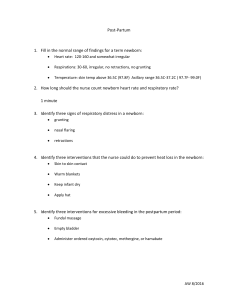
NCM 107 – Care of the Mother, Child and Adolescent S.Y. 2022-20223 | 1st Semester | Final Term Module 9: Care of a Newborn and Family Description This module covers the physiological changes that take place in the newborn during the process of transition. It gives emphasis on the role of the nurse during assessment and interventions to facilitate normal transition of the newborn. Learning Outcomes LO1 Integrate knowledge of newborn growth and development and immediate care needs with application of appropriate nursing care to the newborn and family of the newborn. LO3 Assess the newborn for normal growth and development. LO4 Formulate nursing diagnosis/es related to a newborn and the family of the newborn LO5 Implement safe and quality nursing interventions for a normal newborn. LO7 Evaluate with the mother and family the health outcomes of nurse-client relationship. Module Outline I. Normal characteristics of a term newborn II. Physiologic functioning of the newborn III. Nursing Diagnoses of the newborn and family IV. Outcome Identification and Planning V. Evaluating nursing care Module I. Normal Newborn Newborns undergo profound physiologic changes at the moment of birth (and, probably, psychological changes as well), as they are released from a warm, snug, dark, liquid-filled environment that has met all of their basic needs into a chilly, unbounded, brightly lit, gravitybased, outside world. Within minutes after being plunged into this strange environment, a Module 9: Care of a Newborn and Family 1 newborn has to initiate respirations and adapt a circulatory system to extrauterine oxygenation. Within 24 hours, neurologic, renal, endocrine, gastrointestinal, and metabolic functions must be operating competently for life to be sustained. VITAL STATISTICS Vital statistics measured in a newborn are weight, length, and head and chest circumference. (Table 1) • Weight A newborns weight is important because it helps to determine maturity as well as establish a baseline against which all other weights can be compared. The weight for all newborn is 2.5 kg (5.5 lbs) to 4.0 kg (8.75 lbs). During the first few days after birth, a newborn loses 5% to 10% of birth weight (6 to 10 oz). This physiologic weight loss is due to: 1. Withdrawal of fluid-retaining maternal hormones 2. Dieresis 3. Voids and passes stool 4. Limited intake especially for breast fed babies since colostrums is low in calorie. 5. Effective sucking is not yet established After this initial loss of weight, a newborn has 1 day of stable weight, then begins to gain weight. The breastfed newborn recaptures birth weight within 10 days; a formula-fed infant accomplishes this gain within 7 days. After this, a newborn begins to gain about 2 lb per month (6 to 8 oz per week) for the first 6 months of life • Length A newborn’s length at birth in relation to weight is a second important determinant uses to confirm that a newborn is healthy. The normal range of birth length is 18 to 22 inches (46 to 54 cm) • Head Circumference Module 9: Care of a Newborn and Family 2 Head circumference is measured with a tape measure drawn across the center of the forehead and then around the most prominent potion of the posterior head (the occiput). The head circumference is usually 34 to 35 cm (13.5 to 14 in). Less than 33 cm and more than 37 cm should be carefully assessed for neurologic involvement • Chest Circumference Chest circumference is measured at the level of the nipples. The chest circumference is about 3 cm less than head circumference VITAL SIGNS Vital sign measurements begin to change from those present in intrauterine life at the moment of birth. (Table 1) • Temperature The temperature of newborns is about 99° F (37.2° C) at birth because they have been confined in an internal body organ. The temperature falls almost immediately to below normal because: 1. immature temperature regulating mechanisms 2. low temperature of birthing rooms, approximately 68° to 72° F (21° to 22° C) 3. heat loss Newborns lose heat by four separate mechanisms: convection, conduction, radiation, and evaporation (Fig. 1). A. Convection is the flow of heat from the newborn’s body surface to cooler surrounding air. Eliminating drafts from windows or air conditioners reduces convection heat loss. B. Radiation is the transfer of body heat to a cooler solid object not in contact with the baby, such as a cold window or air conditioner. Moving an infant as far from the cold surface as possible helps reduce this type of heat loss. C. Conduction is the transfer of body heat to a cooler solid object in contact with a baby. For example, a baby placed on a cold counter or on the cold base of a warming unit quickly loses heat to the colder metal surface. Covering surfaces with a warmed blanket Module 9: Care of a Newborn and Family 3 or towel helps to minimize conduction heat loss. Placing the newborn on the mother’s abdomen immediately after birth and cover with a warm blanket for skin to skin contact (DOH, 2011). D. Evaporation is loss of heat through conversion of a liquid to a vapor. Newborns are wet, so they lose a great deal of heat as the amniotic fluid on their skin evaporates. To prevent this heat loss, dry newborns as soon as possible, especially their face and hair as the head, a large surface area in a newborn, can be responsible for a great amount of heat loss (DOH, 2011). Covering the hair with a cap after drying it further reduces the possibility of evaporation cooling. Be certain to remove any wet blankets used to dry the infant immediately and place the infant on a warm, dry blanket. Figure 1. (A) convection (B) Radiation (C) Conduction (D)Evaporation Newborns can conserve heat by: 1. constricting blood vessels and moving blood away from the skin; 2. brown fat, a special tissue found in mature newborns, in the intrascapular region, thorax, and perirenal area which warms the blood; 3. increasing metabolism by kicking and crying Module 9: Care of a Newborn and Family 4 Reaction of the newborn to heat loss are: 1. increase respiratory rate, 2. overexertion, thus fatigue 3. overstressed muscles, releasing lactic acid 4. acidosis All early care of newborns should be done speedily to avoid exposing the newborn to cool air unnecessarily. Any procedure during which a newborn must be uncovered such as resuscitation or circumcision should be done under a radiant heat source to prevent damaging heat loss. If chilling is prevented, a newborn’s temperature stabilizes at 98.6° F (37° C) within 4 hours after birth. • Pulse - Heart rate from 120-160 (in utero) to 180 immediately after birth - 120 to 140 one hour after birth - Irregular heart rate due to immaturity of the cardiac regulatory center in medulla - Transient murmurs may result from the incomplete closure of fetal circulation shunts. - During crying, the rate may rise again to 180 bpm while 90 to 110 bpm during sleeping - Brachial and femoral pulses are palpable but not the radial and temporal pulses - Newborn’s heart rate is always determined by listening for an apical heartbeat for a full minute, rather than assessing a pulse in an extremity. - Absent femoral pulses suggests possible coarctation (narrowing) of the aorta, a common cardiovascular abnormality. • Respiration - Respiratory rate at birth is 90 breaths per minute. - 30 to 60 breaths per minute when at rest. - Irregular in depth, rate, and rhythm Module 9: Care of a Newborn and Family 5 - Periods of apnea (without cyanosis) which last less than 15 seconds, sometimes called periodic respirations, are normal. - Respiratory rate can be observed most easily by watching the movement of a newborn’s abdomen, because breathing primarily involves the use of the diaphragm and abdominal muscles. - Coughing and sneezing reflexes are present at birth to clear the airway. - Newborns are obligate nose-breathers, however, and show signs of acute distress if their nostrils become obstructed. - Short periods of crying, which increase the depth of respirations and aid in aerating deep portions of the lungs, may be beneficial to a newborn. Long periods of crying, however, can exhaust the cardiovascular system. • Blood Pressure - Blood pressure of a newborn is approximately 80/46 mm Hg at birth. - By the 10th day, it rises to about 100/50 mm Hg. - BP not routinely measured unless a cardiac anomaly is suspected. - Blood pressure tends to increase with crying Table 1. Summary of the vital statistics and vital signs of the newborn Vital statistics Normal finding Weight 2.5 kg (5.5 lbs.) to 3.4kg (7.5 lbs.). Length 18 to 22 inches (46 to 54 cm) Head circumference 34 to 35 cm (13.5 to 14 in) Chest circumference 32 to 33 cm 3 cm less than head circumference Vital signs Normal finding Temperature 36.4°C to 37°C (97.6° F to 98.6°) axillary Apical pulse rate 120 to 140 bpm Module 9: Care of a Newborn and Family 6 Respiratory rate 30 to 60 breaths per minute Blood pressure 100/50 mmHg Apgar Scoring At 1 minute and 5 minutes after birth, newborns are observed and rated according to an Apgar score, an assessment scale used as a standard since 1958. As shown in Table 2 heart rate, respiratory effort, muscle tone, reflex irritability, and color of the infant are each rated 0, 1, or 2; the five scores are then added: - 0 to 3, newborn is in serious danger or respiratory car serious danger of respiratory or cardiovascular failure and needs resuscitation. - 4 to 6 means that the infant’s condition is guarded and the baby may need clearing of the airway and supplementary oxygen. - 7 to 10 indicates that the infant scored as high as 70% to 90% of all infants at 1 to 5 minutes after birth or is adjusting well to extrauterine life (10 is the highest score possible). Table 2. Apgar scoring. The Apgar score is repeated every additional 5 minutes, until a minimum score of 7 is reached. The Apgar score standardizes infant assessment at birth and serves as a baseline for future evaluations. The following points should be considered in obtaining an Apgar rating. Module 9: Care of a Newborn and Family 7 Heart Rate Auscultating a newborn heart with a stethoscope is the best way to determine heart rate; however, heart rate also may be obtained by observing and counting the pulsations of the cord at the abdomen if the cord is still uncut. Respiratory Effort Respirations are counted by watching respiratory movements. A mature newborn usually cries and aerates the lungs spontaneously at about 30 seconds after birth. By 1 minute, he or she is maintaining regular, although rapid, respirations. A depressed respiratory effort might be anticipated in a newborn whose mother received large amounts of analgesia or a general anesthetic during labor or birth. Muscle Tone Term newborns hold their extremities tightly flexed, simulating their intrauterine position. Muscle tone is tested by observing their resistance to any effort to extend their extremities. Reflex Irritability One of two possible cues is used to evaluate reflex irritability in a newborn: - Response to a suction catheter in the nostrils or - Response to having the soles of the feet slapped. A good response to these actions would be vigorous crying or a strong facial grimace. A baby whose mother was heavily sedated will probably demonstrate a low score in this category. Color All infants appear cyanotic at the moment of birth. They grow pink with or shortly after the first breath, which makes the color of newborns correspond to how well they are breathing. Acrocyanosis (cyanosis of the hands and feet) is so common in newborns that a score of 1 in this category can be thought of as normal. Physical Assessment HEAD Module 9: Care of a Newborn and Family 8 - A newborn’s head appears disproportionately large because it is about one fourth of the total body length - The fontanelles are the spaces or openings where the skull bones join. The anterior fontanelle is a diamond shaped which closes between 12-18 months; the posterior fontanelle is triangular shaped which closes between 2-3 months. - The anterior fontanelle can be felt as a soft spot. It should not appear indented (a sign of dehydration) or bulging (a sign of increased intracranial pressure) when the infant is held upright. The fontanelle may bulge if the newborn strains to pass a stool or cries vigorously or is lying supine. With vigorous crying, a pulse may additionally be seen in the fontanelle. - Molding results when the part of the infant’s head that engaged the cervix (usually the vertex) molds to fit the cervix contours during labor. After birth, this area appears prominent and asymmetric and appears as a dunce cap. The head will restore to its normal shape within a few days after birth. - Caput succedaneum is edema of the scalp at the presenting part of the head. It may involve wide areas of the head, or it may resemble a large egg. The edema, which crosses the suture lines, is gradually absorbed and disappears at about the third day of life. It needs no treatment. - Cephalhematoma, a collection of blood between the periosteum of a skull bone and the bone itself, is caused by rupture of a periosteal capillary because of the pressure of birth. Swelling usually appears 24 hours after birth and confined to an individual bone, so the associated swelling stops at the bone’s suture line. It often takes weeks to be absorbed. - Craniotabes is a localized softening of the cranial bones that is probably caused by pressure of the fetal skull against the mother’s pelvic bone in utero. The skull is so soft that the pressure of an examining finger can indent it. The bone returns to its normal contour after the pressure is removed. The condition corrects itself without treatment after a few months, as the infant takes in calcium in milk. - Head lag is common when pulling the newborn to a sitting position. When prone, the newborn should be able to lift the head slightly and turn the head from side to side. Module 9: Care of a Newborn and Family 9 EYES - Newborns usually cry tearlessly, because their lacrimal ducts do not fully mature until about 3 months of age. - Gray or blue irises; the sclera may be blue because of its thinness. Infant eyes assume their permanent color between 3 and 12 months of age. - A newborn’s eyes should appear clear, without redness or purulent discharge. - Antibiotic ointment such as erythromycin given at birth, to protect against Chlamydia infection and ophthalmia neonatorum (gonorrheal conjunctivitis) - Subconjunctival hemorrhage due to pressure during birth ruptures a conjunctival capillary of the eye. This appears as a red spot on the sclera, usually on the inner aspect of the eye, or as a red ring around the cornea. The bleeding is slight, requires no treatment, and is completely absorbed within 2 or 3 weeks. - Eyelids often edematous as a result of pressure during birth process and the effects of eye medication. - Round and proportionate size cornea. - Eyes cross because of weak extraocular muscles - Newborns demonstrate sight at birth by blinking at a strong light (blink reflex) or by following a bright light or toy a short distance with their eyes. Because they cannot follow past the midline of vision, they lose track of objects easily. - Newborns focus best on black and white objects at a distance of 9 to 12 in. - A pupillary reflex or ability to contract the pupil is present from birth. EARS - Pinna tends to bend easily; recoils after bending - Top of the pinna should be on a line drawn from the inner canthus to the outer canthus of the eye and back across the side of the head - Low set ears are found in infants with certain chromosomal abnormalities: trisomy 18 and 13. Module 9: Care of a Newborn and Family 10 - A small tag of skin is sometimes found just in front of an ear. Although these tags may be associated with chromosomal abnormalities or kidney disease, they usually are isolated findings that are of no consequence - A preauricular dermal sinus, a pinpoint-size openings in the external ear. - A fetus is able to hear in utero even before birth. As soon as amniotic fluid drains or is absorbed from the middle ear by way of the eustachian tube—within hours after birth— hearing becomes acute. They have difficulty locating the sound but are usually startled with loud noise and calms with the mother’s voice. NOSE - Appear large for the face. - Test for choanal atresia (blockage at the rear of the nose) by closing the newborn’s mouth and compressing one naris at a time with your fingers. Note any discomfort or distress while breathing this way. - Nasal flaring upon inspiration is another indication of respiratory distress and should be further evaluated. - Milia, a clogged sebaceous gland, on the nose. - The sense of smell is present in newborns as soon as the nose is clear of lung and amniotic fluid. Newborns turn toward their mothers’ breast partly out of recognition of the smell of breast milk and partly as a manifestation of the rooting reflex. MOUTH - Opens evenly when newborn cries. If one side of the mouth moves more than the other, cranial nerve injury is suggested. - Tongue appears large and prominent in the mouth. - Epstein’s pearls, one or two small, round, glistening, well circumscribed cysts are present on the palate, a result of extra calcium that was deposited in utero, and will disappear spontaneously within 1 week. - If the mouth is filled with so much mucus that a neonate seems to be blowing bubbles, a tracheoesophageal fistula is suspected. This must be confirmed or ruled out before the Module 9: Care of a Newborn and Family 11 newborn is fed; otherwise, formula can be aspirated into the lungs from the inadequately formed esophagus. - It is unusual for a newborn to have teeth, but sometimes one or two (called natal teeth) will have erupted. Any teeth that are present must be evaluated for stability. If loose, should be removed to prevent aspiration - A newborn has the ability to discriminate taste, because taste buds are developed and functioning even before birth A newborn turns away from a bitter taste such as salt but readily accepts the sweet taste of milk or glucose water. NECK - The neck is short and often chubby, with creased skin folds. The head should rotate freely on it. - If there is rigidity of the neck, congenital torticollis, caused by injury to the sternocleidomastoid muscle during birth, might be present. - In newborns whose membranes were ruptured more than 24 hours before birth, nuchal rigidity suggests meningitis. - The neck of a newborn is not strong enough to support the total weight of the head but in a sitting position, a newborn should make a momentary effort at head control. CHEST - The chest in some newborns looks small because the head is large in proportion. It is actually approximately 2 inches smaller in circumference and as wide in the anteroposterior diameter as it is across. Not until a child is 2 years of age does the chest measurement exceed that of the head. - Respirations are normally rapid (30 to 60 breaths per minute) but not distressed. - Clavicles should be palapated for fractures - In both female and male infants, the breasts may be engorged due to maternal hormones - Witch’s milk, watery fluid from the breasts is common due to maternal hormones. - Retraction (drawing in of the chest wall with inspiration) should not be present. Module 9: Care of a Newborn and Family 12 - An abnormal sound, such as grunting, suggests respiratory distress syndrome; a high, crowing sound on inspiration suggests stridor or immature tracheal development. ABDOMEN - The contour of a newborn abdomen looks slightly protuberant. A scaphoid or sunken appearance may indicate missing abdominal contents or a diaphragmatic hernia (bowel positioned in the chest instead of the abdomen). - Bowel sounds should be present within 1 hour after birth. - The stump of the umbilical cord appears as a white, gelatinous structure marked with the blue and red streaks of the umbilical vein and arteries during the first hour after birth. - After the first hour of life, the cord begins to dry and shrink, and it turns brown like the dead end of a vine. By the second or third day, it has turned black. It breaks free by day 6 to 10, leaving a granulating area a few centimeters wide that heals during the following week. - There should be no bleeding at the cord site. Bleeding suggests that the cord clamp has become loosened, or the cord has been tugged loose by the friction of bedclothes. The base of the cord should appear dry. A moist or odorous cord suggests infection. - Moistness at the base of the cord also may indicate a patent urachus (a canal that connects the bladder and the umbilicus), which will drain urine at the cord site until it is surgically repaired. MALE GENITALIA - The scrotum in most male newborns is edematous and has rugae (folds in the skin). - Both testes should be present in the scrotum. If one or both testicles are not present (cryptorchidism), referral is needed to establish the extent of the problem. - Prepuce (foreskin) covers glans penis - Urethral opening at the tip of the penis FEMALE GENITALIA - The vulva in female newborns may be swollen because of the effect of maternal hormones. - Pseudomenstruation is a blood-tinged vaginal secretion due to maternal hormones is common. Module 9: Care of a Newborn and Family 13 ANUS - Anal opening is present - First stool within first 24 hours SPINE - Back is straight and posture flexed - Chin flexed on upper chest - A degree of hypotonicity or hypertonicity may indicate central nervous system damage. - Hair tuffs and dimples along the spinal column may be indicative of spinal opening. EXTREMITIES - Flexed and full range of motion, symmetrical - Fists clenched - Ten fingers and ten toes, all separate - Legs bowed and major gluteal folds are even - Creases on soles of feet - Absent fractures or dislocation - Slight tremors noted in the newborn may be a common finding but also be a sign of hypoglycemia, hypocalcemia, or drug withdrawal SKIN - Pinkish red (light-skinned newborn) to pinkish brown or pinkish yellow (dark-skinned newborn) - Vernix caseosa, a cheesy white substance, on entire body in preterm newborns, but is more prominent between folds closer to term; may be absent after 42 weeks of gestation. - Lanugo, fine body hair, might be seen, especially on the back. - Milia, small white sebaceous glands, appear on the forehead, nose, and chin - Desquamation, dry peeling skin, is increased in postmature newborns - Cyanosis may be noted with hypothermia, infection, and hypoglycemia and with cardiac, respiratory, or neurological abnormalities. Module 9: Care of a Newborn and Family 14 - Acrocyanosis (peripheral cyanosis of hands and feet) is normal in the first few hours after birth and may be noted intermittently for the next 7 to 10 days. - Erythema Toxicum appears in the first to fourth day of life but may appear up to 2 weeks of age. It begins with a papule, increases in severity to become erythema by the second day, and then disappears by the third day. It is sometimes called a flea-bite rash because the lesions are so minuscule. - Forceps are rarely used for birth today but if they are used, they may leave a circular or linear contusion matching the rim of the blade of the forceps on the infant’s cheek. This mark disappears in 1 to 2 days, along with the edema that accompanies it. - Skin turgor over abdomen to determine hydration status. - Harlequin sign is a deep pink or red color develops over one side of newborn’s body while the other side remains pale or of normal color. It indicates shunting of blood that occurs with a cardiac problem or may indicate sepsis. - Birthmarks (Fig. 2) o Nevus flammeus or portwine stain – capillary angioma directly below epidermis; non elevated, sharply demarcated, red to purple, dense areas of capillaries commonly found in face and thigh. No fading with time and may require future surgery o Telangiectatice nevi or stork bites – pale pink or red, flat, dilated capillaries on eyelids, nose, lower occipital bone, and nape of neck which blanched easily. It is more noticeable during crying periods, disappears o Nevus vasculosus or strawberry mark – capillary hemangioma, raised, clearly delineated, dark red, with rough surface common in head region. It disappears by age 7-9 years old. o Mongolian spots – bluish-black pigmentation on lumbar dorsal area and buttocks. It gradually fades during first and second year of life. Common in Asian and darkskinned individuals. Module 9: Care of a Newborn and Family 15 Figure 2. Birthmarks Types of hemangiomas found on a newborn. (A) Nevus flammeus (port-wine stain) (B) A telangectasia or stork’s beak mark(C) Strawberry hemangiomas (D) Cavernous hemangiomas II. Physiologic Adjustment to Extrauterine Life All newborns seem to move through periods of irregular adjustment in the first 6 hours of life, before their body systems stabilize. Demonstration of this typical reactivity pattern, therefore, is an indication that a newborn is healthy and adjusting well to extrauterine life. The ability to transition from one period to another is an important indicator of neurologic status Table 1. A. The first period of reactivity. The first phase lasts about half an hour. During this time, the baby is alert and exhibits exploring, searching activity, often making sucking sounds. Heart beat and respiratory rate are rapid. B. Resting Period Module 9: Care of a Newborn and Family 16 Next comes a quiet resting period. Heartbeat and respiratory rates slow, and the newborn typically sleeps for about 90 minutes. C. The second period of reactivity This period occurs between 2 and 6 hours of life, occurs when the baby wakes again, often gagging and choking on mucus that has accumulated in the mouth. He or she is again alert and responsive and interested in surroundings. These three periods are summarized in Table 18.1. Newborns who are ill or who had difficulty at birth may not pass through these typical stages; they may never have periods of alertness or periods of quiet. Their vital signs may not fall and rise again but remain rapid; their temperature may remain subnormal. Figure 3. Periods of Reactivity: Normal Adjustment to Extrauterine Life Physiologic Function Just as changes occur in vital signs after birth, so do changes occur in all the major body systems. Cardiovascular System Module 9: Care of a Newborn and Family 17 Changes in the cardiovascular system are necessary after birth because now the lungs must oxygenate the blood that was formerly oxygenated by the placenta. When the cord is clamped, a neonate is forced to take in oxygen through the lungs. As soon the umbilical cord is clamped, which stimulates a neonate to take in oxygen through the lungs, fetal cardiovascular shunts begin to close. With the first breath, blood pressure decreases in the pulmonary artery (the artery leading form the heart to the lungs). As this pressure decreases, the ductus arteriosus begins to close. At the same time, increased blood flow to the left side of the heart causes the foramen ovale to close because of the pressure against the lip of the structure. With the remaining fetal circulatory shunts (umbilical vein and arteries and ductus venosus) no longer receiving blood from the placenta, the blood within them clots and closes them, and the vessels atrophy over the next few weeks (Fig. 3). The peripheral circulation of a newborn remains sluggish for at least the first 24 hours. It is common to observe cyanosis in the infant’s feet and hands (acrocyanosis) and for the feet to feel cold to the touch at this time. • Blood Values: - A newborn’s blood volume is 80 to 110 mL per kilogram of body weight, or about 300 mL total. - Hemoglobin 17 to 18 g/100 ml - Hematocrit 45% to 50% - Red blood cell count 6 million cells/mm3 - Indirect bilirubin 1-4 mg/100ml - White blood cell count 15,000 to 30,000 cells/mm3 at birth, increases to 40,000 cells/mm3 if birth was stressful • Blood Coagulation: - Vitamin K, synthesized through the action of intestinal flora, responsible for the formation of clotting factors. Because a newborn’s intestine is sterile at birth unless Module 9: Care of a Newborn and Family 18 membranes were ruptured more than 24 hours before birth, it takes about 24 hours for flora to accumulate and for vitamin K to be synthesized. This causes most newborns to be born with a lower than usual level of vitamin K, leading to prolonged coagulation or prothrombin. - Vitamin K (Aquamephyton) 1 mg is administered intramuscularly at the vastus lateralis or upper 2/3 of the thigh. Figure 3. Circulatory events at birth Respiratory System A first breath is a major undertaking because it requires a tremendous amount of pressure (about 40 to 70 cm H2O). It is initiated by a combination of cold receptors; a lowered partial pressure of oxygen (PO2), which falls from 80 to as low as 15 mm Hg before a first breath; and Module 9: Care of a Newborn and Family 19 an increased partial carbon dioxide pressure (PCO2), which rises as high as 70 mm Hg before a first breath. Some fluids present in the lungs from intrauterine life makes a newborn’s first breath possible because fluid eases surface tension on alveolar walls and allows alveoli to inflate more easily than if the lung walls were dry. About one third of this fluid is forced out of the lungs by the pressure of vaginal birth, however in in CS fluid is not expelled which makes it difficult to establish respiration. The rest of the fluid is quickly absorbed by lung blood vessels and lymphatics after the first breath. Once the alveoli have been inflated with a first breath, breathing becomes much easier for a baby, requiring only about 6 to 8 cm H2O pressure. Within 10 minutes after birth, most newborns have established a good residual volume. By 10 to 12 hours of age, vital capacity is established at newborn proportions. Gastrointestinal System - Gastrointestinal tract is usually sterile at birth - Bacteria present within 5 hours to 24 hours of life which entered the tract through the newborn’s mouth from airborne source or from vaginal secretions at birth, from hospital bedding, and from contact at the breast. - Bacteria are necessary for digestion and for the synthesis of vitamin K. - Newborn’s stomach holds about 60 to 90 mL - Limited ability to digest fat and starch because the pancreatic enzymes, lipase and amylase, remain deficient for the first few months of life. - Regurgitates easily because of an immature cardiac sphincter between the stomach and esophagus. - Immature liver functions may lead to lowered glucose and protein serum levels. Stools Module 9: Care of a Newborn and Family 20 - Meconium, the first stool of a newborn, is usually passed within 24 hours after birth; consists of, a sticky, tarlike, blackish-green, odorless material formed from mucus, vernix, lanugo, hormones, and carbohydrates that accumulated during intrauterine life. - Absent meconium stool by 24 to 48 hours after birth, the possibility of some factor such as meconium ileus, imperforate anus, or volvulus should be suspected. - Transitional stool is a green loose stool at about the second or third day of life - For breastfed babies, three or four light yellow stools per day that are sweet-smelling, because breast milk is high in lactic acid, which reduces the amount of putrefactive organisms in the stool. - For formula fed babies, two or three bright yellow stools a day, slightly more noticeable odor, compared with the stools of breastfed babies. - Bright green stools for newborn placed under phototherapy lights as therapy for jaundice - Clay-colored (gray) stools indicate bile duct obstruction because bile pigments cannot enter the intestinal tract. - Blood-flecked stools usually indicate an anal fissure. - Mucus is mixed with stool, watery, and loose may indicate milk allergy, lactose intolerance, or conditions interfering with normal digestion of absorption. Urinary System - Newborn voids within 24 hours after birth. - Absent urine within 24 hours should be assessed for the possibility of urethral stenosis or absent kidneys or ureters. - Males should void with enough force to produce a small projected arc; - Females should produce a steady stream, not just continuous dribbling. - The kidneys of newborns do not concentrate urine well, making newborn urine usually light-colored and odorless. The infant is about 6 weeks of age before much control over reabsorption of fluid in tubules and concentration of urine becomes evident. Module 9: Care of a Newborn and Family 21 - A single voiding in a newborn is only about 15 mL and may be easily missed in a thick diaper. - Specific gravity ranges from 1.008 to 1.010. - The daily urinary output for the first 1 or 2 days is about 30 to 60 mL total. By week 1, total daily volume rises to about 300 mL. - The first voiding may be pink or dusky because of uric acid crystals that were formed in the bladder in utero; this is an innocent finding. A small amount of protein may be normally present in voidings for the first few days of life, until the kidney glomeruli are more fully mature. - Diapers can be weighed to determine the amount of urine output. The immune system - Newborns have limited immunologic protection at birth because they are not able to produce antibodies until about 2 months - Born with passive immunity against poliomyelitis, measles, diphtheria, pertussis, chickenpox, rubella and tetanus: IgG (while in utero thru placenta) - Receives passive immunity from colostrums (IgA) - Give Hepatitis B vaccine and BCG (DOH) Neuromuscular System - Term newborns demonstrate neuromuscular function by moving their extremities, attempting to control head movement, exhibiting a strong cry, and demonstrating newborn reflexes. - Limpness or total absence of a muscular response to manipulation is abnormal and suggests narcosis, shock, or cerebral injury. - Occasional twitching or flailing movements of the extremities in the absence of a stimulus is normal because of the immaturity of the nervous system. - Newborn reflexes can be tested with consistency by using simple maneuvers Module 9: Care of a Newborn and Family 22 Reflexes The Blink Reflex - To protect the eye from any object coming near it by rapid eyelid closure. - It may be elicited by shining a strong light such as a flashlight or an otoscope light on an eye. A sudden movement toward the eye sometimes can elicit the blink reflex The Rooting Reflex - If the cheek is brushed or stroked near the corner of the mouth, a newborn infant will turn the head in that direction. - Serves to help a newborn find food: when a mother holds the child and allows her breast to brush the newborn’s cheek, the reflex makes the baby turn toward the breast. - Disappears at about the sixth week of life when eyes can focus steadily and food source can be seen. The Sucking Reflex - When a newborn’s lips are touched, the baby makes a sucking motion. The reflex helps a newborn find food: when the newborn’s lips touch the mother’s breast or a bottle, the baby sucks and so takes in food. - The sucking reflex begins to diminish at about 6 months of age. - It disappears immediately if it is never stimulated such as in a newborn with a tracheoesophageal fistula who cannot take in oral fluids. It can be maintained in such an infant by offering the child a non-nutritive sucking object such as a pacifier . The Swallowing Reflex - Food that reaches the posterior portion of the tongue is automatically swallowed (like in adults). - Gag, cough, and sneeze reflexes also are present in newborns to maintain a clear airway The Extrusion Reflex Module 9: Care of a Newborn and Family 23 - A newborn extrudes any substance that is placed on the anterior portion of the tongue. - This protective reflex prevents the swallowing of inedible substances. - It disappears at about 4 months of age. Until then, the infant may seem to be spitting out or refusing solid food placed in the mouth. The Palmar Grasp Reflex - Newborns grasp an object placed in their palm by closing their fingers on it. - Term newborns grasp so strongly that they can be raised from a supine position and suspended momentarily from an examiner’s fingers. - It disappears at about 6 weeks to 3 months of age. A baby begins to grasp meaningfully at about 3 months of age. The Step (Walk)-in-Place Reflex - Newborns who are held in a vertical position with their feet touching a hard surface will take a few quick, alternating steps - It disappears by 3 months of age. By 4 months, babies can bear a good portion of their weight unhindered by this reflex. The Placing Reflex - It is elicited by touching the anterior lower leg against a surface such as the edge of a table. The newborn makes a few quick lifting motions, as if to step onto the table. The Plantar Grasp Reflex - When an object touches the sole of a newborn’s foot at the base of the toes, the toes grasp in the same manner as do the fingers. - It disappears at about 8 to 9 months of age in preparation for walking. The Tonic Neck Reflex - When the arm and leg on the side toward which the head is turned extend, and the opposite arm and leg contract. - If you turn a newborn’s head to the opposite side, he or she will often change the extension and contraction of legs and arms accordingly. Module 9: Care of a Newborn and Family 24 - This is also called a boxer or fencing reflex, because the position simulates that of someone preparing to box or fence. - The reflex disappears between the second and third months of life. The Moro Reflex - A Moro (startle) reflex can be initiated by startling a newborn with a loud noise or by jarring the bassinet. - The most accurate method of eliciting the reflex is to hold newborns in a supine position and allow their heads to drop backward about 1 inch. - In response to this sudden head movement, the newborn first extends arms and legs, then swings the arms into an embrace position and pulls up the legs, then swings the arms into an embrace position and pulls up the legs against the abdomen. - It is strong for the first 8 weeks of life and then fades by the end of the fourth or fifth month. - A perisistent response lasting more than 6 months may indicate a neurological abnormality The Babinski Reflex - When the sole of the foot is stroked in an inverted “J” curve from the heel upward, a newborn fans the toes. This is in contrast to the adult, who flexes the toes. - This reaction occurs because nervous system development is immature. It remains positive (toes fan) until at least 3 months of age, when it is supplanted by the downturning or adult flexion response. - It disappears after 1 year old - Absence of this reflex indicates the need for a neurological examination The Magnet Reflex - If pressure is applied to the soles of the feet of a newborn lying in a supine position, he or she pushes back against the pressure. - This and the two following reflexes are tests of spinal cord integrity. The Crossed Extension Reflex Module 9: Care of a Newborn and Family 25 - When a newborn is lying supine, if one leg is extended and the sole of that foot is irritated by being rubbed with a sharp object, such as a thumbnail, the infant raises the other leg and extends it, as if trying to push away the hand irritating the first leg. The Trunk Incurvation Reflex - When newborns lie in a prone position and are touched along the paravertebral area by a probing finger, they flex their trunk and swing their pelvis toward the touch (Fig. 18.9). The Landau Reflex - When a newborn is supported in a prone position by a hand, the newborn should demonstrate some muscle tone. A newborn may not be able to lift the head or arch the back in this position but neither should the infant sag into an inverted “U” position. The latter response indicates extremely poor muscle tone, which needs to be investigated. The Deep Tendon Reflexes - A patellar reflex can be elicited in a newborn by tapping the patellar tendon with the tip of the finger. The lower leg moves perceptibly if the infant has an intact reflex. - A patellar reflex is a test for spinal nerves L2–L4. - To elicit a biceps reflex, place the thumb of your left hand on the tendon of the biceps muscle on the inner surface of the elbow. Tap the thumb as it rests on the tendon. You are more likely to feel the tendon contract than to observe movement. III. A biceps reflex is a test for spinal nerves C5 and C6 Essential Newborn Care (ENC) The majority of babies are born healthy and at term. The care they receive during the first hours, days and weeks of life can determine whether they remain healthy. All babies need basic care to support their survival and wellbeing. This basic care is called essential newborn care (ENC) and it includes immediate care at birth, care during the first day and up to 28 days. Module 9: Care of a Newborn and Family 26 The essential newborn care also known as “Unang Yakap” is a series of time bound chronologically – ordered, standard procedures that a baby receives at birth. At the heart of the protocol are four time-bound interventions: 1. Immediate drying prevents hypothermia, which is extremely important to survival. 2. Delayed cord clamping until the umbilical cord stops pulsating decreases anemia in one out of every three premature babies and prevents brain hemorrhage in one out of two. 3. Keeping the mother and baby in uninterrupted skin to skin contact prevents hypothermia, increases colonization with protective family bacteria and imporves breastfeeding initiation and exclusivity. 4. Breast feeding within the first hour of life prevents an estimated 19.1% of all neonatal deaths Immediate Newborn Care I. The First 90 minutes A. Prepare for the delivery - At perineal bulging, with presenting part visible (2nd stage of labor) - Ensure that delivery are is draft-free and between 25-28oC using a room thermometer - Wash hands with clean soap and water - Double glove just before delivery B. Dry and provide warmth – within first 30 seconds - Call out the time of birth - Use a clean, dry cloth to thoroughly dry the baby by wiping the eyes, face, head, front and back, arms and legs. - Remove the wet cloth - Do a quick check of newborn’s breathing while drying. - During the first 30 seconds: Do not ventilate unless the baby is floppy/limp and not breathing; do not suction unless the mouth/nose are blocked with secretions or other material. C. Do skin-to-skin contact – after 30 seconds Module 9: Care of a Newborn and Family 27 - If a baby is crying and breathing normally, avoid any manipulation, such as routine suctioning, that may cause trauma or introduce infection. - Place the newborn prone on the mother’s abdomen or chest skin-to-skin. - Cover newborn’s back with blanket and head with a bonnet - Place identification band on ankle D. Do delayed or non-immediate cord clamping – 1-3 minutes - Remove the set of gloves immediately prior to cord clamping. - Clamp and cut the cord after cord pulsations have stopped (1-3 minutes) - Put ties tightly around the cord at 2cm and 5cm from newborn’s abdomen - Cut between ties with sterile instrument - Observe for oozing blood - Do not milk the cord towards the newborn - After cord clamping, ensure 10 IU IM is given to the mother. E. Provide support for initiation of breastfeeding – within 90 minutes - Leave the newborn on mother’s chest in skin-to-skin contact. - Observe the newborn for feeding cues: opening mouth, tonguing, licking, rooting - Make verbal suggestions to the mother to encourage her newborn to move toward the breast e.g. nudging - Counsel on positioning and attachment, when the baby is ready, advise the mother to: o Make sure the newborn’s neck is not flexed or twisted. o Make sure the newborn is facing the breast, with the newborn’s nose opposite her nipple an chin touching the breast o Hold the newborn’s body close to her body. o Support the newborn’s whole body, not just the neck and the shoulders. F. Do eye care - Administer erythromycin or tetracycline ointment or 2.5% providone-iodine drops to both eyes after newborn has located breast. - Do not wash away the eye antimicrobial. Module 9: Care of a Newborn and Family 28 II. From 90 minutes to 6 hours A. Give Vitamin K prophylaxis – 90 mins to 6 hours - Inject single dose of Vitamin K 1 mg IM at the vastus lateralis B. Inject hepatitis B and BCG vaccination at birth - Inject hepatitis B vaccine IM at the vastus lateralis - Inject BCG intradermally at the right upper arm - Record C. Examine the baby - Thoroughly examine the baby - Weigh the baby and record D. Check for birth injuries and malformations or defects. - Look for possible birth injury. - Look for malformations E. Cord Care - Put nothing on the stump - Fold diaper below the stump. Keep cord stump loosely covered with clean clothes. - If stump is soiled, wash it with clean water and soap. Dry it thoroughly with clean cloth. - Explain to the mother that she should seek care if the umbilicus is red or draining pus. - Do not bandage the stump or abdomen - Do not apply any substances or medicine on the stump - Avoid touching the stump unnecessarily Newborn care practices in the delivery room that should no longer be continued The following practices should never be done anymore to the newborn: • Manipulation such as routine suctioning of secretions if the baby is crying and breathing normally. Doing so may cause trauma or introduce infection. • Putting the newborn on a cold or wet surface. • Wiping or removal of vernix caseosa if present Module 9: Care of a Newborn and Family 29 • Foot printing • Bathing earlier than 6 hours of life • Unnecessary separation of the newborn primarily for weighing, anthropometric measurements, intramuscular administration of vitamin K, Hepatitis B vaccine and BCG vaccine • Transferring of the newborn to the nursery or neonatal intensive care unit without any indication NEEDS OF THE NEWBORN A. THE INITIAL FEEDING The Baby-Friendly Hospital Initiative (BFHI) is a global sponsored by the WHO to encourage and recognize hospitals and birthing centers that offer an optimal level of care for infants that promotes breastfeeding. To qualify as a Baby-Friendly – designated facility, as setting must: 1. Maintain a written breastfeeding policy that is routinely communicated to all healthcare staff. 2. Educate all healthcare staff in skills necessary to implement the written policy. 3. Inform all pregnant women about the benefits and management of breastfeeding. 4. Help mothers initiate breastfeeding within 1 hour of birth. 5. Show mothers how to breastfeed and how to maintain their milk supply, even if they are separated from their infants. 6. Offer breastfed newborns no food or drink other than breast milk unless medically indicated. 7. Practice “rooming in” or allow mothers and infants to remain together 24 hours a day. 8. Encourage unrestricted or “on-demand” breastfeeding. 9. Give breastfeeding infants no pacifiers or artificial nipples. Module 9: Care of a Newborn and Family 30 10. Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the birth setting. The Mother-Baby Friendly Hospital Initiative (MBFI), the name for the Filipino version of the initiative, was launched by the Department of Health in 1992 in line with the Roomingin and Breastfeeding Act of 1992 (RA 7600). In this law, all private and government private hospitals offering maternity and newborn care may be accredited as Mother-Baby Friendly if they implement the 10 Steps to Successful Breastfeeding adopted from UNICEF/WHO criteria of BFI. After a first feeding in the birthing room, both formula-fed and breastfed infants do best with an “on-demand” schedule (i.e., are fed when they are hungry). Many need to be fed as often as every 1.5 to 2 hours in the first few days and weeks of life. B. BATHING Bathing should be delayed until 24 hours after birth. If this is not possible due to cultural reasons, bathing should be delayed for at least six hours. Appropriate clothing of the baby for ambient temperature is recommended. This means one to two layers of clothes more than adults, and use of hats/caps. The mother and baby should not be separated and should stay in the same room 24 hours a day. Bathing of an infant is best done by the parents under a nurse’s supervision. Be sure the room is warm (about 75° F [24° C]), to prevent chilling. Bath water should be approximately 98° to 100° F (37° to 38° C), a temperature that feels pleasantly warm to the elbow or wrist. If soap is used, it should be mild and without a hexachlorophene base. Bathing should take place before, not after, a feeding, to prevent spitting up or vomiting and possible aspiration. Equipment necessary for an infant’s bath consists of a basin of water, soap, washcloth, towel, comb, and clean diaper and shirt. Assemble these items Module 9: Care of a Newborn and Family 31 beforehand, so the baby is not left exposed or unattended while you go for more equipment. Bathing should proceed from the cleanest to the most soiled areas of the body—that is, from the eyes and face to the trunk and extremities and, last, to the diaper area. Wipe a newborn’s eyes with clear water from the inner canthus outward, using a clean portion of the washcloth for each eye to prevent spread of infection to the other eye. Wash the face with clear water only (no soap) to avoid skin irritation; soap may be used on the rest of the body. C. SLEEPING POSITION Stress to parents that a newborn should be positioned on the back for sleep. Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an infant younger than 1 year of age. Although the specific cause of SIDS cannot be explained, placing infants to sleep in a supine position with a pacifier has been shown to decrease the incidence of the syndrome. As one of the reasons that SIDS may occur is the infant rebreathing expired carbon dioxide–rich air, using a fan in the room during sleep or opening a window so there is a breeze in the room may be yet another way the incidence of SIDS can be reduced. D. DIAPER CARE AREA Preventing diaper dermatitis is a practice that parents need to start from the very beginning with their newborns. With each diaper change, the area should be washed with clear water and dried well, to prevent the ammonia in urine from irritating the infant’s skin and causing a diaper rash. After cleaning, a mild ointment such as petroleum jelly or A & D Ointment may be applied to the buttocks. The ointment keeps ammonia away from the skin and also facilitates the removal of meconium, which is sticky and tarry. Wear gloves for diaper care as part of standard precautions. Module 9: Care of a Newborn and Family 32 E. NEWBORN SCREENING PROGRAM Newborn screening program in the Philippines currently includes screening of six disorders: congenital hypothyroidism (CH), congenital adrenal hyperplasia (CAH), phenylketonuria (PKU), glucose-6- phosphate dehydrogenase (G6PD) deficiency, galactosemia (GAL) and maple syrup urine disease (MSUD). The expanded screening will include 22 more disorders such as hemoglobinopathies and additional metabolic disorders, namely, organic acid, fatty acid oxidation, and amino acid disorders. The latter are included in the standard care across the globe. The Comprehensive Newborn Screening (NBS) Program was integrated as part of the country’s public health delivery system with the enactment of the Republic Act no. 9288 otherwise known as Newborn Screening Act of 2004. The Department of Health (DOH) acts as the lead agency in the implementation of the law and collaborates with other National Government Agencies (NGA) and key stakeholders to ensure early detection and management of several congenital metabolic disorders, which if left untreated, may lead to mental retardation and/or death. How the test is Done: 1. After 24 hours to 48 hours from birth but not later than 3 days after complete delivery. A newborn is placed in intensive care may be exempted from the 3-day requirement but must be tested by 7 days of age. 2. A few drops of blood is drawn from picking the baby’s heel. 3. Then it blotched on a special absorbent card and dried for at least 4 hours and send to the newborn screening laboratory. 4. The procedure may be done by the physician, nurse, midwife, or medical technologist. 5. If screening test suggests problem, the baby’s doctor will follow up with further testing. If those tests confirm a problem, the doctor may refer the baby to a specialist for treatment. Following doctor’s treatment plan can save the baby from lifelong health-related and developmental problems. Module 9: Care of a Newborn and Family 33 III. Nursing Diagnoses of the newborn and family Nursing diagnoses associated with a newborn often center on the problems of establishing respirations, beginning nutrition, and assisting with parent–newborn bonding. Examples are: • Ineffective airway clearance related to mucus in airway • Ineffective thermoregulation related to heat loss from exposure in birthing room • Imbalanced nutrition, less than body requirements, related to poor sucking reflex • Readiness for enhanced family coping related to birth of planned infant • Health-seeking behaviors related to newborn needs If a minor deviation from the normal is present, such as a hemangioma, a diagnosis such as “Parental fear related to hemangioma on left thigh of newborn” might be relevant. VI. Outcome Identification and Planning Planning nursing care should take into account both the newborn’s needs during this transition period and a mother’s need for adequate rest during the postpartal period. Try to adapt teaching time to the schedules of the mother and her newborn. Although the woman must learn as much as possible about newborn care, she also must go home from the health care setting with enough energy to practice what she has learned. Important planning measures for newborns include helping them regulate their temperature and helping them grow accustomed to breastfeeding or bottle feeding. A major portion of implementation in the newborn period is role modeling to help new parents grow confident with their newborn. Be aware how closely parents observe you for guidance in newborn care. Conserving newborn warmth and energy, to help prevent hypoglycemia and respiratory distress, should be an important consideration to accompany all interventions. VII. Evaluating nursing care Module 9: Care of a Newborn and Family 34 Evaluation of expected outcomes should reveal that parents are able to give beginning newborn care with confidence. Be certain parents make arrangements for continued health supervision for their newborn, so that evaluation can be continued and the family’s longterm health needs can be met. Examples indicating achievement of outcomes concerning newborns are: • Infant establishes respirations of 30 to 60 per minute. • Infant maintains temperature at 97.8° to 98.6° F (36.5° to 37° C). • Infant bottle feeds or breastfeeds well with a strong sucking reflex References Flagg, J. (2018). Maternal and child health nursing: Care of the childbearing and childbearing family (8thed.). Philadelphia, PA: WoltersKluwer. Credits and Quality Assurance Prepared by: Reviewed by: MELANIE C. TAPNIO, MAN, RN Assistant Professor JENNY ROSE LEYNES-IGNACIO, EdD, MAN, RN Assistant Professor & OBE Facilitator Recommending Approval: Noriel P. Calaguas, MSHSA, RN Assistant Professor & Chairperson, Nursing Program Approved by: PRECIOUS JEAN M. MARQUEZ, PhD, MSN, RN OIC Dean School of Nursing and Allied Medical Sciences Professor & Dean Module 9: Care of a Newborn and Family 35