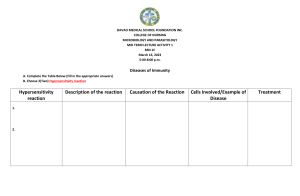
HYPERSENSITIVITY The adaptive immune response is a critical component of host defense against infection and is essential for normal health. The term hypersensivity is used to define a set of responses (result of exaggerated normal responses ) categorized as types I–IV by Gell and Coombs. In one circumstance - harmful immunologically mediated hypersensitivity type I reactions known generally as allergic reactions occur in response to inherently harmless ‘environmental’ antigens such as pollen, food, and drugs. Type I. IgE-mediated reactions (commonly called allergic reactions or allergy) are stimulated by the binding of IgE, via its Fc region, to high-affinity IgE-specific Fc receptors designated FcεRI. FcεRI are expressed on mast cells, basophils, and eosinophils. Binding of antigen to preformed antigen-specific IgE bound to high-affinity FcεRI initiates type I hypersensitivity reactions. When the IgE molecules encounter antigens, a cascade of events leads to degranulation and release of inflammatory mediators and cytokines from mast cells and basophils. This ultimately results in the clinical manifestations of type I hypersensitivity, which include rhinitis, asthma, and, in severe cases, anaphylaxis (from the Greek ana, which means “away from,” and phylaxis, which means “protection”). Type I hypersensitivity reactions are rapid, occurring within minutes after challenge (reexposure to antigen). Consequently, allergic reactions are also called immediate hypersensitivity. GENERAL CHARACTERISITICS OF TYPE I HYPERSENSTIVITY Sequence of events involved in the development of allergic reactions can be divided into several phases: (1) the sensitization phase, during which IgE antibody is produced in response to an antigenic stimulus and binds to specific receptors on mast cells and basophils (2) the activation phase, during which re-exposure to antigen (challenge) triggers the mast cells and basophils to respond by release of the contents of their granules (3) the effector phase, during which a complex response occurs as a result of the effects of the many inflammatory mediators released by the mast cells and basophils. A predisposition to become IgE-sensitized to environmental allergens is called atopy To produce an, allergic reaction against a given antigen: an atopic individual must first be exposed to the antigen under conditions that result in the production of IgE antibodies. Allergic symptoms occur when an individual who has been sensitized in this fashion has subsequent exposure to the antigen. Exposure can lead to different clusters of symptoms, characterized by the tissues that are most prominently affected. Common forms of allergic response: ----airborne allergens,: causing symptoms that affect predominantly the nasal passages (allergic rhinitis), the eyes (allergic conjunctivitis), or the lower airways and lungs (asthma). ------Ingested allergens can lead to food allergy, sometimes affecting only the gastrointestinal tract (for example, eosinophilic esophagitis), ------Allergic reactions also involve locations distant from the site of antigen entry then the reactions are considered to be systemic reactions due to spread of the antigen throughout the body via the blood circulation. Systemic reactions can be limited to a single distant organ, causing: 1. 2. 3. 4. hives (also called urticaria) when they target the skin, wheezing (or bronchospasms) when they involve the lungs, life-threatening lowering of the blood pressure when they target the vascular system. Serious systemic reactions are designated by the term anaphylaxis. It is not known why sensitization with a particular allergen in one individual leads to local reactions at the time of allergen challenge, whereas sensitization with same can cause serious anaphylatic shock in oihers -- Hives also called urticaria is a common skin rash triggered by many things, including certain foods, medication and stress. ---Symptoms include itchy, raised, red or skin-coloured welts on the skin's surface. Mast-cell activation has different effects on different tissues. SEQUENCE OF EVENTS IN ALLERGGIC RESPONSE SENSITIZATION PHASE All normal individuals can make IgE antibody specific for a variety of antigens While most of the population does not develop clinically significant allergic reactions to the majority of potential allergens, some individuals manifest allergic responses to multiple common antigens. TH2 Cell Dependency of IgE Antibody Production >The immune response leading to IgE production in response to antigen is driven by two main groups of signals: (1) signals that favor the differentiation of naive CD4+T cells to a TH2 phenotype (2) TH2 cytokines like IL-4 stimulate B cells to class-switch to the production of IgE. > IL-4 levels are significantly higher in the allergic population. >I gE levels are approximately tenfold higher in allergic individuals. >Low levels of IgE antibody in non-allergic individuals are maintained by suppressor effects mediated by IFN-γ produced by TH1 cells in normal individuals, a balance is maintained between TH2-derived cytokines, which upregulate IgE responses, and TH1-derived cytokines, which downregulate IgE responses. Once adequate exposure to the allergen occurs by repeated mucosal contact, ingestion, or parenteral injection and failure of a control mechanism --- leading to overproduction of IL-4 by TH2 cells -----ultimately, increased IgE production by B cells occurs. ------This IgE rapidly attaches to the Fc receptors on circulating mast cells and basophils and the individual is sensitized. --One of the most important features that mast cells and basophils share is receptors (FcεRI) on their cell membranes that bind with high affinity to the Fc portion of IgE. ---Once bound, the IgE molecules persist at the cell surface for weeks. The cell will remain sensitized as long as enough IgE- antibody remains attached. -- the IgE molecules will trigger the activation of the cell when it comes into contact with antigen. ---The mast cell is not specific for any particular antigen; the IgE bound to it is. Passive Sensitization can be achieved by transfer of serum that contains IgE antibody to a specific antigen. A procedure known as the Prausnitz-Kustner (P-K) test, is performed as a test for the antibodies responsible for anaphylactic reactions. Serum from an allergic individual is injected into the skin of a nonallergic person. After 1–2 days, during which the locally injected antibody diffused toward neighboring mast cells and became bound to them, the site of injection was said to be sensitized, and would respond with an urticarial reaction (hives) when injected with the antigen to which the donor was allergic. Such a reaction in passively sensitized animals is called passive cutaneous anaphylaxis (PCA). ACTIVATION PHASE The activation phase of allergic reactions begins when the mast cell is triggered to release its granules and their inflammatory mediators. At least two of the FcεRIs must be bridged together in a stable configuration for the activation phase to occur. This linkage is accomplished by a multivalent antigen that can bind a different molecule of IgE to each of several epitopes, thus cross-linking them Experimental crosslinking of FcεRI receptors: to activate mast cells Anti-IgE cross-linking, Lectin cross-linking, Chemical cross-linking, Anti Fc εRI cross-linking Natural mechanisms other than IgE Fc receptor cross-linking: Anaphylatoxins C3a and C5a (Mast cells express receptors for complement anaphylatoxins C3a and C5a (i.e., C3aR and C5aR)) Physical factors such as heat, cold, or pressure: cold-induced urticaria, dermatographic uticaria in which the skin becomes raised and inflamed when stroked, scratched, or slapped. The triggering of a mast cell by the bridging of its receptors initiates a rapid and complex series of events culminating in the degranulation of the mast cell and the release of potent inflammatory mediators. Allergic reactions are often referred to as immediate hypersensitivity Physiologic consequences of IgE-mediated mast-cell degranulation depend on the dose of antigen and route of entry. ---Mast cells that degranulate: --In the gastrointestinal tract cause increased fluid secretion and peristalsis, which, in turn, can result in diarrhea and vomiting --in the lung -decrease in airway diameters and increased mucus secretion leading to congestion and blockage of the airways (coughing, wheezing, phlegm), swelling and mucus secretion in nasal passages --degranuulation of mast cells present along the blood vessels causes increased blood flow and vascular permeability > increased fluid in tissues or edema. increased cells and protein in tissues, increased effector response in tissues> Hypotension potentially leading to anaphylactic shock EFFECTOR PHASE Mast-cell degranulation begins within seconds of antigen binding, releasing an array of preformed and newly generated inflammatory mediators 1. preformed mediators such as short-lived vasoactive amine histamine, serine esterases, and proteases such as chymase and tryptase stored in their intracellular granules 2. synthesized de novo. chemokines, cytokines, and lipid mediators—prostaglandins, leukotrienes, thromboxanes (collectively called eicosanoids), and platelet-activating factor (PAF). Granule contents include the short-lived vasoactive amine histamine, serine esterases, and proteases such as chymase and tryptase. Preformed Mediators Histamine. >Histamine is formed in the cell by decarboxylation of the amino acid histidine; it is stored in the cell by binding via electrostatic interaction to an acid matrix protein called heparin. >When released, histamine binds rapidly to a variety of cells via two major types of receptor, H1 and H2, which have different tissue distribution and mediate different effects. ------When histamine binds to H1 receptors in smooth muscles, it causes constriction; -------when it binds to H1 receptors on endothelial cells, it causes separation at their junctions, resulting in vascular permeability. -------H2 receptors are involved in mucus secretion, increased vascular permeability, and the release of acid from stomach mucosa. All these effects are responsible for some of the major signs of systemic anaphylaxis: difficulty in breathing (asthma) or asphyxiation result from the constriction of smooth muscle around the bronchi in the lung, and the drop in blood pressure is a consequence of the extravasation of fluid into tissue spaces as the permeability of blood vessels increases. H1 receptors are blocked by antihistamines, such as Benadryl®, which compete directly for H1 receptor sites with histamine; when these drugs are given soon enough, they can counteract its effects. Blockage of H2 receptors requires other drugs, such as cimetidine. Antihistamines are ineffective in controlling constriction of smooth muscles That has late second onset which is slower but is more persistent than that produced by histamine. This observation led to the discovery of the slow-reacting substance of anaphylaxis (SRS-A), now known to be a group of molecules called leukotrienes. Serotonin. Serotonin is present in the mast cells of humans with effects are similar to those of histamine- causing constriction of smooth muscle and increases vascular permeability. Chemotactic Factors. A variety of chemotactic factors are released following degranulation of mast cells. ----Lowmolecular- weight peptides called eosinophilic chemotactic factors (ECFs) are also released upon degranulation. Heparin. Heparin is an acidic proteoglycan that constitutes the matrix of the granule, and to which basic mediators, such as histamine and serotonin, are bound. Mast cells also synthesize de novo and release chemokines, cytokines, and lipid mediators—prostaglandins, leukotrienes, thromboxanes (collectively called eicosanoids), and platelet-activating factor. ----Platelet-activating factor (PAF) and leukotrienes are late-phase mediators that also participate in the chemotaxis of inflammatory cells to the site --- Important inflammatory cell attracted to the site is the neutrophil. Chemotaxis of these polymorphonuclear granulocytes occurs in response to IL-8 released by activated mast cells. They are are important in the late phase of IgE-mediated hypersensitivity. Other cells attracted to the site in response to mast cell-derived chemotactic factors include basophils, macrophages, platelets, and lymphocytes These secreted products contribute to both acute and chronic inflammation. The lipid mediators, in particular, can act both rapidly and persistently to cause smooth muscle contraction, increased vascular permeability, and the secretion of mucus, as well as induce the influx and activation of leukocytes, which contribute to allergic inflammation. Late-Phase Reaction Many of the substances released during mast-cell activation and degranulation are responsible for the initiation of a profound inflammatory response, which consists of infiltration and accumulation of eosinophils, neutrophils, basophils, lymphocytes, and macrophages. The most important of these elements, which constitute a large percentage of the cells activated during an inflammatory response, are eosinophils and neutrophils. This response, referred to as the late-phase reaction, often occurs within 48 hours and may persist for several days. 1. mast cell, degranulated releases eosinophilic chemotactic factor (ECF-A), > recruits eosinophils to the reaction area. 2. Increased vascular permeability caused by histamine and other mediators> provides passage of eosinophils and other leukocytes from the circulation to the tissue 3. Various cytokines, including GM-CSF, IL-3, IL-4, IL-5, and IL-13, play important roles in eosinophil growth and differentiation, and in the cell adhesion of certain cell types. 4. Together these inflammatory mediators generate a second, milder wave of smooth muscle contraction than the immediate response, along with sustained edema. In allergic asthma, the late-phase reaction also promotes the development of one of the cardinal features of this form of asthma: airway hyperreactivity to nonspecific bronchoconstrictor stimuli like histamine. Late-phase reaction of type I IgE-mediated hypersensitivity showing some of the mediators involved. Eosinophils bind IgE through their low-affinity IgE Fc receptor (FcεRII), They also express Fc receptors to the Fc portion of IgG. Thus, both IgE- and IgG-bound antigen will bind to their respective Fc receptors, causing eosinophil activation, degranulation and release releasing leukotrienes that cause muscle contraction. They also release PAF and major basic protein (MBP). eosinophilic cationic protein (ECP) which damage tissues like the respiratory tract. Recruited neutrophils phagocytose the antigen–antibody immune complexes, degranulation release their powerful lysosomal enzymes that damage tissue; leukotrienes and PAF. T and B lymphocytes and macrophages also enter the area, further sensitizing or immunizing the host against the antigen. These reactions occur in response to antigen like pollen, animal dander, or the common dust mite, and result in tissue damage in actopic individuals. Allergic rhinitis (commonly known as hay fever) is the most common atopic disorder worldwide. It is caused by airborne allergens that react with IgE-sensitized mast cells in the nasal passages and conjunctiva. The route of administration of allergen determines the type of IgE-mediated allergic reaction that results. Food Allergies: intake of certain foods (e.g., peanuts, rice, eggs, etc.). cross-linking of allergen-specific IgE on mast cells of the upper and lower gastrointestinal tract. If the allergen is absorbed into the bloodstream as a consequence of increased permeability of mucous membranes, allowing food allergens to be transported to mast cells present in skin. This causes wheal and flare reactions (atopic urticaria), commonly known as hives. Atopic Dermatitis A form of allergic reaction most frequently seen in young children, allergic dermatitis is caused by the development of inflammatory skin lesions induced by mast cell cytokines released following degranulation. The skin eruptions that develop are erythematous (symmetrical, red, raised skin areas) and pus (white cell)-filled. Asthma is a common form of localized anaphylaxis. a common chronic disorder of the airways that involves a complex interaction of airflow obstruction, bronchial hyperresponsiveness, and an underlying inflammation. three basic pathophysiologic events within the airways: (1) reversible obstruction; (2) augmented bronchial responsiveness to a variety of physical and chemical stimuli (airwayhyperreactivity); and (3) inflammation. Allergens- including airborne pollens, dust, viral antigens, and various chemicals, can induce allergic asthma. Asthma may also be induced by phenomena ranging from exercise to exposure to cold temperatures independent of allergen exposure, a phenomenon known as intrinsic asthma. Corticosteroids (CSTs) remain the gold standard for asthma management. while it improves asthma symptoms, it does not alter the natural course of asthma or offer clear long-lasting improvement of respiratory performance. Allergen introduced into the bloodstream can cause anaphylaxis. If allergen is introduced directly into the bloodstream, for example, by a bee or wasp sting, or is rapidly absorbed into the bloodstream from the gut in a sensitized individual, connective-tissue mast cells associated with blood vessels throughout the body can become immediately activated, resulting in a widespread release of histamine and other mediators that causes the systemic reaction called anaphylaxis. The symptoms of anaphylaxis can range in severity from mild urticaria (hives) to fatal anaphylactic shock (see Fig. 14.12, first and last panels). Acute urticaria is a response to foreign allergens that are delivered to the skin via the systemic blood circulation. Activation of mast cells in the skin by allergen causes them to release histamine, which in turn causes itchy, red swellings all over the body—a disseminated version of the wheal-and-flare reaction. Although acute urticaria is commonly caused by an IgE-mediated reaction against an allergen, the causes of chronic urticaria, in which the urticarial rash persists or recurs over long periods, remain incompletely defined. Some cases of chronic urticaria are caused by autoantibodies In anaphylactic shock, a widespread increase in vascular permeability and smooth muscle contraction results from a massive release of histamine and other mast cell- and basophil-derived mediators such as leukotrienes. The consequences are a catastrophic reduction of blood pressure, culminating in hypotensive shock, (a condition in which low blood pressure leads to inadequate supply of blood to vital organs, often leading to death), and constriction of the airways, culminating in respiratory failure. The most common causes of anaphylaxis are allergic reactions to wasp and bee stings, ingested or injected medications, or allergic responses to foods in sensitized individuals. For example, anaphylaxis in individuals allergic to peanuts is relatively common. Severe anaphylactic shock can be rapidly fatal if untreated, but can usually be controlled by the immediate injection of epinephrine, which via stimulation of βadrenergic receptors causes relaxation of airway smooth muscles, and via stimulation of α-adrenergic receptors reverses the life-threatening cardiovascular effects. Systemic allergic reactions can occur following repeated treatment with many classes of drugs. A relatively common inducer of IgE-mediated allergic reaction is penicillin and other drugs that share aspects of its structure and immunological reactivity. In people who have developed IgE antibodies against penicillin, injection of the drug can cause anaphylaxis and even death. Overview of induction and effector mechanisms in type I hypersensitivity. HYPERSENSITIVITY: TYPES II AND III Hypersensitivity reactions characterized as type II and type III reactions are mediated by antibodies belonging to the IgG, IgM, and, in some cases, IgA or IgE isotypes. > Distinction between these two forms of hypersensitivity: ------type and location of antigen involved -----and the way in which antigen is brought together with antibody. >Type II hypersensitivity reactions are the result of the binding of antibody directly to an antigen on the surface of a cell. >Type III reactions are the result of deposition of antigen–antibody immune complexes. >The target antigens involved in type II and type III hypersensitivity reactions are often self-antigens TYPE II HYPERSENSITIVITY Three different antibody-mediated mechanisms are involved i.e. the targeted cell is either damaged or destroyed through a variety of mechanisms: (a) complement-mediated reactions (b) antibody-dependent cell-mediated cytotoxicity (c) antibody-mediated cellular dysfunction. Many of these reactions are manifestations of antibody-mediated autoimmunity. The antibodies involved in these hypersensitivity reactions are either directed against normal self-antigens (e.g., cross-reactive antibodies elicited following an infection) or modified self-antigens (e.g., drug-induced autoantibodies elicited following the binding of drugs to certain cell membranes). Complement-Mediated Reactions Antibodies react with cell membrane self-antigens and this is followed by complement fixation > activates the complement cascade > leads to lysis of the cell Membrane Attack Complex. Alternatively, binding of antibody to the cell surface and subsequent activation of complement to yield C3b effectively opsonize the target cell. ---Opsonization culminates in the phagocytosis and destruction of the cell by macrophages and neutrophils expressing surface Fc receptors or receptors that bind C3b. Blood cells are most commonly affected by this mechanism. IgG Fc receptor knockout mice fail to mount type II (and type III) hypersensitivity reactions, a finding that underscores the pivotal role played by IgG Fc receptors in initiating these reaction cascades. Antibody-Dependent Cell-Mediated Cytotoxicity Antibody-dependent cell-mediated cytotoxicity (ADCC) utilizes Fc receptors expressed on many cell types (e.g., natural killer [NK] cells, macrophages, neutrophils, eosinophils) as a means of bringing these cells into contact with antibody-coated target cells. Lysis of these target cells requires contact but does not involve phagocytosis or complement fixation. ADCC-mediated lysis of target cells is analogous to that of cytotoxic T cells and involves the release of cytoplasmic granules (modified lysosomes) containing perforin and granzymes. Once released from the lytic granules, perforins insert into the target cell membrane and polymerize to form pores. In contrast, granzymes, which consist of at lease three serine proteases, enter the cytoplasm of the target cell and activate events leading to apoptosis. ADCC reactions are typically triggered by IgG binding to IgG-specific Fc receptors (FcγIII, also known as CD16) on the effector cells. IgE antibodies can also be involved in ADCC. In this situation, the low-affinity IgE Fc receptor (FcεRII) expressed on certain cells, including eosinophils binds to the Fc portion of IgE antibodies bound to target antigens (e.g., parasites) Antibody-Mediated Cellular Dysfunction In some type II hypersensitivity reactions, antibodies bind to cell-surface receptors that are critical for the functional integrity of the cell. ---When autoantibodies bind to such receptors they impair or dysregulate cell function without causing cell injury or inflammation. EXAMPLES OF TYPE II HYPERSENSITIVITY REACTIONS Transfusion Reactions: >Transfusion of ABO-incompatible blood results in complement-mediated cytotoxic reactions > Example, individuals with type O blood have in their circulation IgM anti-A and anti-B antibodies (isohemagglutinins), which react with the A and B blood-group substances, respectively. >a single IgM molecule is sufficient to activate many complement moleculeswhich will destroy transfused A or B type blood cells in recipient of O type blood group. Drug-Induced Reactions: >In some people, certain drugs act as haptens and combine with cells or with other circulating blood constituents and induce antibody formation. >When antibody combines with cells coated with the drug, cytotoxic damage results. Example, some drugs can bind to platelets causing them to become immunogenic. Antibody responses that are generated cause lysis of the platelets and resulting thrombocytopenia (low blood platelet count). Hypersensitivity to drugs may also induce IgE-mediated immediate type I hypersensitivity reactions Rhesus Incompatibility Reactions: Rhesus (Rh) incompatibility reaction seen in infants born of mothers with Rh-incompatible blood groups. Rh− mothers can become sensitized to Rh antigens during their first pregnancy with a child whose RBCs are Rh+. This occurs as a result of the release of some of the baby’s RBCs intothe mother’s circulation perinatally and particularly during birth. If the mother is thereby sufficiently immunized toproduce anti-Rh antibody of the IgG isotype, subsequent Rh+ fetuses will be at risk, since, IgG antibody is capable of crossing the placenta. Thus, in second or subsequent pregnancies, when the anti-Rh IgG antibodies have crossed the placenta, they bind to the Rh antigen on the RBCs of the fetus. Because the density of Rh antigen on the surface of RBCs is low, these antibodies usually fail to agglutinate or lyse the cells directly. However, the antibody-coated cells are readily destroyed by the opsonic effect of the Fc portions of the IgG, which interact with the receptors for Fc on the phagocytic cells of the reticuloendothelial system. The result is progressive destruction of the fetal or newborn RBCs, with the pathologic consequences that come from decreased transport of oxygen and from increased bilirubin from the products of the breakdown of hemoglobin, a condition known as erythroblastosisfetalis (hemolytic disease of the newborn). Prevention of this Rh incompatibility reaction can be achieved with the administration of anti-Rh antibodies (passive Reactions Involving Cell Membrane Receptors: > An example of antibody-mediated cellular dysfunction due to reactivity with a cell receptor is seen in the autoimmune disease myasthenia gravis. --Antagonistic autoantibodies reactive with acetylcholine receptors in the motor end platesof skeletal muscles impair neuromuscular transmission, causing muscle weakness Graves’ disease, the autoantibodies serve as agonists, causing stimulation of the target cells. These antibodies are directed against thyroid-stimulating hormone receptor on thyroid epithelial cells and stimulate the cells, resulting inhyperthyroidism. Reactions Involving Other Cell Membrane Determinants: >As a consequence of certain infectious diseases, or for other, still unknown reasons, some individuals produce autoantibodies reactive against their own blood cells. --When RBCs are the target, binding of anti-RBC autoantibody shortens their life span or destroys them immediately. This may lead to progressive anemia if the production of new RBCs cannot keep pace with destruction. >immune thrombocytopenia purpura (ITP) :antibodies directed to platelets result in platelet destruction > Autoantibodies directed against granulocytes can induce agranulocytosis predisposing individuals to various infections. Antibodies may form against other tissue components such as a type of basement membrane collagen particularly prevalent in the lung and kidneys, causing Goodpasture’s syndrome > desmosomes between keratinocytes in the skin resulting in pemphigus vulgaris. Type III Hypersensitivity Under normal conditions, circulating immune complexes composed of antibodies bound to foreign antigens : 1. Phagocytic cells - Phagocytosis is facilitated by the binding of the Fc regions of the antibodies present in such complexes to IgG Fc receptors expressed on these cells. 2. RBCs that have C3b receptors - bind immune complexes that have fixed complement and transport them to the liver, where the complexes are removed by phagocytic Kupffer cells. 3. Histidine-rich glycoprotein (HRG): abundantly synthesized by the liver and released into the blood stream. HRG does not require pre-activation unlike complements. HRG is readily available to engage in the removal of immune complexes via an FcγRdependent mechanism. HRG has the ability to clear apoptotic cells by binding naked DNA. Through its interactions with naked DNA and immune complexes, HRG may mask epitopes recognized byautoantibody-producing B cells (e.g., rheumatoid factors and anti-double stranded DNA antibodies) When physiologic mechanisms for clearing immune complexes are overwhelmed with large quantities of such complexes, then immune complexes of a certain size can inappropriately deposit in the tissues and trigger a variety of systemic pathogenic events known as type III hypersensitivity reactions. > These reactions can be: --- systemic (also called systemic immune complex disease) ---- localized (also known as localized immune complex disease) > Associated with immune complex deposition in the kidneys, skin, joints, choroid plexus, and ciliary artery of the eye. > Generation of immune complexes can be stimulated by exogenous antigens such as bacteria and viruses or, as in the case of the Arthus reaction, by intradermal or intrapulmonary exposure to large amounts of foreign protein. Alternatively, endogenous antigens, such as DNA, can serve as a target for autoantibodies as seen in systemic lupus erythematosus. Patients with SLE often have both systemic (multiorgan) and localized manifestations of immune complex disease. Like glomerular disease.caused by deposition of IC in kidneys. Mechanism of injury to tissues : ----IgG is the immunoglobulin isotype usually involved in type III hypersensitivity reactions, but IgM can also be involved. As with type II hypersensitivity reactions ---IgG Fc receptors (CD16) expressed on leukocytes play a pivotal role in initiating type III reaction cascades. ---The antibody–antigen complexes may fix complement and/or activate effector cells (the main cell type being the neutrophil) that cause tissue damage. ---C3a and C5a generated by complement activation induce mast cells and basophils to release arachidonic acid metabolites and chemokines that attract additional basophils, eosinophils, macrophages, and neutrophils into the area. ---The polymorphonuclear cells release their lysosomal enzymes at the surface of the affected tissues. ---Macrophages are stimulated to release tumor necrosis factor-α (TNF-α) and interleukin-1 (IL-1) Systemic Immune Complex Disease Pathogenesis of systemic immune complex disease canbe divided into three phases. 1. antigen– antibody immune complexes form in the circulation. 2. This is followed by deposition of immune complexes in various issues that initiates the 3. third phase in which inflammatory reactions in various tissues occur Several factors help to determine whether immune complex formation will lead to tissue deposition and disease. ---The size of the complexes appears to be important. > Very large complexes formed under conditions of antibody excess are rapidly removed from the circulation by phagocytic cells and therefore are harmless. Small or intermediate complexes circulate for longer periods of time and bind less avidly to IgG Fc receptors expressed on phagocytic cells. T Therefore, small-to-intermediate sized immune complexes tend to be more pathogenic as compared with large complexes. ---Integrity of the mononuclear phagocytic system. An intrinsic dysfunction of this system increases the probability of persistence of immune complexes in the circulation. The favored sites of immune complex deposition are the kidneys, joints, skin, heart, and small blood vessels. Serum sickness: Infection by both the Corynebacterium and the Clostridium organisms lead to pathological consequences due to the secretion of exotoxins that are extremely damaging to host cells. In pre-antibiotics era, the strategy that evolved to treat these diseases was to neutralize the toxins rapidly by administering passive immunization by injecting large amounts of a serum containing preformed antitoxin antibody from immunized horses. administration of large quantities of heterologous serum from another species causes the recipient to synthesize antibodies to the foreign immunoglobulin, leading to the formation of antigen–antibody complexes that result in the clinical symptoms associated with serum sickness. The classic clinical manifestations consist of chills, fever, rash, arthritis, and sometimes glomerulonephritis (inflammation of the glomeruli of the kidneys). Infection-Associated Immune Complex Disease. Example: Rheumatic feve: disease is associated with infections (e.g., throat) caused by group A streptococci, and it involves inflammation and damage to heart, joints, and kidneys. A variety of antigens in the cell walls and membranes of streptococci have been shown to be cross-reactive with antigenspresent in human heart muscle, cartilage, and glomerular basement membrane. Antibody to the streptococcal antigens binds to these components of normal tissue and induces inflammatory reactions Rheumatoid arthritis: rheumatoid factor-an IgM autoantibody that binds to the Fc portion of normal IgG. These immune complexes participate in causing inflammation and damage of joints. In a number of infectious diseases (malaria, leprosy, dengue) there may be times during the course of the infection when large amounts of antigen and antibody exist simultaneously and cause the formation of immune aggregates that are deposited in a variety of locations. Thus, the complex of symptoms in any of these diseases may include a component attributable to a type III hypersensitivity reaction. Complement deficiency Complexes that contain C3b bind to erythrocytes bearing CR1. The erythrocytes deliver the complexes to mononuclear phagocytes within the liver and spleen for removal by phagocytosis. The components of the classical complement pathway reduce the number of antigen epitopes that antibodies can bind to by intercalating into the lattice of the complex, resulting in smaller, soluble complexes. It is these small, soluble complexes that bind most readily to the erythrocytes. In patients with complement deficiencies affecting C1, C2, and C4, the complexes remain large and bind poorly to the erythrocytes. These non-erythrocyte-bound complexes are taken up rapidly by the liver and then released to be deposited in tissues such as skin, kidney and muscle, where they can set up inflammatory reactions. A local hypersensitivity reaction called an Arthus reaction : Result of local inflammatory responses generated occur following reactivity of antigen with already formed, antigen-specific IgG antibody. When such preformed antibodies come in contact with antigen at the appropriate concentrations (antibody excess), in or near vessel walls (venules), insoluble immune complexes form and accumulate. The end result is rupture of the vessel wall and hemorrhage, accompanied by necrosis of local tissue. HYPERSENSITIVITY: TYPE IV type IV hypersensitivity is T-cell mediated. type IV responses involve the activation, proliferation, and mobilization of antigenspecific T cells. Thus, type IV hypersensitivity is delayed as compared with antibodymediated hypersensitivity reactions, and it is often referred to as delayed-type hypersensitivity (DTH). DTH reactions can also result in damage to host cells and tissues. DTH reactions are cell-mediated immune responses.- basically TH1 and CD8 cytotoxic T cells Depending on the antigen involved, they mediate beneficial (resistance to viruses, bacteria, fungi, and tumors) or harmful (allergic dermatitis, autoimmunity) aspects of immune function. Other antigens capable of eliciting DTHreactions: ---Alloantigens those expressed by foreign cells in transplantation (allografts) ---one of many chemicals (serving as haptens) capable of penetrating skin and coupling to body proteins that serve as carriers GENERAL CHARACTERISTICS AND PATHOPHYSIOLOGY OF DTH Clinical features of type IV hypersensitivity reactions vary: ---depending on the sensitizing antigen and the route of antigen exposure. These variants include contact hypersensitivity, tuberculin-type hypersensitivity, and granulomatous hypersensitivity Common pathophysiologic mechanisms account for each of these variants: The major events leading to these reactions involve the following three steps: (1) activation of antigen-specific inflammatory TH1 and TH17 cells in a previously sensitized individual (2) elaboration of pro-inflammatory cytokines by the antigen-specific TH1 cells (3) recruitment and activation of antigen-nonspecific inflammatory leukocytes. These events typically occur over a period of several days (48–72 hours). MECHANISM INVOLVED IN DTH REACTION Previous exposure to the antigen is required to generate DTH reactions. Such exposure (the sensitization stage) activates and expands the number of antigen-specific TH1 and TH17 cells that, when subsequently challenged with the same antigen, respond by producing cytokines that promote DTH reactions (the elicitation stage). During the elicitation phase, activated TH1 and TH17 cells mediate the activation and recruitment of innate immune cells (antigen-nonspecific inflammatory cells) to the area of the reaction, including the activation and recruitment of macrophages and NK cells, and neutrophils. The sensitization stage typically occurs over a 1–2 week period The elicitation stage requires approximately 18–48 hours from time of antigenic challenge to recruit and activate these cells, a period that culminates in the histological and clinical features of DTH. The clinical manifestations of DTH can last for several weeks or, in some cases, can be chronic (e.g., DTH occurring in certain autoimmune diseases). The antigen-challenged TH1 cells produce several cytokines during the elicitation stage, most notably chemokines and IFN-γ, which cause chemotaxis and activation of macrophages . Another cytokine produced by these cells is IL-12. IL-12 suppresses the TH2 subpopulation and promotes the expansion of the TH1 subpopulation thereby driving the response to produce moreTH1-synthesized cytokines that activate macrophages. Thus, IL-12 plays an important role in DTH. DTH reactions also involve CD8+ T cells, which are first activated and expanded during the sensitization stage of the response. These cells can damage tissues by cell-mediated cytotoxicity . Activation of CD8+ T cells occurs as a consequence of the ability of many lipid-soluble chemicals capable of inducing DTH reactions. EXAMPLES OF DTH 1. Contact Sensitivity: Contact sensitivity (sometimes called contact dermatitis) is a form of DTH in which the target organ is the skin. The inflammatory response is produced as the result of contact with sensitizing substances on the surface of the skin. Thus, it is primarily an epidermal reaction characterized by eczema at the site of contact with the allergen that typically peaks 48–72 hours after contact. The prototype for this form of DTH is poison ivy dermatitis caused by CD8 T-cell response to urushiol oil (a mixture of pentadecacatechols) in the plant. These chemicals are lipid-soluble and so can cross the cell membrane and attach to intracellular proteins. Within the cell, these chemicals react with cytosolic proteins to generate modified peptides that are translocated to the endoplasmic reticulum and then delivered to the cell surface in the contextof MHC class I molecules. Cells presenting such modified self-proteins are subsequently damaged or killed by CD8+ T cells. 2. Tuberculin-Type Hypersensitivity Tuberculin-type reactions are cutaneous inflammatory reactions characterized by an area of firm red swelling of the skin that is maximal at 48–72 hours after challenge. The term tuberculin-type derives from the prototype DTH reaction in which a lipoprotein antigen isolated from Mycobacterium tuberculosis called tuberculin was used to test for evidence of exposure to the causative agent of tuberculosis. Today, TB tests are performed by intradermally injecting a more purified lipoprotein extract isolated from M. tuberculosis called purified protein derivative (PPD). The PPD test (also called the Mantoux test) is extremely useful for public health surveillance of TB. If an individual has been previously sensitized to antigens expressed by M. tuberculosis as a consequence of infection with this organism, the characteristic tuberculin type lesion will appear at the site of injection within 48–72 hours. Evidence of erythema (redness) and induration (raised thickening) appear, reaching maximal levels 72 hours after the challenge. These reactions, even when severe, rarely lead to necrotic damage and resolve slowly. 3. Allograft Rejection if an individual receives grafts of cells, tissues, or organs taken from an allogeneic donor (a genetically different individual of the same species), it will usually become vascularized and initially be accepted. However, if the genetic differences are within the major histocompatibility complex (MHC), T-cellmediated rejection of the graft ensues, whose duration and intensity is related to the degree of incompatibility between donor and recipient. After vascularization, there is an initial invasion of the graft by a mixed population of antigen-specific T cells and antigen-nonspecific monocytes through the blood vessel walls. This inflammatory reaction soon leads to destruction of the vessels; this deprivation of nutrients is quickly followed by necrosis and breakdown of the grafted tissue. 4. Examples of autoimmune diseases in which DTH reactions are involved include rheumatoid arthritis, type I diabetes, and multiple sclerosis Historically, hypersensitivity reactions due to immunological responses were classified by Gell and Coombs into four broad types, of which type I hypersensitivity reactions represented immediate-type allergic reactions mediated by IgE antibodies, with mast-cell activation the major final effector mechanism. Type II and III hypersensitivity responses were defined as those that were driven by antigen-specific IgG antibodies, the final effector mechanism being complement (type II) or FcR-bearing cellular effectors (type III). Finally, type IV hypersensitivity responses were depicted as being driven by cellular effectors, including lymphocytes and a variety of myeloid cell types. The sequence of events involved in the development of allergic reactions can be divided into several phases: (1) The sensitization phase, during which IgE antibody is produced in response to an antigenic stimulus and binds to specificreceptors on mast cells and basophils (2) the activation phase, during which reexposure (challenge) to antigen triggers the mast cells and basophils to respond by release of the contents of their granules (3) the effector phase, during which a complex response occurs as a result of the effects of the many inflammatory mediators released by the mast cells and basophils. As noted above, the clinical manifestations of these effector mechanisms include rhinitis, asthma, and anaphylaxis.