2013. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789241506649 World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. www.who.int. Published July 16, 2021. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789240031593 U.K. National Institute for Health and Care Excellence. Diabetes in pregnancy: management from preconception to the postnatal period. Published 2020. Accessed December 14, 2023. https://www.nice.org.uk/guidance/ng3/chapter/Recommendations#gestational-diabetes Panel on Treatment of HIV During Pregnancy and Prevention of Perinatal Transmission. Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States. Department of Health and Human Services. Published 2023. Accessed December 16, 2023. https://clinicalinfo.hiv.gov/en/guidelines/perinatal/maternal-hiv-testing-identification-exposure World Health Organization. WHO recommendations: Intrapartum care for a positive childbirth experience. Published 2018. Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/260178/9789241550215-eng.pdf?sequence=1 World Health Organization. WHO Recommendations on Newborn Health. Published 2018. Accessed December 14, 2023. https://iris.who.int/bitstream/handle/10665/259269/WHO-MCA-17.07-eng.pdf?sequence=1 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 85 The Diagnosis of Common Conditions in Primary Care Summary Section: aims to summarize the minimum diagnostic tests for various diseases that are commonly encountered in primary care. The availability of these diagnostic tests in primary care facilities or within the HCPN is critical in achieving UHC. Primary care managers and clinicians should aim to make these tests available and accessible to their clients, through the use of various financing and contracting mechanisms, in line with the UHC Act (e.g., Philhealth financing, LGU procurement, Special Health Fund, etc.) General Principles of Diagnosis ● ● ● ● ● Timely and accurate diagnosis facilitates the administration of early and appropriate management of illnesses and leads to better health outcomes. Always seek to obtain a good history and physical examination since they are central in developing a working diagnosis and differentials and guiding the selection of appropriate diagnostic tests. In the selection of diagnostic tests, always consider the evidence on the diagnostic accuracy (e.g., sensitivity, specificity, yield, discriminatory ability) of the test, together with factors such as patient values and preferences, and the access to and availability of the tests within the system (e.g., within the HCPN). Exercise due diligence when requesting for diagnostic tests and seek to avoid overtesting and overdiagnosis, including the performance of tests with unnecessary benefits or tests that lead to diagnoses which do not otherwise cause problems or symptoms and do not need intervention. Interpret diagnostic data in the context of the patient’s signs and symptoms and communicate the results of tests clearly to the patient. Diagnostic Tests in Primary Care ● ● ● Table 10 is a consolidation of the various tests for conditions commonly encountered in primary care. The list of conditions is arranged alphabetically for ease of navigation. The minimum tests that should be performed or requested for a given condition at the primary care level, to be done within a primary care facility or within the primary care provider network (PCPN) ,are itemized. Additional tests which can only be done at higher levels of care are identified to guide referrals. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 86 Table 10. Diagnostic Tests for Conditions Encountered in Primary Care Condition Minimum Tests at Primary Care Acute Chest Pain (Suspected Acute Coronary Syndrome) Basic Emergency Assessment (ABCDE) Acute Neurologic Symptoms (Suspected Stroke) Basic Emergency Assessment (Airway, Breathing, Circulation, Disability, Exposure [ABCDE]) (WHO-ICRC, 2018)3 12 L- ECG within 10 minutes of presentation if available, provided it does not delay transfer to the nearest ED (UK-NICE, 2016)1 Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Invasive coronary angiography Not Applicable Cardiac biomarkers; Invasive coronary angiography; non-invasive cardiac imaging; functional cardiac testing; tests for suspected or known comorbidities (UK-NICE, 2016)1 (AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR 2021) 2 Computed Tomography (CT) of the brain Not Applicable (N/A) (Immediately transfer to the nearest hospital) At the Emergency Department (ED)/referral hospital: CT of the brain, Complete blood count (CBC), prothrombin time (PT), partial thromboplastin time (PTT), glucose, HbA1c, Creatinine, Lipid profile, and other tests as necessary (AHA/ASA 2021)5 Bacterial culture followed by confirmatory tests–including phage and penicillin sensitivity, and PCR to detect N/A Gram stain and culture of blood, pleural fluid, cerebrospinal fluid (CSF), discharge from skin lesions; tissue biopsy specimens; and Reverse TranscriptasePolymerase Chain Reaction (RT-PCR) testing (if available) FAST (Face Arm Speech Test) for rapid assessment Capillary blood glucose to check for hypoglycemia (UK-NICE, 2022)4 Anthrax Back to Table of Contents Clinical diagnosis, Chest x-ray (US CDC, 2021)6 Additional tests at Higher Levels of Care Omnibus Health Guidelines ver. 2023 | 87 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care genes specific to B. anthracis Asthma Clinical assessment using GINA symptom control tool Spirometry preferred If spirometry is not available, peak expiratory flow rate (PEFR) using a peak flow meter (GINA, 2023)7 GINA, 20237 Breast Cancer Clinical breast examination, diagnostic mammography Strong (DOH, 2022)8 Candidiasis, Bacterial Vaginosis, Trichomoniasis Wet mount, Gram stain Cervical Cancer Cervical Cytology (Pap smear), VIA, HPV DNA Test Back to Table of Contents Spirometry Spirometry Peak expiratory flow (PEF) with reversibility test Chest X-ray (CXR) if the diagnosis is in doubt or considering other etiologies of cough and wheezing (e.g. Pulmonary Tuberculosis [PTB]) (GINA, 2023)7 Core needle Biopsy, histopathologic examination Breast Ultrasound For patients with confirmed breast cancer: Chest x-ray (to check for lung metastasis; Ultrasound of the liver (to check for liver metastasis Culture Strong (PHEX, 2021)9 Biopsy, histopathologic examination Spirometry Bronchial provocation test Allergy test Sputum Eosinophil Count Fractional Concentration of exhaled nitric oxide (FeNO) Other tests relevant to staging and therapeutic goals: CBC Metabolic panel (liver function tests, BUN, creatinine, calcium) Bone scan Biopsy Tumor HR status (ER and PR determinations HER2-receptor status of the recurrence Culture N/A Colposcopy, Biopsy, Tumor Markers (e.g. Cancer Antigen - 125 [CA-125]), Metastatic work-up (e.g. CT Scan, PET Scan) Omnibus Health Guidelines ver. 2023 | 88 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care Other diagnostic tests relevant to staging and therapeutic goals Chronic Kidney Disease (CKD) Clinical risk assessment, urinalysis, FBS,CBC creatinine, eGFR; CKD Risk Assessment Tool Chronic Obstructive Pulmonary Disease (COPD) Clinical Scoring system and handheld spirometry Colorectal Cancer FOBT or FIT Renal biopsy Dipstick Urine test or urinary albumin/creatinine ratio Electrolytes, acid- base workup using arterial blood gas (ABG), renal biopsy, renal US, CT angiogram, urodynamic studies, ureteroscopy; renal biopsy with electron microscopy (EM) and immunofluorescence microscopy (IF) assessment Weak (LCP, University of the Philippines National Institutes of Health Institute of Clinical Epidemiology, 2023)10 Facility-based spirometry CXR to detect causes of exacerbation, rule out other illnesses (GOLD, 2022)11 Facility-based spirometry Strong (PHEX, 2021)9 Biopsy, histopathologic examination N/A Colonoscopy, Biopsy, Tumor markers (e.g. Carcinoembryonic antigen [CEA], Alpha-fetoprotein [AFP]) Whole Abdominal CT Scan, Metastatic work-up Depends on the eye condition N/A Detailed ophthalmologic examination by a specialist Chest x-ray Chest x-ray Sputum gram stain and culture Complete blood count Urine testing for pneumococcal antigen Serum procalcitonin or c-reactive protein Other imaging tests: chest CT or ultrasound *for adults aged at least 50 years Common Eye Problems Basic eye examination (DOH, 201912) Community Acquired Pneumonia Pneumonia Severity Index (PSI) Rapid influenza molecular assay Confusion, Respiratory rate, Blood Pressure and Back to Table of Contents Strong (ATS & IDSA, 2019)13 Conditional (ATS & IDSA, 201913 Omnibus Health Guidelines ver. 2023 | 89 Condition Minimum Tests at Primary Care Age (CRB65) Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care UK-NICE, 202314 Contact Dermatitis Patch testing Weak (JRRMMC, University of the Philippines National Institutes of Health Institute of Clinical Epidemiology, 202315) Patch Testing Repeat open application test (ROAT) Repeat open application test (ROAT) Dengue Dengue NS1 Rapid Diagnostic Test (3 days from onset); Strong (RITM, University of the Philippines National Institutes of Health Institute of Clinical Epidemiology, 2023)16 Nucleic acid amplification tests (NAATs); RT-PCR Complete Blood Count with platelet count Nucleic acid amplification tests (NAATs); RT-PCR Dengue IgM/ IgG Rapid Diagnostic Test (5 days from the onset) Dengue NS1 Ag + IgM/IgG Liver function tests: Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT) Coagulation Test: PT, PTT Strong (RITM, University of the Philippines National Institutes of Health Institute of Clinical Epidemiology, 2023)16 Strong (RITM, University of the Philippines Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 90 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care National Institutes of Health Institute of Clinical Epidemiology, 2023)16 Diabetes Mellitus Asymptomatic: Repeat FBS or HbA1c 75-gram oral glucose tolerance test (75g OGTT) ADA, 202117; IDF, 201718; WHO, 202019 With classic symptoms: Random plasma glucose (RPG) determination FBS OR 75 g OGTT (confirmatory) OR Glycated Hemoglobin A1c Test (HbA1c or A1c) (ADA Professional Practice Committee, 2022)20 Lipid profile Liver function tests Spot urinary albumin-to-creatinine ratio Serum creatinine Estimated glomerular filtration rate (eGFR) Serum potassium (for patients with ACE-inhibitors, ARBs, or Diuretics, patients with Chronic Kidney Disease) Comprehensive eye examination and diabetic retinopathy screening (ADA Professional Practice Committee, 2022)20 Periodic psychosocial screening Symptom screening for sleep disorders and sleep disorders Screening for liver fibrosis in diagnosed T2DM patients with elevated ALT or fatty liver on ultrasound (Evidence C) Age- and sex-appropriate cancer screening tests HbA1c at least two times a year to check for glycemic control (ADA Professional Practice Committee, 202220) Diarrhea (Infectious) Back to Table of Contents Dehydration assessment Strong (PSMID, 2019)21 Stool Culture, PCR depending on etiology Fecalysis RDT: Cholera or shigella Complete Blood Count Urinalysis Serum Electrolytes Stool Culture, PCR depending on etiology Omnibus Health Guidelines ver. 2023 | 91 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care Blood Urea Nitrogen Creatinine Serum bicarbonate Dyslipidemia Lipid Profile (should include total cholesterol, LDL, HDL, and triglycerides) (PLAS 2020)22 NCEP, 200123 Lipid Profile (total cholesterol, LDL, HDL, triglycerides) (PLAS 2020)22 AST, ALT prior to initiation of statins in individuals with cirrhosis or at risk of developing liver injury (PLAS 2020)22 Creatine Kinase Other tests for causes of Dyslipidemia (e.g. metabolic disorders, genetic disorders) Possible genetic testing for patients suspected of having Familial Hypercholesterolemia (FH) Additional diagnostics to be requested based on suspected or known comorbidities Ebola Hemorrhagic Fever Clinical diagnosis RT-PCR N/A RT-PCR, Antibody-capture Enzyme-linked Immunosorbent Assay (ELISA) or Antigen-capture detection tests Filariasis Blood smear microscopy [Nocturnal Blood Exam (NBE)]; Filaria Test Strip RDT (FTS-RDT) NBE; RT-PCR N/A RT-PCR Generalized Anxiety Disorder Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) Detailed psychiatric evaluation; DSM-5 Assessment for self-harming behaviors and suicidal ideations. Thyroid function tests Complete Blood Count 12 lead electrocardiogram 2-hour 75-g oral glucose tolerance test Lipid profile, Serum Creatinine, estimated Glomerular Filtration Rate (eGFR), potassium, Dipstick Urine Gestational Diabetes Mellitus (GDM) in Pregnant Back to Table of Contents 2-hour 75-g oral glucose tolerance test (OGTT) at 24 to AAFP, 202224 Thyroid function tests Complete Blood Count 12 lead electrocardiogram Lipid profile, Serum Creatinine, estimated Glomerular Filtration Rate (eGFR), potassium, Dipstick Urine test or urinary Omnibus Health Guidelines ver. 2023 | 92 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care Women 28 weeks Age of Gestation (AOG) (OGTT) at 24 to 28 weeks (AOG) test or urinary albumin/creatinine ratio, ECG (ADA Professional Practice Committee, 202225) albumin/creatinine ratio, ECG (ADA Professional Practice Committee, 202225) Gestational Hypertension, Preeclampsia, or Chronic Hypertension with Superimposed in Pregnant Women Office BP Measurement using a a manual sphygmomanometer with appropriately-sized upper arm cuff, according to the Standard BP Measurement Protocol (PSH 2020)31 ABPM 12-lead Electrocardiogram (ECG); FBS; lipid profile; serum creatinine, eGFR, sodium, potassium; dipstick urine test or urinary albumin/ creatinine ratio (PSH 2020)31 ABPM Other tests if Pre-eclampsia and/or Hypertension-Mediated Organ Damage (HMOD) is suspected: Renal Ultrasound (US), Echocardiography, Brain Imaging, Ankle Brachial Index (ABI), Carotid Imaging, Retinal Exam (ESC 2018)26 Fundoscopy to check for hypertensive retinopathy Home BP monitoring (HBPM) if possible An oscillometric BP measurement device may be used if it is validated for pregnancy. (PSH 2020)31 Hand, Foot and Mouth Disease Clinical diagnosis DOH Department Memorandum 2022-057228 Viral culture N/A For fetal status: Ultrasonography to determine fetal growth every 3–4 weeks of gestation; amniotic fluid volume assessment at least once weekly Reverse Transcription Polymerase Chain Reaction (RT-PCR) Viral Culture Routine diagnostics plus ancillary tests Samples for virological investigation: Throat swab, Vesicle swab, Rectal swab/stool and CSF Hepatitis B, chronic disease Back to Table of Contents HBsAg Conditional (DOH, 202128) HBsAg AST and CBC to determine AST to Platelet Ratio Index (APRI) Score HBV DNA and ALT to determine treatment eligibility Ultrasound, serum AFP, liver function tests Omnibus Health Guidelines ver. 2023 | 93 Condition Hepatocellular carcinoma Human Immunodeficiency Virus Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Clinical assessment and referral to higher level of care Strong 2021)29 (DOH, HIV Rapid diagnostic test (RDT) Strong (WHO, 2021)30 Gold Standard N/A HIV-1 Nucleic Acid Test Additional Tests at Primary Care Level Bilirubin Liver aminotransferases Alkaline phosphatase Complete Blood Count with platelet count Prothrombin time Albumin Hepatitis B and C serology Blood Urea Nitrogen Creatinine Liver ultrasound Serum AFP ● ● ● ● ● ● ● ● ● ● Hypertension Back to Table of Contents Ambulatory blood pressure monitoring Recommended (PSH, 2020)31 Ambulatory BP Monitoring Plasma HIV RNA (viral load) CD4 cell count for identifying advanced HIV disease or for management of opportunistic infections Complete blood count; Chemistry profile: glucose, blood urea nitrogen and creatinine, liver enzymes and bilirubin Urinalysis Serologies for hepatitis A, B, and C viruses Serum lipids Age-appropriate TB symptom screening Pregnancy testing Syphilis testing Depression screening for adults living with HIV 12-lead Electrocardiogram (ECG); FBS; lipid profile; serum creatinine, Additional tests at Higher Levels of Care Multiphasic, contrast- enhanced CT Scan of the Liver Contrast-enhanced MRI Core needle biopsy Fine needle aspiration biopsy Rapid HIV diagnostic algorithm (rHIVda), CD4 count, Viral load testing HLA-B*5701 test (if abacavir is being considered) Genotypic drug-resistance testing for PLHIV on ART with unsuppressed viral load For patients who have HIV RNA levels <1,000 copies/mL, viral amplification for drug resistance ABPM Other tests if Hypertension-Mediated Omnibus Health Guidelines ver. 2023 | 94 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference (ABPM) Gold Standard (ABPM) Home BP monitoring Office BP Measurement (OBPM) Additional Tests at Primary Care Level eGFR, sodium, potassium; dipstick urine test or urinary albumin/ creatinine ratio Additional tests at Higher Levels of Care Organ Damage (HMOD) is suspected: Renal Ultrasound (US), Echocardiography, Brain Imaging, Ankle Brachial Index (ABI), Carotid Imaging, Retinal Exam (ESC 2018)26 Fundoscopy to check for hypertensive retinopathy Home BP monitoring (HBPM) if possible Influenza A(H5N1) (Highly Pathogenic Avian Influenza) Clinical diagnosis Rapid influenza diagnostic test (if indicated and available) Viral culture N/A Real-time RT PCR, Genome Sequencing, Serological Methods Influenza A H1N1 (Swine Flu) Clinical diagnosis Rapid influenza diagnostic test (if indicated and available) Viral culture N/A Real-time RT-PCR, viral culture and/ or four-fold rise in Influenza H1N1 virus specific neutralizing antibodies Iron-deficiency Anemia (IDA) Clinical diagnosis Hemoglobin Hematocrit CBC with RBC indices Bone marrow examination (if indicated) Peripheral blood smear, RDW (red cell distribution width) Reticulocyte count Ferritin Additional test if indicated: Serum iron concentration, Total iron binding capacity, transferrin saturation Colonoscopy if GI bleeding is suspected as the cause of IDA Leprosy Slit Skin Smear (SSS), complete blood count and chest x-ray Strong (DOH, 2021)32 Slit Skin Smear, Skin biopsy AST, ALT and renal function tests, and sputum smear microscopy Chest x-ray Fasting blood sugar Glucose-6-phosphate dehydrogenase deficiency (G6PD) deficiency screening prior to treatment and pathological examination of skin biopsies. Electrocardiogram and lipid profile Leptospirosis Clinical diagnosis Recommended (DOH, 2019)33 Polymerase Chain Reaction (PCR) or Culture Complete Blood Count with platelet count Urinalysis Culture and isolation, RT-PCR, microagglutination Test (MAT), specific IgM Rapid Diagnostic Tests (RDT), nonspecific Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 95 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care and isolation Blood Urea Nitrogen Creatinine ALT, AST Serologic testing for leptospirosis RDT, rapid diagnostic tests Lung Cancer CXR Conditional (PHEX, 2021)9 Biopsy, histopathologic examination N/A Chest CT Scan with contrast Biopsy, Bronchoscopy, Video-assisted thoracoscopy (VATS) Metastatic work-up Other diagnostic tests relevant to staging and therapeutic goals Major Depressive Disorder DSM-5 AAFP, 201834 Detailed psychiatric evaluation; DSM-5 Thyroid Stimulating Hormone (TSH) Complete Blood Count Serum Electrolytes Liver Function Tests Thyroid Stimulating Hormone (TSH) Complete Blood Count Serum Electrolytes Liver Function Tests Assessment for depression, intention for suicide or self harm. Malaria Malaria microscopy or malaria RDT Malaria microscopy CBC with platelet count Additional tests depending on the presence of severe disease (e.g. Liver function tests, kidney function tests) Meningococcemia Clinical diagnosis Culture of blood and CSF N/A Gram stain and culture of blood and CSF, CSF qualitative and quantitative analysis and quantitative analysis, RT-PCR of CSF Mental Disorders Directed Assessment at Primary Care according to WHO mental health gap action program (mhGAP) Intervention Guide – Version 2.035 Detailed psychiatric evaluation; DSM-5 N/A Detailed psychiatric evaluation; DSM-5 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 96 Condition Minimum Tests at Primary Care MERS-CoV Clinical diagnosis Methamphetamine Use Disorder DSM-5 Strength of Recommendation (if available) and Reference AAFP, 201834 Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care RT-PCR N/A RT-PCR Detailed psychiatric evaluation; DSM-5 Consider requesting laboratory tests as warranted to evaluate other medical conditions (e.g., electrocardiogram) Consider requesting laboratory tests as warranted to evaluate other medical conditions (e.g., electrocardiogram) Confirmatory for Methamphetami ne: gas chromatography /mass spectrometry Assessment for other psychiatric comorbidities, other substance use, medical comorbidities, and cardiovascular risk. Assessment for other psychiatric comorbidities, other substance use, medical comorbidities, and cardiovascular risk. Obesity Weight, height, BMI, waist circumference Weight, height, BMI, waist circumference Additional diagnostics to be requested based on suspected or known comorbidities Additional tests to work-up causes of obesity if not responding to recommended lifestyle modifications Oro-dental disorders Oral Examination (OE) Panoramic and intraoral radiographs Hot and cold water test for pulp vitality; percussion test using mouth mirror handle, palpation Temporomandibular joint (TMJ) series, Cone Beam Computed Tomography (CBCT) scan Scabies Clinical Diagnosis Confirmatory: Microscopic examination of skin scraping or mite examination N/A Dermoscopic examination or skin surface microscopy DOH, 202336 Consider additional tests for possible complications like secondary bacterial infection, sepsis, other systemic complications (e.g. glomerulonephritis), generalized urticaria. Schistosomiasis Fecalysis/Stool Microscopy Kato Katz Technique Ultrasound; Kato Katz Technique Hepatobiliary Ultrasound; Histopathology-Biopsy; Kato Katz Technique Soil-transmitted Fecalysis/Stool Kato Katz N/A Kato Katz Technique Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 97 Condition Minimum Tests at Primary Care Helminths (STH) Microscopy Stable Ischemic Heart Disease/ Chronic Stable Angina Pectoris Clinical assessment for angina ( features: 1) constricting discomfort in the front of the chest, or in the neck, shoulders, jaw or arms, 2) precipitated by physical exertion, 3) relieved by rest or nitroglycerin within about 5 minutes ; if all are present typical angina; if 2 are present - atypical angina; if 1 or none is present - non-anginal chest pain) Resting 12-L ECG in people whom clinical assessment cannot exclude stable angina Syphilis Rapid plasma reagin (RPR) and Treponema Pallidum Hemagglutination Assay (TPHA) Thyroid cancer, welldifferentiated Clinical diagnosis Back to Table of Contents Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care Technique UK-NICE, 20161, UK-NICE, 201637 Invasive coronary angiography Hypertension, Diabetes and Dyslipidemia Screening (UK-NICE, 20161, UK-NICE, 201637) Exercise Testing and Cardiac Imaging may be requested if clinically warranted (UK-NICE, 20161, UK-NICE, 201637) Strong (JRRMMC, 2021)38 Exercise testing (UK-NICE, 201637) Non-invasive cardiac imaging Functional cardiac testing Invasive coronary angiography Treponema Pallidum Hemagglutinat ion Assay (TPHA) Rapid syphilis test using immunochromatography (ICT) RPR-quantitative, when RPR-qualitative test is Reactive Confirmatory treponema test (TPHA or TPPA) is recommended whenever the RPR-qualitative is reactive Fine-needle aspiration biopsy Serum TSH, T4 (free or total) Diagnostic neck ultrasound Radionuclide thyroid scan FNAB US-guided FNAB Molecular testing Omnibus Health Guidelines ver. 2023 | 98 Condition Minimum Tests at Primary Care Strength of Recommendation (if available) and Reference Gold Standard Additional Tests at Primary Care Level Additional tests at Higher Levels of Care CT scan and/or MRI with intravenous contrast Tinea Clinical Diagnosis UpToDate, 202339; RACGP, 201940 Fungal Culture Potassium hydroxide (KOH) preparation on skin scrapings Fungal Culture Tuberculosis, pulmonary Sputum Xpert MTB/RIF or Xpert Ultra Strong (WHO, 2022)41 TB culture with phenotypic drug susceptibility test (DST) Acid-fast Bacilli (AFB) Sputum Smear Microscopy Chest X-ray Loop-mediated isothermal amplification (LAMP) Moderate Complexity NAAT Xpert MTB/XDR TB culture/phenotypic DST Sputum Trunat MTB-Rif Dx Low complexity Nucleic Acid Amplification Test (NAAT) Back to Table of Contents High complexity reverse hybridization based NAAT First-line line-probe assay (LPAs) Second-line LPAs Sequence-based testing (ie. Whole genome sequencing, pyrosequencing, Sanger sequencing) Omnibus Health Guidelines ver. 2023 | 99 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. U.K. National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. . Published November 30, 2016. Accessed December 16, 2023. https://www.nice.org.uk/guidance/cg95 Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22). doi:https://doi.org/10.1161/cir.0000000000001029 Basic emergency care: approach to the acutely ill and injured. Geneva: World Health Organization and the International Committee of the Red Cross 2018. Licence: CC BY-NC-SA 3.0 IGO. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/275635/9789241513081-eng.pdf?sequence=1 U.K. National Institute for Health and Care Excellence. Stroke and transient ischaemic attack in over 16s: diagnosis and initial management | Guidance | NICE. Nice.org.uk. Published 2022. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng128 Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021;52(7). doi:10.1161/str.0000000000000375 US Centers for Disease Control and Prevention. Anthrax Infection Diagnosis & Testing | CDC. www.cdc.gov. Published November 19, 2020. Accessed December 16, 2023. https://www.cdc.gov/anthrax/lab-testing/index.html Global Initiative for Asthma. GINA Main Report, Global Strategy for Asthma Management and Prevention.; 2023. Accessed December 16, 2023. https://ginasthma.org/2023-gina-main-report/ Department of Health. Breast Cancer National Clinical Practice Guidelines. 2022. https://drive.google.com/file/d/10i6pFr43H4cUAnOaY9bQNRC2_ETrtU6d/view Philippine Guidelines on Periodic Health Examination (PHEX) 1 Task Force Philippine Guidelines on Periodic Health Examination (PHEX) Phase 1. 2021. https://drive.google.com/drive/folders/1UXFurxj0dLH1J-Ua1KmrYaTuky7pON8Z Lung Center of the Philippines & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guidelines for the Management of Chronic Obstructive Pulmonary Disease. Published 2023. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/1kAx4VZrlqH3AQkQ-E35TSQLg7Z6wQud1 Global Initiative for Chronic Lung Disease, Inc [GOLD]. Global Strategy for the Diagnosis, Prevention, and Management of Chronic Obstructive Pulmonary Disease (2022 Report); 2022/ Accessed December 16, 2023. https://goldcopd.org/2022-gold-reports-2/ Department of Health. Administrative Order 2019-0055 “National Policy on the Prevention of Blin dness Program (PBP)” Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine. 2019;200(7):e45-e67. doi:https://doi.org/10.1164/rccm.201908-1581st UK National Institute of Health and Care Excellence. 1 Recommendations | Pneumonia in adults: diagnosis and management | Guidance | NICE. www.nice.org.uk. Published October 31, 2023. Accessed December 16, 2023. https://www.nice.org.uk/guidance/cg191/chapter/recommendations#lower-respiratory-tract-infection Jose R. Reyes Memorial Medical Center & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Philippine Clinical Practice Guidelines on Contact Dermatitis. 2023. https://drive.google.com/file/d/12x0ZdDhg9lBbTfLdCZ0qjCFuDE_8OWCg/view Research Institute for Tropical Medicine & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guideline on the Diagnosis, Management and Prevention of Dengue for Adult and Pediatric Filipinos. 2023. https://drive.google.com/file/d/1dsYIHm4UibfyP7FyFJeWsRQ5jXMZZNJp/view American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S15-S33. doi:https://doi.org/10.2337/dc21-s002 International Diabetes Federation. Type 2 diabetes. International Diabetes Federation. Published 2023. Accessed December 16, 2023. https://idf.org/about-diabetes/type-2-diabetes/ World Health Organization. HEARTS D: diagnosis and management of type 2 diabetes. 2020. https://www.who.int/publications/i/item/who-ucn-ncd-20.1 American Diabetes Association Professional Practice Committee. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2021;45(Supplement_1):S46-S59. doi:https://doi.org/10.2337/dc22-s004 Philippine Society for Microbiology and Infectious Disease. Clinical Practice Guidelines on the Management of Acute Infectious Diarrhea in Children and Adults. 2019. https://drive.google.com/drive/u/1/folders/1m-e_DkAucR9O_U58IrK2nCVnhYT3bFj9 Philippine Lipid and Atherosclerosis Society. Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. 2020. https://drive.google.com/file/d/1-_k8Uk9Lct56jT5T8xUcFQZoBAv_z8VL/view Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA: The Journal of the American Medical Association. 2001;285(19):2486-2497. doi:https://doi.org/10.1001/jama.285.19.2486 American Academy of Family Physicians. Generalized Anxiety Disorder and Panic Disorder in Adults. American Family Physician. 106(2):157-164. 2022. https://www.aafp.org/pubs/afp/issues/2022/0800/generalized-anxiety-disorder-panic-disorder.html American Diabetes Association Professional Practice Committee, American Diabetes Association Professional Practice Committee:, Draznin, B., Aroda, V. R., Bakris, G., Benson, G., Brown, F. M., Freeman, R., Green, J., Huang, E., Isaacs, D., Kahan, S., Leon, J., Lyons, S. K., Peters, A. L., Prahalad, P., Reusch, J., Young-Hyman, D., Das, S., & Kosiborod, M. 2022. 15. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2022. Diabetes care, 45(Suppl 1), S232–S243. https://doi.org/10.2337/dc22-S015 Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021-3104. doi:https://doi.org/10.1093/eurheartj/ehy339 Department of Health. DOH Department Memorandum 2022-0572: Guidelines on the Prevention, Detection, Isolation, Treatment and Reintegration - PDITR Strategy for Hand Foot and Mouth Disease. Published 2022. Accessed December 16, 2023. https://doh.gov.ph/sites/default/files/basic-page/Guidelines-on-the%20Prevention-Detection-Isolation-Treatment-and-Reintegration-P Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 100 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. DITR-Strategy-for-Hand-Foot-and-Mouth-Disease-HFMD.pdf Department of Health. Clinical Practice Guidelines for the Management of Hepatitis B in the Philippines. Published 2021. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/16PonztbznskCZhLpf1ro58ECYihNFOxP Department of Health. Philippine Clinical Practice Guideline for the Diagnosis and Management of Hepatocellular Carcinoma. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1jsxkDiqNgDw4353N2Ivl81waBHmmCsaY/view World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. www.who.int. Published July 16, 2021. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789240031593 Philippine Society of Hypertension. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 16, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view Department of Health. Leprosy Clinical Practice Guidelines. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1OmRtxsx4_02L-FDZjEcGZ28i7I7an0k4/view Department of Health. DOH Guidelines for Leptospirosis for Hospitals. Published 2019. Accessed December 16, 2023. https://drive.google.com/drive/folders/1pxQDWu3H1rmtGlXhJB2G1ZA1x09DREgk American Academy of Family Physicians. Stimulant and Designer Drug Use: Primary Care Management. American Family Physician. 98(2):85-92. 2018. https://www.aafp.org/pubs/afp/issues/2018/0715/p85.html World Health Organization. mhGAP Intervention Guide Mental Health Gap Action Programme for mental, neurological and substance use disorders in non-specialized health settings Version 2.0. Published 2016. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/250239/9789241549790-eng.pdf?sequence=1 Department of Health. Interim Guidance for the Diagnosis and Management of Scabies. Published 2023. Accessed December 16, 2023 https://doh.gov.ph/sites/default/files/basic-page/Interim-Guidance-for-the-Diagnosis-and-Management-of-Scabies.pdf UK National Institute of Health and Care Excellence. Overview | Stable angina: management | Guidance | NICE. www.nice.org.uk. Published August 25, 2016. Accessed December 16, 2023. https://www.nice.org.uk/guidance/cg126 Jose R. Reyes Memorial Medical Center. Philippine Interim Clinical Practice Guidelines for the Diagnosis and Management of Well-Differentiated Thyroid Cancer. 2021. https://drive.google.com/file/d/1RIcCFw2LWt30jufz7v3Y3jRocPsOEWFJ/view UpToDate. Dermatophyte (tinea) infections. Published 2023. Accessed December 16, 2023 https://www.uptodate.com/contents/dermatophyte-tinea-infections?search=tinea&source=search_result&selectedTitle=1~118&usage_ty pe=default&display_rank=1# Royal Australian College of General Practitioners. Superficial fungal infections. Australian Journal of General Practice. Published 2022. Accessed December 16, 2023. https://www1.racgp.org.au/ajgp/2019/october/superficial-fungal-infections World Health Organization. WHO consolidated guidelines on tuberculosis Module 5: Management of tuberculosis in children and adolescents. www.who.int. Published March 18, 2022. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789240046764 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 101 The Treatment of Common Conditions in Primary Care Summary Section: aims to summarize the first-line treatments for various diseases, including acute, chronic, and urgent/emergent conditions that are commonly encountered in primary care. The availability of these first-line treatments, including medications, procedures, and basic emergency interventions in primary care facilities or access within the HCPN is critical in achieving UHC and in ensuring quality care is provided at initial contact to all primary care clients. Primary care managers and clinicians should aim to make these available and accessible to their clients, through the use of various financing and contracting mechanisms, in line with the UHC Act (e.g., Philhealth financing, LGU procurement, Special Health Fund, etc.) General Principles ● ● ● ● ● ● ● An accurate diagnostic process, inclusive of well-performed history-taking, physical examination, and diagnostic testing, is a prerequisite for proper treatment. In the selection of treatment for a certain condition, always consider the evidence on safety, efficacy, and cost of the test, together with factors such as patient values and preferences, and the access to and availability of the treatment within the system (e.g., within the HCPN). Clearly communicate with the patient the benefits and harms of various treatment options and encourage participatory decision-making. Respect the patient’s autonomy and act in his/her best interests. Seek the patient’s informed consent for therapeutic interventions. Use clear language when providing instructions about treatment. Encourage and monitor treatment adherence. Treatment Options in Primary Care ● ● ● ● Table 11 is a consolidation of the first-line medications for conditions commonly encountered in primary care. Table 12 is a consolidation of the first-line procedures in primary care. Table 13 is a consolidation of basic emergency services that may be provided in primary care while awaiting or facilitating transfer to the nearest higher level facility. The list of conditions is arranged alphabetically for ease of navigation. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 102 Table 11. Summary of First-line medications for Conditions Encountered in Primary Care Disease/Condition First-line Medications Alzheimer’s Newly-diagnosed, mild, or moderate severity: Disease and Cholinesterase inhibitors - Donepezil 5mg orally once daily as starting dose, then 10mg daily as Vascular Dementia maintenance dose (increase after 4-6 weeks) Anthrax Strength of Recommendation (if available) and Guideline/Reference Grade 2A UpToDate, 20231 Moderate to advanced severity - Memantine 10mg twice daily (as add-on or as monotherapy) Grade 2B UpToDate, 20231 Severe Dementia - continue Memantine 10mg twice daily Grade 2C UpToDate, 20231 For post-exposure prophylaxis: Doxycycline 100mg every 12 hours,or Ciprofloxacin 500mg every 12 hours US CDC, 20142 For treatment of systemic anthrax: refer for admission and intravenous antibiotic administration (e.g. Ciprofloxacin 400mg every 8 hours PLUS Meropenem 2g every 8 hours PLUS Linezolid 600mg every 12 hours) Anxiety Disorders (Panic Disorder, Generalized Anxiety Disorder (GAD), Social Anxiety Disorder) Selective Serotonin Reuptake Inhibitors (SSRIs): Sertraline initial dose of 25-50mg daily then 50-200mg daily Fluoxetine initial dose of 10-20mg daily then 20-60mg daily Escitalopram initial dose of 5-10mg daily then 10-20mg daily Grade 2C Recommendation UpToDate, 20233 Asthma Inhaled corticosteroid (ICS)-formoterol: Budesonide-formoterol combination metered dose inhaler (MDI) 160mcg-4.5mcg/inhalation or dry powder inhaler (DPI) 200 mcg-6 mcg/inhalation Evidence B GINA, 20234 Step 1: 1 inhalation as needed Back to Table of Contents Evidence B GINA, 20234 Step 2: 1 inhalation as needed Evidence A GINA, 20234 Step 3: 1 inhalation once or twice daily, PLUS 1 inhalation whenever needed Evidence A GINA, 20234 Omnibus Health Guidelines ver. 2023 | 103 Disease/Condition First-line Medications Step 4: 2 inhalations twice daily, PLUS 1 inhalation whenever needed Strength of Recommendation (if available) and Guideline/Reference Evidence D GINA, 20234 Bacterial vaginosis Metronidazole 500 mg orally twice a day for 7 days, or (not a Metronidazole gel 0.75% 5g one full applicator intravaginally once a day for 5 days sexually-transmitt Clindamycin cream 2% 5g once full applicator intravaginally at bedtime for 7 days ed disease) US CDC, 20215 Bipolar Disorder Grade2B UpToDate, 20236 First line maintenance treatment is the same regimen that successfully treated the acute bipolar mood episode. Valproate Initial dose 500-750 mg/day in 1-4 divided doses, increase by 250-500mg every 1-3 days to reach usual therapeutic dose 1.5-2.5g, or Quetiapine Initial dose of 100-200 mg once daily at bedtime then increase by 100 mg/day to reach 400mg/day by day 4 Cancer Candidiasis Back to Table of Contents General Palliative care: Pain: Morphine 5-15mg every 4 hours as needed or scheduled around the clock UpToDate, 20237 Nausea and vomiting: metoclopramide 10mg every 4-6 hours, haloperidol 0.5-2mg every 6-8 hours, OR olanzapine 5mg once daily for 7 days Constipation: 8.6 sennosides/tablet 2 tablets once daily Xerostomia: oral hygiene Dysphagia: modify food and fluid consistency Insomnia: modify environment, encourage healthy sleep-wake cycle, minimize disruptions Depression: treat uncontrolled symptoms like pain, supportive psychotherapy Airway secretions: proper positioning, suctioning if available, Glycopyrronium 0.2 subcutaneous every 4-6 hours or IV infusion 0.6-1.2mg/day, or 0.1mg SL every 6 hours as needed UptoDate, 20238 Uncomplicated vulvovaginitis in non-pregnant: Single dose of oral fluconazole 150mg Grade 2C UpToDate, 20239 Vulvovaginitis in pregnancy: Clotrimazole 1% cream 1 applicatorful (5g) vaginally at bedtime for 7 days, or Miconazole 2% cream 1 applicatorful (5g) vaginally at bedtime for 7 days, or Grade 2C UpToDate, 20239 Omnibus Health Guidelines ver. 2023 | 104 Disease/Condition First-line Medications Strength of Recommendation (if available) and Guideline/Reference Nystatin suppository (100,000 units) 1 suppository vaginally at bedtime for 14 nights Cervicitis caused by chlamydial infection Doxycycline 100 mg orally twice a day for 7 days US CDC, 202110 Chronic Obstructive Pulmonary Disease (COPD) FEV≥80% or mmRC <2, not in exacerbation: Long acting Muscarinic Antagonist (LAMA) monotherapy E.g. Tiotropium dry powder inhaler (DPI) 18 mcg/capsule 1 inhalation daily or soft mist inhaler (SMI) 2.5mcg/actuation 2 inhalation once daily Weak recommendation LCP, University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology 202311 FEV<80% or mmRC≥2, not in exacerbation: Long Acting β2-Agonists (LABA)-LAMA combination therapy E.g. Tiotropium 2.5 mcg/olodaterol 2.5 mcg per actuation SMI 2 inhalations once daily Glycopyrrolate 50 mcg/indacaterol 110 mcg DPI 1 inhalation once daily Strong recommendation LCP, University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology 202311 FEV1<80% or mmRC≥2, with increased risk for exacerbations and absence of concurrent respiratory infection: Inhaled corticosteroids-LABA E.g. Budesonide-formoterol 160/4.5 mcg/actuation MDI 2 inhalations twice daily Strong recommendation LCP, University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology 202311 Pregnant Women: Azithromycin 1g orally in a single dose Community Acquired Pneumonia (Low Risk) For Low Risk CAP without comorbidities: Amoxicillin 500mg-1g thrice a day for 5-7 Low Risk CAP with stable comorbidities: β-lactam with β-lactamase inhibitor combinations (BLIC e.g. Co-amoxiclav 500/125mg thrice a day for 5-7 days) or second generation cephalosporins (e.g. Cefuroxime 500mg twice a day for 5-7 days) with or without extended macrolides (Azithromycin 500mg once a day OR clarithromycin 500mg twice a day for 3-5days) Dengue Oral rehydration solution for dengue without warning signs RITM, University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology, 202315 Diabetes Mellitus Metformin Alternatives: sulfonylureas, DPP4- inhibitors, SGLT-2 inhibitors, Insulin ADA, 202316 Dyslipidemia Statins Recommended Back to Table of Contents Strong Recommendation ATS & IDSA, 201912 UK-NICE, 201913 IDST, 201914 Omnibus Health Guidelines ver. 2023 | 105 Disease/Condition First-line Medications Strength of Recommendation (if available) and Guideline/Reference PLAS, 202017 Ebola Supportive care Hydrate orally or through IV infusion Give usual medication to support blood pressure, reduce vomiting and diarrhea, and to manage fever and pain. Treat other infections, if they occur. US CDC, 202118 Epilepsy, Juvenile Myoclonic Broad spectrum antiseizure drugs E.g. Valproate 10-15mg/kg/day in 1-4 divided doses Levetiracetam 500mg twice daily Grade 1A UpToDate, 202319 Extrapyramidal Symptoms (EPS) Diphenhydramine 25-50mg IV then continue orally for 2-3 days UpToDate, 202320 Hand, Foot and Mouth Disease (HFMD) Symptomatic treatment Give usual medications for fever and pain such as paracetamol or ibuprofen. Hydrate orally. US CDC, 202321 Hepatitis B infection, chronic, non-cirrhotic or cirrhotic Tenofovir Disoproxil Fumarate (TDF) or (Tenofovir Alafenamide) TAF or (Entecavir) ETV Strong DOH, 202151 Highly Pathogenic Avian Influenza A(H5N1) Oseltamivir 75mg orally twice daily for five days Grade 2C UpToDate, 202322 Hypertension Monotherapy or combination therapy using the following first-line drug classes: Recommended Angiotensin-converting enzyme inhibitors (ACEI) (e.g. Enalapril, captopril, lisinopril), PSH, 202023 Angiotensin-receptor blockers (ARB) (e.g., Telmisartan, Losartan, Valsartan), Calcium channel blockers (CCBs) (e.g. Amlodipine, Felodipine), Thiazide/Thiazide-like diuretics (e.g., Hydrochlorothiazide, Chlorthalidone Human Immunodeficiency Virus (HIV) Tenofovir (TDF) + Lamivudine (3TC) + Dolutegravir (DTG) 300mg once daily, 150mg twice daily or 300mg once daily, 50mg once daily (with additional dose of DTG 50mg if with Rifampicin-based regimen for TB treatment), or Back to Table of Contents Strong Recommendation WHO, 202124 Omnibus Health Guidelines ver. 2023 | 106 Disease/Condition First-line Medications Strength of Recommendation (if available) and Guideline/Reference TDF + Emtricitabine (FTC) + DTG 300 mg once daily, 200 mg once daily, 50 mg once daily, or TDF + 3TC (or FTC) + EFV 400 mg 300 mg once daily, 150 mg twice daily or 300 mg once daily, 400 mg once daily Ischemic Heart Disease For secondary prevention of cardiovascular event: Aspirin 75-100mg/day (If contraindicated, Clopidogrel 75 mg/day) Atorvastatin 40-80mg/day or Rosuvastatin 20-40mg/day UpToDate, 202325 UpToDate, 202325 Grade 2B UpToDate, 202325 Colchicine 0.5-0.6mg/day Rivaroxaban 2.5mg orally twice per day added with aspirin for high risk patients UpToDate, 202325 Others: beta-blockers, ACE inhibitors, ARBs, aldosterone blockers UpToDate, 202325 Leprosy Multi-drug treatment (MDT) Paucibacillary (PB) Leprosy Multibacillary (MB) Leprosy PB - 6 blister packs of Rifampicin, Dapsone and Clofazimine taken within 6-9 months MB - 12 blister packs of Rifampicin, Dapsone and Clofazimine taken within 12-18 months Weak recommendation DOH, 202126 For Leprae reaction: Corticosteroid Prednisolone 0.5mg/kg to 1mg/kg daily tapered by 5mg every 2 weeks until completion of 20 weeks Strong recommendation DOH, 202126 Leptospirosis For Mild leptospirosis: Doxycycline100 mg tab twice daily orally for 7-10 days For severe leptospirosis: intravenous antibiotics e.g. Penicillin G 1.5 million units IV q6 hours for 7 days, or Ceftriaxone 1g q24 hours for 7 days DOH, 201927 UpToDate, 202328 Filariasis (microfilaremia) Diethylcarbamazine(DEC) 6mg/kg for 12 days UpToDate, 202329 Major Depressive Disorder Escitalopram initial dose 10mg daily then 10-20mg daily, or fluoxetine initial dose 20mg daily then 20-60mg daily, sertraline initial dose 50mg daily then 50-200 daily Recommendation for Use APA, 201930 Strong Recommendation ACP, 202331 UK-NICE, 202232 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 107 Disease/Condition First-line Medications Strength of Recommendation (if available) and Guideline/Reference UpToDate, 202333 Malaria Uncomplicated Malaria For all species (P. falciparum, P. vivax, P. malariae, P. ovale, P. knowlesi), regardless if it is single species Strong Recommendation infection or a mixed type: Artemether Lumefantrine (AL) Target dose: Artemether 5-24mg/kg and WHO, 202334 lumefantrine 29-144mg/kg, to be given twice a day for 3 days (total of 6 doses), the first 2 doses should be given 8 hours apart. For uncomplicated P. falciparum with treatment failure or hypersensitivity with AL, or with limited Strong Recommendation access to AL: Pyronaridine-artesunate (PA) 60 mg + 180 tablet55 WHO, 202334 DM 2023-012856 Meningococcemia Ceftriaxone 2g IV every 12 hours US CDC, 202235 Grade 1B UpToDate, 202336 Methamphetamine Psychosocial therapy using contingency management with or without other behavioral interventions Use Disorder Weak Recommendation US DVA, 202137 UpToDate, 202338 Middle Eastern Respiratory Syndrome Coronavirus (MERS-CoV) Supportive Care Treat with antibiotics if with secondary bacterial infection US CDC, 201939 Rabies Post exposure prophylaxis: DOH AO 2018-001340 Category I ● No vaccine or Rabies Immunoglobulin (RIG) needed Category II ● Rabies Vaccination regimen until Day 7 for WHO Prequalified (PQ) vaccines and until day 28 for Non PQ vaccines ● RIG not indicated Category III ● Give both vaccine and RIG ● Complete rabies vaccination regimen until Day 7 for WHO PQ vaccines and until day 28 for Non PQ vaccines Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 108 Disease/Condition First-line Medications Strength of Recommendation (if available) and Guideline/Reference Purified Verocell rabies Vaccine (PVRV) 0.5ml/ vial ● ID 0.1ml given at Day 0, 3, 7, 28 ● IM 0.5ml given at Day 0, 7, 21 or Day 0, 3, 7, 14 Purified Chick Embryo Cell Vaccine (PCECV) 1ml/vial ● ID 0.1ml given at Day 0, 3, 7, 28 ● IM 1.0ml given at Day 0, 7, 21 or Day 0, 3, 7, 14 Human Rabies Immune Globulin (HRIG) 150 IUml at 2ml/vial dose: 20 IU/kg Equine Rabies Immune Globulin (ERIG) 200IU/ml at 5ml/vial dose: 40 IU/kg *Procurement of non-WHO Prequalified Cell Culture & Embryonated Egg-based Vaccine (CCEEV) shall cease when WHO-prequalified vaccines become available and have a stable supply in the market. Schistosomiasis Praziquantel 60mg’kg per day orally in 3 divided doses for one day US CDC, 202041 Seizure, Focal Onset Gabapentin 300-600mg thrice a day Oxcarbazepine 300-600mg/day in 2 divided doses Carbamazepine Initial 2-3mg/kg/day in 2-4 divided doses, may gradually increase every ≥5 days in increments of ≤200 mg/day to a usual maintenance dose of ~10 mg/kg/day in 2 to 4 divided doses UpToDate, 202342 Seizure, Generalized Onset Valproate 10-15mg/kg/day in 1-4 divided doses Levetiracetam 500mg twice daily Topiramate 50mg/day UpToDate, 202342 Seizure, Unknown Onset Valproate 10-15mg/kg/day in 1-4 divided doses Levetiracetam 500mg twice daily Topiramate 50mg/day UpToDate, 202342 Soil-transmitted Helminthiasis Albendazole (400 mg) Mebendazole (500 mg) Strong Recommendation WHO, 202343 Syphilis Parenteral Benzathine Penicillin G administered parenterally, is the preferred drug for treating patients Strong Recommendation in all stages of syphilis. USPSTF, 201844 Trichomoniasis Metronidazole For Women: Metronidazole 500 mg 2 times/day for 7 days For Men: Metronidazole 2 g orally in a single dose Back to Table of Contents Strong Recommendation US CDC, 202145 Omnibus Health Guidelines ver. 2023 | 109 Disease/Condition Tuberculosis First-line Medications Strength of Recommendation (if available) and Guideline/Reference For drug-susceptible TB: ● Regimen 1: 2HRZE (Isoniazid-RifampicinPyrazinamide-Ethambutol)/4HR ● Regimen 2: 2HRZE/10HR (for EPTB of CNS, bones, joints) Wherein: Isoniazid (H): 4 - 6 mg/kg, 300 mg formulation Rifampicin (R): 8 - 12 mg/kg, 300 mg formulation Ethambutol (E): 15 - 25 mg/kg, 400 mg formulation Pyrazinamide (Z): 20 - 30 mg/kg, 500 mg formulation Strong recommendation WHO, 202246 For TB Preventive Treatment: ● Weekly: Isoniazid/Rifapentine for 12 weeks ● Daily Isoniazid for 6 months ● Daily Isoniazid/Rifampicin for 3 months ● Daily Rifampicin for 4 months Uncomplicated Gonococcal infections of the cervix, urethra, and rectum; Ceftriaxone 500 mg* IM in a single dose for persons weighing <150 kg Strong recommendation US CDC, 202147 * For persons weighing ≥150 kg, 1 g ceftriaxone should be administered. Table 12. Summary of First-line Procedures for Conditions Encountered in Primary Care Condition Primary Care Procedures Animal Bite Aseptic Wound Care Referral to Animal Bite Center Dengue Supportive care-rehydration with oral or intravenous fluids Dental caries Atraumatic Restorative Treatment (ART) using fluoride releasing restorative material (Glass Ionomers) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 110 Dental root caries Topical application of Silver Diamine Fluoride Food and water-borne diarrhea/gastroenteritis) Diseases (infectious Supportive care-rehydration with oral or intravenous fluids Foreign Body Foreign body removal Gingivitis Oral Prophylaxis Known Rheumatic Heart Disease Monthly intramuscular injections of Penicillin G prophylaxis Musculoskeletal Injuries Immobilization with bandage or splint Non-bite Traumatic Wound (minor wound) Wound Care; Rest, immobilize, apply cold compress, and elevate injured part (RICE) Application of topical antiseptic Debridement and/or suturing, as needed Tetanus vaccination (according to immunization status) Oral Urgent Treatment (OUT) Relief of pain, removal of unsavable tooth, referral of complicated cases to higher levels of care Periodontitis Deep scaling, root planing and debridement, referral to higher levels of care (if necessary) Various Vaccine-Preventable Conditions Immunization White spot lesion (White opacities seen on tooth/teeth) Topical application of Fluoride Varnish Table 13. Summary of Basic Emergency Services at Primary Care Condition First Line Medication First Line Procedure or Procedures that can be done at primary care Active gastrointestinal bleeding (hematochezia/ hematemesis) Intravenous proton pump inhibitor (e.g. Omeprazole) IV Fluid resuscitation Nasogastric tube (NGT) insertion (for decompression) Acute infectious diarrhea/ gastroenteritis with severe dehydration Oral rehydration solution NGT insertion if unable to tolerate oral intake Acute Neurologic Symptoms due to hypoglycemia Intravenous glucose (Dextrose 50% solution)48 IV Access Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 111 Condition First Line Medication First Line Procedure or Procedures that can be done at primary care Aggressive or agitated behavior Evaluate for possible underlying causes and rule out other possible causes: ● Check blood glucose. If low, give glucose ● Check vital signs. If with desaturation, give oxygen. ● Rule out delirium, medical causes including poisoning, drug and alcohol use, and agitation due to psychosis or manic episodes in bipolar disorder. ● Sedate as appropriate to prevent injury (WHO, 2016b): ○ Agitation due to mania or psychosis: Haloperidol 2 mg PO/IM hourly up to 5 doses (maximum 10 mg). Cautiously check for dystonic reactions from high doses of Haloperidol. Biperiden may be used to treat acute reactions. ○ Agitation due to ingestion of substances, such as alcohol/ sedative withdrawal or stimulant intoxication, use Diazepam 10-20 mg PO and repeat as needed. ○ Extreme violence: Haloperidol 5 mg IM, repeat in 15-30 mins if needed (maximum 15 mg) In case of extreme violence, seek help from police or staff, consult a specialist, and facilitate transfer to a capable facility. Altered Mental Status Oxygen support IV fluids IV glucose for hypoglycemia (CBG <70 mg/dL) Other medications depending on the cause of altered mental status (e.g. naloxone for opioid overdose, benzodiazepine for active seizure/convulsion, magnesium sulfate for suspected eclampsia, glucose and benzodiazepine for alcohol withdrawal)48 Rapid assessment (ABCDE), AVPU assessment to check level of consciousness, GCS to check trauma patients, quick focused history taking and PE, capillary blood glucose measurement, basic emergency care48 Anaphylaxis Epinephrine48 IV Access, Basic Emergency Care for shock, airway obstruction/ respiratory distress, cardiac arrest48 Asthma Exacerbation See Asthma Disease-specific Guidance Transfer to Acute Care Facility if not responding to medications. Cardiac Arrest Epinephrine, intravenous (IV) fluids BLS/CPR, including bag-valve ventilation48, 50 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 112 Condition First Line Medication First Line Procedure or Procedures that can be done at primary care Closed Fracture Pain reliever Splint/Immobilization COPD Exacerbation See COPD Disease-specific Guidance Refer immediately to at least a Level 2 health facility, preferably with an ICU. Dental extraction with uncontrolled or profuse bleeding Tranexamic acid Suturing of the extraction site Dental injury, traumatic Pain reliever (e.g. Non-steroidal anti-inflammatory drugs like Mefenamic acid, Ibuprofen) and antibiotics For avulsed teeth (permanent) at the place of accident: Find the tooth; avoid touching the root portion; transfer it in a suitable & convenient storage medium with milk, HBSS or saliva; and urgently bring the medium with the patient to the clinic the soonest for higher chance of reimplantation. Tooth splint and referral to dentist, dental professional or to higher levels of care (orthodontist, oral and maxillofacial surgeon) Difficulty of breathing (DOB) Oxygen Support Other medications depending on suspected cause of difficulty of breathing (e.g. Epinephrine for anaphylaxis, short-acting beta-agonist (SABA) for asthma exacerbation, aspirin for suspected ACS, naloxone for opioid overdose)48 Rapid assessment (ABCDE), quick focused history taking and PE, basic emergency care (including bag-valve-mask ventilation if unconscious)48 Disorders due to Substance Use: Alcohol intoxication, Opioid Overdose, Alcohol or Sedative Withdrawal, Stimulant Intoxication, Delirium Associated with Substance Use Naloxone if with suspected opioid overdose If with sedative intoxication (e.g. alcohol, opioids, other sedatives), drug overdose, or withdrawal - Check Airway, Breathing, Circulation (ABC), provide initial respiratory support (e.g. bag-valve -mask ventilation), give oxygen, provide basic emergency care as needed48 Benzodiazepine (e.g Diazepam) if with suspected alcohol, Benzodiazepine or other sedative withdrawal. Thiamine 100 mg daily for five days if with suspected alcohol withdrawal Diazepam for acute stimulant intoxication; Haloperidol if not responding to Diazepam Haloperidol if with suspected alcohol or sedative withdrawal and delirium Back to Table of Contents Additional interventions: 1. Psychoeducation 2. Motivational Interviewing 3. Strategies for Reducing and Stopping Use: a. Identify triggers for use and ways to avoid them b. Identify emotional cues for use and ways to cope with them c. Encourage the person not to keep substances at home Omnibus Health Guidelines ver. 2023 | 113 Condition First Line Medication First Line Procedure or Procedures that can be done at primary care Methadone or Buprenorphine for opioid withdrawal; if either is not available - use another opioid e.g. Morphine Sulphate or an alpha agonist e.g. Clonidine or Lofexidine Eclamptic Seizure Magnesium sulfate Solution (for intravenous and intramuscular administration)48 Supplemental oxygen IV access Place patient in lateral position, if possible Immediately transfer to CEmONC facility Emergency labor Administer a loading dose of life saving drugs, as applicable, prior to transport to a Referral Hospital such as52: ● Oxytocin, ● Magnesium sulfate, ● Antibiotics, ● Maternal steroids IV Access Immediately transfer to CEmONC facility Hypertensive Emergency/ Hypertensive Crisis (severe BP Intravenous Nicardipine or Labetalol if available53 IV Access Adjust/intensify maintenance medications, ensure adherence to therapy, and arrange follow-up within a short period53 Not applicable Close follow-up on an outpatient basis elevation accompanied by new or worsening target organ damage or dysfunction) Hypertensive Urgency (severe BP elevation in a stable patient WITHOUT acute organ damage or change in baseline target organ damage or dysfunction) Medically Serious Act of Self Harm/ Imminent Risk of Self-Harm / Suicide See Table 7 for the management of concurrent Mental Health conditions Musculoskeletal injury with profuse bleeding Tranexamic acid Back to Table of Contents 1. 2. 3. 4. 5. Place the person in a secure and supportive environment (do not leave them alone) Remove access to means of self-harm Refer to mental health specialist/higher level of care Ensure continuity of care Include the carers if the person wants their support during assessment and treatment49 IV fluid resuscitation If with profuse or life-threatening bleeding - Direct manual pressure application if a manufactured tourniquet is not immediately Omnibus Health Guidelines ver. 2023 | 114 Condition First Line Medication First Line Procedure or Procedures that can be done at primary care available or fails to stop bleeding; tourniquet application with a manufactured tourniquet is available50 Non-eclamptic Seizure Benzodiazepine (e.g. Midazolam, Diazepam)48 IV access Airway protection48 Poisoning (includes chemicals, snakebites and toxins) Antidote/antivenom54 if available IV fluids and oxygen support as needed Emergency stabilization, Basic Emergency Care, Decontamination, Immediate transport to nearest hospital Possible Acute Coronary Syndrome Aspirin loading dose Statin Sublingual nitroglycerin or nitrate (e.g. isosorbide dinitrate [ISDN]) for pain relief. Note: the absence or presence of response to nitroglycerin or nitrate administration should not be used to diagnose the absence or presence of acute coronary syndrome (UK-NICE, 2016) Basic emergency care48, 50 Possible Stroke Not applicable at primary care (imaging needed to rule out hemorrhagic stroke) Basic emergency care48 Shock IV fluids appropriate for the patient’s age and condition (Ringer’s lactate if with normal nutritional status)48 Hydration via nasogastric tube if no IV fluid available Oxygen support Other medications depending on the cause of shock (e.g. oxytocin for postpartum hemorrhage, aspirin for suspected heart attack, epinephrine for anaphylaxis) Rapid assessment (ABCDE), quick focused history taking and PE, basic emergency care including IV access and fluid resuscitation48 Trauma IV fluids if bleeding or in shock48, 50 Rapid assessment (ABCDE) and basic emergency care, proper immobilization (e.g. cervical spine immobilization) If with profuse or life-threatening bleeding - Direct manual pressure application if a manufactured tourniquet is not immediately available or fails to stop bleeding; tourniquet application with a manufactured tourniquet is available48, 50 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 115 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. UpToDate. Treatment of Alzheimer Disease. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/treatment-of-alzheimer-disease?search=alzheimer%20dementia&source=search_result&selectedTitle=2~150&usag e_type=default&display_rank=2#H23 Hendricks KA, Wright ME, Shadomy SV, et al. US Centers for Disease Control and Prevention Expert Panel Meetings on Prevention and Treatment of Anthrax in Adults. Emerging Infectious Diseases. 2014;20(2). doi:https://doi.org/10.3201/eid2002.130687 UpToDate. Generalized anxiety disorder in adults: Management. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/generalized-anxiety-disorder-in-adults-management?search=generalized%20anxiety%20disorder&source=search_ result&selectedTitle=2~150&usage_type=default&display_rank=2# Global Initiative for Asthma. GINA Main Report, Global Strategy for Asthma Management and Prevention. Published 2023. Accessed December 16, 2023. https://ginasthma.org/2023-gina-main-report/ United States Center for Disease Control and Prevention. Bacterial Vaginosis - STI Treatment Guidelines. www.cdc.gov. Published 2021. Accessed December 16, 2023. https://www.cdc.gov/std/treatment-guidelines/bv.htm UpToDate (2023). Bipolar disorder in adults: Choosing maintenance treatment. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/bipolar-disorder-in-adults-choosing-maintenance-treatment?search=bipolar%20II%20treatment&source=search_r esult&selectedTitle=1~150&usage_type=default&display_rank=1# UpToDate. Cancer pain management with opioids: Optimizing analgesia. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/cancer-pain-management-with-opioids-optimizing-analgesia?search=cancer%20pain%20management&source=se arch_result&selectedTitle=1~150&usage_type=default&display_rank=1# UpToDate. Overview of managing common non-pain symptoms in palliative care.Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/overview-of-managing-common-non-pain-symptoms-in-palliative-care?source=history_mobile# UpToDate. Candida vulvovaginitis in adults: Treatment of acute infection. 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/candida-vulvovaginitis-in-adults-treatment-of-acute-infection?search=candidiasis%20treatment&source=search_r esult&selectedTitle=2~150&usage_type=default&display_rank=2# United States Centers for Disease Control and Prevention. Diseases Characterized by Urethritis and Cervicitis.Published 2021. Accessed December 16, 2023. https://www.cdc.gov/std/treatment-guidelines/urethritis-and-cervicitis.htm Lung Center of the Philippines & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guidelines for the Management of Chronic Obstructive Pulmonary Disease. Published 2023. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/1kAx4VZrlqH3AQkQ-E35TSQLg7Z6wQud1 Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. American Journal of Respiratory and Critical Care Medicine. 2019;200(7):e45-e67. doi:https://doi.org/10.1164/rccm.201908-1581st U.K. National Institute for Health and Care Excellence. Pneumonia (community-acquired): antimicrobial prescribing. Published 2019. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng138/chapter/Recommendations Chou CC, Shen CF, Chen SJ, et al. Recommendations and guidelines for the treatment of pneumonia in Taiwan. Journal of Microbiology, Immunology and Infection. 2019;52(1):172-199. doi:https://doi.org/10.1016/j.jmii.2018.11.004 Research Institute for Tropical Medicine & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guideline on the Diagnosis, Management and Prevention of Dengue for Adult and Pediatric Filipinos. 2023. https://drive.google.com/file/d/1dsYIHm4UibfyP7FyFJeWsRQ5jXMZZNJp/view American Diabetes Association. Standards of Care in Diabetes—2023 Abridged for Primary Care Providers. Clinical Diabetes. 2022;41(1). doi:https://doi.org/10.2337/cd23-as01 Philippine Lipid and Atherosclerosis Society. Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. 2020. https://drive.google.com/file/d/1-_k8Uk9Lct56jT5T8xUcFQZoBAv_z8VL/view United States Centers for Disease Control and Prevention. Ebola Disease: Treatment. CDC. Published February 26, 2021. Accessed December 16, 2023. https://www.cdc.gov/vhf/ebola/treatment/index.html UpToDate. Juvenile myoclonic epilepsy. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/juvenile-myoclonic-epilepsy?search=epilepsy%20juvenile%20myoclonic&source=search_result&selectedTitle=1~39 &usage_type=default&display_rank=1# UpToDate. First-generation (typical) antipsychotic medication poisoning. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/first-generation-typical-antipsychotic-medication-poisoning?search=extrapyramidal%20symptoms%20treatment& source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1# United States Centers for Disease Control and Prevention. How to Treat Hand, Foot, and Mouth Disease. Published 2023. Accessed December 16, 2023. https://www.cdc.gov/hand-foot-mouth/about/treatment.html#:~:text=There%20is%20no%20specific%20medical%20treatment%20for%20HFMD.&text =You%20can%20make%20 steps%20to,can%20include%20acetaminophen%20or%20ibuprofen UpToDate. Avian influenza: Treatment and prevention. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/avian-influenza-treatment-and-prevention?search=avian%20influenza%20treatment&source=search_result&select edTitle=1~40&usage_type=default&display_rank=1# Philippine Society of Hypertension. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 16, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. www.who.int. Published July 16, 2021. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789240031593 UpToDate. Prevention of cardiovascular disease events in those with established disease (secondary prevention) or at very high risk. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/prevention-of-cardiovascular-disease-events-in-those-with-established-disease-secondary-prevention-or-at-veryhigh-risk?search=ischemic%20heart%20disease%20%20treatment&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2# Department of Health. Leprosy Clinical Practice Guidelines. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1OmRtxsx4_02L-FDZjEcGZ28i7I7an0k4/view Department of Health. DOH Guidelines for Leptospirosis for Hospitals. 2019 edition. DOH: 2017. https://drive.google.com/drive/folders/1pxQDWu3H1rmtGlXhJB2G1ZA1x09DREgk UpToDate. Leptospirosis: Treatment and prevention. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/leptospirosis-treatment-and-prevention/print Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 116 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. UpToDate. Lymphatic filariasis: Treatment and prevention. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/lymphatic-filariasis-treatment-and-prevention?search=lymphatic%20filariasis&source=search_result&selectedTitl e=2~33&usage_type=default&display_rank=2# Mcquaid J, Lin E, Washington K, et al. Clinical Practice Guideline for the Treatment of Depression across Three Age Cohorts American Psychological Association Guideline Development Panel for the Treatment of Depressive Disorders. APA; 2019. Accessed December 16, 2023. https://www.apa.org/depression-guideline/guideline.pdf Qaseem A, Owens DK, Etxeandia-Ikobaltzeta I, Tufte J, Cross JT, Wilt TJ. Nonpharmacologic and Pharmacologic Treatments of Adults in the Acute Phase of Major Depressive Disorder: A Living Clinical Guideline From the American College of Physicians. Annals of Internal Medicine. 2023;176(2):239-252. doi:https://doi.org/10.7326/m22-2056 U.K. National Institute for Health and Care Excellence. Recommendations | Depression in adults: treatment and management | Guidance | NICE. www.nice.org.uk. Published June 29, 2022. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng222/chapter/Recommendations#further-line-treatment UpToDate. Unipolar major depression in adults: Choosing initial treatment. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/unipolar-major-depression-in-adults-choosing-initial-treatment?search=major%20depressive%20disorder%20trea tment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1# World Health Organization. WHO Guidelines for Malaria. Published October 16, 2023. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/373339/WHO-UCN-GMP-2023.01-Rev.1-eng.pdf?sequence=1 United States Centers for Disease Control and Prevention. Meningococcal Disease. Published 2022. Accessed December 16, 2023. https://www.cdc.gov/meningococcal/clinical-info.html UpToDate. Treatment and prevention of meningococcal infection. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/treatment-and-prevention-of-meningococcal-infection?search=meningococcemia&source=search_result&selected Title=2~40&usage_type=default&display_rank=2# United States Department of Veteran Affairs. Clinical Practice Guideline for the Management of Substance Use Disorders. Published 2021. Accessed December 16, 2023. https://www.healthquality.va.gov/guidelines/MH/sud/VADoDSUDCPG.pdf UpToDate. Stimulant Use Disorder: Treatment Overview.Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/stimulant-use-disorder-treatment-overview United States Centers for Disease Control and Prevention. Middle East Respiratory Syndrome (MERS): Prevention & Treatment. Published 2019. Accessed December 16, 2023. https://www.cdc.gov/coronavirus/mers/about/prevention.html Department of Health. DOH AO 2018-0013: Revised Guidelines on the Management of Rabies Exposures. Published 2018. Accessed December 16, 2023. https://www.psmid.org/wp-content/uploads/2020/03/CPG-rabies-AO-2018-0013.pdf United States Centers for Disease Control and Prevention. Parasites - Schistosomiasis: Resources for Health Professionals. Published 2020. Accessed December 16, 2023. https://www.cdc.gov/parasites/schistosomiasis/health_professionals/index.html#tx UpToDate. Initial treatment of epilepsy in adults. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/initial-treatment-of-epilepsy-in-adults?search=focal%20seizure%20treatment&source=search_result&selectedTitl e=1~150&usage_type=default&display_rank=1# World Health Organization. Soil-transmitted helminth infections. Published 2023. Accessed December 16, 2023. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections#:~:text=and%20heavy%20intensity.-,Treatment,few%20and% 20minor%20side%2Deffects United States Preventive Services Task Force. Syphilis Infection in Pregnant Women: Screening. Published September 4, 2018. Accessed December 16, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/syphilis-infection-in-pregnancy-screening United States Centers for Disease Control and Prevention. Sexually Transmitted Infections Treatment Guidelines, 2021 - Trichomoniasis. Published 2021. Accessed December 16, 2023. https://www.cdc.gov/std/treatment-guidelines/trichomoniasis.htm World Health Organization. WHO operational handbook on tuberculosis: module 4: treatment: drug-resistant tuberculosis treatment. Published 2020. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789240006997 United States Centers for Disease Control and Prevention. Sexually Transmitted Infections Treatment Guidelines, 2021 - Gonococcal Infections Among Adolescents and Adults. Published 2021. Accessed December 16, 2023. https://www.cdc.gov/std/treatment-guidelines/gonorrhea-adults.htm Basic emergency care: approach to the acutely ill and injured. Geneva: World Health Organization and the International Committee of the Red Cross 2018. Licence: CC BY-NC-SA 3.0 IGO. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/275635/9789241513081-eng.pdf?sequence=1 World Health Organization. Practice Manual for establishing and maintaining surveillance systems for suicide attempts and self-harm. Published 2016. Accessed December 16, 2023. https://iris.who.int/bitstream/handle/10665/208895/9789241549578_eng.pdf?sequence=1 Pellegrino JL, Charlton NP, Carlson JN, et al. 2020 American Heart Association and American Red Cross Focused Update for First Aid. Circulation. 2020;142(17). doi:https://doi.org/10.1161/cir.0000000000000900 Department of Health. Clinical Practice Guidelines for the Management of Hepatitis B in the Philippines. Published 2021. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/16PonztbznskCZhLpf1ro58ECYihNFOxP Department of Health. DOH Administrative Order No. 2015-0020 : Guidelines in the Administration of Life-Saving Drugs During Maternal Care Emergencies by Nurses and Midwives in Birthing Centers. Published 2015. Accessed December 16, 2023. https://elibrary.judiciary.gov.ph/thebookshelf/showdocs/10/70257#:~:text=This%20Guideline%20mandates%20the%20health,and%20other%20related %20training%20courses Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Journal of the American College of Cardiology. 2018;71(19):e127-e248. doi:https://doi.org/10.1016/j.jacc.2017.11.006 Research Institute of Tropical Medicine. First aid for snake bite: What to do when bitten by a snake. Published August 27, 2018. Accessed December 16, 2023. https://ritm.gov.ph/first-aid-for-snake-bite-what-to-do-when-bitten-by-a-snake/ World Health Organization. Model List of Essential Medicines. n.d. https://list.essentialmeds.org/?query=Pyronaridine-artesunate+ Department of Health. Department Memorandum No. 2023-0128: Guidelines on the Use of Pyronaridine-artesunate as Second-line Artemisinin-based Combination Therapy (ACT) for the Treatment of Malaria. 2023. https://drive.google.com/file/d/1qsBkQeZj2av8U-cTzp5kOT25cegy9ce3/view Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 117 PART II: Specific Guidance for Common and High Burden Diseases in Adults This part provides more detailed evidence-based standards on common and/or high-burden conditions presenting at primary care and encompasses the signs, symptoms, and the disease-specific spectrum of care from screening (if applicable) to referral. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 118 NonCommunicable Diseases (NCDs) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 119 Acute Myeloid Leukemia is a type of leukemia which is characterized as a “heterogeneous malignancy defined by clonal proliferation and improper differentiation of myeloid precursors”1. In AML, chromosomal translocations result in the production of chimeric proteins that are disruptive to the normal myeloid precursor cell maturation process1. From 1990 to 2017, worldwide disease burden of AML has risen steadily from 63,840 to 119,570 cases1 with the highest prevalence found in Western Europe and South Asia geographical zones1. In the Philippines, cancer remains to be among the top three leading causes of mortality1. Among cancer-related mortalities, leukemia ranks 5th among all cases, with up to 4,370 deaths1. The five-year survival rate of AML for those under 20 years of age is 68% which sharply decreases to 26% for those over 20 years old1. Early recognition and management are key to improving the survival of patients. Table 14. Acute Myeloid Leukemia Continuum of Care Overview Acute Myeloid Leukemia (AML) Overview Risk Factors Screening Diagnosis Pharmacologic Treatment Supportive and Palliative Care History of Myelodysplastic syndrome History of Myelofibrosis Aplastic anemia Down's syndrome Bloom syndrome Exposure to radiation therapy and/or cytotoxic agents like, tobacco, and/or benzene Not Applicable Minimum at primary care: Complete blood count (CBC) with platelet count, Peripheral Blood Smear (PBS), Reticulocyte Count Gold Standard. Confirmatory Multiparameter flow cytometry for patients with low RBC and low WBC counts, if available. Refer to higher level of care for appropriate treatment Psychosocial Care Palliative Care Pain Management End-of-life Care Concerns Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 120 Signs and Symptoms ● Suspect the presence of a hematologic malignancy such as Acute Myeloid Leukemia in an adult who presents with any of the following symptoms, appearing over a few weeks and becoming more severe over time1: ○ Fatigue/exhaustion ○ Weight loss ○ Fever ○ Night sweats/ excessive sweating ○ Loss of appetite ○ Headache ○ Pale or "washed-out" skin ○ Breathlessness ○ Frequent infections ○ Unusual and frequent bleeding ○ Easily bruised skin ○ Flat red or purple spots on the skin ○ Bone and joint pain ○ A feeling of fullness or discomfort in the tummy ○ Swollen glands in the neck Diagnostic Tests ● ● ● Minimum at primary care. Obtain a complete history and perform a complete physical examination on patients exhibiting signs and symptoms. Request the following tests in patients with suspected AML1 ○ Complete blood count (CBC) with platelet count ○ Peripheral Blood Smear (PBS) ○ Reticulocyte Count Gold Standard. To confirm AML, refer the patient to a higher level of care for multiparameter flow cytometry of the bone marrow core biopsy and aspirate smears among patients presenting with low RBC and WBC counts. (Strong Recommendation)1 Other tests. Refer the patient for the following additional tests: ○ Test for HBsAg, anti-HBc total, anti-HBs, anti-HCV, and/or HIV especially among high-risk populations (Good Practice Statement)1: ○ Immunohistochemistry (Strong Recommendation)1 ○ Cytogenetic study using conventional karyotyping for risk stratification of patients and to guide individualized therapy. (Strong Recommendation)1 ○ Baseline molecular analysis of c-KIT, FLT3-ITD, FLT3-TKD, NPM1, CEBPA, IDH1, IDH2, RUNX1, ASXL1, and TP53 for gene mutations may be recommended (Weak Recommendation)1. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 121 Diagnostic Tests ○ In cases with inadequate karyotype analysis, addition of fluorescence in situ hybridization (FISH) can be recommended. (Strong Recommendation)1 Treatment and Referral ● ● ● ● ● ● Refer to higher levels of care for the confirmation of the diagnosis and specialized treatment of patients with AML. For Supportive and Palliative Care: Advise referral of patients and their families to provision of health systems support interventions at any point in the course of illness to address (RA 11215)2 Financial support: Cancer patients, persons living with cancer and cancer survivors are considered persons with disabilities (PWDs) and are accorded the same rights, privileges, social welfare and benefits as other PWDs.2,3,4,5,6,7 Palliative care: Cancer patients and families of patients that need palliative support may consult with/ may be referred to accredited associations and institutions handling hospice and palliative care.8 Psychosocial needs: Cancer patients and families of patients that need psychosocial support may consult with/ may be referred to support groups, associations and institutions handling psychosocial care. 8,9,10 Pain and symptom management: Medical professionals caring for cancer patients may consult the WHO Analgesic Ladder and the DOH Cancer Pain Relief Program for guidance on pain management and referral11 ■ End-of-life care concerns: Cancer patients who are contributors and their families are eligible to apply for illness, disability, and funeral benefit claims from SSS and GSIS 2,6,7 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Department of Health. Acute Myeloid Leukemia National Clinical Practice Guidelines. National Integrated Cancer Control Program. 2022. https://drive.google.com/file/d/1PtOyZbMV1krEGQAcQvnli7Pp4LvYKa2u/view Republic Act No. 11215 "National Integrated Cancer Control Act" Republic Act No. 7277 “Magna Carta for Disabled Persons, and for Other Purposes” Department of Health and Department - Department of Budget and Management. DOH-DBM Joint Memorandum Circular 2022-0002: Implementing Guidelines for the Use of Cancer Assistance Fund (CAF). 2022. https://www.dbm.gov.ph/wp-content/uploads/Issuances/2022/Joint-Memorandum-Circular/DOH-DBM-Joint-Memorandum-CircularNo-2022-0002.pdf Department of Labor and Employment. DOLE Labor Advisory No. 20 series of 20223: Guidelines on the Implementation of the Workplace Policy and Program on Cancer Prevention and Control in the Private Sector. 2023. https://oshc.dole.gov.ph/wp-content/uploads/2023/10/LA-20-series-of-2023.pdf Social Security System. SSS Benefits Overview. N.d. https://www.sss.gov.ph/sss/appmanager/pages.jsp?page=ssbenefits Government Service Insurance System. GSIS Policy and Procedural Guidelines No. 274-14. 2016. https://www.gsis.gov.ph/downloads/ppg-br/20160304-PPG-274-14.pdf Philippine Cancer Society. Hospice Groups. N.d. https://www.philcancer.org.ph/index.php/support/hospice-groups Silakbo PH. Mental Health Resources. N.d. http://www.silakbo.ph/help/ MentalHealthPH. Directory. N.d. https://mentalhealthph.org/directory/ Department of Health. The Philippine Cancer Control Program. N.d. https://doh.gov.ph/sites/default/files/health_programs/The-Philippine-Cancer-Control-Program.pdf Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 122 Asthma is described in the Global Initiative for Asthma (GINA) 20231 as a heterogenous disease, usually characterized by chronic airway inflammation. It is common and affects 1-29% of the population in different countries. According to the World Health Organization, it is also in these countries that asthma is under-diagnosed and under-treated2. In the Global Asthma Report 20223, the Philippines ranked second in the age-standardized deaths per million population covering the years 2011-2015. The symptoms and airflow limitation from asthma is described as varying over time and intensity. Its features can resolve spontaneously, respond to medications or be absent for weeks or months. However, asthma exacerbations can also occur which can lead to death. In addition, the majority of deaths due to asthma happen in low- and middle-income countries1. Asthma poses a threat to the productivity of individuals and to the economics of families and the community, hence, it is important that asthma recognition and management is strengthened at the primary care level. Table 15. Asthma Continuum of Care Overview Asthma Overview Risk Factors Prevention Screening Diagnosis Pharmacologic Treatment Non-pharmacologic management ● Tobacco smoke exposure ● Occupational exposure to noxious aerosols ● Allergic rhinitis ● Obesity The development of asthma cannot be prevented but exacerbations can be prevented and symptoms can be controlled by the identification and avoidance of asthma “triggers” and respiratory irritants e.g. allergens, fumes, cigarette exposure (secondary and tertiary prevention) (See General Wellness and Preventive Measures for general guidance). Not applicable Minimum at primary care. Consider probable asthma by clinical history among patients with typical symptoms. Gold Standard. Confirm the diagnosis of asthma through spirometry pre-and post-bronchodilator. Additional laboratory tests depending on the clinical indication. PEF with reversibility test, bronchial provocation test, allergy tests, Chest X-ray, sputum eosinophil count, FeNO. Reliever. First-line reliever is inhaled corticosteroid (ICS)-formoterol. Second-line reliever is ICS-short acting beta-agonist (SABA). SABA alone treatment is not recommended. Maintenance. Stepwise approach depending on clinical presentation and asthma control is followed for maintenance therapy. ● Patient education, written asthma plan ● Smoking and vape use cessation ● Weight reduction among overweight and obese patients ● Mental health assessment for anxiety/panic attacks ● Food allergen avoidance ● Avoidance of occupational/domestic triggers ● Influenza vaccination every year ● Breathing exercises Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 123 Signs and Symptoms ● Consider asthma among adults presenting with the following1. ○ Wheezing, shortness of breath, chest tightness, and cough that vary over time, including in their frequency and intensity ○ Symptoms that are often worse at night or in the early morning ○ Symptoms that are triggered by viral infections (colds), exercise, allergen exposure, changes in weather, laughter, or irritants such as car exhaust fumes, strong smells, cigarette or vape smoke Screening ● Not applicable Diagnostic Tests ● ● ● Minimum at primary care. Consider the diagnosis of probable asthma by clinical history among patients presenting with typical symptoms that respond promptly and completely to therapy4. ○ Consider classifying asthma severity into mild, moderate, and severe based on difficulty to treat or the level of treatment required to control the patient’s symptoms and exacerbations after at least several months of treatment1 ○ Consider classifying asthma as well-controlled, partly controlled, or uncontrolled using the GINA symptom control tool1,5 Gold standard. Confirm the diagnosis of asthma among adults with clinical history of asthma symptoms through spirometry pre- and post-bronchodilator to demonstrate variable expiratory airflow limitation. 1,4 ○ Excessive variability in lung function: increase in FEV1 of >12% and >200 ml compared with pre-bronchodilator values, AND ○ Expiratory airflow limitation: FEV1/FVC reduced compared with lower limit of normal (usually >0.75-0.80 in adults) Other laboratory tests. Additional laboratory tests may be requested depending on the clinical indication and the availability of the test: ○ May use peak expiratory flow (PEF) with reversibility test to confirm variable expiratory flow in diagnosing asthma. Consider PEF also for short and long-term monitoring of asthma.1 ○ May use bronchial provocation test to assess airway hyperresponsiveness.1 ○ Consider performing allergy tests to determine presence of atopy which increases the probability that a patient with respiratory symptoms has allergic asthma.1 ○ Consider performing imaging studies such as Chest X-ray to investigate the possibility of comorbid conditions or alternative diagnoses in those with difficult-to-treat asthma.1 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 124 Diagnostic Tests ○ ○ Consider requesting for sputum eosinophil count among adult patients with moderate or severe asthma for adjusting ICS-containing maintenance. (Evidence A)1 Consider requesting for fractional concentration of exhaled nitric oxide (FeNO) among young adults with asthma for adjusting ICS-containing maintenance. (Evidence A)1 Treatment ● Pharmacologic Therapy. Follow a step-wise approach to pharmacologic therapy treatment to achieve control of asthma. Do not give short-acting beta-agonist (SABA)-only treatment in adults with asthma since those treated with SABA alone compared with inhaled corticosteroid (ICS) are at increased risk of asthma-related death (Evidence A) and urgent asthma-related healthcare (Evidence A).1 ○ Step 1. I If patient has infrequent symptoms, e.g. less than twice a month and no risk factors for exacerbations, including no exacerbations in the last 12 months: therapy. As-needed low-dose ICS--formoterol [e.g. ■ First-line budesonide-formoterol combination metered dose inhaler (MDI) 160mcg-4.5mcg/inhalation or dry powder inhaler (DPI) 200 mcg-6 mcg/inhalation, 1 inhalation]. (Evidence B)1 ■ Alternative therapy. Low dose ICS taken whenever SABA is taken, in combination or separate inhaler. (Evidence B)1 ○ Step 2. If patient has symptoms or need for reliever twice a month or more: ■ First-line therapy. As-needed low-dose ICS formoterol (Evidence A)1 ■ Alternative. May give any of the following1: ● Daily low-dose ICS plus as-needed SABA (Evidence A) ● As-needed low-dose ICS-SABA ● Daily leukotriene receptor antagonist (LTRA) plus as-needed SABA, although LTRA were found to be less effective than ICS, particularly for exacerbations1 ○ Step 3. If patient has troublesome symptoms on most days e.g. 4-5 days a week, or waking due to asthma once a week or more, especially if with risk factors for exacerbations (smoking, allergen exposure if sensitized, previous intubation or intensive care unit stay for asthma, low FEV1 esp. <60% predicted, obesity, food allergy, chronic rhinosinusitis, and poor adherence/inhaler technique): ■ First Line. Low-dose ICS-formoterol maintenance-and-reliever therapy (MART). (Evidence A)1 ■ Alternative. May give any of the following1: ● Daily low-dose ICS-long acting beta-agonist (LABA) plus as-needed SABA (Evidence A) or plus as-needed ICS-SABA (Evidence B) ● Daily medium-dose ICS plus as-needed SABA (Evidence A) or plus as-needed ICS-SABA. (Evidence B) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 125 Treatment Daily low dose ICS and LTRA daily plus as needed- SABA (Evidence A) Daily low dose ICS and low-dose, sustained release theophylline daily plus as needed SABA (Evidence B) Step 4. If patient initially presented with severely uncontrolled asthma, or with an acute exacerbation, daily symptoms, waking with asthma once a week or more, and low lung function: ■ First Line. May give medium-dose ICS-formoterol maintenance and reliever therapy (MART) and a short course of oral corticosteroids. (Evidence D)1 ■ Alternative. May give any of the following1: ● Daily medium-high-dose ICS-LABA plus as-needed SABA or plus as-needed ICS-SABA (Evidence D) ● High-dose ICS plus as-needed SABA (Evidence A) ● Add-on long-acting muscarinic antagonist (LAMA) to ICS-LABA or switch to ICS-LAMA-LABA (Evidence A) plus as-needed SABA ● Add-on LTRA to medium or high-dose ICS as controller (Evidence A) ● Add-on theophylline to medium or high-dose ICS as controller (Evidence B) ● ● ○ Consider stepping down gradually to find the patient’s lowest treatment when good asthma control is achieved and maintained for 2-3 months.1 ○ Consider stepping up when symptoms are confirmed to be due to asthma and not from common problems such as inhaler technique, adherence, allergen exposure, and multimorbidity1 Non-pharmacologic therapy. Consider providing or teaching the following non-pharmacologic interventions to improve asthma control: ○ Patient education to address the mentioned common problems.1 ○ Written asthma action plan for patient use, including short-term changes to their treatment in response to changes in their symptoms and/or PEF and when to access medical care. (Evidence A)1 ○ Smoking cessation, including cessation of vape use through providing access to counseling and smoking cessation programs. (Evidence A)1 ○ Strategies for weight reduction among overweight and obese patients with asthma. (Evidence B)1 ○ Mental health assessment for patients with symptoms of asthma and anxiety. May also provide advice about management of panic attacks. (Evidence D)1 ○ Food allergen avoidance to reduce risk of asthma exacerbation. (Evidence D)1 ○ Exposure avoidance among those with occupational/domestic asthma triggers. (Evidence A)1 ○ Utilization of non-polluting heating and cooking sources of pollutants to be vented outdoors where possible. (Evidence B)1 ○ Influenza vaccination every year. (Evidence C)1,6 ○ ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 126 Treatment ○ Breathing exercises to supplement pharmacotherapy for symptom relief and improvement of quality of life. (Evidence A)1 Referral ● Refer patients with any of the following to higher level facility or specialized care when patient has any of the following1: ○ Difficulty confirming the diagnosis of asthma ○ Persistent or severely uncontrolled asthma or frequent exacerbations, described as the following: ■ Symptoms remain uncontrolled or the patient has ongoing exacerbations or low lung function despite correct inhaler technique and good adherence with Step 4 treatment. ■ The patient frequently uses asthma-related health care (e.g. multiple emergency department visits or urgent primary care visits). ○ Severe or life-threatening exacerbations described as with symptoms of drowsiness, confusion, or silent chest ○ Low FEV1, especially if <60% predicted ○ Suspected occupational asthma ○ Any risk factors for asthma-related death (near-fatal asthma attack at any time in the past, suspected or confirmed anaphylaxis or food allergy) ○ Evidence of, or risk of, significant treatment side-effects ○ Symptoms suggesting complication (e.g. allergic bronchopulmonary aspergillosis) or subtypes of asthma (e.g. aspirin-exacerbated respiratory disease/aspirin-induced asthma, perimenstrual/catamenial asthma) First Aid Measures and Basic Emergency Care ● ● Assess patients for asthma exacerbations in patients presenting with progressive increase in symptoms of shortness of breath, cough, wheezing, or chest tightness and progressive decrease in lung function. Consider administering the following main initial therapies in patients suspected of having asthma exacerbation: repetitive administration of rapid-acting inhaled bronchodilators, early introduction of systemic corticosteroids, and controlled flow oxygen supplementation1. ○ Mild to moderate exacerbation: ■ Inhaled SABA 4-10 puffs by pMDI + spacer or nebulizer, repeat every 20 minutes for 1 hour. (Evidence A)1 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 127 First Aid Measures and Basic Emergency Care Consider immediate transfer to higher facility if with worsening of symptoms or no relief despite 3 doses of SABA. After the first hour, consider giving additional SABA (can range from 4-10 puffs every 3-4 hours up to 6-10 puffs every 1-2 hours), ipratropium bromide, oxygen therapy, and systemic corticosteroid while waiting transfer to a higher facility1 ■ May give oral corticosteroids such as prednisolone 40-50mg (maximum of 50mg/day) and continue for 5-7 days. (Evidence B) (GINA, 20231) ■ May give controlled oxygen therapy to maintain oxygen saturation of 93-95%1 ■ Assess response to treatment after 1 hour or earlier then assess for discharge. May discharge the patient if with the following1: ■ Symptoms improved, not needing SABA ■ PEF improving, and >60-80% of personal best or predicted ■ Oxygen saturation >94% room air ■ Resources at home adequate Severe or life-threatening exacerbation: Facilitate immediate transfer to a higher level facility. Give SABA, ipratropium bromide, oxygen therapy, and systemic corticosteroid while waiting transfer to a higher facility1 ■ ○ ○ References 1. 2. 3. 4. 5. 6. Global Initiative for Asthma. 2023 GINA Report. Published July 10, 2023. Accessed December 12, 2023. https://ginasthma.org/2023-gina-main-report/ World Health Organization. Asthma. 2023. https://www.who.int/news-room/fact-sheets/detail/asthma Global Asthma Network. The Global Asthma Report 2022. The International Journal of Tuberculosis and Lung Disease. 2022;26(1):1-104. doi:https://doi.org/10.5588/ijtld.22.1010 UpToDate. Asthma in adolescents and adults: Evaluation and diagnosis. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/asthma-in-adolescents-and-adults-evaluation-and-diagnosis?search=asthma&source=search_ result&selectedTitle=3~150&usage_type=default&display_rank=3# Global Initiative for Asthma. GINA Implementation Toolbox: GINA symptom control tool. Published 2018. Accessed December 12, 2023. https://ginasthma.org/wp-content/uploads/2019/01/GINA-Implementation-Toolbox-2019.pdf#page=20 Philippine Society for Microbiology and Infectious Diseases. Philippine Clinical Practice Guidelines for Adult Immunization. Makati: Zurbano Publishing and Printing Corp. Published 2018. Accessed December 14, 2023. https://drive.google.com/file/d/1pdl986x5sLNzSCBwRGC9HNBAvgGHl06N/view Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 128 Chronic Obstructive Pulmonary Disease is a disease characterized by chronic respiratory symptoms and airflow obstruction. Chronic respiratory diseases like Chronic Obstructive Pulmonary Disease (COPD) are among the top 10 causes of mortality and morbidity in the Philippines1. It also affects quality of life, due to exacerbations and hospitalizations. The most common and most important risk factor remains smoking, hence interventions for smoking cessation are critical in COPD management. The long-term goals of management include the improvement of health outcomes and quality of life, reduction of symptoms, exacerbations, hospitalizations, and mortality, and improvement of lung function2. Table 16. Chronic Obstructive Pulmonary Disease Continuum of Care Overview COPD Overview Risk Factors ● Cigarette smoking or vaping - most important ● Asthma and airway hyperresponsiveness ● Childhood pneumonia ● Respiratory infections - risk factor for COPD exacerbations ● Occupational exposures to dust and fumes (e.g. coal mining, gold mining, cotton textile dust) ● Biomass/biofuel combustion - particularly among women ● Genetic risk factors (e.g., α1 antitrypsin deficiency) Avoidance/cessation of smoking, avoidance of second-hand exposure - most important preventive measure for primary, secondary, and tertiary prevention Avoidance of environmental exposure to biomass smoke, pollution, etc. Adequate treatment of respiratory infections including pneumonia (particularly in infancy/childhood) and TB Prevention Screening Diagnosis Pharmacologic Treatment Non-pharmacologic management (See General Wellness and Preventive Measures for general guidance) In asymptomatic patients. Not recommended. In symptomatic patients. Use clinical scoring systems to assess the probability of COPD. Minimum at Primary Care. Clinical scoring system + handheld spirometer Classify confirmed COPD patients using the Modified Medical Research Council (mmRC) Dyspnea Scale Gold standard. Facility-based spirometer Stable COPD, not in exacerbation: ● FEV1≥80% or mmRC <2: LAMA Monotherapy ● FEV1<80% or mmRC ≥2: LABA + LAMA Combination; if unavailable, LAMA monotherapy ○ If with increased risk of exacerbation and without infection: add ICS COPD in exacerbation: SABA + SAMA; if unavailable, SABA monotherapy COPD + bacterial infection: Oral antibiotics ● COPD Action Plan ● Smoking or vaping Cessation ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 129 Signs and Symptoms ● Consider COPD in adults with a history of smoking and presenting with persistent and progressive respiratory symptoms such as difficulty of breathing, cough, and phlegm production2 Screening ● ● Screening for COPD is not recommended in asymptomatic adults3 Assess patients with symptoms of probable COPD using a clinical scoring system to identify patients for confirmatory testing (Strong Recommendation)2 Diagnostic Tests ● ● ● ● Minimum at Primary Care. ○ Confirm the diagnosis among probable COPD patients by using the combination of a clinical scoring system and handheld spirometry, as alternative to facility-based spirometry (Weak recommendation)2. Examples of a clinical scoring system are: ■ COPD Diagnostic Questionnaire (CDQ) ■ COPD Population Screener (COPD-PS) ■ Lung Function Questionnaire (LFQ) ■ COPD Assessment in Primary Care to Identify Undiagnosed Respiratory Disease and Exacerbation Risk (CAPTURE) Screening Tool ○ Do not use clinical scoring system, handheld spirometer, or peak flow meter alone to confirm the diagnosis (Strong recommendation against use)2 ○ COPD is confirmed if there is non-fully reversible airflow limitation: FEV1/FVC 0.7 post-bronchodilation. Gold Standard. If available and accessible, request for the gold standard - facility-based spirometry, to confirm the diagnosis2. Refer to a higher level facility for this test, if necessary. Initial assessment of confirmed COPD. Consider determining the following four fundamental aspects in COPD assessment among those confirmed with COPD by spirometry:4 ○ Severity of airflow limitation ○ Nature and magnitude of current symptoms ○ Previous history of moderate and severe exacerbations ○ Presence and type of other disease (multimorbidity) Classification of confirmed COPD. Classify the patient’s symptoms according to the Modified Medical Research Council (mmRC) Dyspnea Scale to identify the appropriate treatment. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 130 Diagnostic Tests Table 17. Modified Medical Research Council (mmRC) Dyspnea Scale2 mmRC Classification Symptoms mmRC 0 Dyspnea only with strenuous exercise mmRC 1 Dyspnea when hurrying or walking up a slight hill mmRC 2 Walks slower than people of the same age because of dyspnea or has to stop for breath when walking at own pace mmRC 3 Stops for breath after walking 100 yards (91 meters) or after a few minutes mmRC 4 Too dyspneic to leave house or breathless when dressing Treatment ● ● ● Start treatment in all adults who have COPD. Pharmacologic Management of Stable COPD. ○ First-line therapy. Choose the appropriate therapy according to the FEV1 and mmRC classification of the patient. ■ FEV1≥80% or mmRC <2 and not in exacerbation: ● LAMA monotherapy (Weak recommendation)2 ■ FEV1<80% or mmRC ≥2 and not in exacerbation: ● Long-acting B2-agonist (LABA)/Long-acting antimuscarinic antagonist (LAMA) combination therapy (Strong recommendation)2 ● If LABA/LAMA combination therapy is not available, use LAMA instead of LABA (Weak recommendation)2 ■ FEV1<80% or mmRC ≥2 with increased risk of exacerbation and absence of concurrent respiratory infection: ● Add an inhaled corticosteroid (ICS) on top of long-acting bronchodilator (LABD) (e.g. LABA/LAMA/ICS or LABA/ICS + LAMA/LABA) (Strong recommendation)2 ○ Second-line therapy. If inhaled long-acting bronchodilators (e.g. LAMA, LABA) are not available or accessible , offer oral methylxanthines However, long-acting bronchodilators remain preferred over oral methylxanthines. (Strong recommendation)2. ■ Methylxanthines include Theophylline and Doxofylline. Pharmacologic Management of COPD in Exacerbation. ○ First-line. Administer short-acting B2-agonist (SABA) + short-acting antimuscarinic antagonist (SAMA) combination. If SABA + SAMA is not available, administer SABA alone (Strong recommendation)2. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 131 Treatment Add-on therapy. If the patient in exacerbation has worsening symptoms and does not respond to bronchodilators (SABA + SAMA or SABA alone), give a short course of oral steroids (5-10 days) (Strong recommendation)2. ○ Refer patients with COPD in exacerbation to higher levels of care as necessary. Management of Bacterial Coinfection in Outpatients with COPD Exacerbation. ○ Initiate oral antibiotics in patients with COPD who present with at least 2 of the following symptoms: increased dyspnea, increased frequency of cough, increased sputum volume or purulence (Anthonsen’s criteria) (Strong recommendation)2. ■ Antibiotic options, to complete course in 5-10 days (2018 National Antibiotics Guideline): ● Amoxicillin 500 mg 3 times a day ● Doxycycline 100 mg tab 2 times a day ● Cefuroxime 500 mg tab 2 times a day Nonpharmacologic Management. ○ Smoking or vaping cessation in current smokers or vapers ○ Develop a COPD Action Plan (sample5) with the patient to be used for self-guided management (Strong recommendation)2. ○ ● ● Referral ● ● Refer patients with COPD who have any of the following conditions which are associated with higher risk of moderate to severe exacerbation to higher level of care (Strong recommendation)2: ○ Prior history of exacerbations ○ Presence of comorbidities ○ Severe or very severe airflow limitation Refer patients with COPD who have any of the following conditions which are associated with higher risk mortality to higher level of care (Strong recommendation)2: ○ Presence of uncontrolled diabetes or cardiovascular disease ○ Previous hospitalization for acute exacerbation within the past year ○ Hospital readmission within 30 days ○ Use of long-term oxygen therapy. Palliative Care ● Consider giving low flow oxygen therapy to relieve dyspnea in symptomatic COPD patients with moderate to severe breathlessness (mmRC 3-4) who are not hypoxemic and who do not fulfill the criteria for long-term oxygen therapy (LTOT), provided it is used with caution and the patient is closely supervised (Weak recommendation)2: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 132 Palliative Care ● ○ Prior history of exacerbations ○ Presence of comorbidities ○ Severe or very severe airflow limitation Consider giving opioids (e.g., Morphine) to relieve dyspnea despite maximized medical managements in patients with advanced-stage or end-stage COPD and/or refractory dyspnea (Strong recommendation)2: ○ Presence of uncontrolled diabetes or cardiovascular disease ○ Previous hospitalization for acute exacerbation within the past year ○ Hospital readmission within 30 days ○ Use of long-term oxygen therapy First-aid Measures and Basic Emergency Care ● ● Manage exacerbations as indicated in the Treatment Section Facilitate the immediate transfer of patients in severe respiratory distress to higher levels of care. ○ Ensure IV access prior to transfer. ○ Administer oxygen therapy. References 1. 2. 3. 4. 5. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet. 2020;396(10258):1204-1222. doi:https://10.1016/S0140-6736(20)30925-9 Lung Center of the Philippines & University of the Philippines Manila - National Institutes of Health - Institute of Clinical Epidemiology. Clinical Practice Guidelines for the Management of Chronic Obstructive Pulmonary Disease. Published 2023. Accessed December 16, 2023. https://drive.google.com/drive/u/1/folders/1kAx4VZrlqH3AQkQ-E35TSQLg7Z6wQud1 Webber EM, Lin JS, Thomas RG. Screening for Chronic Obstructive Pulmonary Disease. JAMA. 2022;327(18):1812. doi:https://doi.org/10.1001/jama.2022.4708 Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for Prevention, Diagnosis and Management of COPD: 2023 Report. Published 2023. Accessed December 16, 2023. https://goldcopd.org/2023-gold-report-2/ Living Well with COPD. Plan of Action. Published 2022. Accessed December 16, 2023. https://www.livingwellwithcopd.com/DATA/DOCUMENT/64_en~v~plan-of-action.pdf Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 133 Diabetes Mellitus is a disorder of glucose metabolism, leading to chronic elevation of blood sugar, which leads to various complications. Between 2009 and 2019, diabetes mellitus (DM) was the seventh leading cause of combined death and disability in our country1. DM is initially a silent disease, with people having asymptomatic subclinical disease for 5-7 years before its actual diagnosis2. This period between the asymptomatic phase of the disease and the development of its various clinical manifestations and complications (e.g. blindness from diabetic retinopathy, chronic kidney disease from diabetic nephropathy, ischemic heart disease and peripheral arterial disease from accelerated atherosclerosis) is a window of opportunity for aggressive screening, risk management, and blood sugar control in the primary care setting. The scope of this section is limited to Type 2 Diabetes Mellitus. Table 18. Type 2 Diabetes Mellitus Continuum of Care Overview Type 2 Diabetes Mellitus Overview Screening Overweight or obese Smoking Maternal history of diabetes or having Gestational Diabetes Mellitus (GDM) during pregnancy Family history of type 2 Diabetes in first- or second-degree relative Signs of insulin resistance or conditions associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovary syndrome, or small-for-gestational-age birth weight) Healthy diet, exercise and physical activity, weight management (See General Wellness and Preventive Measures for general guidance) FBS (strong recommendation) OR HbA1c (Weak)3 Diagnosis Minimum at Primary Care. Repeat FBS, HbA1c or 75-g OGTT to confirm. DM is confirmed if: Risk Factors 3 ,11 Prevention ● ● ● ● ● FBS ≥126 mg/dL (7.0 mmol/L) after at least 8 hours of no caloric intake or HbA1c ≥6.5% (48 mmol/mol) or 2–hour postprandial plasma glucose after ingestion of 75 gram anhydrous glucose load ≥ 200 mg/dL (11.1mmol/L) or ● RBS ≥ 200 mg/dL (11.1mmol/L) + classic symptoms of hyperglycemia (polydipsia, polyuria, weight loss) Additional tests for comorbidities/complications: ● Lipid profile (including LDL, HDL, triglycerides), liver function tests, spot urinary albumin-to-creatinine ratio, serum creatinine and estimated glomerular filtration rate (eGFR), serum potassium ● TB Screening by symptomatic screening or by chest X-ray ● Age and sex-appropriate cancer screening tests First-line: Metformin Alternatives as monotherapy or in combination depending on glycemic status and targets: Sulfonylureas, thiazolidinedione, DPP-4 inhibitor, SGLT2 inhibitor, GLP-1 receptor agonist, insulin For primary prevention of CVD: Moderate-intensity statin for all patients with diabetes, Aspirin for DM with high CVD risk ● Medical nutrition therapy, (MNT), weight loss/management, exercise, psychosocial care, smoking cessation/avoidance ● ● ● Pharmacologic Treatment Non-pharmacologic management Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 134 Signs and Symptoms ● ● ● At the early stages or subclinical phase of DM, individuals are often asymptomatic. Consider the presence of overt DM in patients presenting with classic symptoms of hyperglycemia (polyuria, polydipsia, and weight loss) or symptoms of hyperglycemic crisis (nausea, vomiting, abdominal pain, altered mental status or decreased sensorium)2, 4,5 Uncontrolled diabetes can lead to the following complications: ○ Diabetic retinopathy, presenting with visual symptoms of curtain falling, floaters, or decreased visual acuity that cannot be corrected with refraction6 ○ Diabetic neuropathy, presenting with numbness, loss of balance, and tingling and pain of the toes and feet usually worse at night, foot ulcers, and foot deformity7 ○ Diabetic nephropathy is asymptomatic at an early stage but microscopic albuminuria is a sign. It is the leading cause of chronic kidney disease, which manifests as poorly controlled blood pressure or resistant hypertension, fatigue, edema, and congestion. Screening ● ● Fasting blood sugar (FBS). Screen all apparently healthy adults who are 40 years old and above, or those younger if with risk factors, using FBS. (Strong recommendation)3. Risk factors that should prompt screening in younger patients include: ○ Overweight or obese ○ Maternal history of diabetes or having Gestational Diabetes Mellitus (GDM) during pregnancy ○ Family history of type 2 diabetes in first- or second-degree relative ○ Signs of insulin resistance or conditions associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovary syndrome, or small-for-gestational-age birth weight) Hemoglobin A1c (HbA1c). Consider using HbA1c as an alternative to FBS for screening. (Weak recommendation)3. Diagnostic Tests ● Minimum at Primary Care. ○ In asymptomatic adults with initial positive screening test, confirm the diagnosis of DM using any of the following tests: repeat FBS, repeat HbA1c, or 75-gram oral glucose tolerance test (75 g OGTT). The diagnosis is confirmed if any of the following diagnostic criteria are met2, 4,5: ■ FBS ≥126 mg/dL (7.0 mmol/L) after at least 8 hours of no caloric intake or ■ HbA1c ≥6.5% (48 mmol/mol) or Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 135 Diagnostic Tests 2–hour postprandial plasma glucose after ingestion of 75 gram anhydrous glucose load ≥ 200 mg/dL (11.1mmol/L) ○ In adults with classic symptoms of hyperglycemia or hyperglycemic crisis, confirm the diagnosis of DM using a random plasma glucose (RPG) determination. ■ RPG ≥200 mg/dL (11.1 mmol/L) confirms the diagnosis in symptomatic patients 2, 4,5 . ○ If HbA1c is requested to confirm the diagnosis of DM, ensure the accuracy of the test by having it performed in a laboratory that uses a method that is NGSP-certified and standardized according to the Diabetes Control and Complications Trial (DCCT) assay (Evidence B)4 or certified by the National Reference Laboratory (NRL). ○ Evaluate for diabetes complications and comorbid conditions by performing a comprehensive diabetes medical evaluation, including comprehensive history taking, physical examination (including visual acuity determination and foot examination), and laboratory evaluation (Evidence A)4. ○ Perform cardiovascular risk assessment to identify and appropriately manage risk factors. Additional tests at Primary Care. Request for the following laboratory tests to assess for comorbidities and complications: ○ Lipid profile (including LDL, HDL, triglycerides) ○ Liver function tests ○ Spot urinary albumin-to-creatinine ratio ○ Serum creatinine and estimated glomerular filtration rate (eGFR) ○ Serum potassium in patients who are being treated with ACE-inhibitors, ARBs, or Diuretics, especially in patients with Chronic Kidney Disease ○ Screening for liver fibrosis in diagnosed T2DM patients with elevated ALT or fatty liver on ultrasound (Evidence C)8 Other tests. Consider additional tests at higher level care facilities to assess for comorbidities and complications: ○ Refer to an ophthalmologist for a comprehensive eye examination and diabetic retinopathy screening. ○ Age- and sex-appropriate cancer screening tests ○ Consider periodic psychosocial screening and when there is a change in the disease, treatment, or life circumstances of the patient (Evidence C)8 ○ Consider screening for symptoms of sleep disorders and sleep disruptions in people with diabetes (Evidence B)8. ■ ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 136 Treatment ● ● ● Start treatment in all adults who are confirmed to have diabetes. Glycemic Targets. ○ HbA1c Targets. ■ Target HbA1c of <7% (53 mmol/mol) in nonpregnant adults who have no significant hypoglycemia (Evidence A)8 ■ Consider targeting HbA1c of <8% (64 mmol/mol) in adults who have limited life expectancy or when harms of treatment are greater than the benefits (e.g., if with hypoglycemic episodes with more stringent sugar control) (Evidence B)8. ○ HbA1c Monitoring. ■ Monitor A1c according to the achievement of glycemic targets: ● If glycemic targets are met, do HbA1c at least 2 times a year (Evidence E)8 ● If glycemic targets are not met or if the therapeutic regimen was recently changed, assess HbA1c quarterly (Evidence E)8. ○ Capillary plasma glucose monitoring may be used as an alternative to HbA1c monitoring. The following glycemic targets appear to correlate with a HbA1c of <7%8. ■ Preprandial capillary plasma glucose: 80–130 mg/dL (4.4–7.2 mmol/L) ■ Peak postprandial (taken 1-2 hours after the beginning of the meal) capillary plasma glucose: <180 mg/dL (10.0 mmol/L) Pharmacologic Therapy. ○ First line medications. Offer metformin, a biguanide, as the first-line oral medication for T2DM8. Discontinue or avoid metformin in patients with eGFR <30 mL/min/1.73 m2. ○ Alternatives. ■ Consider initiating a dual-combination therapy or more potent glucose-lowering drugs in patients who have A1C is ≥1.5-2% (>12.5 mmol/mol) above the glycemic target. Options include: ■ Sulfonylureas (e.g., glimepiride, glipizide, glyburide) ■ Thiazolidinedione (e.g. Pioglitazone) ■ Dipeptidyl peptidase 4 (DPP-4) inhibitors (e.g. Linagliptin, Saxagliptin, Sitagliptin) ■ Sodium–glucose cotransporter 2 (SGLT2) inhibitors (e.g. Canaglifozin, Empaglifozin, Dapaglifozin) ■ Glucagon-like peptide 1 receptor agonists (GLP-1 RAs) (injectables) (e.g. Exenatide, Semaglutide, Liraglutide) ■ Insulin ○ Additional considerations. ■ Offer SGLT-inhibitors or GLP-1 RAs to patients with T2DM and established atherosclerotic cardiovascular disease, high cardiovascular risk, heart failure, or established kidney disease, for their demonstrated cardiovascular and renal benefits on top of glucose-lowering effects (Evidence A)9. ■ Metformin should be continued upon initiation of insulin therapy (unless contraindicated or not tolerated) for ongoing glycemic and metabolic benefits (Evidence A)9. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 137 Treatment Combine insulin with GLP-1 RAs for greater efficacy, durability of treatment effect, and weight and hypoglycemia benefit (Evidence A)9. ■ Consider factors such as the presence or cardiovascular and renal comorbidities, efficacy of the medications, risk of hypoglycemia and other side effects, effect on weight, cost and access, and patient preferences, when choosing among the various pharmacologic therapies (Evidence E)9 ○ Cardiovascular Risk Management ■ Primary Prevention. Offer the following primary prevention measures to patients with diabetes to prevent the occurrence of atherosclerotic cardiovascular disease (e.g., acute coronary syndrome/heart attack, stroke, etc.) ● Give a moderate-intensity statin to all patients with diabetes aged 40–75 years without atherosclerotic cardiovascular disease for primary prevention (Evidence A)10 ● Consider initiating statin therapy in people with diabetes aged 20-39 years old, with additional atherosclerotic disease risk factors (Evidence C)10 ● Consider giving Aspirin (75-162 mg/day) in those with diabetes who have an increased cardiovascular risk based on CV risk assessment, after a comprehensive discussion with the patient about the CVD prevention benefit versus the comparable increased bleeding risk (Evidence A)10. ■ Secondary Prevention. Offer the following secondary prevention measures to all patients who have diabetes and a history of atherosclerotic cardiovascular disease. ● Give a high-intensity statin. (Evidence A)10 ● Monitor and target LDL goal of less than 55 mg/dL. (Evidence B) ● Give Aspirin (75-162 mg/day) (Evidence A)10. ○ Diabetic retinopathy is not a contraindication to Aspirin use for cardioprotection (Evidence A)8 ● If patient has a documented Aspirin Allergy, give Clopidogrel 75 mg/day (Evidence B)10 Nonpharmacologic Therapy ○ Medical nutrition therapy (MNT). Offer medical nutrition therapy among individuals with diabetes to improve health, achieve and maintain body weight goals, attain glycemic, blood pressure and lipid goals, and delay or prevent diabetes complications or refer to a qualified dietician nutritionist. ○ Exercise. Teach individuals with diabetes to engage in at least 150 minutes or more of moderate-vigorous intensity aerobic activity per week, over at least 3 days/week and with no more than 2 consecutive days without activity (Evidence B)8. ■ Instruct patients to decrease sedentary behavior (Evidence B)8, interrupt prolonged sitting every 30 minutes (Evidence C)8, and increase non sedentary ■ ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 138 Treatment ○ ○ ○ activities above baseline (e.g. walking, housework, gardening, swimming, dancing, yoga) (Evidence B)8. Weight loss. Advise patients with type 2 DM who are overweight or obese to target weight loss of at least 5% using nutrition, physical activity, and behavioral therapy (Evidence B)8 Psychosocial Care. Provide psychosocial care using a collaborative, person-centered, culturally-informed approach (Evidence A)8 or refer to a qualified mental health HCP for targeted mental health interventions as indicated (Evidence B)8 Smoking and e-cigarette use/vape avoidance or cessation. (Evidence A)8, 11 Monitoring and follow-up ● Consider scheduling follow-up at least every 3-6 months to monitor the effects of the therapeutic regimen and medication-taking behavior (Evidence E)9. ○ Also review for occurrence and risk for hypoglycemia during each follow-up or clinical encounter. Referral ● ● To specialists or higher levels of care. Refer the following patients to specialists or higher levels of care: ○ Refer newly-diagnosed patients with DM to an ophthalmologist for an initial dilated and comprehensive eye examination (Evidence B)8. Subsequent follow-up schedule with eye specialists depends on the presence and severity of diabetic retinopathy. ○ Refer patients with DM for individualized MNT provided by a registered dietitian nutritionist who is knowledgeable and skilled in providing diabetes-specific MNT.8 ○ Patients with a history of prior lower-extremity complications, loss of protective sensation, structural abnormalities (e.g . foot ulcers, Charcot foot), or peripheral arterial disease (PAD) to foot care/vascular specialists (Evidence B)8 ○ Patients needing more specialized assessment or treatment for symptoms of distress, depression, suicidality, anxiety, treatment-related fear of hypoglycemia, disordered eating and/or cognitive issues (Evidence B)8 ○ Patients with sleep disturbance or suspected sleep disorders (Evidence B)8 ○ Patients with uncontrolled neuropathic pain despite initial pharmacologic treatment Immediate transfer to a higher level of care. Refer and immediately facilitate the transfer of patients presenting with symptoms of hyperglycemic crisis or severe hypoglycemia to a hospital. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 139 First Aid Measures and Basic Emergency Care ● ● Hypoglycemia. Recognize and immediately treat a patient presenting with signs and symptoms of hypoglycemia (blood glucose <70 mg/dL). ○ Immediately check blood glucose in a diabetic patient presenting with symptoms of hypoglycemia such as shakiness, irritability, confusion, hunger, and tachycardia. Severe hypoglycemia can present as loss of consciousness, seizure or coma. ○ Immediately administer Glucose 15-20 mg orally if able to ingest food or drinks (e.g. glucose tablets, soda, table sugar, candies) (Evidence B)8 ○ Immediately check blood glucose in a diabetic patient presenting with symptoms of hypoglycemia such as shakiness, irritability, confusion, hunger, and tachycardia. Severe hypoglycemia can present as loss of consciousness, seizure or coma. ○ Immediately administer Glucose 15-20 mg orally if able to ingest food or drinks (e.g. glucose tablets, soda, table sugar, candies) (Evidence B)8 Hyperglycemic crisis. Secure IV access, delivery of basic emergency care, and facilitate immediate transfer of patients presenting with symptoms of hyperglycemic crisis (e.g., air hunger, nausea, vomiting, abdominal pain, altered sensorium, polyuria, polydipsia, weakness). References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet. 2020;396(10258):1204-1222. doi:https://doi.org/10.1016/S0140-6736(20)30925-9 World Health Organization. HEARTS D: diagnosis and management of type 2 diabetes. Published 2020. Accessed December 16, 2023. https://www.who.int/publications/i/item/who-ucn-ncd-20.1 University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX) Phase 3: Task Force on Renal, Metabolic, Nutrition, and Endocrine Disorders. Published 2023. Accessed December 16, 2023. https://drive.google.com/file/d/1jViG7Whi45tBVHADBKraV06mUnpKvnNS/view American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2021. Diabetes Care. 2021;44(Supplement 1):S15-S33. doi:https://doi.org/10.2337/dc21-s002 International Diabetes Federation. Type 2 diabetes. No date. Accessed December 16, 2023. https://idf.org/about-diabetes/type-2-diabetes/ UpToDate. Diabetic retinopathy: Classification and clinical features. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/diabetic-retinopathy-classification-and-clinical-features?search=diabetic%20retinopathy&sou rce=search_result&selectedTitle=2~150&usage_type=default&display_rank=2# UpToDate. Screening for diabetic polyneuropathy. 2023. https://www.uptodate.com/contents/screening-for-diabetic-polyneuropathy?search=diabetic%20neuropathy%20symptoms&sectio nRank=1&usage_type=default&anchor=H2&source=machineLearning&selectedTitle=1~150&display_rank=1# American Diabetes Association. Standards of Care in Diabetes—2023 Abridged for Primary Care Providers. Clinical Diabetes. 2022;41(1). doi:https://doi.org/10.2337/cd23-as01 ElSayed NA, Aleppo G, Aroda VR, et al. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement_1):S140-S157. doi:https://doi.org/10.2337/dc23-s009 ElSayed NA, Aleppo G, Aroda VR, et al. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement_1):S158-S190. doi:https://doi.org/10.2337/dc23-s01 UpToDate. Type 2 diabetes mellitus: Prevalence and risk factors. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/type-2-diabetes-mellitus-prevalence-and-risk-factors?search=diabetes%20mellitus%20type% 202&source=search_result&selectedTitle=13~150&usage_type=default&display_rank=12#H10 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 140 Dyslipidemia is a known risk factor for cardiovascular disease. It can also co-exist with other risk factors for CVD, including diabetes mellitus, overweight/obesity, metabolic syndrome, and hypertension 1, 2, 3. Dyslipidemia ranks second among the top risk factors among Filipinos for cardiovascular related diseases [1,194 disability-adjusted life years (DALYs) per 100,000]4. The primary and secondary prevention of CVD involves adequate recognition of risk factors, diagnosis of dyslipidemia, and management of cholesterol levels through a combination of pharmacologic and nonpharmacologic measures. Table 19. Dyslipidemia Continuum of Care Overview Dyslipidemia Overview Risk Factors Overweight or obesity Diabetes mellitus Metabolic syndrome Alcoholism Hypothyroidism Kidney disease (e.g. nephrotic syndrome) Liver Disease Prevention Healthy diet, exercise and physical activity, weight management (See General Wellness and Preventive Measures for general guidance) Screening Fasting lipid profile in adults 40 years and above with at least one cardiovascular risk factor Diagnosis Dyslipidemia is present if lipid profile shows: ● LDL-C ≥ 130 mg/dl; ● HDL-C <40 mg/dL in males and <50 mg/dL in females; ● TG ≥ 150 mg/dL Source:NCEP, 20015 Pharmacologic Treatment First-line therapy. Statins Second-line therapies. Fibrates, ezetimibe, pure eicosapentaenoic acid (EPA) Treatment intensity should be adjusted according to LDL-C goals. See Statin Initiation and Titration Guide . Non-pharmacologic management Low fat, low cholesterol diet, rich in fruits and vegetables Adequate exercise Weight management Smoking/vaping avoidance/cessation Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 141 Signs and Symptoms ● Consider dyslipidemia among adult patients with the following: alcoholism, ○ Overweight or obesity, diabetes mellitus, metabolic syndrome, 1,6 hypothyroidism, kidney disease such as nephrotic syndrome, or liver disease. ○ Presence of arcus cornealis (before 45 years of age), tendon xanthoma and xanthelasma. (Recommended1); (Strong recommendation2) Screening ● Screen for dyslipidemia in asymptomatic adults 40 years and above with at least one cardiovascular risk factor (e.g., Diabetes mellitus, hypertension, history of smoking) using a lipid profile test (Conditional recommendation3). Diagnostic Tests ● ● Minimum at primary care. ○ Confirm the diagnosis of dyslipidemia if the lipid profile tests shows any of the following NCEP 5: ■ LDL-C ≥ 130 mg/dl; ■ HDL-C <40 mg/dL in males and <50 mg/dL in females; ■ TG ≥ 150 mg/dL ○ Perform thorough history and physical examination in all individuals diagnosed with dyslipidemia to assess primary and/or secondary causes of dyslipidemia. Primary causes include Familial Hypercholesterolemia (FH) while secondary causes include diabetes mellitus, hypothyroidism, Cushing syndrome, alcoholism, etc. Request for additional tests if clinically indicated. Additional tests. ○ Consider requesting for liver transaminases in patients at risk of liver injury prior to initiating statin therapy and 1 to 3 months after (MOH).6 ○ Consider requesting for creatine kinase if myositis is suspected after initiating statin therapy (MOH).6 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 142 Treatment ● ● ● First line pharmacologic therapy. Initiate statin therapy (see Statin Initiation and Titration Guide2) among adults with dyslipidemia as follows: ○ Elevated LDL with risk factors but without atherosclerotic cardiovascular disease. Prescribe low to medium intensity statin among adults without diabetes mellitus age ≥ 45 years with LDL-C ≥ 130 mg/dL and ≥ 2 risk factors (male sex, postmenopausal women, smoker, hypertension, BMI > 25 kg/m2, with family history of premature cardiovascular disease, proteinuria, and left ventricular hypertrophy) without atherosclerotic cardiovascular disease (ASCVD) to reach LDL-C goal of <130 mg/dL. (Recommended)1 ○ Diabetes mellitus. Prescribe moderate to high intensity statin among adults with diabetes mellitus and optimize therapy to reach the following LDL-C goals: (Recommended) 1 ■ <100 mg/dL among most adults with diabetes and without evidence of ASCVD ■ <70 mg/dL among adults with diabetes and with >1 risk factor or target organ damage ■ <55 mg/dL among adults with diabetes and at high risk of recurrent cardiovascular events ○ Suspected or confirmed familial hypercholesterolemia (FH). Give statin therapy to all adults suspected or confirmed to have familial hypercholesterolemia (FH) to reach the following LDL-C goals: (Strongly Recommended)1 ■ FH without ASCVD: <70 mg/dL ■ FH with ASCVD and risk factors: LDL <55 mg/dL ○ Chronic Kidney Disease. Give statin therapy to adults with Chronic Kidney Disease not on dialysis. (Recommended)1 ○ Acute coronary syndrome. Immediately initiate early high intensity statin therapy and continue among adults with acute coronary syndrome to reach the goal of LDL-C <55 mg/dL. (Recommended)1 Other therapies. The following patient groups may benefit from additional therapies: ○ Hypertriglyceridemia. Consider prescribing fibrates to adults with persistently high triglycerides (>200 mg/dL) with low HDL-C (<35 mg/dL) and to men with controlled diabetes1 ○ Persistently high triglycerides but at goal LDL-C. May consider prescribing omega fatty acids (pure eicosapentaenoic acid [EPA]) to adults with ASCVD on statin therapy at goal LDL-C, but with persistently high triglyceride levels of 135-499 mg/dL1 ○ Persistently elevated LDL-C despite maximally-tolerated statin therapy. Prescribe ezetimibe in addition to maximally tolerated statin therapy to adults with ASCVD and have not reached LDL-C goal as secondary prevention of cardiovascular disease. (Recommended)1 Non-pharmacologic therapies. Advice adults at any level of cardiovascular risk on the following: ○ Low fat, low cholesterol diet, rich in fruits and vegetables. (Recommended)1, Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 143 Treatment ○ ○ Cigarette smoking and vaping cessation (Cigarette Smoking Cessation: Strongly Recommended, Vaping Cessation: Recommended)1, Advice adequate exercise of approximately 150 minutes of moderate- to high-intensity exercise per week to adults capable of exercise after assessing functional capacity. (Recommended)1, Referral ● ● Refer to a specialist/higher level of care if lipid goals are not met despite uptitration of statin to maximally tolerated dose and good patient adherence to therapy, or if the patient has other comorbidities needing specialty care (e.g., atherosclerotic cardiovascular disease). Consider referring adults who are incapable of safely performing moderate to high intensity exercise to the next level of care.1, References 1. 2. 3. 4. 5. 6. Philippine Lipid and Atherosclerosis Society. Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. Published 2020. Accessed December 13, 2023. https://drive.google.com/file/d/1-_k8Uk9Lct56jT5T8xUcFQZoBAv_z8VL/view University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Cardiovascular Disease. Published 2021. Accessed December 13, 2023. . https://drive.google.com/file/d/1LyjMZhD0hAh2DJI6ta-IUPEDZacI8yow/view University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Phase 1. Published 2021. Accessed December 13, 2023. https://drive.google.com/drive/u/1/folders/1UXFurxj0dLH1J-Ua1KmrYaTuky7pON8Z GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet. 2020;396(10258):1204-1222. doi:https://doi.org/10.1016/S0140-6736(20)30925-9 Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA: The Journal of the American Medical Association. 2001;285(19):2486-2497. doi:https://doi.org/10.1001/jama.285.19.2486 Ministry of Health - Malaysia. 5th Edition of Clinical Practice Guidelines: Management of Dyslipidaemia. Putrajaya, Malaysia. Published 2017. Accessed December 13, 2023. https://www.moh.gov.my/moh/resources/Penerbitan/CPG/CARDIOVASCULAR/4.pdf Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 144 Generalized Anxiety Disorder is characterized by persistent and excessive worry about a number of different things that are difficult to control. It occurs more days than not for at least 6 months. It can cause significant impairments in daily functioning, and diminished quality of life.1 It is considered as one of the world’s most common mental health disorders, affecting 301 million people in 2019, which is mostly women rather than men. In 2019, Anxiety Disorder contributed to 1.45% of DALYs among Filipinos.2 With the increase in the global anxiety prevalence, this represents a significant threat to the population's well-being and quality of life. Symptoms often have early onset during childhood or adolescence. But with early detection, there are available highly effective treatments.3 Table 20. Generalized Anxiety Disorder Continuum of Care Overview Generalized Anxiety Disorder Overview Risk Factors Screening Diagnosis Pharmacologic Treatment Non-pharmacologic management Age Gender Socioeconomic Status Substance Abuse Genetic factor Environmental Change Standardized instrument: GAD-7, GAD-2, or Hospital Anxiety and Depression Scale-Anxiety (HADS-A) once a year Diagnose according to the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) Criteria First-line: 1. Cognitive behavior therapy (CBT) 2. Selective serotonin reuptake inhibitor or selective norepinephrine reuptake inhibitor Lifestyle modification such as healthy eating habits, having good sleep, regular exercise and reduced intake of caffeine, tobacco, nicotine, and alcohol Community-based drug rehabilitation programs (e.g. Katatagan, Kalusugan, at Damayan ng Komunidad) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 145 Signs and Symptoms ● Consider the presence of an anxiety disorder among adult patients with the following4,5: ○ Excessive anxiety, fear or worry about events or activities that are out of proportion to the situation or difficult to control occurring more days than not in the past six months and causes impairment of functioning. ○ Symptoms are often associated with three or more physical symptoms such as restlessness or feeling keyed up or on edge, easily fatigued, difficulty concentrating or mind going blank, irritability, muscle tension, or sleep disturbance. Screening ● ● Screen adults for Generalized Anxiety Disorder using standardized instruments such as GAD-7, GAD-2, or Hospital Anxiety and Depression Scale-Anxiety (HADS-A) once a year (Strong recommendation)6. This screening may be incorporated in annual health visits. Screen for anxiety among pregnant adults and during postpartum period. (Recommended)7 Diagnostic Tests ● Minimum at primary care. Diagnose general anxiety disorder among adults using the following criteria from the Diagnostic and Statistical Manual of Mental Disorders 5th Edition 4,5: A. Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least six months, about a number of events or activities (such as work or school performance). B. The individual finds it difficult to control the worry. C. The anxiety and worry are associated with three (or more) of the following six symptoms (with at least some symptoms having been present for more days than not for the past six months): 1. Restlessness or feeling keyed up or on edge 2. Being easily fatigued 3. Difficulty concentrating or mind going blank 4. Irritability 5. Muscle tension 6. Sleep disturbance (difficulty falling or staying asleep, or restless, unsatisfying sleep) D. The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. E. The disturbance is not attributable to the physiological effects of a substance (eg, a drug of abuse, a medication) or another medical condition (eg, hyperthyroidism). F. The disturbance is not better explained by another mental disorder (eg, anxiety or worry about having panic attacks in panic disorder, negative evaluation in social anxiety disorder [social phobia], contamination or other obsessions in OCD, separation from attachment figures in separation anxiety disorder, reminders of traumatic events in posttraumatic stress disorder, Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 146 Diagnostic Tests ● ● gaining weight in anorexia nervosa, physical complaints in somatic symptom disorder, perceived appearance flaws in body dysmorphic disorder, having a serious illness in illness anxiety disorder, or the content of delusional beliefs in schizophrenia or delusional disorder). Because the majority of the anxiety symptoms are not specific to GAD, it is important to exclude the other anxiety disorders before making the diagnosis. Consider assessing adults with anxiety disorders for self-harming behaviors and suicidal ideations.8 Additional laboratory tests at primary care. ○ Consider requesting laboratory tests as warranted, such as thyroid function tests, complete blood count, 12 lead electrocardiogram, to rule out other medical conditions.4,5 Treatment ● ● ● First-line Management. Offer the following first-line interventions for 4-6 weeks after shared decision-making with the patient and his/her family4, 5;8,9: ○ Monotherapy using either: ■ Cognitive behavior therapy (CBT); ■ Pharmacotherapy with selective serotonin reuptake inhibitor (such as Citalopram 10mg tablet, Escitalopram 5 to 10mg tablet, Sertraline 25 to 50mg tablet, Paroxetine 10 to 20 mg tablet, Fluoxetine 10 to 20 mg capsule, or Fluvoxamine 50 mg tablet) or selective norepinephrine reuptake inhibitor (such as Venlafaxine 75 mg capsule, or Duloxetine 30 mg capsule) starting at low dose; ○ Combination therapy using CBT and pharmacotherapy ○ Consider CBT for pregnant and nursing adult women with anxiety (Consensus-based Recommendation)8 Alternative Pharmacotherapy. ○ Consider the following medications as alternative to first line medications: Mirtazapine 15 mg tablet or Quetiapine 25 to 50 mg tablet.5 ○ Consider the following medications as augmentation of treatment: Buspirone 10 mg tablet, Gabapentin 300 mg tablet, Pregabalin 50 mg tablet in divided doses, or Hydroxyzine 50 mg tablet.5 Other Non-pharmacologic Therapy. Consider offering the following advice to improve symptoms: ○ Lifestyle modification such as healthy eating habits, having good sleep, regular exercise and reduced intake of caffeine, tobacco, and alcohol (Consensus-based recommendation) 8 ○ ○ Yoga, tai chi, meditation, spiritual activities, music therapy, aromatherapy, acupuncture or massage as additional management to adults with anxiety.4,10 Cessation of cigarette smoking and vaping (Cigarette Smoking Cessation: Strongly Recommended, Vaping Cessation: Recommended)1. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 147 Treatment ○ Development of a safety plan among adults with anxiety who have self-harmed or at risk of suicide.12 Referral ● Refer the following adults to mental health specialists or higher level of care4,8,13: ○ With significant physical or mental health comorbidities such as personality disorder, substance use or misuse disorder ○ With learning disability or cognitive impairment ○ With marked functional impairment or self-neglect ○ With history of self-harm or with suicidal or self-harm intentions ○ With poor response to treatment. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Anxiety & Depression Association of America. Generalized Anxiety Disorder (GAD) . Adaa.org. Published 2019. Accessed December 16, 2023. https://adaa.org/understanding-anxiety/generalized-anxiety-disorder-gad GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet. 2020;396(10258):1204-1222. doi:https://doi.org/10.1016/S0140-6736(20)30925-9 World Health Organization. Anxiety disorders. www.who.int. Published September 27, 2023. Accessed December 16, 2023. https://www.who.int/news-room/fact-sheets/detail/anxiety-disorders DeGeorge KC, Grover M, Streeter GS. Generalized Anxiety Disorder and Panic Disorder in Adults. American Family Physician. 2022;106(2):157-164. Accessed December 16, 2023. https://www.aafp.org/pubs/afp/issues/2022/0800/generalized-anxiety-disorder-panic-disorder.html UpToDate. Generalized anxiety disorder in adults: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/generalized-anxiety-disorder-in-adults-epidemiology-pathogenesis-clinical-manifestations-cou rse-assessment-and-diagnosis?search=generalized%20anxiety%20disorder&source=search_result&selectedTitle=1~150&usage_type =default&display_rank=1# University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Mental Health and Addiction. Published 2021. Accessed December 16, 2023. . https://drive.google.com/file/d/1Nq-QO0UYMh0MiLWeKmO8CSdcuZyFdlbg/view U.S. Preventive Services Task Force. Recommendation: Anxiety Disorders in Adults: Screening | United States Preventive Services Taskforce. www.uspreventiveservicestaskforce.org. Published June 20, 2023. Accessed December 16, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/anxiety-adults-screening#bootstrap-panel--12 Andrews G, Bell C, Boyce P, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Australian & New Zealand Journal of Psychiatry. 2018;52(12):1109-1172. doi:https://doi.org/10.1177/0004867418799453 Mazza, D., Brijnath, B., Chakraborty, S.P. and the Guideline Development Group. Clinical guideline for the diagnosis and management of work-related mental health conditions in general practice. Melbourne: Monash University; 2019. https://www.racgp.org.au/FSDEDEV/media/documents/Clinical%20Resources/Guidelines/Mental%20health/Work-related-mental-he alth-conditions-in-general-practice.pdf UpToDate. Complementary and alternative treatments for anxiety symptoms and disorders: Physical, cognitive, and spiritual interventions. 2023. https://www.uptodate.com/contents/complementary-and-alternative-treatments-for-anxiety-symptoms-and-disorders-physical-cog nitive-and-spiritual-interventions?search=generalized%20anxiety%20disorder&topicRef=101879&source=see_link#H5472412 Philippine Lipid and Atherosclerosis Society. Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. Published 2020. Accessed December 13, 2023. https://drive.google.com/file/d/1-_k8Uk9Lct56jT5T8xUcFQZoBAv_z8VL/v U.K. National Institute for Health and Care Excellence. Overview | Self-harm: Assessment, management and preventing recurrence | Guidance | NICE. www.nice.org.uk. Published September 7, 2022. Accessed December 16, 2023. https://www.nice.org.uk/guidance/NG225 U.K. National Institute for Health and Care Excellence. Recommendations | Generalised anxiety disorder and panic disorder in adults: management | Guidance | NICE. www.nice.org.uk. Published June 15, 2020. Accessed December 16, 2023. https://www.nice.org.uk/guidance/cg113/chapter/Recommendations Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 148 Hepatocellular Carcinoma is a primary tumor of the liver and constitutes more than 90% of the primary tumors of the liver. It occurs in approximately 85% of patients diagnosed with cirrhosis. HCC is now the fifth most common cause of cancer worldwide1 and is the fourth leading cause of cancer-related deaths in the world, according to the World Health Organization GLOBOCAN database2. According to recent data from the Philippine Statistics Authority, liver diseases accounted for 27.3 cases per 1000 deaths in the country in 2020. Liver cancer is the fourth most common cancer type after breast, lung and colon cancer and the second most common cause of cancer deaths. The calculated incidence rate for liver cancer in the country is 11.4 and the mortality rate of 10.8 per 100,000. The most common cause of HCC in the country is still chronic hepatitis B infection.3 The prognosis of patients with HCCA remains poor, with a five-year survival rate of 18 percent. Because it is frequently diagnosed late due to the absence of symptoms in patients with early disease, and the lack of surveillance for high-risk patients, screening is essential. The goal is to detect the tumors early when they are ≤2 cm in size to improve survival since the five-year survival rate of patients whose tumors are detected at an early stage and who receive proper treatment exceeds 70 percent.2,4 Table 21. Hepatocellular Carcinoma Continuum of Care Overview Hepatocellular Carcinoma Overview Risk Factors Prevention Screening Diagnosis Treatment and Referral Gender Race/ Ethnicity Chronic infection with HBV, or HCV Liver Cirrhosis Non alcoholic fatty liver disease Excessive alcohol consumption Smoking Inherited Metabolic Diseases Screening and treatment of hepatitis B/C infection Avoidance of excessive alcohol consumption Liver Ultrasound with alpha fetoprotein every 6 months among adults at risk Multiphasic, contrast- enhanced CT Scan of the Liver Refer adults with hepatocellular carcinoma to the higher level of care for appropriate management Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 149 Signs and Symptoms ● Signs and Symptoms. Suspect hepatocellular carcinoma (HCCA) among adults with liver cirrhosis with or without signs and symptoms of liver decompensation such as variceal bleeding or ascites, adults with palpable mass in the upper abdomen, weight loss, or early satiety.4 Screening ● Screen the following adults at risk of HCCA using liver ultrasound with alpha-fetoprotein every 6 months. (Strong recommendation5): ○ hepatitis B and/or C infection ○ family history of hepatocellular carcinoma ○ metabolic diseases ○ non-alcohol/ alcohol liver disease ○ prolonged heavy alcohol consumption ○ Smokers x ○ males aged 40 years and above Diagnostic Tests ● ● Minimum at Primary Care. Refer to higher level of care or a capable facility for confirmation of diagnosis using multiphasic, contrast-enhanced CT scan to diagnose hepatocellular carcinoma among adults. (Strong recommendation)6 Other Laboratory Tests. ○ Consider requesting for bilirubin, liver aminotransferases, alkaline phosphatase, complete blood count with platelet count, prothrombin time, albumin, hepatitis B and C serology, blood urea nitrogen and creatinine.4 ○ Refer to higher levels of care for further diagnostic work-up, including: ■ Contrast-enhanced MRI, should be available, to diagnose hepatocellular carcinoma among adults. (Strong Recommendation)6 ■ Core needle biopsy to adults who do not fulfill the imaging criteria such as small size of the lesion or cirrhotic liver. (Strong Recommendation)6 ■ Fine needle aspiration biopsy to adults wherein core needle biopsy cannot be done and adults who do not fulfill the imaging criteria such as small size of the lesion or cirrhotic liver. (Conditional Recommendation6) Treatment and Referral ● Refer adults with hepatocellular carcinoma to the higher level of care for appropriate treatment7 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 150 Treatment and Referral ● ● ● ● ● For Supportive and Palliative Care: Advise referral of patients and their families to provision of health systems support interventions at any point in the course of illness to address8 Financial support: Cancer patients, persons living with cancer and cancer survivors are considered persons with disabilities (PWDs) and are accorded the same rights, privileges, social welfare and benefits as other PWDs.8,9,10,11,12,13 Palliative care: Cancer patients and families of patients that need palliative support may consult with/ may be referred to accredited associations and institutions handling hospice and palliative care14 Psychosocial needs: Cancer patients and families of patients that need psychosocial support may consult with/ may be referred to support groups, associations and institutions handling psychosocial care.14,15,16 Pain and symptom management: Medical professionals caring for cancer patients may consult the WHO Analgesic Ladder and the DOH Cancer Pain Relief Program for guidance on pain management and referral.17 ○ End-of-life care concerns: Cancer patients who are contributors and their families are eligible to apply for illness, disability, and funeral benefit claims from SSS and GSIS8,12,13 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Asafo-Agyei KO, Samant H. Hepatocellular Carcinoma. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559177/ World Health Organization. Global Cancer Observatory. Iarc.fr. Published 2020. Accessed December 17, 2023. https://gco.iarc.fr/ Ornos ED, Murillo KJ, Ong JP. Liver diseases: Perspective from the Philippines. Ann Hepatol. 2023;28(3):101085. doi:https://doi.org/10.1016/j.aohep.2023.101085 UpToDate. Clinical features and diagnosis of hepatocellular carcinoma. Published 2023. Accessed December 17, 2023. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of-hepatocellular-carcinoma University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Neoplastic Diseases. Published 2021. https://drive.google.com/file/d/1oMATzGvpulZZrarfVktgVJzNt_7eavH4/view UpToDate. Epidemiology and risk factors for hepatocellular carcinoma. Published 2023. Accessed December 17, 2023. https://www.uptodate.com/contents/epidemiology-and-risk-factors-for-hepatocellular-carcinoma?search=hepatocellular%20carcin oma&source=search_result&selectedTitle=6~150&usage_type=default&display_rank=6#H2020279294 Department of Health. Philippine Clinical Practice Guideline for the Diagnosis and Management of Hepatocellular Carcinoma. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1jsxkDiqNgDw4353N2Ivl81waBHmmCsaY/view UpToDate. Overview of treatment approaches for hepatocellular carcinoma. Published 2023. Accessed December 17, 2023. https://www.uptodate.com/contents/overview-of-treatment-approaches-for-hepatocellular-carcinoma?search=hepatocellular%20ca rcinoma&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1# Republic Act No. 11215 "National Integrated Cancer Control Act" Republic Act No. 7277 “Magna Carta for Disabled Persons, and for Other Purposes” Department of Health & Department of Budget and Management. DOH-DBM Joint Memorandum Circular 2022-002: Implementing Guidelines for the Use of Cancer Assistance Fund (CAF). Published 2022. Accessed December 17, 2023. https://www.dbm.gov.ph/wp-content/uploads/Issuances/2022/Joint-Memorandum-Circular/DOH-DBM-Joint-Memorandum-CircularNo-2022-0002.pdf Department of Labor and Employment. DOLE Labor Advisory No. 20: Guidelines on the Implementation of the Workplace Policy and Program on Cancer Prevention and Control in the Private Sector. Published 2023. Accessed December 17, 2023. https://oshc.dole.gov.ph/wp-content/uploads/2023/10/LA-20-series-of-2023.pdf Social Security System. SSS Benefits Overview. N.d. Accessed December 17, 2023. https://www.sss.gov.ph/sss/appmanager/pages.jsp?page=ssbenefits Government Service Insurance System. Policy and Procedural Guidelines No. 274-14. Published 2016. Accessed December 17, 2023. https://www.gsis.gov.ph/downloads/ppg-br/20160304-PPG-274-14.pdf Philippine Cancer Society. Hospice Groups. N.d. Accessed December 17, 2023. https://www.philcancer.org.ph/index.php/support/hospice-groups Silakbo PH. Mental Health Resources. N.d. Accessed December 17, 2023. http://www.silakbo.ph/help/ MentalHealthPH. Directory. N.d. Accessed December 17, 2023. https://mentalhealthph.org/directory/ Department of Health. The Philippine Cancer Control Program. N.d. Accessed December 17, 2023. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 151 https://doh.gov.ph/sites/default/files/health_programs/The-Philippine-Cancer-Control-Program.pdf Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 152 Hypertension is defined as the presence of an office blood pressure (BP) of 140/90 mm Hg or above, typically at least twice taken on 2 separate days 1. It is a common disorder affecting Filipinos with an estimated prevalence of 19.2% among adults in 2018. Hypertension is an important risk factor for other cardiovascular diseases including ischemic heart disease (IHD), heart failure (HF), stroke, chronic kidney disease (CKD), and peripheral arterial disease. IHD, stroke, and CKD are among the top 10 causes of mortality and morbidity in our country. Hence, the early detection and appropriate management of hypertension are public health priorities. Because individuals tend to have multiple risk factors for cardiovascular diseases, it is important that primary providers perform an overall assessment of cardiovascular disease risk in hypertensive patients and patients at risk of developing hypertension and create an individualized plan to address all CV risk factors. Table 22. Hypertension Continuum of Care Overview Hypertension Overview Risk Factors ● ● ● ● Prevention Healthy diet, limitation of sodium intake, exercise and physical activity, weight management (See General Wellness and Preventive Measures for general guidance) Screening Office BP measurements. Use standardized BP measurement protocol at every clinic visit. History and PE. Screen for other cardiovascular risk factors, secondary causes of hypertension. A single BP measurement is not enough to confirm the diagnosis of hypertension. Confirm diagnosis using any of the following confirmatory methods: ● Ambulatory BP monitoring (preferred) ● Home BP monitoring (HBPM) ● Repeat Office BP measurement (OBPM) using standardized BP measurement protocol Request for basic laboratory tests: 12 -L ECG, FBS, Lipid Profile, Serum Creatine, Sodium, Potassium, GFR BP reduction to <130/80 mmHg in most hypertensive patients First-line. Angiotensin-converting enzyme inhibitors (ACEI), Angiotensin-receptor blockers (ARB), Calcium channel blockers (CCBs), Thiazide/Thiazide-like diuretics (TZD/TZDL) (as monotherapy or in combination) Dosing should be titrated according to BP response and BP targets ● Sodium intake <1500 mg/day ● Healthy diet ● Regular exercise ● Weight loss >5% in those who are overweight or obese ● Avoid or moderate alcohol intake ● Stop/avoid smoking Diagnosis Therapeutic Goal Pharmacologic Treatment Non-pharmacologic management Age Obesity and weight gain High dietary sodium intake Low dietary calcium and potassium intake ● ● ● ● ● Smoking/vaping Alcohol consumption Low levels of physical activity Psychosocial stress Genetics Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 153 Signs and Symptoms ● Most hypertensive individuals are asymptomatic, leading to complacency and poor adherence to medical management. Therefore, primary care providers should: ○ Ensure that all adults are well-informed about the consequences of untreated hypertension. ○ Observe due diligence in eliciting signs and symptoms of hypertensive complications or hypertension-mediated organ damage (HMOD) such as the following2: ■ Brain and eyes: headache, vertigo, syncope, impaired vision, transient ischemic attack, sensory or motor deficit, stroke, carotid revascularization, cognitive impairment, dementia (in the elderly) ■ Heart: chest pain, shortness of breath, oedema, myocardial infarction, coronary revascularization, syncope, history of palpitations, arrhythmias (especially AF), heart failure ■ Kidney: thirst, polyuria, nocturia, haematuria, urinary tract infections ■ Peripheral arteries: cold extremities, intermittent claudication, pain-free walking distance, pain at rest, peripheral revascularization Screening ● ● Office BP measurement ○ Screen all adult Filipinos for hypertension through office BP measurement using a properly validated automated/digital/electronic oscillometric device with an appropriately-sized cuff during each clinic visit.1,2,3 If no automated oscillometric device is available, consider using a manual sphygmomanometer in office BP measurement Office BP Measurement with an appropriately-sized upper arm cuff, according to the Standard BP Measurement Protocol.1 ○ Perform office BP measurement using the Standard Office BP Measurement Protocol 4 Cardiovascular disease (CVD) risk assessment ○ Obtain comprehensive history and cardiovascular disease risk assessment using the WHO CVD Risk Charts 5 or other validated CV risk assessment tools/calculators (e.g. ASCVD risk calculator). Diagnostic Tests ● Minimum at Primary Care. Confirm the diagnosis of hypertension through any of the following methods, depending on the availability and patient values/preferences: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 154 Diagnostic Tests Out of office BP Measurement: Ambulatory blood pressure monitoring (ABPM) (preferred method if available, gold standard) (Recommended)1 ○ Out of office BP Measurement: Home BP monitoring (HBPM) (Recommended)1 ○ Office BP Measurement (OBPM): Repeat office BP measurements on succeeding visit1 Note that a single measurement of blood pressure is not enough to confirm the diagnosis of hypertension due to the phenomena of white coat hypertension and masked hypertension. ■ Use the following BP classification for adult Filipinos (Recommended)1 ● Normal: BP <120/80 mmHg ● Borderline: BP 120-139/80-89 mmHg ● Hypertension: BP more than or equal to 140/90 mmHg Additional tests at primary care. Perform basic laboratory testing in hypertensive patients to search for HMOD and important comorbidities, ideally within 1 month from the confirmation of the diagnosis of hypertension in an adult patient 2,3,6 : ■ 12-lead ECG - to screen for LVH and other cardiac abnormalities and, document baseline heart rate and rhythm ■ Fasting blood glucose - to screen for Diabetes Mellitus ■ Lipid profile - to determine baseline lipid levels and guide cardiovascular risk reduction (primary or secondary prevention) strategy ■ Serum Creatinine, estimated Glomerular Filtration Rate (eGFR), sodium, potassium - to detect possible renal disease and electrolyte abnormalities that can affect choice of anti-hypertensive drugs ■ Dipstick Urine test or urinary albumin/creatinine ratio - to detect possible renal disease and guide choice of anti-hypertensive treatment Additional tests at a higher level of care. ○ Perform additional tests, such as the following if Hypertension-Mediated Organ Damage (HMOD) is strongly suspected 2,3. Alternatively, facilitate referral to a higher level of care as necessary. ■ Renal Ultrasound (US) ■ Echocardiography ■ Brain Imaging ■ Ankle Brachial Index (ABI) ■ Carotid Imaging ■ Retinal Exam ○ ● ● Treatment ● Start treatment in all adults who are confirmed to have hypertension through any of the previously mentioned confirmatory methods (ABPM, HBPM, OBPM). Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 155 Treatment ● ● BP Target. ○ Target to control the BP of hypertensive adults, including individuals with diabetes or chronic kidney disease or history of stroke, to a goal BP of <130/80 mmHg (Recommended)1. ○ Avoid lowering systolic BP to less than 120 mmHg and diastolic BP to less than 70 mmHg in patients with hypertension and concomitant coronary artery disease. Non-pharmacologic therapy. Advise all patients who have hypertension or pre-hypertension to observe the following (Recommended)1: ○ Limit sodium intake to less than 1500 mg/day (approximately equivalent to less than ¾ teaspoon of salt) ○ Adhere to a healthy dietary pattern, guided by the Dietary Approaches to Stop Hypertension (DASH) meal plan7 and PInggang Pinoy8. ○ Perform moderate to vigorous aerobic physical activities, consisting of at least 150 minutes per week of accumulated moderate-intensity physical activity or 75 minutes per week of vigorous-intensity physical activity, unless medically contraindicated, and dynamic resistance exercises 1, 9. ○ Maintain body weight between recommended limits10 ■ For obese or overweight adults, target weight loss of least 3% of baseline weight 1.1 ● ○ Avoid alcohol intake or drink in moderation. ○ Stop/avoid smoking/vaping. First line pharmacologic therapy. ○ Offer pharmacologic treatment in all patients with hypertension. The following are the first-line antihypertensive drugs and can be used as monotherapy (one drug in one pill) or in combination (at least two drugs) (Recommended)1. ■ Angiotensin-converting enzyme inhibitors (ACEI) (e.g., Enalapril, Captopril, Lisinopril, etc., ) ■ Angiotensin-receptor blockers (ARB) (e.g., Telmisartan, Valsartan, Losartan., etc.) ■ Calcium channel blockers (CCBs) (e.g., Amlodipine, Felodipine, etc.,) ■ Thiazide/Thiazide-like diuretics (TZD/TZDL) (e.g., Hydrochlorothiazide, Chlorthalidone, etc.) ■ If using combination-therapy, the following may be combined (2 drugs in one pill or free combinations) (Recommended, PSH 2020): ■ ACEI + CCB ■ ACEI + TZD/TZDL ■ ARB + CCB ■ ACEI + TZD/TZDL ○ Other combination therapies may be used if with compelling indications. ■ Use an ACEI or ARB as first-line medication for CKD patients with urinary albumin-to-creatinine ratio more than or equal to 30 mg/g (or equivalent) (Recommended)1. Administer the antihypertensive medication at bedtime. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 156 Treatment Prioritize the use of the following BP-lowering drug classes for specific types of hypertensive patients with coronary artery disease 2,3: ● For patients with a history of heart attack/myocardial infarction: beta-blockers and RAS blockers (ACEI or ARB): ● For patients with angina but no prior history of heart attack/myocardial infarction: beta blockers and/or CCBs ● Prioritize the use of an ACE inhibitor or ARB, and a beta-blocker and diuretic and/or mineralocorticoid receptor antagonist in the treatment of Hypertension in a patient diagnosed with Heart Failure with reduced Ejection Fraction (HFrEF) 2,3 ○ Titrate the dosing of medications and add additional first-line drugs as needed to lower BP and achieve BP targets (see sample Titration Guide). Special considerations in administering anti-hypertensive medications ○ Do not combine ACEIs with ARBs or ACEIs and ARBs with direct renin inhibitors.1 ○ In hypertensive women who are of reproductive age and without consistent contraception, perform a pregnancy test to rule out pregnancy prior to the initiation of ACE inhibitors, ARBs, or thiazide diuretics. ○ Discontinue ACEI or ARB and shift to a non-dihydropyridine CCB (Diltiazem or Verapamil) if a hypertensive patient with CKD develops any of the following: ■ Serum creatinine level increases by 30 % over baseline during the first two months of treatment. ■ Hyperkalemia (K+ more than or equal to 5.6 mmol/L). ■ Adverse effects are experienced by the patient. ■ ● Monitoring and Follow-up ● Schedule regular follow-up to monitor achievement of BP target, check for adverse effects, and titrate dose of antihypertensive medications. ○ Consider scheduling monthly follow-up after initiation of treatment or modifying a patient’s antihypertensive therapy until the BP target is reached. (Conditional)6 Consider scheduling longer follow-up periods (e.g., every 3-6 months) in patients who ○ have reached their BP targets/whose BP are under control. (Conditional)6 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 157 Referral ● ● Refer the following hypertensive patients to a specialist for outpatient evaluation and individualized management (Recommended)1: ○ Patients with Diabetic Kidney Disease ○ Patients with Grade 4 and 5 CKD ○ Patients with proteinuria of more than 1g/day ○ Patients with Coronary Artery Disease and very low diastolic BP < 50 mmHg ○ Patients with White Coat Hypertension ○ Patients with symptomatic postural hypotension ○ Patients with resistant hypertension (BP remains uncontrolled despite receiving maximally-tolerated doses of 3 drug classes, including a diuretic) ○ Suspicion of pheochromocytoma (repetitive episodes of sweating, headache, anxiety, or palpitations) and other causes of secondary hypertension ○ Patients with suspected coronary artery disease ○ Patients with suspected heart failure ○ Patients above 90 years of age, very frail or with limited life expectancy Refer patients presenting with hypertensive emergencies immediately for inpatient emergent specialty care 2,3. ○ Severely elevated blood pressure (SBP≥180 mmHg or DBP ≥110 mmHg) PLUS any of the following: ○ New-onset blurring or loss of vision, retinal hemorrhage or papilledema on fundoscopy ○ Lethargy, seizures, cortical blindness, and coma in the absence of other explanations ○ New onset neurologic deficit - consider acute stroke ○ New onset chest pain or difficulty of breathing - consider acute coronary syndrome or acute heart failure First-aid Measures and Basic Emergency Care ● Administer the following measures to patients presenting with hypertensive urgency or emergency. ○ For Hypertensive Urgency (severe BP elevation in a stable patient WITHOUT acute organ damage or change in baseline target): ■ Adjust/intensify maintenance medications, ensure adherence to therapy, and arrange follow-up within a short period12 ■ BP reduction is best achieved with oral medication according to the drug treatment algorithm and initiation of long-acting BP medications 2 (ESC, 20182) ○ Hypertensive Emergency/ Hypertensive Crisis (severe BP elevation accompanied by new or worsening target organ damage or dysfunction): ■ Create intravenous access and administer intravenous Nicardipine or Labetalol (if available) 12 while awaiting/facilitating transfer to a higher level of care. Do not delay immediate transfer. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 158 First-aid Measures and Basic Emergency Care ● ● Nicardipine continuous IV infusion: Initial: 5 mg/hour; titrate by 2.5 mg/hour at 5- to 15-minute intervals to achieve target blood pressure; maximum dose: 15 mg/hour 13 Labetalol ○ Intermittent IV: Initial: 10 to 20 mg over 1 to 2 minutes followed by 20 to 80 mg every 10 minutes until target blood pressure is reached; consider a continuous infusion if unable to obtain target blood pressure 14 ○ Continuous IV infusion: Initial loading dose: 10 to 20 mg over 2 minutes (optional if intermittent dosing is used), followed by 0.5 to 2 mg/minute; some patients may require titration up to 10 mg/minute 14 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Philippine Society of Hypertension & Philippine Heart Association. Clinical Practice Guidelines for the Management of Hypertension in the Philippines. Published 2020. Accessed December 14, 2023. https://drive.google.com/file/d/1t3UFLQG6XxTUNkVniliIbKnvnUVmDuKD/view Williams B, Mancia G, Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal. 2018;39(33):3021-3104. doi:https://doi.org/10.1093/eurheartj/ehy339 Unger et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension, 75(6), 1334-1357. PMID: 32370572. 10.1161/HYPERTENSIONAHA.120.15026. 2020. https://www.ahajournals.org/doi/epub/10.1161/HYPERTENSIONAHA.120.15026 Department of Health. Draft CSTs for Hypertension. N.d. Accessed December 14, 2023. https://docs.google.com/presentation/d/1ArqWhDhR4GqXGj1F0G1h3n1kTQy0mKv_ZAE1O7lku-Y/edit#slide=id.g1be13ff716f_3_439 World Health Organization. WHO cardiovascular disease risk laboratory-based charts. N.d. Accessed December 16, 2023. https://cdn.who.int/media/docs/default-source/ncds/cardiovascular-diseases/southeast-asia--corrected.pdf?sfvrsn=e7994290_0 World Health Organization. Guideline for the Pharmacological Treatment of Hypertension in Adults.; 2021. Accessed December 17, 2023. https://iris.who.int/bitstream/handle/10665/344424/9789240033986-eng.pdf?sequence=1 National Institutes of Health. DASH Eating Plan. N.d. Accessed December 16, 2023. https://www.nhlbi.nih.gov/education/dash-eating-plan Department of Science and Technology. Pinggang Pinoy - Adults. N.d. Accessed December 16, 2023. https://www.fnri.dost.gov.ph/images/sources/PinggangPinoy-Adult.pdf World Health Organization. Guidelines on physical activity and sedentary behaviour. Published 2020. Accessed December 16, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7719906/pdf/bjsports-2020-102955.pdf World Health Organization. A healthy lifestyle - WHO recommendations. Published 2010. Accessed December 16, 2023. https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations U.K. National Institute for Health and Care Excellence. Weight management: lifestyle services for overweight or obese adults. Published 2014. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ph53/chapter/4-considerations Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269-1324. doi:https://doi.org/10.1161/hyp.0000000000000066 Uptodate. Nicardipine Drug information. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/nicardipine-drug-information?search=nicardipine&source=panel_search_result&selectedTitle =1~85&usage_type=panel&kp_tab=drug_general&display_rank=1 Uptodate. Labetalol: Drug information. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/labetalol-drug-information?search=labetalol%20hypertensive%20urgency&source=search_res ult&selectedTitle=2~149&usage_type=default&display_rank=2 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 159 Major Depressive Disorder is described as depressed mood or sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, tiredness and poor concentration. These symptoms affect one’s ability to cope with life, including ability to study or work.1 The Department of Health recognizes Major Depressive Disorder (MDD) as one of the most common mental health conditions in the Philippines, occurring mostly in younger adults, with one in every ten young adult Filipinos having MDD.2,3 It is estimated that MDD contributed to 0.95% of total DALYs among Filipinos.4 Because it predominantly affects young adults, MDD may also affect community productivity and economic status. Moreover, MDD may also lead to death through suicide. According to WHO, there is a substantial increase in the suicide rate of the Philippines in the past three decades. The latest estimated mortality from suicide in the country was 2.5 per 100,000 in 2019, although the WHO also recognized the possibility of underreporting due to religious beliefs and likely stigmatization of the family1. All of these data emphasize that MDD has to be recognized and managed early and clinical and public health interventions to safeguard mental health are necessary. Table 23. Major Depressive Disorder Continuum of Care Overview Major Depressive Disorder Overview Risk Factors Screening Diagnosis Pharmacologic Treatment Non-pharmacologic management Internal factors: female sex, history of anxiety, low self-esteem, Neuroticism External factors: conduct disorder, substance use Adverse life events: childhood sexual abuse, chronic medical conditions, disturbed family environment, history of divorce, lifetime trauma, low educational status, low social support, parental loss Center for Epidemiologic Studies Depression Scale (CES-D) among ill adults and caregivers Patient Health Questionnaire-9 (PHQ-9) among healthcare workers PHQ-2 among adults in the general population Edinburgh Postnatal Depression Scale or PHQ-9 among pregnant adults Diagnose depression among adults using the criteria from the Diagnostic and Statistical Manual of Mental Disorders 5th Edition. Additional laboratory tests: thyroid stimulating hormone, complete blood count, serum electrolytes, and liver function test to rule out other medical conditions. ● ● ● First-line: Monotherapy using either non-pharmacologic interventions (e.g. therapy) or second generation antidepressant (Escitalopram, Fluoxetine, Sertraline Venlafaxine, Bupropion, Mirtazapine), or Combination therapy using second generation antidepressant with CBT or interpersonal psychotherapy ● Exercise monotherapy ● St. John’s Wort ● Bright light therapy ● Yoga ● Acupuncture Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 160 Signs and Symptoms ● ● Suspect depression among adults presenting with depressed mood, interest deficit (anhedonia), changes in sleeping patterns (insomnia or sleeping more), guilt (worthlessness, hopelessness or regret), energy deficit, concentration deficit, changes in appetite, psychomotor agitation or retardation, and suicidality or self-harm.5 Consider depression particularly among adults with symptoms who have a past history of depression or who have chronic comorbidities especially those with associated functional impairment.6 Screening ● ● ● Screen high-risk adults for depression using Center for Epidemiologic Studies Depression Scale (CES-D) among ill adults and caregivers and using Patient Health Questionnaire-9 (PHQ-9) among healthcare workers. (Strong Recommendation)7 Consider screening for depression among adults in the general population regardless of risk factors for depression using PHQ-2 followed by PHQ-9 if depression is identified.5 (Recommended)8 Consider screening for depression among pregnant adults at least once during perinatal period and at least once during four to eight weeks after delivery using Edinburgh Postnatal Depression Scale or PHQ-9.5 Diagnostic Tests ● Minimum at primary care. Diagnose depression among adults using the following criteria from the Diagnostic and Statistical Manual of Mental Disorders 5th Edition 5,14: A. Five (or more) of the following symptoms have been present during the same two-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure. NOTE: Do not include symptoms that are clearly attributable to another medical condition. 1) Depressed mood most of the day, nearly every day, as indicated by either subjective report (eg, feels sad, empty, hopeless) or observations made by others (eg, appears tearful). (NOTE: In children and adolescents, can be irritable mood.) 2) Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation). 3) Significant weight loss when not dieting or weight gain (eg, a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. (NOTE: In children, consider failure to make expected weight gain.) 4) Insomnia or hypersomnia nearly every day. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 161 Diagnostic Tests ● 5) Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down). 6) Fatigue or loss of energy nearly every day. 7) Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick). 8) Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by their subjective account or as observed by others). 9) Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. C. The episode is not attributable to the direct physiological effects of a substance or to another medical condition. NOTE: Criteria A through C represent a major depressive episode. NOTE: Responses to a significant loss (eg, bereavement, financial ruin, losses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode. Although such symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should also be carefully considered. This decision inevitably requires the exercise of clinical judgement based on the individual's history and the cultural norms for the expression of distress in the context of loss. D. The occurrence of the major depressive episode is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified and unspecified schizophrenia spectrum and other psychotic disorders. E. There has never been a manic or hypomanic episode. NOTE: This exclusion does not apply if all of the manic-like or hypomanic-like episodes are substance-induced or are attributable to the physiological effects of another medical condition. Specify: With anxious distress With mixed features With melancholic features With atypical features With psychotic features With catatonia With peripartum onset With seasonal pattern Consider assessing adult patients with depression regarding ideation or intention for suicide or self-harm.6 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 162 Diagnostic Tests ● Additional laboratory tests. Consider requesting laboratory tests as warranted, such as thyroid stimulating hormone, complete blood count, serum electrolytes, and liver function test, to rule out other medical conditions.5 Treatment ● ● ● ● First Line. Provide interventions to adults after shared decision making with them and their families as first line management6: (Recommendation for Use9); (Strong recommendation 10) ○ Monotherapy using either: ■ Non-pharmacologic interventions (such as behavioral therapy, cognitive behavioral therapy (CBT), mindfulness based cognitive therapy, interpersonal psychotherapy, psychodynamic therapies, or supportive therapy), or ■ Second generation antidepressant (such as Escitalopram 10mg tablet, Fluoxetine 30 mg capsule, Sertraline 50mg tablet, Venlafaxine 75 mg capsule, Paroxetine 20 mg tablet, Duloxetine 30 mg capsule, Vortioxetine 5 mg tablet, Bupropion 150 mg tablet, or Mirtazapine 15mg tablet) ○ Combination therapy using second generation antidepressant with CBT or interpersonal psychotherapy. Provide pregnant adults at-risk for depression or those depressed with counseling interventions such as CBT or interpersonal psychotherapy. (Recommended)11 Consider developing a safety plan among adults with depression who have self-harmed or at risk of suicide.6,12 Other Non-Pharmacologic Options. Consider offering the following as adjunctive treatment such as exercise monotherapy, St. John’s Wort, bright light therapy, yoga, or acupuncture to adults with depression. (Conditional recommendation for use)9 Referral ● Refer adults with severe symptoms, with marked or significant impairment on personal or social functioning, self-neglect, or risk for self-harm or suicide, harm to others, those with personality disorder or with psychotic symptoms, adults not responsive to treatment, or pregnant adults, to the next level of care.6,10,11 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 163 First Aid Measures and Basic Emergency Care ● Assess the general status of the patient and provide urgent and appropriate medical care to adults who have self-harmed or have attempted suicide prior to referral to the next level of care.12,13 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. World Health Organization. Prevention and management of mental health conditions in The Philippines: The case for investment. Published 2021. Accessed December 16, 2023. https://www.who.int/docs/default-source/wpro---documents/countries/philippines/reports/investment-case-report-mental-healthphilippines-2021.pdf?sfvrsn=d0f436e7_9 Department of Health. Depression. HealthyPilipinas. N.d. Accessed December 16, 2023. https://healthypilipinas.ph/health-a-z/depression Puyat JH, Gastardo-Conaco MaC, Natividad J, Banal MA. Depressive symptoms among young adults in the Philippines: Results from a nationwide cross-sectional survey. Journal of Affective Disorders Reports. 2021;3:100073. doi:https://doi.org/10.1016/j.jadr.2020.100073 Institute for Health Metrics and Evaluation. GDB Compare. Published 2019. Accessed December 16, 2023. https://vizhub.healthdata.org/gbd-compare/ Maurer DM, Raymond TJ, Davis BN. Depression: Screening and Diagnosis. American Family Physician. 2018;98(8):508-515. Accessed December 17, 2023. https://www.aafp.org/pubs/afp/issues/2018/1015/p508.html U.K. National Institute for Health and Care Excellence. Depression in adults: treatment and management. Published 2022. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng222/chapter/Recommendations University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Mental Health and Addiction. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1Nq-QO0UYMh0MiLWeKmO8CSdcuZyFdlbg/view U.S. Preventive Services Task Force. Depression and Suicide Risk in Adults: Screening. Published 2023. Accessed December 16, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-depression-suicide-risk-adults American Psychological Association. Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts. Published 2019. Accessed December 16, 2023. https://www.apa.org/depression-guideline/guideline.pdf Qaseem A, Owens DK, Etxeandia-Ikobaltzeta I, Tufte J, Cross JT, Wilt TJ. Nonpharmacologic and Pharmacologic Treatments of Adults in the Acute Phase of Major Depressive Disorder: A Living Clinical Guideline From the American College of Physicians. Annals of Internal Medicine. 2023;176(2):239-252. doi:https://doi.org/10.7326/m22-2056 U.S. Preventive Services Task Force. Perinatal Depression: Preventive Interventions. Published 2019. Accessed December 16, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/perinatal-depression-preventive-interventions U.K. National Institute for Health and Care Excellence. Self-harm: assessment, management and preventing recurrence. Published 2022. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng225/chapter/Recommendations#involving-family-members-and-carers UpToDate. Suicidal ideation and behavior in adults. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/suicidal-ideation-and-behavior-in-adults?search=self%20harm&source=search_result&selecte dTitle=5~150&usage_type=default&display_rank=5# American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C.: 2013. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 164 Methamphetamine Use Disorder Methamphetamine is an illicit psychostimulant that is smoked, snorted, injected or ingested orally that causes the release and blocks the reuptake of neurotransmitters such as dopamine, norepinephrine, and serotonin. Methamphetamine use disorder refers to the illicit use of methamphetamines that might involve dependence and/or substance abuse 1,2. The estimated lifetime prevalence of substance and drug use disorder among Filipinos was 1%3. According to the latest available statistical analysis report of the Philippine Dangerous Drugs Board (2022), Methamphetamine Hydrochloride in the form of shabu remains as the leading drug of abuse in the Philippines seen as 92.06% of total admissions in their rehabilitation program3. Worldwide, amphetamine-type stimulants such as methamphetamine are recorded as the fastest rising drug of abuse, with increasing use recorded in Asia and Oceania1. Because of their symptoms, drug dependence, and or exacerbation of existing other physical or psychological issues, heavy and frequent methamphetamine users eventually encounter physical, familial, social, and economical issues in their lives due to lack of/altered functionality and productivity.1,4 Table 24. Methamphetamine Use Disorder Continuum of Care Overview Methamphetamine Use Disorder Overview Signs and Symptoms Acute changes in behavior, symptoms and signs of nervous system activation, psychosis, delusions, or hallucinations, catatonia, symptoms of abstinence syndrome, may present with cognitive changes Screening Use of standardized tools one a year during annual check-up -Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), National Institute on Drug Abuse (NIDA) -Prenatal Risk Overview (PRO) for pregnant adults Diagnosis Non-pharmacologic management Urine screening tests, including confidentiality of records, conducted in accordance with RA 9165 “Comprehensive Dangerous Drugs Act of 2002.” Assess using the Diagnostic and Statistical Manual of Mental Disorders 5th Edition Urine testing (+) to undergo confirmatory testing using gas chromatography/ mass spectrometry First Line Therapy. Psychosocial therapy using contingency management with or without other behavioral interventions, such as: individual or group therapy, intensive outpatient therapy, cognitive behavioral therapy, or motivational interviewing for 3 weeks, taking patient preference and availability of treatment. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 165 Signs and Symptoms ● Consider methamphetamine (MAP) use disorder among adults who use methamphetamine, in various ways including orally, smoked, snorted, or dissolved in liquids, accompanied by clinical manifestations such as the following1,4: ○ Acute changes in behavior (e.g., increased energy and alertness, decreased need for sleep, euphoria, increased sexuality, grinding teeth, itching, disorganized thinking, etc.) ○ Symptoms and signs of nervous system activation (e.g., sweating, gastrointestinal symptoms, pupillary dilatation, increased heart rate) ○ Psychosis, predominantly paranoia, persecutory delusions, auditory, visual, and tactile hallucinations ○ Catatonia ○ With or without cognitive changes ○ Symptoms of abstinence syndrome in individuals who discontinue MAP (e.g., anhedonia, irritability, poor concentration, hyperphagia, insomnia or hypersomnia, psychomotor agitation or retardation). Screening ● ● Screen adults for methamphetamine use disorder using standardized tools, such as Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), National Institute on Drug Abuse (NIDA), or for pregnant adults using Prenatal Risk Overview (PRO), at least once a year during annual check-up. (Strong Recommendation5) (Recommended6) Urine screening tests, including confidentiality of records, shall be conducted in accordance with the provisions of the Republic Act No. 9165 “Comprehensive Dangerous Drugs Act of 2002”. Diagnostic Tests ● Minimum at primary care. ○ Diagnose methamphetamine use disorder among adults using the criteria from the Diagnostic and Statistical Manual of Mental Disorders 5th Edition.1,4,11 ■ A problematic pattern of amphetamine-type substance, cocaine or other stimulant use (eg, methamphetamine use) leading to clinically significant impairment or distress, as manifested by two or more of the following within a 12-month period: ● Methamphetamine is often taken in larger amounts or over a longer period than was intended ● There is a persistent desire or unsuccessful efforts to cut down or control methamphetamine use Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 166 Diagnostic Tests A great deal of time is spent in activities necessary to obtain methamphetamine, use methamphetamine, or recover from its effects ● Craving, or a strong desire or urge to use methamphetamine ● Recurrent methamphetamine use resulting in a failure to fulfill major role obligations at work, school, or home ● Continued methamphetamine use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of methamphetamine ● Important social, occupational, or recreational activities are given up or reduced because of methamphetamine use ● Recurrent methamphetamine use in situations in which it is physically hazardous ● Continued methamphetamine use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by methamphetamine ● Tolerance* ● Withdrawal* * These criteria are not considered to be met for those taking methamphetamine solely under appropriate medical supervision, such as for attention deficit hyperactivity disorder or narcolepsy. ○ Adults who screened positive in urine testing shall undergo confirmatory testing using gas chromatography/ mass spectrometry and shall be conducted with confidentiality in accordance with the provisions of the Republic Act No. 9165 “Comprehensive Dangerous Drugs Act of 2002.” Assess for other psychiatric comorbidities (e.g., depression, anxiety, psychosis, potential for self-harm, personality disorders), other substance use, medical comorbidities, and cardiovascular risk. Other Laboratory Tests. Consider requesting laboratory tests as warranted to evaluate other medical conditions (e.g., electrocardiogram).1,4, ● ● ● Treatment ● ● First Line Therapy. Consider providing psychosocial therapy using contingency management with or without other behavioral interventions, such as individual or group therapy, intensive outpatient therapy, cognitive behavioral therapy, or motivational interviewing, taking patient preference and availability of treatment. (Weak Recommendation7);8 ○ Consider continuing psychosocial treatment for up to one year for adults who responded8 Other Non-Pharmacologic Treatment. Consider active group involvement on community-based drug rehabilitation programs (e.g.Katatagan, Kalusugan, at Damayan ng Komunidad), using peer Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 167 Treatment ● ● linkage or 12-step facilitation therapy, to adults in early recovery, or following relapse. (Weak Recommendation7) Add-on Pharmacologic Treatment. Consider pharmacologic treatment, such as bupropion 450 mg once a day or mirtazapine 30 mg once a day, in addition to psychosocial interventions, to adults with suboptimal response 8 to 12 weeks after initial treatment.8 Special considerations. Treatment may commence in Drug Treatment and Rehabilitation Centers designated by the Dangerous Drug Board (DDB) for individuals who voluntarily submit for treatment and rehabilitation for drug dependency, according to the provisions of Republic Act No. 9165 “Comprehensive Dangerous Drugs Act of 2002.9 Referral ● Refer adults suspected of methamphetamine intoxication presenting with diaphoresis, hypertension, tachycardia, severe agitation, psychosis, delirium or in coma, hyperthermia, symptoms of metabolic acidosis, or in shock to higher level facilities.10 First Aid Measures and Basic Emergency Care ● ● Provide immediate first aid measures and basic emergency care to adults suspected of methamphetamine intoxication depending on the signs and symptoms of the patient10 and refer immediately to higher level of care: ○ For agitated patients, consider benzodiazepines using Midazolam 5 to 10 mg Intramuscularly (IV) or 2.5 to 5 mg Intravenously, Lorazepam 2 to 4 mg IV, or Diazepam 5 to 10 mg IV, repeated every 10 minutes as needed. Avoid physical restraints. ○ For hypertension and tachycardia, consider benzodiazepine doses as above. Consider using a calcium channel blocker to decrease the heart rate and the blood pressure (e.g. Diltiazem). Avoid beta-blockers. ○ For hyperthermia, consider benzodiazepine doses as above. Antipyretics are not recommended. Additionally, provide evaporative cooling measures or cooling blankets. ○ For hypovolemia, give fluid resuscitation using isotonic saline coupled with regular fluid monitoring. Consider cardiovascular complications (e.g., myocardial ischemia/infarction, valvular dysfunction, aortic rupture/dissection) in patients presenting with signs and symptoms such tachycardia, hypertension, and chest pain10. ○ Administer basic emergency care and facilitate immediate referral and transfer of these patients to higher levels of care. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 168 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. UpToDate. Methamphetamine use disorder: Epidemiology, clinical features, and diagnosis. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/methamphetamine-use-disorder-epidemiology-clinical-features-and-diagnosis?topicRef=10687 8&source=see_link# Paulus MP, Stewart JL. Neurobiology, Clinical Presentation, and Treatment of Methamphetamine Use Disorder. JAMA Psychiatry. 2020;77(9). doi:https://doi.org/10.1001/jamapsychiatry.2020.0246 Dangerous Drugs Board. 2022 Statistical Analysis. Published 2022. Accessed December 16, 2023. https://ddb.gov.ph/2022-statistical-analysis/ Klega AE, Keehbauch JT. Stimulant and Designer Drug Use: Primary Care Management. American Family Physician. 2018;98(2):85-92. Accessed December 17, 2023. https://www.aafp.org/pubs/afp/issues/2018/0715/p85.html University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX): Screening for Mental Health and Addiction. Published 2021. Accessed December 16, 2023. https://drive.google.com/file/d/1Nq-QO0UYMh0MiLWeKmO8CSdcuZyFdlbg/view U.S. Preventive Services Task Force. Unhealthy Drug Use: Screening. Published 2020. Accessed December 16, 2023. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening United States Department of Veteran Affairs. Clinical Practice Guideline for the Management of Substance Use Disorders. Published 2021. Accessed December 16, 2023. https://www.healthquality.va.gov/guidelines/MH/sud/VADoDSUDCPG.pdf UpToDate. Stimulant use disorder: Treatment overview. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/stimulant-use-disorder-treatment-overview Republic Act No. 9165 “Comprehensive Dangerous Drugs Act of 2002” UpToDate. Methamphetamine: Acute intoxication. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/methamphetamine-acute-intoxication?topicRef=82952&source=see_link# American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C.: 2013. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 169 Infectious Diseases Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 170 Community Acquired Pneumonia (CAP) is an acute infection of the pulmonary parenchyma acquired outside the hospital. The clinical manifestation of community-acquired pneumonia (CAP) can vary widely, encompassing mild cases with symptoms like fever and a productive cough, to more severe instances marked by respiratory distress and sepsis. Due to the diverse range of clinical features it presents, CAP is considered in the differential diagnosis of nearly all respiratory conditions1. Locally, pneumonia in general is the seventh leading cause of morbidity in the Philippines. Based on the 2022 FHSIS data, the incidence of pneumonia is at 180.87 per 100,000 population2. Pneumonia remains one of the top causes of mortality among Filipinos with about 5% of deaths attributable to it. This guide mainly focuses on the management of low-risk CAP. Table 25. Community-Acquired Pneumonia Continuum of Care Overview Community Acquired Pneumonia Overview Risk Factors ● ● ● ● ● ● Prevention Pneumococcal vaccination in eligible patients Hand hygiene and respiratory protection (e.g., masking) , smoking cessation (See General Wellness and Preventive Measures for general guidance) Pneumocystis jiroveci prophylaxis in patients living with HIV Not applicable Screening Diagnosis Pharmacologic Treatment Non-pharmacologic management Older Age Chronic comorbidities Viral respiratory infections Impaired airway protection (e.g., stroke, seizure, drug or alcohol use, dysphagia) Smoking, vaping, or alcohol overuse Crowded living conditions, low income settings, environmental toxin exposures Minimum at Primary Care. Clinical diagnosis and risk assessment through history and PE. Gold standard for etiologic diagnosis: culture For Low Risk CAP without comorbidities: Amoxicillin 500mg-1g thrice a day for 5-7 days Low Risk CAP with stable comorbidities: β-lactam with β-lactamase inhibitor combinations (BLIC e.g. Co-amoxiclav 500/ 125mg thrice a day for 5-7 days) or second generation cephalosporins (e.g. Cefuroxime 500mg twice a day for 5-7 days) with or without extended macrolides (Azithromycin 500mg once a day OR clarithromycin 500mg twice a day for 3-5 days) ● Smoking Cessation Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 171 Signs and Symptoms ● Consider community acquired pneumonia among adults presenting with acute symptoms including cough, breathlessness, and fever.3 Diagnostic Tests ● ● ● Minimum at primary care. Determine and classify the severity of pneumonia among adults during history and physical examination using validated clinical prediction tools1,3,4 such as Pneumonia Severity Index (PSI) or Confusion, Respiratory Rate, Blood Pressure and Age (CRB65). (PSI - Strong recommendation; Conditional recommendation4) ○ Risk stratification of patients with CAP ■ CAP Low-risk: normal vital signs, no coexisting or stable comorbidities, with CRB-65 score 0, PSI Score class I to II ■ CAP Moderate-risk: with oxygen saturation of <92%, CRB-65 score 1 to 2, PSI Score class III ■ CAP High-Risk: with respiratory failure requiring mechanical ventilation, with sepsis requiring vasopressor support, altered mental status, unstable vital signs, CRB-65 score score 3 to 4, PSI Score class IV to V Other laboratory tests. ○ Request rapid influenza molecular assay among adults with pneumonia in cases wherein there is a high influenza activity in the community (Strong recommendation4) ○ May consider requesting for chest radiography among adults with pneumonia5 Tests at higher level care. Transfer adults with moderate and severe pneumonia to a hospital for further diagnostic work-up, which can include the following depending on the clinical indication: ○ Sputum gram stain and culture 3,4 (Strong recommendation 4) ○ Complete blood count5 ○ Urine testing for pneumococcal antigen (Strong recommendation4) ○ Serum biomarkers such as Procalcitonin or C-Reactive Protein4,5,7 ○ Other imaging such as chest computed tomography scan or chest ultrasound5 Treatment ● First Line. Initiate empiric antimicrobial therapy within 4 hours of establishing diagnosis: ○ For adult patients without comorbidities or history of antibiotic therapy within 3 months: Amoxicillin 500 mg to 1 g capsule three times a day for 5 to 7 days4,6,8 (Strong recommendation4) ○ For adult patients with comorbidities such as chronic diseases, diabetes mellitus, alcoholism, cancers, or asplenia, and those with risk factors for methicillin resistant Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 172 Treatment ● Staphylococcus aureus or Pseudomonas aeruginosa, or with history of antibiotic therapy within 3 months 4,8: ■ Amoxicillin/ Clavulanate 500/125mg capsule three times a day for 5 to 7 days, or ■ Ampicillin/ Sulbactam 375 to 750 mg every 12 hours for 5 to 7 days, or ■ Cephalosporins such as: Cefpodoxime 200 mg two times a day or Cefuroxime 500 mg two times a day or Cefaclor 500 mg three times a day for 5 to 7 days, with or without ● Macrolide such as Azithromycin 500 mg once a day or Clarithromycin 500 mg two times a day for 3 to 5 days, or ● Doxycycline 100 mg two times a day for 3 to 5 days Alternative Therapy. Consider the following as alternative therapy: ○ For adult patients without comorbidities or history of antibiotic therapy within 3 months: ■ Doxycycline 100 mg twice a day for 5 days 4,6 (Conditional recommendation4), or ■ For adults with penicillin allergy or when the local pneumococcal resistance is <25%: Macrolide such as Azithromycin 500 mg D1 then 250 mg daily, or Clarithromycin 500 mg twice a day for 5 days (Conditional recommendation4) ○ For adult patients with comorbidities such as chronic diseases, diabetes mellitus, alcoholism, cancers, or asplenia, and those with risk factors for methicillin resistant Staphylococcus aureus or Pseudomonas aeruginosa, or with history of antibiotic therapy within 3 months, consider Fluoroquinolones such as Moxifloxacin, Levofloxacin, Gemifloxacin or Nemonoxacin.4,8 Prophylaxis ● Prophylaxis. Prescribe trimethoprim-sulfamethoxazole double strength oral tablet (160mg/800mg) once a day for Pneumocystis pneumonia prophylaxis to the following adults with HIV: ○ Adults with severe or advanced HIV clinical disease (WHO stage 3 or 4). (Strong recommendation9) ○ Adults with HIV regardless of CD4 count with active tuberculosis disease. (Strong recommendation9) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 173 Referral ● Refer adults with pneumonia who are hypotensive, exhibiting respiratory distress, in cardiopulmonary failure, with sepsis, with moderate to severe pneumonia, those who are not improving with antibiotic therapy, worsening symptoms, or unable to take oral antibiotics to higher levels of care.4, 6 First Aid Measures and Basic Emergency Care ● ● Consider supplemental oxygenation using a non rebreather mask for adults who appear clinically ill or hypoxic with pulse oxygen saturation <90 percent.10 Facilitate immediate transfer of patients presenting with septic shock. ○ Provide intravenous fluid resuscitation using crystalloids while awaiting/facilitating transfer (Strong Recommendation11) References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. UpToDate. Overview of community-acquired pneumonia in adults. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/overview-of-community-acquired-pneumonia-in-adults Department of Health. FHSIS - August 2022. Published 2022. Accessed December 16, 2023. https://doh.gov.ph/sites/default/files/publications/FHSIS_2022_Aug.pdf U.K. National Institute for Health and Care Excellence. Pneumonia in adults: diagnosis and management. 2023. https://www.nice.org.uk/guidance/cg191/chapter/recommendations#lower-respiratory-tract-infection American Thoracic Society and Infectious Diseases Society of America. Diagnosis and Treatment of Adults with Community-acquired Pneumonia: An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6812437/ UpToDate. Clinical evaluation and diagnostic testing for community-acquired pneumonia in adults. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/clinical-evaluation-and-diagnostic-testing-for-community-acquired-pneumonia-in-adults?topi cRef=117561&source=see_link# U.K. National Institute for Health and Care Excellence. Pneumonia (community-acquired): antimicrobial prescribing. Published 2019. Accessed December 16, 2023. https://www.nice.org.uk/guidance/ng138/chapter/Recommendations UpToDate. Procalcitonin use in lower respiratory tract infections. Published 2022. Accessed December 16, 2023. https://www.uptodate.com/contents/procalcitonin-use-in-lower-respiratory-tract-infections?sectionName=Community-acquired%2 0pneumonia%20in%20hospitalized%20patients&topicRef=7032&anchor=H3117849100&source=see_link#H3117849100 Chou CC, Shen CF, Chen SJ, et al. Recommendations and guidelines for the treatment of pneumonia in Taiwan. Journal of Microbiology, Immunology and Infection. 2019;52(1):172-199. doi:https://doi.org/10.1016/j.jmii.2018.11.004 World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. www.who.int. Published July 16, 2021. Accessed December 16, 2023. https://www.who.int/publications/i/item/978924003159 UpToDate. Approach to the adult with dyspnea in the emergency department. Published 2022. Accessed December 16, 2023. https://www.uptodate.com/contents/approach-to-the-adult-with-dyspnea-in-the-emergency-department?topicRef=1436&source=s ee_link#H4139199473 Philippine Society for Microbiology and Infectious Diseases. Clinical Practice Guidelines for Sepsis and Septic Shock. Published 2020. Accessed December 16, 2023. https://drive.google.com/drive/folders/1hNd6ImqyCqiPw1p1hHBA6jytGgLWLsC0 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 174 Coronavirus Disease (COVID-19) is a disease caused by the SARS-COV-2 virus. It spreads mostly through respiratory droplets but may also undergo airborne transmission, particularly during aerosol-generating procedures or AGPs (e.g., intubation, nebulization). Causing a pandemic and a declaration of public health emergency (PHE) in 2020, COVID-19 eventually affected millions of Filipinos, prompting nation-wide health system and service delivery changes. The clinical manifestation of this COVID-19 infection ranges from asymptomatic infection, to mild disease commonly presenting with fever, cough, tiredness and loss of taste or smell, to severe disease presenting with difficulty of breathing, neurologic changes, and cardiovascular symptoms such as chest pain1. In the initial phase of the pandemic, without vaccines and proven treatments, COVID-19 was difficult to manage, leading to disproportionately high mortality among affected individuals. As scientific evidence was generated worldwide, safe and efficacious vaccines and medications were developed, and effective non-pharmacologic interventions (NPIs) were utilized. These led to the successful control of the pandemic and eventual lifting of its global PHE status on May 5, 2023 by the WHO2, followed by the Philippines on July 21, 2023 through Proclamation No. 297. As of December 12, 2023, COVID-19 has affected 4,127,769 Filipinos, with a case fatality rate of 1.6%3. Continuing success in the prevention and control of COVID-19 entails collaborative multisectoral and multidisciplinary efforts. Table 26. COVID-19 Continuum of Care Overview COVID-19 Overview Risk Factors Prevention Screening Anyone can be infected but the following increase the risk of transmission4: ● Longer exposure to an infected person ● Shorter distance from an infected person ● Exposure to a symptomatic person ● Coughing, singing, shouting, or breathing heavily due to exertion ● Poor ventilation or air filtration Risk Factors for severe disease: ● Increasing age: older adults are more likely to get sick and hospitalized ● Immunocompromised /immunodeficient and pregnant individuals ● Presence of comorbidities/underlying health conditions (e.g., obesity, chronic obstructive pulmonary disease) Prevention of severe disease: Vaccination with primary series and updated boosters Prevention of transmission of the virus: ● Masking especially in crowded, enclosed, and poorly ventilated spaces ● Observance of proper hand hygiene ● Adherence to national and local public health protocols 7-day symptom-based test Diagnosis Minimum at Primary Care. Rapid antigen test (RAT) Gold standard: Reverse transcription polymerase chain reaction (RT-PCR) Pharmacologic Treatment for outpatients For mild-moderate disease in non-hospitalized patients with high risk of progression, within 5 days of symptom onset: ● First-line: Nirmatrelvir + Ritonavir (Paxlovid) , dosing depends on renal function5 ● Normal or mildly decreased renal function (eGFR ≥ 60 mL/min): 300 mg Nirmatrelvir + 100 mg Ritonavir BID PO x 5 days ● Moderately decreased renal function (eGFR 30-59 mL/min): 150 mg Nirmatrelvir + 100 mg Ritonavir BID PO x 5 days Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 175 Severely depressed renal function: not recommended by manufacturer ● Alternative: Remdesivir 200 mg as a single dose on day 1, followed by 100 mg once daily on days 2 and 3. Initiate as soon as possible after COVID-19 diagnosis and within 7 days of symptom onset5 ● Alternative: Molnupiravir 800 mg every 12 hours orally for 5 days; initiate as soon as possible after COVID-19 diagnosis, and within 5 days of symptom onset5 After initiating treatment with molnupiravir, if hospitalization is ● required, completion of 5-day course is at the health care provider's discretion Supportive treatment: Give supportive treatments to address the patient’s symptoms ● Antipyretics for fever ● Analgesics for headache, myalgia ● Antitussives for cough ● Advise the following: ● Oral hydration ● Advise adequate rest and sleep ● Home or facility for non-hospitalized patients ● Non-pharmacologic management Signs and Symptoms ● ● Consider the presence of COVID-19 in adults presenting with the following symptoms 1: ○ Most common symptoms: fever, chills, sore throat ○ Less common symptoms: muscle aches and heavy arms or legs, severe fatigue or tiredness, runny or blocked nose, or sneezing, headache, sore eyes, dizziness, new and persistent cough, tight chest or chest pain, shortness of breath, hoarse voice, numbness or tingling, appetite loss, nausea, vomiting, abdominal pain or diarrhea, loss or change of sense of taste or smell, difficulty sleeping COVID-19 and influenza are both respiratory diseases. It is difficult to distinguish COVID-19 from influenza by symptoms alone. If clinically indicated and/or necessary for surveillance, simultaneous testing for COVID-19 and influenza may be done 4. Screening ● Utilize a 7-day symptom-based test to determine the probability of possible COVID-19 infection among asymptomatic adults. (Strong recommendation6) ○ The 7-day symptom-based test includes assessment for the development of the following in asymptomatic individuals with history of exposure to a confirmed case or who are close contacts: ■ Fever (≥ 38 degrees Celsius) AND cough (WHO Case Definition for ILI7) OR Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 176 Screening Acute onset of 3 or more of the following: fever, cough, generalized weakness/fatigue, headache, myalgia, sore throat, coryza, dyspnea, nausea/diarrhea/anorexia Close contacts are defined as individuals who experienced the following 8: ■ Interacted with a person with COVID-19 within one meter for more than 15 minutes ■ Had direct physical interaction with probable or confirmed COVID-19 case ■ Had interaction with a person with COVID-19 without wearing protective equipment Avoid using rapid antigen testing for screening purposes in asymptomatic patients (Weak recommendation 6) ■ ○ ○ Diagnostic Tests ● ● ● Minimum at primary care. ○ Consider testing symptomatic patients with rapid antigen tests (RAT) for the diagnosis of COVID-19 (Weak recommendation6) ○ In the setting of an outbreak, consider testing using RAT for the diagnosis of COVID-19, provided the all of the following conditions are met (Weak recommendation 6): ■ Individuals are in the early phase of illness (≤ 7 days from symptom onset) AND ■ RAT kits use have sensitivity of ≥80% and specificity of ≥97% ○ Advise symptomatic individuals to use self-administered RAT if able, provided all of the following conditions are met (Strong recommendation6): ■ Ease of collecting samples is ensured; ■ Ease of interpretation is ensured; ■ Test kits have passed flex studies; AND ■ Symptoms have been present for ≤ 7 days. ○ In individuals whose RAT is negative but are highly suspected to have COVID-19, request for RT-PCR to confirm diagnosis, if available. Gold standard. RT-PCR remains the gold standard in confirming the diagnosis of COVID-19. However, it is not widely available in primary care settings and is more costly. Determine and classify the severity of COVID-19 among symptomatic individuals using the following criteria to guide management: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 177 Diagnostic Tests Table 27. Severity Classification of COVID-196 Classification Criteria Mild COVID-19 ● ● No pneumonia or desaturation# Acute onset of fever and cough or any three (3) or more of the following: ○ Fever ○ Cough ○ Coryza ○ Sore throat ○ Diarrhea ○ Anorexia/nausea/vomiting ○ Loss of sense of smell or taste ○ General weakness/body malaise/fatigue ○ Headache ○ Myalgia Moderate COVID-19 ● With pneumonia* BUT no difficulty of breathing or shortness of breath, RR < 30 breaths/min, oxygen saturation# >/= 94% at room air OR Without pneumonia but with risk factors for progression: elderly (60 years old and above) and/or with comorbidities ● Severe COVID-19 ● With pneumonia* and ANY one of the following: ○ Signs of respiratory distress ○ Oxygen saturation# < 94% at room air ○ Respiratory rate of ≥30 breaths/minute ○ Requiring oxygen supplementation Critical COVID-19 ● With pneumonia* and ANY one of the following: ○ Impending respiratory failure requiring high flow oxygen, non-invasive or invasive ventilation ○ Acute respiratory distress syndrome ○ Sepsis or shock ○ Deteriorating sensorium ○ Multi-organ failure ○ Thrombosis *Pneumonia – evidence of lower respiratory disease during clinical assessment (e.g. cough, fever plus crackles) and/or imaging (CXR, ultrasound, CT scan) #Proper recording of the O2 saturation: finger should be inserted in the oximeter for about 10-20 seconds; patient should be still and not talking. ● Other tests. ○ Obtain baseline peripheral oxygen saturation using a calibrated pulse oximeter. ○ Consider requesting a chest-x ray to facilitate rapid triage, infection control, and clinical management in the following types of patients (Weak recommendation6): ■ Patients who have mild COVID-19 but at risk of progression [e.g., elderly (60 years old and above) and/or with comorbidities] Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 178 Diagnostic Tests ● ■ Patients with moderate-severe COVID-19 ■ Patients with symptoms of at least 5 days duration ○ Consider testing for other differentials e.g. influenza, if clinically indicated. ○ Consider requesting for basic laboratory tests (e.g. BUN, Creatinine) if planning to administer Nirmatrelvir + Ritonavir (Paxlovid). Tests at higher level care. Transfer adults with moderate-severe COVID-19 for further diagnostic work-up, clinical management, and monitoring. Additional tests in higher levels of care may include the following: ○ More advanced imaging tests (e.g., CT Scan) ○ Laboratory tests: CBC, BUN, CRP, LDH, Ferritin, D-Dimer, etc. Treatment ● ● ● The following are the treatment options for outpatients with mild-moderate COVID-19. First Line. ○ For symptomatic individuals with mild-moderate COVID-19, with risk factors for progression to severe disease5, and within 5 days from symptom onset, offer Nirmatrelvir + Ritonavir (Paxlovid) (Strong recommendation 6); ■ Risk factors for progression based on studies on Nirmatrelvir + Ritonavir include: ≥60 years of age; BMI >25 kg/m2; cigarette smoking; immunosuppressive disease (including HIV infection with CD4 cell count <200mm3 and viral load <400 copies/mL) or prolonged iatrogenic immunosuppression; chronic lung, cardiovascular, kidney, or sickle cell disease; hypertension; diabetes; cancer; neurodevelopmental disorders or other medically complex conditions; or medical-related technological dependence ■ Adjust dosing based on renal function5: ■ Normal or mildly decreased renal function (eGFR ≥ 60 mL/min): 300 mg Nirmatrelvir + 100 mg Ritonavir BID PO x 5 days ■ Moderately decreased renal function (eGFR 30-59 mL/min): 150 mg Nirmatrelvir + 100 mg Ritonavir BID PO x 5 days ■ Severely depressed renal function: not recommended by manufacturer Alternatives to Nirmarelvir + Ritonavir. Consider offering the following treatments depending on the patient’s characteristics and drug availability: ○ For symptomatic individuals with mild-moderate COVID-19 with at least 1 risk factor* for progression to severe disease, consider offering Remdesivir5 (Weak recommendation 6 ); ■ Risk factors for progression based on studies on Remdesivir include: ≥60 years old, hypertension, cardiovascular or cerebrovascular disease, diabetes mellitus, Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 179 Treatment ● obesity (BMI≥30), immune compromise, chronic mild or moderate kidney disease, chronic liver disease, chronic lung disease, current cancer, or sickle cell disease ■ Remdesivir 200 mg as a single dose on day 1, followed by 100 mg once daily on days 2 and 3. Initiate as soon as possible after COVID-19 diagnosis and within 7 days of symptom onset5 ○ For symptomatic individuals with moderate COVID-19 who are non-oxygen-requiring and with at least 1 risk factor for progression, consider offering Molnupiravir (Weak recommendation6): ■ Risk factors for progression based on studies on Molnupiravir include: age >60 years, active cancer, chronic kidney disease, chronic obstructive pulmonary disease, obesity, serious heart conditions or diabetes mellitus ■ Molnupiravir 800 mg every 12 hours orally for 5 days; initiate as soon as possible after COVID-19 diagnosis, and within 5 days of symptom onset.5 ● After initiating treatment with molnupiravir, if hospitalization is required, completion of the 5-day course is at the health care provider's discretion. Symptom management. Provide supportive therapy (e.g. antipyretic, analgesic, mucolytics, etc.) to help address the symptoms of the patient. Non-pharmacologic Interventions ● Infection prevention and control measures. Ensure the observance of proper infection prevention and control (IPC) measures: ○ For healthcare workers. Observe standard precautions for all patients including the following9: ■ Hand hygiene through proper handwashing or by using an alcohol-based hand rub and respiratory hygiene. ■ Use appropriate PPE. ● Use well-fitting medical masks in healthcare facilities especially in areas of known or suspected community or cluster transmission (Strong recommendation9). ■ Observe proper cleaning, disinfection, and healthcare waste disposal according to IPC protocols ■ Also apply transmission-based precautions when indicated (e.g., when performing aerosol-generating procedures among patients with suspected or confirmed COVID-19, perform the procedure in an adequately ventilated room and use appropriate PPE (e.g. N95/FFP2 respirator or equivalent)9 ○ For patients. Advise to wear a medical mask. Advise hand and respiratory hygiene9. ○ For the community. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 180 Non-pharmacologic Interventions Encourage the community members to wear face masks for preventing COVID-19 in crowded, enclosed, and poorly ventilated spaces (Strong recommendation6). ■ Encourage vaccination against COVID-19 (Strong recommendation6) Ventilation. ■ Encourage the use of natural ventilation, including the opening of doors, windows, and use of electric fans in indoor spaces, if possible and safe to do so (Strong recommendation6). Isolation. Immediately isolate individuals with suspected, probable or confirmed COVID-19.9 ■ Advise patients to self-isolate in well-ventilated, ideally single rooms and accessible bathrooms. If patients are cohorted in isolation facilities, ensure bed space of at least 1 meter apart9. ■ Ensure availability of home monitoring kit (e.g. thermometer, pulse oximeter, etc.) ■ Observe the following updated masking and isolation protocols in accordance with DOH Department Circular 2023-0324: ■ ○ ○ Patient Characteristics Masking Isolation Quarantine Asymptomatic but confirmed COVID-19 Wear a well-fitted mask for 10 days Not applicable Not needed Confirmed COVID-19 case with mild symptoms OR individuals with acute respiratory symptoms (suspected/probably COVID-19) Wear a well-fitted mask for 10 days Home isolation for 5 days from onset of signs and symptoms OR until afebrile/fever-free for at least 24 hours without using antipyretics (e.g., Paracetamol) and with improvement of respiratory symptoms, whichever is earlier * duration of isolation may be shorted upon the advice of the healthcare provider Not applicable Confirmed COVID-19 case with moderate to severe symptoms, OR immunocompromised individuals with COVID-119 Wear a well-fitted mask for 10 days Isolation for at least 10 days from onset of signs and symptoms following the advice of the attending physician, including whether to be admitted to a healthcare facility Not applicable ● General advice. Advice all patients to observe the following: ○ Get adequate rest and sleep. ○ Be adequately hydrated. ○ Symptom monitoring ○ Do pulse oximetry monitoring at home. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 181 Non-pharmacologic Interventions ○ Use telemedicine modalities for communicating with healthcare providers for medical, psychosocial and mental health support Referral ● Refer all individuals with manifestations of severe and critical COVID-19 or progressive disease to higher level facilities (i.e. through the DOH National Patient Navigation and Referral Center (NPNRC) through 1555 and select option (2) for immediate and proper assessment as well as corresponding management and interventions) First Aid Measures and Basic Emergency Care ● ● ● Facilitate immediate transfer of patients presenting with the following symptoms to higher level facilities1: ○ Difficulty breathing, especially at rest, or inability to speak in sentences ○ Confusion, drowsiness, or loss of consciousness ○ Neurologic deficits (e.g., loss of speech or movement) ○ Persistent chest pain or pressure ○ Cold clammy skin or cyanosis Administer supplemental oxygenation using a low-flow system (ie, up to 6 L/minute) via nasal cannula10 in patients with mild desaturations, while awaiting transfer to a higher level facility, provided adequate IPC measures are observed. Balance the benefit and safety of administering high-flow oxygen (e.g. via oxygen mask) and nebulization to patients with suspected, probable, or confirmed COVID-19, given the risk of aerosolization. References 1. 2. 3. 4. 5. World Health Organization. Coronavirus Disease (COVID-19). N.d. Accessed December 16, 2023. https://www.who.int/health-topics/coronavirus#tab=tab_3 World Health Organization. WHO Director-General's opening remarks at the media briefing. Published 2023. Accessed December 16, 2023. https://www.who.int/news-room/speeches/item/who-director-general-s-opening-remarks-at-the-media-briefing--5-may-2023 Department of Health. COVID-19 Tracker. Published 2023. Accessed December 12, 2023. https://doh.gov.ph/covid19tracker U.S. Centers for Disease Control and Prevention. Understanding Exposure Risks. Published 2022. Accessed December 12, 2023. https://www.cdc.gov/coronavirus/2019-ncov/your-health/risks-exposure.html UpToDate. COVID-19: Management of adults with acute illness in the outpatient setting. Published 2023. Accessed December 12, 2023. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 182 6. 7. 8. 9. 10. https://www.uptodate.com/contents/covid-19-management-of-adults-with-acute-illness-in-the-outpatient-setting ?search=paxlovid&source=search_result&selectedTitle=2~52&usage_type=default&display_rank=1 Philippine Society for Microbiology and Infectious Diseases. Philippine COVID-19 Living Recommendations. Published 2023. Accessed December 12, 2023. https://www.psmid.org/philippine-covid-19-living-recommendations-3/ World Health Organization. WHO surveillance case definitions for ILI and SARI. Published 2014. Accessed December 12, 2023. https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring/case-definitions-for-ili-andsari Department of Health. COVID-19 FAQS. Published May 2021. Accessed December 12, 2023. https://doh.gov.ph/COVID-19/FAQs. World Health Organization. Clinical Management of COVID-19: living guideline. Published 2023. Accessed December 12, 2023. https://app.magicapp.org/#/guideline/j1WBYn/section/L0bmdE UpToDate. COVID-19: Respiratory care of the nonintubated hypoxemic adult (supplemental oxygen, noninvasive ventilation, and intubation). Published 2023. Accessed December 12, 2023. https://www.uptodate.com/contents/covid-19-respiratory-care-of-the-nonintubated-hypoxemic-adult-supplementa l-oxygen-noninvasive-ventilation-and-intubation?search=covid-19%20oxygen%20supplementation&source=search_ result&selectedTitle=1~150&usage_type=default&display_rank=1# Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 183 Dengue is a mosquito-borne infection transmitted by Aedes aegyptii or Aedes albopictus. The wide range of manifestations of dengue include asymptomatic infection, mild febrile illness, to multi-organ failure. Dengue is an important cause of morbidity and mortality in the country, with 220,705 cases reported in 2022, which is 182% higher than the cases in 2021, and a case fatality rate of 0.3%, which is 182%.1 Prevention, early detection, and timely administration of interventions, including simple and inexpensive hydration, are critical in reducing mortality and morbidity.2 Table 28. Dengue Continuum of Care Overview Dengue Overview Risk Factors ● ● ● Prevention Screening Diagnosis Treatment Environmental factors leading to increased dengue transmission: crowding/population density, human mobility, access to reliable water source, water storage practices Lack of vector control activities in the community Previous dengue infection - increased risk of developing severe disease Enhanced 4S Strategy (DOH Administrative 2018-0021) Avoidance of mosquito bites (See General Wellness and Preventive Measures for general guidance) Not applicable ● ● Minimum at Primary Care. Clinical diagnosis and risk assessment through history and PE; Dengue NS1 rapid diagnostic test (RDT) (first-line for confirmation); Dengue IgM/IgG RDT (alternative) First-line for dengue without warning signs: oral rehydration solution Adjunctive therapy: papaya (Carica papaya) leaf extract or juice preparations Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 184 Signs and Symptoms ● ● ● Suspect Dengue infection in a patient presenting with fever plus any two of the following3,4: ○ Nausea/vomiting ○ Rash ○ Headache, eye pain, muscle ache, or joint pain ○ Leukopenia ○ Positive tourniquet test Dengue with warning signs of severe infection includes the clinical presentation above and in addition of any of the following: ○ Abdominal pain or tenderness ○ Persistent vomiting ○ Clinical Fluid accumulation ○ Mucosal bleeding ○ Lethargy or restlessness ○ Hepatomegaly of > 2 cm ○ Increase in hematocrit concurrent with rapid decrease in platelet count Severe dengue infection includes infection with at least one of the following: ○ Severe plasma leakage leading to: shock; fluid accumulation with respiratory distress ○ Severe bleeding (as evaluated by clinician) ○ Severe organ involvement: AST or ALT ≥ 1000 units/L; impaired consciousness; organ failure Screening ● Not applicable Diagnostic Tests ● Minimum at primary care. Perform complete history taking and physical examination in all patients presenting with symptoms of Dengue. ○ Assess the following clinical parameters to determine if the patient should be referred to a hospital for inpatient management (Strong recommendation5): ■ Signs and symptoms: ● Vomiting/persistent vomiting ● Abdominal pain/tenderness ● Lethargy/restlessness ● Mucosal bleeding ● Impaired consciousness Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 185 Diagnostic Tests ● ● ● Hepatomegaly ● Acute renal failure (e.g., Urine Output <0.5 mg/kg/hr) ■ Presence of comorbidities: ● Pregnancy ● Obesity ● Others (cardiac, renal, hematologic, pulmonary) ○ Perform NS1 rapid diagnostic test (RDT) to confirm the diagnosis of dengue infection in individuals presenting within at least 3 days of symptom onset (Strong recommendation5). ■ Alternative: Request for combined Dengue NS1/IgM/IgG RDT to confirm the diagnosis, if available (Strong recommendation5). ■ If the patient presents more than 5 days from the onset of symptoms, request for Dengue IgM/IgG RDT (Strong recommendation5). Additional tests at baseline. Request for CBC with platelet count, liver function tests (AST, ALT) , and coagulation tests (PT, PTT). ○ Consider transferring patient for in-hospital management if any of the following laboratory parameters are present (Weak recommendation5): ■ Increased hematocrit with or without decrease in platelet count ■ Elevated transaminases ■ Impaired PT or PTT ■ Thrombocytopenia Tests for monitoring. Consider requesting CBC daily or every 3 days to monitor disease progression, as clinically indicated (Good Practice Statements5): ○ Depending on volume status, urine output, temperature, ability to tolerate feeding, presence of warning signs ○ Discontinue CBC monitoring when the patient is already in the recovery phase (e.g., increasing platelet count trends, 48 hours afebrile, adequate urine output, and improved sense of well-being/appetite). Treatment ● ● First-line therapy. Give oral rehydration solution (ORS) to all patients with probable or confirmed dengue fever.5 Adjunctive therapy. ○ Consider giving papaya (Carica papaya) leaf extract or juice preparations as a supplement ○ to standard therapy (Strong recommendation5). ○ Avoid giving the following: ■ Acid suppressants (Strong recommendation - Against5) ■ Guava (Psidium guajava) preparations (Strong recommendation - Against5) ■ Tawa-tawa (Euphorbia hirta) preparations (Weak recommendation - Against5) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 186 Referral ● ● Refer patients with confirmed or suspected Dengue to a hospital for inpatient management if the following danger/warning signs are present: ○ Vomiting/persistent vomiting ○ Abdominal pain/tenderness ○ Lethargy/restlessness ○ Mucosal bleeding ○ Impaired consciousness ○ Hepatomegaly ○ Acute renal failure (e.g., Urine Output <0.5 mg/kg/hr) ○ Increased hematocrit with or without decrease in platelet count ○ Elevated transaminases ○ Impaired PT or PTT ○ Thrombocytopenia Ensure IV access is present and provide IV fluid resuscitation in patients with confirmed or suspected hypotension or in shock while awaiting or facilitation transfer. References 1. 2. 3. 4. 5. Philippine Star. Philippines logs 220,705 dengue cases in 2022. Published January 17, 2023. Accessed December 16, 2023. https://www.philstar.com/nation/2023/01/17/2238093/philippines-logs-220705-dengue-cases-2022 World Health Organization. Handbook for clinical management of dengue. Published 2012. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789241504713 World Health Organization. Dengue guidelines, for diagnosis, treatment, prevention and control. Published 2009. Accessed December 16, 2023. https://www.who.int/publications/i/item/9789241547871 UpToDate. Dengue virus infection: Clinical manifestations and diagnosis. Published 2022. Accessed December 16, 2023. https://www.uptodate.com/contents/dengue-virus-infection-clinical-manifestations-and-diagnosis?search=severe%20dengue&sour ce=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 Department of Health. Clinical Practice Guideline on the Diagnosis, Management and Prevention of Dengue for Adult and Pediatric Filipinos. Published 2023. Accessed December 16, 2023. https://drive.google.com/file/d/1dsYIHm4UibfyP7FyFJeWsRQ5jXMZZNJp/view Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 187 Human Immunodeficiency Virus - Acquired Immunodeficiency Syndrome (HIV AIDS) is a retrovirus that destroys cell-mediated immunity, leading to immunodeficiency. It is usually acquired through sexual intercourse, exposure to infected blood, or perinatal transmission. It remains a major global public health issue, with countries like the Philippines reporting increasing trends in new infections.1,2 Incidence has risen to 411% from 2012 to 2023, with the increase in cases noted among the 15 - 24 year old age group.1 The Philippines has yet to meet its target on viral load suppression, with the country reaching 94% in 2021 (DOH, 2021). By 2025, 95% of all people living with HIV (PLHIV) should have a diagnosis, 95% of those should be taking lifesaving antiretroviral treatment (ART) and 95% of PLHIV on treatment should achieve a suppressed viral load for the benefit of the person’s health and for reducing onward HIV transmission.2 This section contains updated recommendations on effective health technologies across the continuum of care to achieve this target. Table 29. HIV-AIDS Continuum of Care Overview HIV-AIDS Overview Risk Factors Prevention Screening Diagnosis Treatment Men who have sex with men Transgender women and heterosexual men Women who have sexual partners with undiagnosed or untreated HIV infection People who inject drugs (PWID) Safe and responsible sexual and reproductive health practices (See General Wellness and Preventive Measures for general guidance and Family Planning Section for Barrier method and other pericoital contraceptives ) ● Antigen/antibody immunoassays ● Rapid diagnostic test kit Minimum at Primary Care. Combinations of antigen/antibody immunoassays or rapid diagnostic test kit First-line: ● Dolutegravir (DTG) - based regimens with nucleoside reverse transcriptase inhibitor (NRTI) backbones ● Efavirenz with NRTI backbone Second line: ● Boosted protease inhibitors in combination with an optimized NRTI backbone ● DTG in combination with an optimized NRTI backbone of previously on a non-DTG regimen ● ● ● ● ● Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 188 Signs and Symptoms ● ● Primary HIV infection may be asymptomatic or cause nonspecific symptoms.3 Consider HIV infection on adults at risk for HIV (among men who have sex with men, transgender women and heterosexual men, women who have sexual partners with undiagnosed or untreated HIV infection, sharing of infected needles for PWID, presenting with the following3, 4;: ○ Constitutional symptoms (e.g. fever, fatigue, and myalgia), ○ Adenopathies (i.e. axillary, cervical, and occipital nodes) ○ Oropharyngeal findings (e.g. sore throat with ulcers) ○ Gastrointestinal symptoms (e.g. nausea, diarrhea, anorexia, weight loss) ○ Neurologic findings (e.g. headache) ○ Generalized rash (i.e. pink to red macules) Screening ● Encourage voluntary HIV testing, especially among adults at risk . Written informed consent from the person taking the test must be obtained before HIV testing.5 ○ Screen adults for HIV infection with approved antigen/antibody immunoassays or rapid , diagnostic test kits. (Strong recommendation 6 7) ● HIV self-testing, with rapid diagnostic test kits, should be offered as an approach to HIV testing services (Strong recommendation11) Diagnostic Tests ● ● ● Minimum at Primary Care. Perform three consecutive tests using combinations of antigen/antibody immunoassays or rapid diagnostic tests to diagnose HIV infection.4 Gold Standard. Confirm negative or indeterminate results with HIV-1 nucleic acid test3,6 (Strong recommendation6) Additional Tests. Request for the following tests during initial patient visits, to assist in the selection of antiretroviral (ARV) or pre-exposure prophylactic drug regimens, and monitor for treatment failure or toxicity, as appropriate. Refer to higher level facilities for testing if these are not available at primary care. ○ Plasma HIV RNA (viral load) (Evidence A)8. ○ CD4 cell count for identifying advanced HIV disease (Evidence A)8 ○ Complete blood count; chemistry profile, including glucose, blood urea nitrogen and creatinine, liver enzymes and bilirubin, urinalysis, and serologies for hepatitis A, B, and C viruses (Evidence A)8 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 189 Diagnostic Tests Serum lipids at baseline Age-appropriate TB symptom screening4 Pregnancy testing4 Syphilis testing4 HLA-B*5701 test (if abacavir is being considered) (Evidence A)8 Genotypic drug-resistance testing (Evidence A)8 For patients who have HIV RNA levels <1,000 copies/mL, viral amplification for drug resistance testing should still be performed; however, it may not always be successful (Evidence B)8 ○ Depression screening for adults living with HIV using validated screening tools (conditional recommendation)4. Clinical Staging. Classify diagnosed patients according to the WHO clinical staging of HIV to guide management9 Monitoring. Refer to Section 4.7 of the WHO Consolidated Guidelines for monitoring the response to ARV.4 ○ ○ ○ ○ ○ ○ ○ ● ● Treatment ● Pharmacologic Therapy. Offer antiretroviral treatment (ART) to all patients diagnosed to have HIV infection after thorough clinical and laboratory evaluation.4 ○ First-line. Offer the following first-line regimens to eligible patients (strong recommendation). ■ Tenofovir Disoproxil Fumarate (TDF) + lamivudine (3TC) + Dolutegravir (DTG) 300 mg once daily, 150 mg twice daily or 300 mg once daily, 50 mg once daily ■ TDF + Emtricitabine (FTC) + DTG 300 mg once daily, 200 mg once daily, 50 mg once daily ■ TDF + 3TC (or FTC) + EFV 400 mg, 300 mg once daily, 150 mg twice daily or 300 mg once daily, 400 mg once daily ■ Second Line. Offer the following second-line regimens if the patient manifests with symptoms of drug toxicity, adverse reactions, or treatment failure with first-line regimens: boosted protease inhibitors in combination with an optimized nucleoside reverse-transcriptase inhibitor backbone (Strong recommendation); DTG in combination with an optimized nucleoside reverse-transcriptase inhibitor backbone of previously on a non-DTG regimen (Conditional recommendation)4 ● Adults on TDF + 3TC (or FTC) + DTG be shifted to Zidovudine (AZT) + 3TC + Atazanavir/ritonavir [(ATV/r) or Lopinavir/ritonavir (LPV/r)] or AZT + 3TC + darunavir/ritonavir (DRV/r) [or raltegravir (RAL) + LPV/r)] ● Adults on TDF + 3TC (or FTC) + EFV be shifted to AZT + 3TC + DTG or AZT + 3TC + ATV/r (or LPV/r or DRV/r) in cases of clinical or immunological failure or non-suppression of viral load (viral load >1000 copies/mL) ● Adults on AZT + 3TC +EFV be shifted to TDF + 3TC (or FTC) + DTG or TDF + Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 190 Treatment 3TC (or FTC) + ATV/r (or LPV/r or DRV/r) Start ART as soon as possible within two weeks of initiating TB treatment, regardless of CD4 cell count (Strong recommendation).4 ■ Immune reconstitution inflammatory syndrome (IRIS) is a paradoxical inflammatory syndrome occurring within 4 to 8 weeks following ART initiation among people living with HIV newly started on ART, after re-initiation of ART, or after a change to a more effective ART regimen in patients who fail to achieve viral suppression10. ● Symptoms depend on the existing opportunistic infection, but patients responding to TB treatment may have worsening of pulmonary symptoms, X-ray findings that suggest worsening of TB disease, enlarging lymph nodes causing airway obstruction, or meningeal symptoms. ● IRIS is usually accompanied by an increase in CD4 count and/or a rapid decrease in viral load ● Monitor the presence of symptoms of tuberculosis or other opportunistic infections (e.g. cryptococcal infections, herpes zoster, hepatitis B or C, Kaposi sarcoma) ● Initiate appropriate treatment for the underlying condition and continue ART. Nonpharmacologic Interventions. ○ Offer counseling for adults living with HIV on the potential benefits and risks of disclosing their HIV status to others and empowered and supported to determine whether, when, how and to whom to disclose (Conditional recommendation)4 ○ Inform adults living with HIV on the Undetectable = Untransmittable (U=U) principle, whereby maintaining a plasma HIV RNA (viral load) of <200 copies/mL, including any measurable value below this threshold value, with ART prevents sexual transmission of HIV to their partners (Evidence A)8 ○ Advise mothers living with HIV to breastfeed for at least 12 months and continue breastfeeding for up to 24 months or longer (similar to the general population) while being fully supported for ART adherence (Strong recommendation)4 ○ Advise the correct and consistent use of condoms with condom-compatible lubricants (Strong recommendation)4 ○ ● Chemoprophylaxis ● Pre-exposure prophylaxis ○ Start pre-exposure prophylaxis (PrEP) containing TDF [(e.g (TDF 300 mg + FTC 200 mg; tenofovir alafenamide-emtricitabine (TAF-FTC)] daily for 90 days for adults at substantial risk for HIV infection, as applicable, following the 2+1+1 approach before each sexual activity (strong recommendation). It should be taken as long as the risk of infection exists.4;11 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 191 Chemoprophylaxis Offer the dapivirine vaginal ring for adult women at substantial risk of HIV infection, to be worn for 28 days (Conditional recommendation)4 ○ Offer long-acting cabotegravir 600 mg IM once monthly for two doses (3 mL) (Conditional recommendation)12;11 Post-exposure prophylaxis. ○ Start adults on a TDF + 3TC + DTG or TDF + FTC + DTG regimen within 72 hours after exposure to HIV for 28 days (Strong recommendation)4;13 ○ Offer ATV/r, DRV/r, LPV/r and RAL as alternative third drug options for PEP (Conditional recommendation).4 Prophylaxis for opportunistic infections ○ Provide co-trimoxazole prophylaxis to all people living with HIV with active TB disease regardless of CD4 cell count (Strong recommendation)4 ○ Provide TPT for PLHIV without active TB disease (Strong recommendation)4 ○ ● ● Referral ● Refer people living with HIV4 to higher levels of care or qualified healthcare providers if they: ○ have advanced HIV disease (defined as WHO stage 3 or 4 or a CD4 count <200 cells/mm3). ○ are in need of social support services for palliative care. Palliative Care ● ● Administer pain medications appropriate for the adult’s condition.14 Provide appropriate basic palliative for people living with HIV, as appropriate. All health–care providers should be trained in at least basic palliative care working at the primary care or community level who care for people living with HIV4 References 1. 2. 3. 4. 5. 6. Department of Health. HIV/AIDS & ART Registry of the Philippines. Epidemiology Bureau. Published 2023. https://www.ship.ph/wp-content/uploads/2023/06/EB_HARP_March_AIDSreg2023.pdf World Health Organization. HIV and AIDS. 2023. https://www.who.int/news-room/fact-sheets/detail/hiv-aids UpToDate. Acute and early HIV infection: Clinical manifestations and diagnosis. 2023. https://www.uptodate.com/contents/acute-and-early-hiv-infection-clinical-manifestations-and-diagnosis?search=hiv&source=searc h_result&selectedTitle=1~150&usage_type=default&display_rank=1 World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. 2021. https://www.who.int/publications/i/item/9789240031593 Republic Act No. 11166, “Philippine Aids Prevention and Control Act of 1998” U.S. Preventive Services Task Force. Human Immunodeficiency Virus (HIV) Infection: Screening. 2019. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/human-immunodeficiency-virus-hiv-infection-screening#f Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 192 7. 8. 9. 10. 11. 12. 13. 14. ullrecommendationstart University of the Philippines National Institutes of Health - Institute of Clinical Epidemiology. Philippine Guidelines on Periodic Health Examination (PHEX) Phase 3: Screening for Infectious Diseases. Published 2023. https://drive.google.com/file/d/1up5YnRyy6S5YpTsGgRoZHo4XDCOSrjR7/view HHS Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. 2023. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/adult-adolescent-arv/guidelines-adult-adolescent-arv.pdf World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach, 2nd Ed. 2016. https://www.who.int/publications/i/item/9789241549684 Brust et al. Management of Immune Reconstitution Inflammatory Syndrome (IRIS). 2021. https://www.hivguidelines.org/guideline/hiv-iris/ UpToDate. HIV pre-exposure prophylaxis. 2023. https://www.uptodate.com/contents/hiv-pre-exposure-prophylaxis?search=hiv%20pre%20exposure%20prophylaxis&source=search _result&selectedTitle=1~150&usage_type=default&display_rank=1# World Health Organization. Guidelines on long-acting injectable cabotegravir for HIV prevention. 2022. https://www.who.int/publications/i/item/9789240054097 UpToDate. Management of nonoccupational exposures to HIV and hepatitis B and C in adults. 2023. https://www.uptodate.com/contents/management-of-nonoccupational-exposures-to-hiv-and-hepatitis-b-and-c-in-adults?search=hi v%20post%20exposure%20prophylaxis&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2# World Health Organization. WHO Model List of Essential Medicines for Children - 8th list. 2021. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.03 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 193 Infectious Diarrhea The burden of diarrheal diseases is estimated to be 3.6% of the total DALYs worldwide. Based on the Field Health Information (DOH) report, acute watery diarrhea (AWD) ranked seventh among the top leading causes of morbidity, affecting 76.3 per 100,000 population.1 In resource-limited settings, crowding, poor sanitation, and microbiologic origins such as Campylobacter, Salmonella, Shigella, Escherichia, Vibrio, and human immunodeficiency virus are the risk factors and causative agents of infectious diarrhea, respectively.2 Appropriate prevention, diagnosis, and management of infectious diarrhea are necessary to reduce the risk of outbreaks, prevent complications, and prevent the development of antimicrobial resistance. Table 30. Infectious Diarrhea Continuum of Care Overview Infectious Diarrhea Overview Risk Factors Prevention Screening Diagnosis Treatment Nonpharmacologic Management Consumption of contaminated food or water Travel to an endemic area or an area with outbreak Observance of hand hygiene and infection control practices, hygiene and sanitation in the household and community, in line with the Water, Sanitation and Hygiene (WASH) Strategy (See General Wellness and Preventive Measures) Immunization for select groups Salmonella screening in food handlers who had a recent bout of diarrhea Minimum at primary care: History-taking and PE, including assessment of degree of dehydration Gold Standard: Stool culture only for severe cases of acute diarrhea and only during outbreaks of enteric infections First Line: Adequate oral hydration with reduced osmolarity oral rehydration salts/solutions (ORS) Adjunctive therapy: Racecadotril Limit antibiotic use to suspected or confirmed cases of Cholera, Shigella, Non-typhoidal Salmonellosis, and Amoebiasis Hand hygiene Avoidance of open defecation Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 194 Signs and Symptoms ● Suspect acute infectious diarrhea among adult patients presenting with the following: ○ a passage of 3 or more loose, watery, or bloody stools within 24 hours that may be accompanied by any of the following: nausea, vomiting, abdominal pain, or fever. (Strong Recommendation1) Screening ● Salmonella. Consider screening food handlers for Salmonella after a bout of acute diarrhea. (Good Practice Statement1) Diagnostic Tests ● ● ● ● Minimum at primary care. Perform history-taking and physical examination. ○ Assess for dehydration. Ascertain and classify the degree of dehydration among adults with acute infectious diarrhea during physical examination by assessing the following: (Strong Recommendation1) ■ Mild dehydration: With or without fatigue or thirst; normal BP, respiratory rate (RR), pulse rate (PR), warm extremities, alert, moist oral mucosa, normal skin turgor and capillary refill time (CRT) ≤ 2 seconds, urine output (UO) ≥ 0.5 mg/kg/hr, body weight (BW) reduction 3-5% in ≤ 7 days OR increase of 3-5% BW in ≤ 7 days after rehydration ■ Moderate dehydration: With fatigue, thirst, sunken eyes, orthostatic hypotension, increased RR (21-25), increased pulse rate (≥ 100), cold, clammy skin, lethargy, dry oral mucosa, mild-moderate muscle weakness, skin turgor >2 seconds and CRT >2 seconds, UO <0.5 ml/kg/hr, BW reduction of >5% ■ Severe dehydration: Clinical parameters similar to moderate dehydration but accompanied by hypovolemic shock (BP <90/60 mmHg), tachypnea (RR ≥ 25), faint or thready pulses, coma or stupor, and severe muscle weakness Request for stool examination only when suspecting parasitic infection or in the presence of bloody diarrhea. (Strong Recommendation1) Gold Standard: Stool Culture. Request stool cultures only for severe cases of acute diarrhea and only during outbreaks of enteric infections, within 3 days from the symptom onset and before administration of antibiotics. (Strong Recommendation1) Additional laboratory tests. Consider requesting for additional tests depending on clinical indication or suspicion: Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 195 Diagnostic Tests ○ ○ When suspecting complications of acute diarrhea such as moderate to severe dehydration, acute kidney injury, or electrolyte imbalance: CBC, Urinalysis, Serum Electrolytes, BUN, Creatinine, serum bicarbonate (Strong Recommendation1) ■ Increased urine specific gravity (≥1.010), increased urine osmolality (>800 mosm/kg), increased serum osmolality (≥295 mosm/kg), increased BUN/creatinine ratio (>20), Metabolic Acidosis (pH<7.35, HCO3 <22 mmol/L). During suspected outbreaks of cholera or shigella: rapid diagnostic tests (Strong Recommendation1) Treatment ● ● ● ● ● First line therapy. Give ORS 1.5 to 2 times the estimated volume deficit to adult patients with mild diarrhea. (Strong Recommendation1) ○ If commercial ORS is not available/accessible, teach patients and their caregivers to prepare homemade ORS: 4-5 teaspoons sugar plus 1 teaspoon salt in 1 liter of clean drinking water (sterilized or boiled) When not to give antibiotics. Empiric antibiotic treatment is not recommended for adults with acute infectious diarrhea with the following clinical features: mild to moderate dehydration, non-bloody stools, and symptoms less than 3 days. (Strong Recommendation1) When to give antibiotics. Prescribe the following antibiotics to adults suspected or confirmed to have acute infectious diarrhea caused by the following organisms: ○ Cholera: prescribe Azithromycin 1 gram tablet orally as single dose or Ciprofloxacin 500 mg tablet orally twice a day for 3 days (Strong Recommendation1) ○ Shigella: prescribe Azithromycin 1 gram tablet orally as single dose or Ciprofloxacin 500 mg tablet orally twice a day for 5 days (Strong Recommendation1) ○ Non-Typhoidal Salmonella: prescribe Ciprofloxacin 500 mg tablet orally twice a day for 5 days (Strong Recommendation1) ○ Amoebiasis: Prescribe Metronidazole 500-750 mg tablet orally three times a day for 10 days (Strong Recommendation1) Supportive Therapy. Consider giving Racecadotril 100 mg capsule 3 times a day to adults as adjunctive therapy to shorten duration of diarrhea. (Weak Recommendation1) Non-pharmacologic management: ○ Hygiene and sanitation. Advise all patients and household members regarding the following: ■ Observe hand hygiene to reduce the transmission of organisms that cause diarrhea. (Strong Recommendation1) ■ Avoid open defecation practices. (Strong Recommendation1) Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 196 Referral ● Refer to higher level of care patients with acute infectious diarrhea with the following (Strong Recommendation1): ○ Poor tolerance to oral rehydration ○ Moderate to severe dehydration ○ Acute kidney injury ○ Electrolyte abnormality ○ Unstable comorbid conditions ○ Poor nutritional status ○ Unique social circumstances ○ Elderly or at risk of fluid overload (e.g., heart failure, kidney disease) References 1. 2. Department of Health. Clinical Practice Guidelines on the Management of Acute Infectious Diarrhea in Children and Adults. Published 2019. Accessed December 14, 2023. https://drive.google.com/drive/folders/1m-e_DkAucR9O_U58IrK2nCVnhYT3bFj9 UpToDate. Approach to the adult with acute diarrhea in resource-limited settings. Published 2023. Accessed December 14, 2023. https://www.uptodate.com/contents/approach-to-the-adult-with-acute-diarrhea-in-resource-limited-settings?search=infectious%2 0diarrhea&source=search_result&selectedTitle=6~150&usage_type=default&display_rank=5#H77501856 Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 197 Leptospirosis is a zoonosis coming from direct or indirect contact with the pathogenic spirochetes of the genus Leptospira from domesticated and wild animals. Sources of infection come from water, soil and/or surfaces contaminated with infected urine or tissues. Upon contact, the bacteria may enter through cuts and abrasions in the skin or mucosal surfaces; the conjunctiva; or by inhalation of droplets or aerosols of fluid containing leptospires. After penetrating intact mucous membranes or epithelium, leptospires enter the bloodstream and are rapidly carried to all parts of the body.1 In the Philippines, leptospirosis contributes to around 0.2% causes of morbidity in 2020.2 Leptospirosis tends to occur frequently in urban flood-prone areas such as Metro Manila. More and more frequent outbreaks of leptospirosis in the Philippines are expected to occur with increasing number of flood prone-areas and increasing occurrence of flooding due to heavy rainfall, rapid urbanization (dramatic increase in populations), deforestation, poor road and disaster risk reduction infrastructures among many other factors1. Table 31. Leptospirosis Continuum of Care Overview Leptospirosis Overview Risk Factors Prevention Screening Diagnosis Pharmacologic Treatment Wading or swimming in floods- with or without wounds Ingestion of flood/ contaminated water Residing in a flood-prone area Contact with animal fluids especially carcass Avoid wading/swimming in floods, ingestion of flood/contaminated water (See General Wellness and Preventive Measures) Pre-and post-exposure prophylaxis: ● Pre-exposure prophylaxis: Doxycycline 200 mg orally once a week, to begin 1 to 2 days before exposure and continued throughout the period of exposure, for short-term exposures ● Post-exposure prophylaxis. Mild Risk: Doxycycline 200 mg single dose, immediately within 24 to 72 hours from exposure Moderate Risk: Doxycycline 200 mg once daily for 3-5 days to be started immediately within 24 to 72 hours from exposure High Risk: Doxycycline 200 mg once weekly until the end of exposure Not applicable Minimum at primary care: Clinical history-taking, physical examination. Gold Standard: PCR or culture of blood during the first 4 to 6 days of symptoms, or urine after the first week of illness First Line: Doxycycline 100 mg tab twice daily orally for 7-10 days Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 198 Signs and Symptoms Suspect leptospirosis among patients presenting with: ● Acute febrile illness of at least 2 days, and ● With two or more of the following symptoms: myalgia, calf tenderness, conjunctival suffusion, chills, abdominal pain, headache, jaundice, or oliguria, and ● With risk factors including: wading or swimming in floods, with or without wounds, ingestion of flood/ contaminated water, residing in a flooded area, contact with animal fluids especially carcass.1 Screening ● Not applicable Diagnostic Tests ● ● ● Minimum at primary care. Perform thorough clinical history-taking and physical examination. A high index of suspicion and early recognition is needed for initiation of treatment to prevent complications and mortality.1 ○ Classify leptospirosis as anicteric (mild) or moderate to severe(icteric): ■ Mild (anicteric) Leptospirosis: stable vital signs, anicteric sclera, no jaundice, with good urine output, no meningismus, no dyspnea, no tachypnea, no bleeding, no hemoptysis, not in sepsis, and can take oral medications ■ Moderate-Severe (Icteric) Leptospirosis: unstable vital signs, with jaundice, icteric sclera, abdominal pain, nausea, vomiting and diarrhea, with oliguria or anuria, bleeding, meningismus, with sepsis, altered mental status, hemoptysis or difficulty of breathing Gold Standard. Request for PCR or culture of appropriate clinical specimens depending on the timing of the illness as follows: blood during the first 4 to 6 days of symptoms, or urine after the first week of illness3. Confirmation with the gold standard may not always be available at primary care; hence, a high index of clinical suspicion is necessary to prompt appropriate management. Additional laboratory tests at primary care. ○ Request for Complete Blood Count with Platelet Count, Urinalysis, Blood Urea Nitrogen, Creatinine, ALT and AST among adults with mild leptospirosis1. ○ Consider requesting a serologic test (e.g. microscopic agglutination test) to confirm ○ leptospiral infection if PCR and culture are not available.1 Other tests should be requested for inpatients or patients with complications, depending on the clinical indication. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 199 Treatment ● ● ● First line therapy. Doxycycline 100 mg tab twice daily orally for 7-10 days 1,4 Alternative. Consider either of the following antibiotics as an alternative to the first line management if with contraindications (e.g., allergy) to first-line therapy: ○ Amoxicillin 500mg four times a day or 1 g every 8 hours orally1 ○ Azithromycin 1g initially followed by 500 mg once a day for the next 2 days or 500 mg once a day for 3 days 1,4 Treatment in Pregnancy. For pregnant adults, consider prescribing azithromycin 500 mg orally once daily for three days or amoxicillin (25 to 50 mg/kg in three equally divided doses for seven days.4 Chemoprophylaxis ● ● Pre-exposure prophylaxis ○ Consider prescribing Doxycycline 200 mg orally once a week, to begin 1 to 2 days before exposure and continued throughout the period of exposure, for adults with short-term exposures such as those who intend to visit highly endemic areas including travelers, soldiers, or adults who engage in water-related recreational and occupational activities, disaster relief workers deployed to flooded or post-typhoon areas 1,5. Post-exposure prophylaxis. This also requires prior consultation with a physician. Depending on the risk exposure, consider prescribing the following1,5: ○ Mild Risk: adults with single exposure, non-mucosal or no breaks in the skin: Doxycycline 200 mg single dose, immediately within 24 to 72 hours from exposure ○ Moderate Risk: adults with mucosal exposure, presence or wound: Doxycycline 200 mg once daily for 3-5 days to be started immediately within 24 to 72 hours from exposure ○ High Risk: adults with repeated or continuous exposure: Doxycycline 200 mg once weekly until the end of exposure1 ○ Pregnant women: Amoxicillin 500 mg/tablet - 1 tablet twice a day for 3 days. If allergic to amoxicillin, may give erythromycin 250 mg/tablet twice a day for 3 days5. Referral ● Refer patients suspected of having moderate to severe (icteric) leptospirosis who present with the following signs and symptoms to higher level of care1 ○ Unstable vital signs ○ Jaundice/ icteric sclerae ○ Abdominal pain, nausea, vomiting or diarrhea ○ Oliguria or anuria Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 200 Referral ○ ○ ○ ○ ○ Bleeding Meningismus/ meningeal irritation/ nuchal rigidity, Altered mental status, seizures Difficulty of breathing or hemoptysis Sepsis First Aid Measures and Basic Emergency Care ● Administer the following first aid measures to adults prior to referral to next level of care1: ○ Loading dose of Penicillin G 1.5 million units IV divided in 6 hours or Ceftriaxone 1gm IV ○ Fluid resuscitation, as warranted, to adults using balanced crystalloids/ NSS at 20ml/kg/h or 500ml of crystalloids within 15- 30 minutes References 1. 2. 3. 4. 5. Department of Health. DOH Guidelines for Leptospirosis for Hospitals. Published 2019. Accessed December 14, 2023. https://drive.google.com/drive/folders/1pxQDWu3H1rmtGlXhJB2G1ZA1x09DREgk Department of Health. 2020 Philippine Health Statistics. Published 2020. Accessed December 14, 2023. https://doh.gov.ph/sites/default/files/publications/2020PHS_FINAL_PDF.pdf UpToDate. Leptospirosis: Epidemiology, microbiology, clinical manifestations, and diagnosis. Published 2023. Accessed December 14, 2023. https://www.uptodate.com/contents/leptospirosis-epidemiology-microbiology-clinical-manifestations-and-diagnosis?search=l eptospirosis&source=search_result&selectedTitle=1~84&usage_type=default&display_rank=1#H6 UpToDate. Leptospirosis: Treatment and prevention.Published 2023. Accessed December 14, 2023. https://www.uptodate.com/contents/leptospirosis-treatment-and-prevention/print Department of Health. DOH DM 2023-0309: Guidelines on the Prevention, Control, Management, and Surveillance of Leptospirosis.Published 2023. Accessed December 14, 2023. https://drive.google.com/file/d/1rjEaSd-2_wWckYQipCJPRtxnn5v55cQe/view Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 201 Tinea Infection is a fungal infection more commonly called “ringworm” due to its classic appearance of circular, erythematous, pruritic rash. Fungal skin diseases contributed to about 0.17% of total DALYs among Filipinos in 2019.1 Tinea infection has a specific name depending on the part affected, such as tinea pedis for foot, tinea cruris for groin, tinea capitis for scalp, and tinea corporis for other parts of the body.2 Though tinea infection is not included in the WHO fungal priority pathogens list 20223, it is common in the country. In a study conducted by Handog, E. and Dayrit, J. in 20054, it is found that fungal infections rank as second leading cause of dermatology consultation with tinea corporis (22.63%), tinea cruris (16.7%), and tinea pedis (16.38%) belonging to the most frequently encountered cases. Table 32. Tinea Infection Continuum of Care Overview Tinea Infection Overview Risk Factors ● ● ● ● ● ● ● Weakened immune system (e.g. diabetes) Use of public showers or locker rooms Athletes particularly those in contact sports Wearing tight shoes Excessive sweating Obesity Close contact with infected human or animal Prevention Screening Diagnosis Observance of proper personal hygiene (See General Wellness and Preventive Measures) Not applicable. Minimum at Primary Care. History and physical examination Gold standard. Fungal culture. Pharmacologic Treatment First Line: topical antifungal once or twice a day for 1-2 weeks Alternative: oral antifungal for extensive lesions, or refractory response to topical antifungal Non-pharmacologic management ● ● ● Avoid sharing towels or clothes. Avoid occlusive footwear or clothing Avoid walking barefoot in pools or public showers. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 202 Signs and Symptoms ● Consider tinea infection among adults presenting with pruritic rashes on various areas of the body such as5,6: ○ Tinea pedis: pruritic, erythematous and scaly lesions on the foot, usually on the interdigits appearing as maceration or scales between the toes and is often caused by walking barefoot in locker rooms, swimming pools or communal spaces, or by using occlusive footwear. ○ Tinea corporis: appearing as a pruritic, circular, erythematous patch with scales and with central clearing on various parts of the body, and is often transmitted by direct skin contact or fomites. ○ Tinea cruris: manifesting as pruritic, erythematous scaly patch with central clearing usually starting on the medial thigh and is more common among males, or those who sweat profusely, obese adults, with diabetes mellitus or adults with immunodeficiency. Diagnostic Tests ● ● ● Minimum at primary care ○ Diagnose tinea infections through history and physical examination of the affected areas5,6 Gold Standard ○ Consider requesting fungal culture to confirm the diagnosis of tinea among adults6 Additional Tests ○ Consider potassium hydroxide (KOH) preparation on skin scrapings from the affected areas.5,6 Treatment ● Pharmacologic Therapy ○ First line: Consider topical anti-fungal preparations once or twice a day for 1 to 2 weeks for localized infections6: ■ Azoles: ● Clotrimazole 1% cream, ointment, or solution ● Econazole 1% cream or foam ● Ketoconazole 2% cream, gel or foam ● Luliconazole 1% cream ● Miconazole 2% cream, ointment, solution, or powder ● Oxiconazole 1% cream or lotion ● Sertaconazole 2% cream Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 203 Treatment ● ● Sulconazole 1% cream or solution ■ Allylamines ● Naftifine 1% or 2% cream or gel ● Terbinafine 1% cream or spray solution ■ Benzylamine: Butenafine 1% cream ○ Alternative: Consider oral anti-fungal preparations for extensive lesions, or those with refractory response to topical anti-fungal6: ■ Terbinafine 250 mg tablet, 1 tablet daily for 1 to 2 weeks ■ Itraconazole 200 mg tablet twice a day for 1 week ■ Fluconazole 150 to 200 mg tablet once weekly for 2-6 weeks ■ Griseofulvin 250 mg tablet, 4 tablets a day for 4-8 weeks Nonpharmacologic ○ May advise adult patients with tinea to avoid sharing towels or clothes, avoid occlusive footwear or clothing, and avoid walking barefoot in pools or public showers.5,6 References 1. 2. 3. 4. 5. 6. Institute of Health Metrics and Evaluation. GBD Compare. Published 2019. Accessed December 15, 2023. https://vizhub.healthdata.org/gbd-compare/ U.S. Centers for Disease Control and Prevention. About Ringworm. Published 2021. Accessed December 15, 2023. https://www.cdc.gov/fungal/diseases/ringworm/definition.html World Health Organization. WHO fungal priority pathogens list to guide research, development and public health action. Published 2022. Accessed December 15, 2023. https://www.who.int/publications/i/item/9789240060241 Handog EB, Dayrit JF. Mycology in the Philippines, Revisited. Nippon Ishinkin Gakkai Zasshi. 2005;46(2):71-76. doi:https://doi.org/10.3314/jjmm.46.71 UpToDate. Dermatophyte (tinea) infections. Published 2023. Accessed December 16, 2023. https://www.uptodate.com/contents/dermatophyte-tinea-infections?search=tinea&source=search_result&selectedTitle=1~118& usage_type=default&display_rank=1#H2696183692 Kovitwanichkanont T, Chong AH. Superficial fungal infections. Australian Journal of General Practice. 2022;48(10). Accessed December 17, 2023. https://www1.racgp.org.au/ajgp/2019/october/superficial-fungal-infections Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 204 Tuberculosis, Pulmonary is a lung infection caused by Mycobacterium tuberculosis, which can be transmitted through the air by infected individuals, mainly through coughing. Pulmonary Tuberculosis (PTB) manifests in two disease states - latent tuberculosis infection (LTBI) and acute tuberculosis disease, with drug-resistant strains posing a global health challenge. In 2022, approximately 10.6 million people worldwide developed TB. Notably, the Philippines is one of the eight countries contributing to two-thirds of global TB cases. Although in contrast, the country, along with India and Indonesia, collectively accounted for ≥ 60% of the global reductions in the number of newly diagnosed TB in 2020 and 20211. PTB remains a priority public health problem and the goal is to align with the Sustainable Development Goals to reduce global TB incidence by 80% and a 90% reduction in TB deaths by 2030. However, the prevalence rate for the Philippines is still at 638 per 100,000 population in 2022. The country is aiming to contribute to the endeavors of reducing the prevalence rate globally to only less than 10 per 100,000 population in 20351. The scope of this section is limited to drug-susceptible and drug-resistant pulmonary tuberculosis and does not include specific management for the different forms of extrapulmonary TB. Table 32. Pulmonary Tuberculosis Continuum of Care Overview Pulmonary Tuberculosis Overview Risk Factors Prevention Screening Diagnosis Pharmacologic Treatment Structural risk factors: Urban poor/homeless communities, Geographically Isolated and Disadvantaged Areas (GIDA), Indigenous populations, Migrants, Refugees, Prisons and penitentiary institutions, Internally displaced and other marginalized groups Occupational risk factors: Current and former workers in workplaces with silica exposure, miners, Health care workers Clinical risk factors: TB prevalence in the general population is 100/100,000 population is higher, Untreated fibrotic lesions seen on chest x-ray, Diabetes mellitus, History of TB, Chronic lung disease, Smoking/vaping, Alcohol use disorder, Substance use disorder, Malnourishment, Pregnancy, Immunocompromising condition (e.g. organ transplant, renal failure, dialysis) Cough etiquette and respiratory hygiene (See General Wellness and Preventive Measures) Chemoprophylaxis: TB Preventive Treatment (TPT) to all eligible contacts of TB patients Minimum at primary care: Systematic screening using: symptom screen tool, chest x-ray or molecular WHO-recommended rapid diagnostic test, alone or in combination Alternative: Chest x-ray with computer-aided detection (CAD-AI) software, Xpert MTB/RIF Minimum at primary care: Sputum Xpert MTB/RIF or Xpert Ultra Gold Standard: TB culture with phenotypic drug susceptibility test (DST) First Line for Drug-susceptible Pulmonary TB: Regimen 1: 2HRZE/4HR comprised of: Isoniazid (H), Rifampicin (R), Ethambutol (E), Pyrazinamide (Z) First Line for Drug-resistant Pulmonary TB: Depending on the resistance patterns, regimen may vary as Standard Short All Oral Regimen (SSOR), Standard Long All Oral Regimen for fluoroquinolone susceptible (SLOR FQ-S), SLOR for fluoroquinolone resistance (SLOR FQ-R) that may be comprised of: Group A: Levofloxacin, Moxifloxacin, Bedaquiline, and Linezolid Group B: Clofazimine, and Cycloserine Group C: Ethambutol, Delamanid, Pyrazinamide, and Prothionamide Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 205 Signs and Symptoms ● Suspect pulmonary tuberculosis among adults with: ○ Any of the following symptoms: cough > 2 to 3 week’s duration or wheezing, lymphadenopathy, fevers, night sweats, unexplained weight loss, or ○ Relevant epidemiologic factors: history of prior TB infection or disease, known or possible TB exposure for at least 2 weeks, and/or past or present residence in or travel to an area where TB is endemic2. Screening ● ● Minimum at primary care. Consider conducting systematic screening using a symptom screen tool, and/or chest x-ray for adults with signs and symptoms, or those with the following risk factors (conditional recommendation)2: ○ Subpopulations with structural risk factors (urban poor communities, homeless communities, GIDA, indigenous populations, migrants, refugees, internally displaced persons and other marginalized groups) (conditional recommendation)3 ; ○ Adults living with HIV (strong recommendation)3; ○ Household contacts and other close contacts of individuals with TB disease (strong recommendation)3; ○ Prisons and penitentiary institutions (strong recommendation)3 ○ Current and former workers in workplaces with silica exposure (strong recommendation)3; and ○ In settings where the TB prevalence in the general population is at least 100/100,000 population, such as the Philippines, consider screening among adults with clinical risk factors for TB who are either seeking health care or who are already in care (conditional recommendation)3: ■ Untreated fibrotic lesions seen on chest x-ray ■ Diabetes mellitus (DM) ■ History of TB ■ Chronic lung disease ■ Smoking ■ Alcohol use disorder ■ Substance use disorder ■ Malnourishment ■ Pregnancy ■ Immunocompromising condition (e.g. organ transplant, renal failure, dialysis) ■ Health care workers Alternative screening tests. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 206 Screening ○ ○ Consider requesting chest x-ray with computer-aided detection (CAD-AI) software programs in place of human readers for interpreting digital chest x-rays as an alternative for screening and triage of TB disease for adults. (Conditional recommendation4) Consider requesting Xpert MTB/RIF as additional screening test for TB in high-risk groups (Conditional recommendation4) Diagnostic Tests ● ● ● Minimum at Primary care. Request for Sputum Xpert MTB/RIF or Xpert Ultra as initial diagnostic test for TB and rifampicin-resistance detection in sputum for adults. (Strong recommendation5) Gold standard. Consider requesting the TB confirmatory and gold standard, TB culture with phenotypic drug susceptibility test (DST) for the definitive diagnosis and drug resistance testing for TB2. Additional tests. The following may be requested when clinically indicated and/or when available programmatically: ○ Alternative tests. Consider requesting the following as alternative, as indicated: ■ AFB sputum smear microscopy and culture, if Chest X-ray is suggestive of TB in the lungs or airways2; ■ Sputum Truenat MTB or MTB Plus as an initial diagnostic test, alternative to smear microscopy or culture, for Adults with signs and symptoms of pulmonary TB. (Conditional recommendation5); ■ Loop-mediated isothermal amplification (TB-LAMP) as an alternative to sputum smear microscopy for diagnosing TB or a follow-on test to smear microscopy in adults (Conditional recommendation5); ○ Drug susceptibility testing. Consider requesting the following as additional or alternative test to culture-based phenotypic DST (Conditional recommendations5): ■ Sputum Truenat MTB-RIF Dx as an initial test for rifampicin resistance for adults with signs and symptoms of pulmonary TB and a Truenat MTB or MTB Plus positive result; ■ Low complexity NAAT for the detection of isoniazid and second-line TB agents resistance (Conditional recommendation); ■ Moderate complexity automated nucleic acid amplification test (NAAT) for detection of TB and resistance to rifampicin and isoniazid; ■ High complexity reverse hybridization-based NAATs for the detection of pyrazinamide resistance; ■ First-line line-probe assay (LPAs) for the detection of rifampicin and isoniazid resistance in adults with a sputum smear-positive specimen or a cultured isolate of Mycobacterium tuberculosis complex; ■ Second-line LPAs for the detection of fluoroquinolones and second-line injectable drug resistance in adults with confirmed MDR/RR-TB. Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 207 Diagnostic Tests ○ ○ ○ Consider requesting sequence-based testing such as pyrosequencing, Sanger sequencing, and next generation sequencing for adults with pulmonary TB to determine genetic identity of a particular mycobacterial mutation and predict drug resistance2. Consider requesting lateral flow urine lipoarabinomannan assay for HIV-positive adults in outpatient settings with signs and symptoms of TB or seriously ill, and irrespective of signs and symptoms of TB and with a CD4 cell count of less than 100 cells/mm3 (Conditional recommendation5). Drug Toxicity Monitoring ■ Conduct liver function tests (serum transaminases and bilirubin) as baseline prior to initiation of treatment, and monthly evaluation of symptoms of hepatitis among adults, and pregnant women with TB disease or TB infection2. ■ Assess baseline platelet count and serum creatinine of adult patients receiving rifampin, in addition to the hepatic enzyme evaluation prior to the initiation of therapy6. ■ Consider conducting periodic monitoring of adverse effects of antituberculous drugs through the following tests, as appropriate7: ● Creatinine clearance ● Physical Examination maneuvers such as but not limited to, visual acuity and red-green color discrimination, and brief peripheral neuropathy screening. ● Renal function ● Electrolytes (potassium, calcium, magnesium) ● Audiology testing and evaluation for tinnitus and vestibular toxicity ● Thyroid stimulating hormone ● Psychiatric symptom monitoring (depression and mood changes). Refer to the Screening for Anxiety, and Depression section. ● Complete blood count ● Electrocardiogram Treatment for Active Disease ● Pharmacologic Therapy. ○ First-line regimens for drug-susceptible TB Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 208 Treatment for Active Disease Give the six-month treatment Regimen 1: 2HRZE/4HR for all adults with drug-susceptible TB (Strong recommendation8) with either of the following eligibility criteria9: ● New or retreatment with the following Xpert results: ○ MTB, RIF Sensitive, ○ MTB, RIF indeterminate ● New pulmonary TB patient with positive SM/TB LAMP or clinically diagnosed, and: ○ Xpert not done ○ Xpert result is MTB not detected ■ Recommended daily doses for 2HRZE/4HR in adults8;10: ● Isoniazid (H): 4 - 6 mg/kg, 300 mg formulation ● Rifampicin (R): 8 - 12 mg/kg, 300 mg formulation ● Ethambutol (E): 15 - 25 mg/kg, 400 mg formulation ● Pyrazinamide (Z): 20 - 30 mg/kg, 500 mg formulation First-line regimens for drug-resistant TB ■ Depending on the TB resistance patterns, give the following treatment regimen for adults with confirmed drug-resistant TB: ● Regimen 3: Standard Short All Oral Regimen (SSOR) for MDR-TB and RR-TB eligible to SSOR, give, 4-6 months: Linezolid (Lfx) - Bedaquiline (Bdq) - Clofazamine (Cfz) - Prothionamide (Pto) - Ethambutol (E) Pyrazinamide (Z) - High dose Isoniazid (HdH) [Bdq shall always be given for 6 months] for 4-6 months; or Linezolid - Clofazamine (Cfz) Pyrazinamide (Z) - Ethambutol (E) for 5 months. ● Regimen 4: Standard Long All Oral Regimen for FQ Susceptible (SLOR FQ-S) for MDR-TB and RR-Tb eligible to SLOR (no FQ resistance), give Levofloxacin (Lfx) - Bedaquiline (Bdq) - Linezolid (Lzd) - Clofazamine (Cfz) for 6 months; or Levofloxacin (Lfx) - Linezolid (Lzd) - Clofazamine (Cfz) for 12 - 14 months. ● Regimen 5: Standard Long All Oral Regimen for FQ Resistance (SLOR FQ-R) for MDR-TB and RR-TB eligible to SLOR (with FQ resistance), give 6 Months: Linezolid (Lzd) - Bedaquiline (Bdq) - Delamanid (Dlm) Clofazamine (Cfz) - Cycloserine (Cs) for 6 months; or 12 - 14 Months: Linezolid (Lzd) - Clofazamine (Cfz) - Cycloserine (Cs) for 12 - 14 months. ● Recommended daily doses of anti-TB medicines for treatment of multidrug-resistant TB for adults8;10: ○ Group A - Levofloxacin: no weight-based dosing proposed, usual upper daily dose of 1.5g, 250 mg formulation; Moxifloxacin: no weight-based dosing proposed, usual upper daily standard dose of 400 mg, 400 mg formulation; Bedaquiline: no weight-based dosing proposed, usual upper daily dose of 400 mg, 100 mg ■ ○ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 209 Treatment for Active Disease ○ ○ formulation; Linezolid: no weight-based dosing proposed, usual upper daily dose of 1.2 g, 600 mg tab formulation. ○ Group B - Clofazimine: no weight-based dosing proposed, usual upper daily dose of 100 mg, 50 mg or 100 mg formulation; Cycloserine: 10 - 15 mg/kg, 250 mg formulation. ○ Group C - Ethambutol: 15 - 25 mg/kg, 400 mg formulation; Delamanid: no weight-based dosing proposed, usual upper daily dose of 200 mg, 50 mg formulation; Pyrazinamide: 20 - 30 mg/kg, 500 mg formulation; Prothionamide: 15 - 20 mg/kg, 250 mg formulation. Second-line regimens for drug-susceptible TB ■ Consider giving a four-month drug-susceptible pulmonary TB treatment regimen of isoniazid, rifapentine, moxifloxacin and pyrazinamide: 2HPMZ/2HPM to adults with body weight >40 kg, including those who are also HIV-positive with CD4 count of >100 cells/mm3 (Conditional recommendation11) ● The following criteria excludes the adult patient in receiving the 2HPMZ/2HPM regimen: ○ Patients with < 40 kg of weight ○ Patients with severe extrapulmonary TB ○ PLHIV with a CD4 of < 100 cells/mm3 ○ pregnant , breastfeeding and postpartum women Second-line regimens for drug-resistant TB ■ Consider giving a 6-month treatment regimen consisting of bedaquiline, pretomanid, linezolid (600 mg) and moxifloxacin (BPaLM) to adults with MDR/RR-TB and in whom resistance to fluoroquinolones has been excluded (Conditional recommendation11). ■ Consider the use of the 9-month all-oral regimen in patients with MDR/RR-TB and in whom resistance to fluoroquinolones has been excluded (Conditional recommendation11). ■ Consider giving rifampicin, ethambutol, pyrazinamide and levofloxacin, with or without isoniazid for 6 months, for adults with confirmed rifampicin-susceptible, isoniazid-resistant tuberculosis (Hr-TB) (Conditional recommendation4). ■ Consider preparing an Individualized Treatment Regimen by constructing at least 4–5 likely effective drugs for adults undergoing retreatment MDR-TB and/or with RR-TB cases (not eligible to SSOR nor SLOR)9. ■ Consider giving longer regimens (18 - 20 months) comprised of all Group A agents and at least one Group B agent for adults with multidrug- or rifampicin-resistant tuberculosis (MDR/RR TB). Throughout the remainder of the treatment, a minimum of three agents should be maintained, even if bedaquiline is discontinued. If only one or two agents from Group A are utilized, both agents from Group B should be included. In cases where a regimen cannot be formulated Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 210 Treatment for Active Disease ● ● solely with agents from Groups A and B, agents from Group C are introduced to complete the treatment (Conditional Recommendation11). ■ Longer treatment regimens may be used in the following situations11: ● Additional resistance to key medicines of the BPaLM/BPaL regimen (except moxifloxacin) or the 9-month oral regimen. ● Lack of response to shorter treatment regimens ● Drug tolerance to the component medicines of the BPaLM/BPaL regimen (except moxifloxacin) or 9 months shorter all-oral treatment regimen. ● Pregnant and lactating women who could not benefit from the 9-month shorter all-oral regimen because of certain clinical conditions ■ Consider the following recommendations for the composition of longer treatment regimens for adults: ● Should be included (Strong recommendation11): Levofloxacin or moxifloxacin ; Bedaquiline; Linezolid ● May be included (Conditional recommendation11): Clofazimine and cycloserine or terizidone; ethambutol; Delamanid; Pyrazinamide; Imipenem-cilastatin or meropenem; amikacin (if adequate adverse reactions are ensured to be monitored, may be replaced by streptomycin if amikacin is not available); ethionamide or prothionamide, and p-aminosalicylic acid (if bedaquiline, linezolid, clofazimine or delamanid are not used or if better options to compose a regimen are not possible) ● Not to be included: Kanamycin and capreomycin (Conditional recommendation11); clavulanic acid (Strong - Against use11) Other pharmacologic therapies. Offer as clinically appropriate12. ○ Ancillary medicines for the management of drug side effects (antiemetics, antacids, pyridoxine, potassium replacement, thyroxine, medicines for psychiatric conditions, etc.); ○ Medicines for the management of possible comorbidities (cotrimoxazole, antiretroviral drugs, metformin) Non-pharmacologic Therapy ○ Nutrition buildup. ■ Assess and provide counseling based on nutritional status of all adults with active TB (Strong recommendation13). This includes the provision of nutritional sustenance on patients under treatment for faster healing and recovery, or the rendering nutritional advice to identify appropriate food for the patient’s condition, as well as fostering healthy eating habits and practices9. ○ Provide health education and counseling for adults on TB treatment, including smoking cessation Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 211 Preventive Treatment for Contacts ● Offer TB Preventive Treatment (TPT) to all eligible contacts of TB patients. ○ Either a tuberculin skin test (TST) or interferon-gamma release assay (IGRA) can be used to test for Latent TB Infection (Strong Recommendation14) ○ Give TPT to adults who are in contact with a person with TB who are found not to have active TB by an appropriate clinical evaluation or according to the eligibility criteria set by the National Tuberculosis Program: a. Offer TPT to the following risk groups once active TB is ruled out. Tuberculin Skin Test (TST) or interferon-gamma assays (IGRA) are not required prior to TPT initiation in these patients: ● PLHIV aged 1 year or older ● Individuals 5 years and older with other TB risk factors and who are household contacts of bacteriologically confirmed pulmonary TB b. Offer TPT to the following risk groups upon ruling out TB infection using TST or IGRA: ● Household contacts of bacteriologically confirmed pulmonary TB cases who are 5 years and older with no other risk factors for TB. ● Close contacts of bacteriologically confirmed pulmonary TB ● Any of the following patients: receiving dialysis, preparing for an organ or hematological transplantation, patients initiating anti-TNF treatment, those with silicosis. ○ Tuberculosis preventive treatment options: ■ Regardless of HIV status: ● 6 or 9 months of daily isoniazid (6H, 9H) or 3-month regimen of weekly rifapentine plus isoniazid (3HP)14: ○ 6H, 9H: daily isoniazid (5 mg/kg/day) for 6 or 9 months ○ 3HP: weekly rifapentine (150 mg) plus isoniazid (300 mg) [or Isoniazid + Rifapetine FDC 300mg/300mg] regimen for 3 months ● Offer 1-month daily rifapentine plus isoniazid (1HP) or 4 months daily rifampicin (4R) as alternative regimens (Conditional recommendation14). ● 1HP: daily rifapentine (600 mg/day) plus isoniazid (300 mg/day) for one month (28 doses) ● 4R: daily rifampicin for four months 10 mg/kg/day, not to exceed 600 mg daily ■ Offer 36 months daily isoniazid preventive treatment for adults living with HIV who have an unknown or a positive LTBI test and are unlikely to have active TB disease, irrespective of ART status, degree of immunosuppression, TB treatment history and pregnancy status (Conditional recommendation14). Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 212 Referral ● Refer to following adult TB patients to higher levels of care: ○ With presumptive severe forms of extrapulmonary tuberculosis (such as TB meningitis, disseminated TB and osteoarticular TB) ○ With presumptive DR-TB ○ With other comorbidities such as Severe Acute Malnutrition and Human Immunodeficiency Virus Infection13 ○ With altered or depressed mental status or seizures, including status epilepticus ○ Adults suspect of antituberculous drug toxicity such as: hepatotoxicity, dermatologic effects, severe systemic reactions, QT prolongation, neurotoxicity, ototoxicity and nephrotoxicity, hematologic effects, ophthalmic toxicity, musculoskeletal and endocrine effects, among others. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. World Health Organization. Global Tuberculosis Report. Published 2023. Accessed December 14, 2023. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023 UpToDate. Diagnosis of pulmonary tuberculosis in adults. Published 2022.Accessed December 14, 2023. https://www.uptodate.com/contents/diagnosis-of-pulmonary-tuberculosis-in-adults?search=pulmomary%20tuberculosis%20r eferral&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2 World Health Organization . WHO consolidated guidelines on tuberculosis - Module 2: screening – systematic screening for tuberculosis disease. Published 2021. Accessed December 13, 2023. https://tbksp.org/en/node/1274 World Health Organization. WHO consolidated guidelines on tuberculosis - Module 5: management of tuberculosis in children and adolescents. Published 2022. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789240046764 World Health Organization. WHO consolidated guidelines on tuberculosis - Module 3: diagnosis: rapid diagnostics for tuberculosis detection. Published 2021. Accessed December 13, 2023. https://tbksp.org/en/node/4 UpToDate. Rifamycins (rifampin, rifabutin, rifapentine). Published 2022. Accessed December 13, 2023. https://www.uptodate.com/contents/rifamycins-rifampin-rifabutin-rifapentine?search=tuberculosis%20toxicity&source=searc h_result&selectedTitle=9~150&usage_type=default&display_rank=9#H9 UpToDate. Antituberculous drugs: An overview. Published 2022. Accessed December 14, 2023. https://www.uptodate.com/contents/antituberculous-drugs-an-overview?search=tuberculosis%20drug%20toxicity&source=se arch_result&selectedTitle=1~150&usage_type=default&display_rank=1#H2636671244 World Health Organization. WHO operational handbook on tuberculosis: module 4: treatment: drug-resistant tuberculosis treatment. Published 2020. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789240006997 Department of Health. National Tuberculosis Program - Manual of Procedures, 8th Edition. Published 2020. Accessed December 14 2023. https://ntp.doh.gov.ph/download/ntp-mop-6th-edition/ Department of Health. Philippine National Formulary. DOH Pharmaceutical Division. Published 2019. Accessed December 14, 2023. https://drive.google.com/file/d/1QA05jVfoQu7DJZihMRx5Mq53TobWTwah/view World Health Organization. WHO consolidated guidelines on tuberculosis - Module 4: treatment: drug-susceptible tuberculosis treatment. Published 2022. Accessed December 14, 2023. https://www.who.int/publications/i/item/9789240048126 International Union Against Tuberculosis and Lung Disease. Management of Tuberculosis: A Guide to Essential Practice. Published 2019. Accessed December 14, 2023. https://theunion.org/sites/default/files/2020-08/TheUnion_Orange_2019.pdf World Health Organization. WHO consolidated guidelines on tuberculosis - Module 6: Nutritional care and support for TB patients Book traversal links for Module 6: Nutritional care and support for TB patients. Published 2013. Accessed December 14, 2023. https://tbksp.org/en/node/704 World Health Organization. WHO consolidated guidelines on tuberculosis - Module 1: tuberculosis preventive treatment. Published 2020. Accessed December 14, 2023. https://tbksp.org/en/node/ Back to Table of Contents Omnibus Health Guidelines ver. 2023 | 213 National Practice Guidelines Program Products The Omnibus Health Guidelines www.doh.gov.ph/dpcb/omnibus-health-guid elines The Omnibus Health Guideline: Rollout Guide ver. 1. 2023 bit.ly/OHGRolloutGuide_v1 The DOH-Approved Clinical Practice Guidelines www.doh.gov.ph/dpcb/doh-approved-cpg Quick Guide on the Adoption and Implementation of Clinical Practice Guidelines and Other Case Management Protocols for Local Health Systems Maturity Level Monitoring www.doh.gov.ph/sites/default/files/npg-lhs ml-guide.pdf Interim Public Health and Clinical Guidance www.doh.gov.ph/dpcb/interim-guidance Sample Clinician Support Tool (CST) for Hypertension Link to Sample Hypertension CST Health Examination Forms for Children Five (5) to Under 10 years old bit.ly/HEF2023-Child Health Examination Forms for Adolescents bit.ly/HEF2023-Adolescent Health Examination Forms for Adults 20 to 59 years old bit.ly/HEF2023-Adult Health Examination Forms: Users’ Quick Guide ver. 1. 2023 bit.ly/HEFGuide_v1


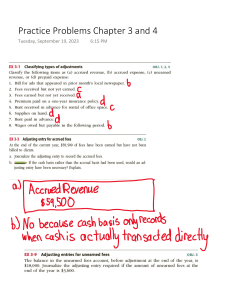

![Avoiding Trafficked Labor [English]](http://s2.studylib.net/store/data/027039054_1-3047401815af88cce843a8404da043fb-300x300.png)