Premalignant Cervical Disease: CIN, Diagnosis & Treatment
advertisement

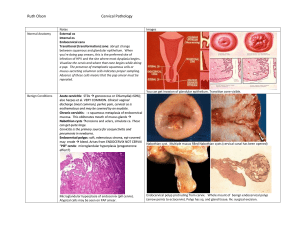
Dr shameem R. ALaasam Introduction Carcinoma of the cervix is the second commonest cancer among women worldwide, with only breast cancer occurring more commonly. While the natural history of breast cancer is poorly understood, cervical cancer is a preventable condition and considerable effort goes into detecting and treating the preinvasive disease CERVICAL INTRAEPITHELIAL NEOPLASIA CIN (formerly cervical dysplasia) refers to premalignant changes in the cervical epithelium that have the potential to progress to cervical cancer. CIN is most commonly diagnosed in women in their 20s; CIS is diagnosed most commonly in women of age 25 to 35 years; and invasive cancer is typically diagnosed after the age of 40. pathophysiology • The cervix is composed of the columnar epithelium, which lines the endocervical canal, and squamous epithelium, which covers the exocervix. • The point at which they meet is called as squamocolumnar junction (SCJ). • The SCJ rarely remains restricted to external os. Instead, it is a dynamic point that changes in response to puberty, pregnancy, menopause, and hormonal stimulation. • In neonates, SCJ is located on the exocervix. At menarche, the production of estrogen causes the vaginal epithelium to fill with glycogen. Lactobacilli act on the glycogen and lower the pH, stimulating the subcolumnar reserve cells to undergo metaplasia. Metaplasia advances from the original SCJ inward, toward the internal os and over the columnar villi. This process establishes an area called the transformation zone (TZ). The TZ extends from the original SCJ to the physiologically active SCJ. These metaplastic cells are more susceptible to oncogenic factors; therefore, CIN most commonly occurs during menarche and after pregnancy when metaplasia is most active. The transformation zone (TZ) is the site where premalignancy and malignancy develop. Normal cervix with transformation zone. Risk factors for CA cervix/CIN: a. Young age at first intercourse (<16 years) b. Multiple sexual partners c. Cigarette smoking d. Race e. High parity f. Low socioeconomic status g. Human papillomavirus (HPV) infection h. HIV i. Immunosuppression • HPV is now accepted as the primary causative agent in CIN and cervical cancer. DNA fragments of HPV have been found incorporated into the DNA of cells from 80% of all CIN lesions and 90% of all invasive cervical cancers. • There are more than 100 different serotypes of HPV. Serotypes 6 and 11 are among the types with the lowest oncogenic potential. They are responsible for causing 90% of condylomas. Serotypes 16 and 18 and 31 and 41 are of higher oncogenic potential. These so-called “high risk” types of HPV are responsible for about 70% (types 16 and 18) and 5% to 10% (types 31 and 45) of cervical cancers. • We are now able to test for high-risk HPV types in Pap smear specimens. This testing allows providers to more accurately predict which precancerous lesions have the potential to progress to cancer if left untreated and which will most likely spontaneously regress. • Moreover, HPV vaccines are now available (e.g., Gardasil and Cervarix) that prevent HPV infections and reduce the risk of cervical cancer by 70%. • Gardasil immunizes against types 6, 11, 16, and 18. • Cervarix immunizes against types 16, 18, 31, and 45. • Both are given as three injections over 6 months to males and females age 9-26. Classification of CIN CIN can be divided into low-grade (CIN 1) and high-grade disease (CIN 2 and 3). ØCIN I: Cellular dysplasia confined to the basal third of the epithelium (formerly mild dysplasia) ØCIN II (formerly moderate dysplasia), two-thirds of the epithelium is involved. ØCIN III (formerly severe dysplasia), more than two-thirds of the epithelium shows abnormal changes. The atypical cells in CIN III can expand the full thickness of the epithelium (formally CIS or carcinoma in situ). Histologic classification of cervical intraepithelial neoplasia (CIN). DIAGNOSIS Pap Smear Screening Because cervical dysplasia is otherwise asymptomatic, the Pap smear has revolutionized our ability to identify, monitor, and treat premalignant cervical changes before cancer arises. The goal of cytologic screening is to sample the TZ, the area where transformation from squamous epithelium to columnar endocervical epithelium takes place and where dysplasia and cancer arise. The Pap smear involves scraping endocervical and ectocervical cells from the external os of the cervix with a spatula to sample cells from the TZ . Because the squamocolumnar junction (SCJ) may be in the endocervical canal, it is important to also sample the endocervical canal with a cytobrush. The sample is then placed directly on a glass slide (conventional Pap smear) or into a liquid-based medium that is then used to make a slide. The prepared slides are then examined by a cytopathologist with or without aid of an automated cytology screening with pap smear alone every 3 years is acceptable for women 30 and over. A categorize infection i The ce (ASC) cat to infectio plastic les Pap smea treated. T appearing dysplasia t ASC-US ( ASC-H (a lesion). Pa ! TAB Abn ASC-US significa ASC-H: squamou LSIL: Lo B Figure 28-3 s Performing a Pap. (A) Spatula. (B) Endocervical brush. (From Bickley LS, Szilagyi P. Bates’ Guide to Physical Examination and History Performing a Pap. (A) Spatula. (B) Endocervical brush. Taking, 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2003.) HSIL: H SCC: Sq AGC: A Abnormal Pap Smear Management • Pap smear reports may show findings consistent with normal cellular material, inflammatory changes, infection, dysplasia, or cancer. • the major classes of epithelial abnormalities as they are reported using the 2001 Bethesda classification system. Major Classes of Epithelial Cell Abnormalities Found on Pap Smears • the ASC category has been divided into two groups: • ASC-US (atypical squamous cells of unknown significance) and ASC-H (atypical squamous cells—cannot rule out high-grade lesion). • Patients in the ASC-H category should be evaluated with colposcopy. Patients with ASC-US should undergo HPV testing to determine whether colposcopy is indicated or not. • Patients who receive an ASC-H, low-grade squamous intraepithelial lesion (LSIL), or high-grade squamous intraepithelial lesion (HSIL) Pap smear result should proceed directly to colposcopy Management of Abnormal Pap Smear Results in Adult Womena • Fortunately, many epithelial abnormalities found on Pap smears will regress to normal over 6 months to 2 years. Some of the abnormalities will persist at their current level, and the remainder will progress to more serious lesions or cervical cancer . • ASC and LSIL lesions usually represent a transient infection with HPV, so the majority will regress spontaneously over time. • However, HSIL lesions are more likely to be associated with persistent infection and progression to cancer. Therefore, patients who receive an ASC-H, LSIL, or HSIL Pap smear result should proceed directly to colposcopy Natural History of Cervical Intraepithelial Lesions HPV Testing • With the advent of HPV DNA testing, it is now recommended that women with an ASC-US result be tested immediately for the presence of high-risk HPV subtypes. This process is known as reflex HPV testing. • “Reflex” testing can be achieved using either the residual liquid from the liquid-based Pap test or a separate sample collected at the time of the initial Pap for HPV testing. • The HPV results are added to the initial Pap smear interpretation. This eliminates the need for the patient to return for repeat testing, and it allows the clinician to predict a patient’s risk for a high-grade lesion with more accuracy and to better direct the plan of care. • If the woman with an ASC-US Pap test is , where directed biopsies can be performed if indicated. • However, if the patient with an ASC-US Pap , she can continue with routine screening appropriate for her age COLPOSCOPY AND CERVICAL BIOPSY • Once a diagnosis of epithelial abnormalities has been made on Pap smear, a examination is needed to make the diagnosis of cervical dysplasia or cancer. • This histologic evaluation can be achieved during to determine the severity of dysplasia and to identify any invasive carcinoma. • Colposcopy is the outpatient examination of the magnified cervix using a light source . It is used for both diagnosis and treatment. • After a history and counselling, the woman undresses and places her legs in the semi-lithotomy position. A speculum is passed and the cervix examined with the light source under magnification (5 to 20 X). Usually 5 per cent acetic acid and iodine are applied to the cervix and biopsies taken when necessary. • Acetic acid causes nucleoproteins within cells to coagulate temporarily, therefore areas of increased cell turnover, for example in CIN will appear white at colposcopy . • Areas of CIN lack the presence of intracellular glycogen and therefore stain yellow as opposed to the normal squamous epithelium which will stain brown when iodine is applied. • Changes may include acetowhite epithelium, mosaicism, punctations, and atypical vessels • These lesions should be biopsied, and the specimens should be sent to pathology where more definitive histologic diagnoses can be made Cervix with acetic acid. Colposcope. Cervix with cervical intraepithelial neoplasia (CIN) and new vessels. Colposcopic view of the cervix. Abnormalities shown include acetowhite epithelium, punctations, and mosaic patterns. Treatment of Cervical Dysplasia • When the diagnosis of CIN is made on cervical biopsy, several treatments may ensue. • CIN I is commonly followed with repeat Pap smears (every 6 months for 12 months) or HPV testing in 1 year. If either the repeat Pap smears are abnormal or if the testing for high-risk HPV is positive, the patient should have a repeat colposcopy and biopsy if indicated. • If the repeat Pap smears are all within normal limits or if the patient is found to be HPV negative, the patient can return to routine cervical screening appropriate for her age • Women with CIN I that persists for more than 2 years or with CIN II may be treated with cryotherapy or surgical excision. • An alternative to treatment in young women with CIN II is observation with colposcopy and Pap testing every 6 months for 24 months. • Women with CIN III are treated with surgical excision. Historically, a coldknife conization (CKC) was performed, which removes a wedge-shaped portion of the cervical stroma and endocervical canal • This is no longer the standard of care for CIN. The loop electrosurgical excision procedure (LEEP) or large-loop excision of the transformation zone (Lletz) is now more commonly performed to treat CIN II and CIN III. • LEEP, loop, and Lletz all refer to the same procedure that involves removing a cone-shaped piece of cervical portio (conization), typically with a cauterized fine-wire loop or with a laser . • The LEEP can be performed as an office procedure under local anesthesia and is quicker and has less blood loss than the CKC. F Figure 28-5 s Cold-knife cone of the cervix. Figure 28-6 s Methods of cervical conization. (A) Cold-knife conization. (B) LEE (From Beckmann CRB, Ling FW, Laube DW, et al. Obstetrics and Gynecology, 4th ed. Wilkins; 2002.) Cold-knife cone of374 the cervix. Figure 28-5 s Cold-knife cone of the cervix. s of cervical conization. (A) Cold-knife conization. (B) LEEP/Lletz conization procedure. ng FW, Laube DW, et al. Obstetrics and Gynecology, 4th ed. Baltimore, MD: Lippincott Williams & LEEP/Lletz conization procedure. • In general, cervical excision procedures remove cervical tissue without causing extensive damage to the stroma of the cervix, although scarring of the endocervical canal may still ensue. Infrequent complications include • The persistence rate is about 4% for CIN II and CIN III and the recurrence rate is 10% and 15%, respectively. • Therefore, after surgical conization, patients should be followed every 6 months with a repeat Pap smear or repeat Pap smear and colposcopy for 1 year. If the results all remain normal, the patient can return to routine screening for at least 20 years. • Alternatively, after a cervical conization with unsatisfactory colposcopy, the patient can be followed with HPV testing every 6 months for 1 year after the procedure. If not high risk, the patient can return to routine screening for at least 20 years. • In either scenario, any abnormal cytology or the presence of high-risk HPV should result in repeat colposcopic examination and cervical biopsies if indicated. cervical cancer screening • The new guidelines recommend that all women should begin cervical cancer screening at age 21 regardless of risk factors, including age of onset of sexual activity. • Women aged 21 to 29 should have Pap testing every 3 years. • The preferred option for women aged 30 and above is to screen with both a Pap test and an HPV test, and if both are negative, to re-screen no sooner than every 5 years. • Co-testing with a Pap and an HPV test is 95% to 100% sensitive for CIN III. • If HPV testing is unavailable, screening with pap smear alone every 3 years is acceptable for women 30 and over. • It is reasonable for women over age 65 to 70 to stop cervical cancer screening if they have had three or more normal Pap tests in a row have not had CIN 2/3 or higher in the past 20 years, or if a woman has had a total hysterectomy (removal of both the uterine corpus and cervix) for benign indications (such as bleeding or fibroids) and she does not have a history of CIN 2/3 or higher, she may stop pap screening at the time of her hysterectomy. • Women with a history of CIN II or III who undergo hysterectomy may safely discontinue Pap smear screening after three consecutive negative screening tests (either the three most recent Pap smears prior to the hysterectomy or three consecutive screening examinations subsequent to the hysterectomy). • Importantly, women who have undergone a supracervical hysterectomy and have an intact cervix still need to continue routine Pap smear screening appropriate for their age.