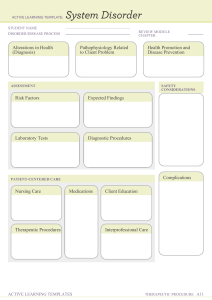
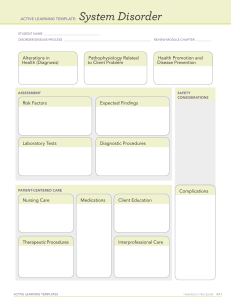
Pediatric Illnesses: Diagnostic Tests & Alterations
advertisement

2F – SICK GROWING CHILD NCM109 (THEORY) – CARE OF MOTHER, AND CHILD AT-RISK OR WITH PROBLEMS (ACUTE AND CHRONIC) MODULE 2F – SICK GROWING CHILD Source: Wong’s-Pillitteri Book, Reporting ALTERATIONS FUNCTIONS IN RESPIRATORY 9. Bronchopulmonary Dysplasia – Xray, CBC, Echocardiogram, Pulse Oximetry, Nasal Continuous Positive Airway Pressure, Surfactant Replacement Therapy 10. Cystic Fibrosis – Stool analysis, CBC, Sweat Chloride Test, Sputum Culture, Chest X-ray, Genetic Test 1. Apnea – med history, PE, sleep study, positive airway pressure therapy, Somnoplasty, Tonsillectomy, UPPP, Mandibular, Nasal Surgery 11. Bronchitis – Pulmonary Functioning Testing, High Resolution Computed Tomography (HRCT), X-Ray, Sputum Examination 2. Apparent Life-Threatening Event – med., PE, CBC, Serum Bicarbonate & Lactate (acidosis), Urinalysis, Chest Radiography 12. Bronchiolitis – CBC, Chest Radiograph, Nasopharyngeal Swabs, Bacterial Cultures 3. Sudden Infant Death Syndrome 4. Respiratory Failure – CBC, Spirometry, Pulmonary Functioning Test, Peak Flow, Arterial Blood Gas 5. Croup Syndrome – Lateral Neck Radiograph, CBC, Heliox 6. Asthma – PE, Spirometry, Peak Flow, Methacholine Challenge, Chest X-ray, Skin Test/Allergy Test, Nitric Oxide, Sputum Eosinophils, provocative testing for exercise and cold asthma 7. Status Asthmaticus – Spirometry, Peak Flow Meter Tests, Exhaled Nitric Oxide Test, Challenge Tests, CBC, Xray, Gas & Diffusion Tests 2F 8. Neonatal Respiratory Distress Syndrome – Blood Gas Analysis, Xray, Blood Test, Echocardiography MINGUITO, SHANIA D. | BSN 2-B 1 2F – SICK GROWING CHILD ALTERATIONS FUNCTIONS IN CARDIOVASCULAR 12. Truncus Arteriosus – Echocardiogram, Cardiac Cath Xray, 1. Patent Ductus Arteriosus – Echocardiogram, Sound waves, X-ray 13. Total Anomalous Pulmonary Venous Return – ECG, Cardiac Cath., Xray 2. Atrial Septal Defect – X-ray, Electrocardiogram, Echocardiogram, Cardiac Catheterization 14. Rheumatic Fever – Throat Swab, CBC, ECG, Echocardiogram 3. Atrioventricular Septal Defect – Prenatal Ultrasound, ECG, Echocardiogram, X-Rays, Cardiac Catheterization 4. Ventricular Septal Defect – Cardiac Catheterization, ECG, X-Ray, Echocardiography 15. Infectious Endocarditis – Blood Culture, CBC, Echocardiogram, Electrocardiogram, Xray, CT Scan 16. Kawasaki Disease – CBC, ECG, Echocardiogram, Urine Testing 5. Pulmonic Stenosis – X-Ray, Electrocardiogram, Echocardiogram, Cardiac Cath. 6. Aortic Stenosis – X-ray, ECG, Echocardiogram, Cardiac Catheterization, Exercise Testing, Pulse Oximetry 7. Coarctation of the Aorta – X-ray, ECG, Echocardiogram, Cardiac Catheterization, CT Scan, MRI 8. Tetralogy of Fallot – Chest X-Ray, Echocardiography, Cardiac Cath., ECG, PO 9. Transposition of the Great Arteries – Echocardiogram, X-ray, ECG, Cardiac Cath. 2F 10. Hypoplastic Left Heart Syndrome – Echocardiogram, ECG, Xray, PO, Cardiac Cath, Cardiac MRI 11. Tricuspid Atresia/Pulmonary Atresia – Echocardiogram, ECG, PO, Xray, Cardiac Cath MINGUITO, SHANIA D. | BSN 2-B 2 2F – SICK GROWING CHILD ALTERATIONS FUNCTION IN HEMATOLOGIC 1. Iron Deficiency Anemia – CBC, Peripheral Smear, Serum Iron, Total Binding Capacity, Serum Ferritin, Hemoglobin Electrophoresis and Measurement of Hemoglobin A2, Reticulocyte Hemoglobin Content, Stool Testing, Incubated Osmotic Fragility, Issue Lead Concentrations, Bone Marrow Aspiration 2. Normocytic Anemia – CBC, Reticulocyte Test, Bone Marrow Biopsy 3. Sickle-Cell Anemia – Hemoglobin Electrophoresis Test ALTERATIONS IN CELLULAR GROWTH 1. Neuroblastoma – Blood and Urine Tests, Biopsy, Bone Marrow Biopsy, CT Scan, MRI Scan, Methyliodobenzylguanine (MIBG), Ultrasound, Xray 2. Wilm’s Tumor (Nephroblastoma) – Abdominal Ultrasound, MRI, Xray, CT Scan, Inferior Venacavogram, Bone Marrow Aspiration, Excretory Urography, CBC 3. Bone Tumors a. Osteosarcoma – Xray, MRI, CT Scan, PET Scan 4. B-Thalassemia – CBC, Hemoglobin Electrophoresis Test, Splenectomy, Cholecystectomy b. Ewing’s Sarcoma – CBC, Xray, CT Scan, MRI, PET Scan, Bone Scan, Biopsy, Bone Marrow Aspiration and Biopsy 5. Aplastic Anemia – Bone Marrow Biopsy, CBC 4. Leukemia – PE, Blood Test, Bone Marrow Test 6. Hemophilia – CBC, Activated Partial Thromboplastin Time (APTT) Test, Prothrombin Time (PT) Tests, Fibrinogen Test 5. Soft Tissue Tumors a. Hodgkin’s Disease – Lymph Node Biopsy, Lab Results, CT Scan, XRay, Bone Marrow Analysis, Liver Function Tests, MRI Scans, Lymphangiography, Abdominal Biopsy 7. Von Willebrand Disease – Factor VIII Clotting Activity, Von Willebrand Factor Antigen 8. Disseminated Intravascular Coagulation – CBC, Prothrombin Time (PT), Partial Thromboplastin Time (PTT), Comprehensive Metabolic Panel (CMP), D-Dimer Tests, Peripheral Blood Smear, Serum Fibrinogen Tests 2F 9. Idiopathic Thrombocytopenic Purpura – CBC, PE, Bone Marrow Aspiration b. Non-Hodgkin’s Disease – Physical Examination, Total Body Imaging, Bone Marrow Aspiration and Biopsy, Blood and Urine Tests, Blood Chemistry Tests, Lumbar Puncture (Spinal Tap), Cytogenetics, Fluorescent in Situ Hybridization (FISH) c. Rhabdomyosarcoma – Imaging Studies, Biopsy, Blood Tests, Bone Marrow Aspiration and Biopsy MINGUITO, SHANIA D. | BSN 2-B 3 2F – SICK GROWING CHILD d. Retinoblastoma – PE, Health History, Bone Scan, Bone Marrow Aspiration and Biopsy, Lumbar Puncture, Electroretinography, RB1 Gene Test, Ultrasound, MRI Renal Ultrasonography, Sonography Cranial 10. Umbilical Hernias – PE, Abdominal Ultrasound, CT Scan 11. Colic – Clinitest, Stool Exam ALTERATIONS FUNCTION IN GASTROINTESTINAL 1. Cleft lip and cleft Palate – Ultrasound, Amniocentesis, Cheiloplasty, Platoplasty 2. Esophageal Atresia and Tracheoesophageal Fistula – Esophagram, Bronchoscopy, Echocardiography 3. Pyloric Stenosis – Electrolyte Lvl, pH Lvl, BUN Lvl, Creatinine Lvl, Ultrasonography, Radiography 4. Gastroesophageal Reflux – 24 hr Intraesophageal pH Monitoring Study, Upper GI Series, pH Probe, Esophageal Manometry, Endoscopy 5. Omphalocele – Prenatal Ultrasonography, Amniocentesis, Fetal Echocardiogram 6. Intussusception – Abdominal XRay, Ultrasound, Air or Contrast Enema 7. Hirschsprung’s Disease – Abdominal XRay, Rectal Biopsy, Contrast Enema, Anal Manometry 2F 8. Anorectal Malformations – Abdominal XRay, Renal Ultrasound, Pelvic Ultrasound, Spinal Ultrasound, MRI 9. Diaphragmatic Hernias – Chest Radiography, Cardiac Ultrasonography, Echocardiography, 12. Rumination – Endocrine Hormone Functions, Test for Anemia, Serum Electrolytes 13. Celiac Disease – PE, Blood Test, HLA Genetic Test, Endoscopy ALTERATIONS FUNCTION IN GENITOURINARY 1. Bladder Exstrophy – MRI, Xray 2. Hypospadias & Epispadias – Dorsal Hood, Chordee, Mucosal Strip 3. Obstructive Uropathy – PE, Med His., Ultrasonography, IV Pyelogram, Diethylenetriamine Pentacetic Acid (DTPA), Dimercaptosuccinic Acid (DMSA) Renal Scan, VCUG 4. Nephrotic Syndrome – Urine test, CBC, Kidney Biopsy 5. Glomerulonephritis – Urinalysis, CBC, Ultrasound, Kidney Biopsy 6. Phimosis – PE 7. Cryptorchidism – MRI, Laparoscopy, Open Surgery, PE, Ultrasound 8. Inguinal Hernia & Hydrocele – Ultrasound, Transillumination, Duplex Ultrasonography, Plain Abdominal Radiography 9. Testicular Torsion Ultrasound, Urinalysis – Doppler MINGUITO, SHANIA D. | BSN 2-B 4 2F – SICK GROWING CHILD ALTERATIONS FUNCTION IN NEUROLOGIC ALTERATIONS IN MUSCULOSKELETAL FUNCTION 1. Seizure Disorders – Neuro Exam, CBC, Spinal Tap, EEG, MRI, CT 1. Metatarsus Adductus – PE, Leopold’s Maneuver, Ultrasound, Hip Examination, Interview, MRI 2. Infectious Disease a. Reye’s Syndrome – CT, MRI, Urine Test, Blood Test, Skin Biopsy, Spinal Tap, Liver Biopsy b. Guillain-Barre Syndrome – Spinal Tap, Electromyography, Nerve Conduction Studies 2. Clubfoot – Ultrasound, Radiography, MRI, CT, Xray 3. Genu Varum & Genu Valgum – PE, Xray, Blood Test, CT Scan, 4. Dysplasia of the Hip – Ortolani Test, Barlow Maneuver, Ultrasound, Xray 3. Hydrocephalus – Ultrasound, MRI, CT, Spinal Tap, ICP, Fundoscopic Examination 5. Legg-Calve-Perthes Disease – Xray, MRI, CBC 4. Spina Bifida – Blood tests, MSAFP Test, Amniocentesis 6. Supped Capital Femoral Epiphysis – PE, Xray 5. Craniosynostosis – PE, CT Scan, Ultrasound 7. Scoliosis – Plumb Line Test, Xray “Cobb Technique”, Risser Scale 6. Cerebral Palsy – Brain Imaging Tests, Metabolic and Genetic Testing, EEG, Functional Independence and WeeFIM, Pediatric Evaluation of Disability Inventory 8. Torticollis – Xray, CT, Ultrasound, CBC 9. Kyphosis – CT, MRI, Bone Scan 10. Lordosis – PE, Xray, CT Scan 11. Osteomyelitis – Xray, MRI, CT, Biopsy 12. Skeletal Tuberculosis – Tuberculin Skin Test, CBC, Xray, Bone Biopsy 13. Septic Arthritis – Joint Fluid Analysis, Blood Tests, Imaging Tests 2F 14. Osteogenesis Imperfect – Xrays, Lab tests, Dual Energy XRay Absorptiometry Scan 15. Duchenne’s Muscular Dystrophy – PE, Muscle Biopsy MINGUITO, SHANIA D. | BSN 2-B 5 2F – SICK GROWING CHILD 16. Becker’s Muscular Dystrophy – Creatine Kinase Level, Muscle Biopsy, Genetic Testing 9. Klinefelter’s Syndrome – Amniocentesis, Hormone Testing, Chromosome Analysis 17. Fascioscapulohumeral Dystrophy – Serum Creatinine Kinase, EMG, Surgical Removal, Microscopic Exam 10. Phenylketonuria – Guthrie Bacterial Inhibition Assay, PKU Screening Test 18. Emery-Dreyfuss Muscular Dystrophy – CPK Test, Transaminase, Lactate dehydrogenase, aldolase levels, PCR, ultrasonography, EMG, ECG, PFT, Muscle biopsy 11. Galactosemia – CBC, Urine Test, Newborn Screening, Buetler Test 12. Maple Syrup Urine Disease – Plasma Amino Acids Testing, CBC, Urinalysis, Chorionic Villus Sampling, Amniocentesis 19. Congenital Muscular Dystrophy – EMG, Lab Test, Biopsy, Genetic testing ALTERATIONS IN SKIN INTEGRITY ALTERATIONS IN ENDOCRINE FUNCTION 1. Growth Hormone Deficiency – PE, Blood Test, Imaging Tests 2. Hyperpituitarism – CBC, Ultrasound, Thyroid Scan Thyroid 3. Diabetes Insipidus – Urine Collection, Water Deprivation Test, Vasopressin Test, MRI 1. Contact Dermatitis – Patch Test, CBC, Challenge Test, Nasal Smear Test 2. Diaper Dermatitis – PE, Lab Tests 3. Seborrheic Dermatitis – PE, Lab, Skin Biopsy 4. Eczema – Allergic Skin Test, CBC, Skin Biopsy 4. Precocious Puberty – CBC, Xray, MRI 5. Impetigo – PE, Swab Test 5. Cushing’s Syndrome – Urine Collection, Saliva Test, Steroid Test 6. Congenital Adrenal Hyperplasia – ACTH Stimulation Test, Genetic Test, Urine Test, Karyotypes Test, Pelvic Ultrasound, Bone Age Studies 2F 6. Scabies – Scabies Ink Test, Tetracycline Solution, Videodermatoscopy, Dermoscopy, Skin Scraping, Adhesive Tape Test 7. Addison’s Disease – CBC, ACTH Stimulation Test, Xray, CT Scan, Thyroid Functioning Test 8. Furner’s Syndrome – Karyotype Analysis, CBC, Echocardiography, MRI, Maternal Serum Screening MINGUITO, SHANIA D. | BSN 2-B 6 2F – SICK GROWING CHILD some15 APNEA URGENT RESPIRATORY THREATS Apnea is a pause in respirations longer than 20 seconds with accompanying bradycardia (cyanosis also may be present). Types: 1. Central – Both airflow and chest wall movement are absent. 2. Obstructive – Airflow is absent but chest wall motion is present. 3. Mixed – Both central and obstructive components are present. - Medical conditions such as type 2 DM, - congestive heart failure, high blood pressure, Parkinson’s disease, PCOS, hormonal disorders, prior stroke, or chronic lung disease like asthma. TAKE NOTE! Gently shaking an infant or flicking the sole of the foot often stimulates the baby to breathe again, almost as if the child needed to be reminded to maintain this function. If an infant does not respond to these simple measures, resuscitation is necessary. As a result of: ✓ Fatigue ✓ Immaturity of their respiratory mechanisms. ✓ Secondary stress – infection, hyperbilirubinemia, hypoglycemia, or hypothermia. Apnea during infancy can be a symptom of any one of many disorders – including: Sepsis Seizures or other Neurologic Disorder Upper/Lower Airway Infection Gastroesophageal Reflux Hypoglycemia or other Metabolic Problems ✓ Impaired regulation of breathing during sleep or feeding ✓ ✓ ✓ ✓ ✓ Risk Assessment: - Being overweight - A large neck circumference that could make - your airways more narrow - A narrowed airway that you inherited or - developed from large tonsils or adenoids - Being male - Older age - A family history of sleep apnea - Smoking - Use of alcohol, sedatives, or tranquilizers - Nasal congestion 2F APNEA: Therapeutic and Nursing Care Management 1. Closely observe all newborns, especially preterm ones, to detect these apneic episodes. 2. Apnea monitors that record respiratory movements are invaluable tools to detect failing respiration and sound a warning an infant needs attention. 3. Infants with frequent or difficult-tocorrect episodes may be placed on ventilators to provide respiratory coordination until they are more mature. 4. To help prevent episodes of apnea, maintain a neutral thermal environment and use gentle handling to avoid excessive fatigue. 5. Always suction gently to minimize nasopharyngeal irritation, which can cause bradycardia because of vagal stimulation. 6. Using indwelling nasogastric tubes rather than intermittent ones can also reduce the amount of vagal stimulation. 7. After feeding, observe an infant carefully because a full stomach can put pressure on the diaphragm and can potentially compromise respirations. Careful burping also helps to reduce this effect. 8. Never take rectal temperatures in infants prone to apnea because the MINGUITO, SHANIA D. | BSN 2-B 7 2F – SICK GROWING CHILD resulting vagal stimulation can reduce the heart rate (bradycardia). 9. Theophylline or caffeine sodium benzoate may be prescribed to stimulate respirations. → Increase the infant’s sensitivity to carbon dioxide, which stimulates respiratory function. Infants who have had an apneic episode severe enough to require resuscitation are at a high risk for SIDS. Such infants may be discharged home with a monitoring device to be used for 2 to 6 months. APPARENT LIFE-THREATENING EVENT URGENT RESPIRATORY THREATS Formerly referred to as aborted SIDS death or near-miss SIDS, generally refers to ➔ An event that is sudden and frightening to the observer in which the infant exhibits a combination of: ▪ Apnea ▪ Change in color (pallor, cyanosis, redness) ▪ Change in muscle tone (usually hypotonia) ▪ Choking ▪ Gagging ▪ Coughing ➔ ALTE – May include apnea, but ALTE may occur without apnea. (Apnea is not an immediate precursor to SIDS) ➔ Common Risk Factor for SIS and ALTE is maternal smoking. Diagnostic Evaluation: 2F ✓ Who witnessed the event? ✓ Where the infant was during the event? ✓ What, if any, activities were involved? (Such as during or after a feeding and etc.) ✓ Prenatal and postnatal history must be obtained. ✓ Observe the infant’s respiratory pattern and response to feeding. Commonly used monitoring is continuous recording of cardiorespiratory patterns are the following: a) Pneumocardiogram b) Four-channel pneumocardiograms → monitor heart rate c) Respirations (chest impedance) d) Nasal Airflow e) Oxygen Saturation Risk Factors: - Infants <2 months of age - History of prematurity especially if <32 weeks at birth - More than 1 event Risk Assessment: - Male predominance Gestational age Low birth weight Very low birth weight Incident of small for gestational age Age at the event Multiparity Maternal age Smoking Polysomnography (sleep study) → Records brain waves, eye and body movements, esophageal manometry, and end-tidal carbon dioxide measurements.a ALTE: Therapeutic Management: ✓ 24 hour observation ✓ Monitors with respiratory impedance plethysmography (RIP) are capable of detecting obstruction as well as central apnea. MINGUITO, SHANIA D. | BSN 2-B 8 2F – SICK GROWING CHILD ALTE: Nursing Care Management: 1. Nurse can be a major source of support to the family in terms of education about the equipment. 2. Education regarding observation of the infant’s status. 3. Instructions regarding immediate intervention during apneic episodes including CPR. 4. To help the family cope with the numerous procedures they must learn. 5. Adequate preparation before discharge and written instructions are essential. 6. Encourage parents to look first at the infant if an alarm goes off and ensure the infant is breathing, and then determine the cause of the alarm. 7. Nurses, especially those involved in the care at home, must become familiar with the equipment, including its advantages and disadvantages. Safety is a major concern because monitor can cause electrical burns and electrocution. The following precautions are recommended: Electrode placement for apnea monitoring. In small infants, one fingerbreadth may be used. ✓ Remove leads from infant when not attached to the monitor. ✓ Unplug the power cord from the electrical outlet when the cord is not plugged into the monitor. ✓ Use safety covers on electrical outlets to discourage children from inserting objects into sockets. Home apnea monitor uses a soft belt with a Velcro attachment to hold two leads in the appropriate position on the chest. 2F MINGUITO, SHANIA D. | BSN 2-B 9 2F – SICK GROWING CHILD ALTE: TAKE NOTE! If the infant is apneic, gently stimulate the trunk by patting or rubbing it. Call loudly for help even if alone. If the infant is prone, turn to the back and flick the heels of the feet. If there is still no response, immediately begin CPR, starting with chest compressions. After approximately 2 minutes of CPR, activate the emergency medical service – “CALL 911!”and then resume CPR until emergency responders arrive or the infant starts breathing. Never vigorously shake the child. No more than 10 seconds are spent on stimulation before implementing CPR. stimulation < IOS SUDDEN INFANT DEATH SYNDROME URGENT RESPIRATORY THREATS Sudden death of an infant younger than 1 year of age that remains unexplained after a complete postmortem examination, including an investigation of the death scene, and a review of the case history. Sudden Unexpected Early Neonatal Death (SUEND) and Sudden Unexpected Infant Death (SUID) share similar features but differ in regards to the timing of death. abnormalities disorders. in CNS and respiratory Health Status – History of Illness Sleep Habits – Prone Siblings – Siblings of SIDS victims Maternal – Young age; cigarette smoking, poor postnatal care and etc. SIDS: Etiology One hypothesis → Related to a brainstem abnormality in the neurologic regulation of cardiorespiratory control. → Affects arousal and physiologic responses to a life-threatening challenge during sleep. Abnormalities include: ✓ Prolonged sleep apnea ✓ Increased frequency of brief inspiratory pauses ✓ Excessive periodic breathing ✓ Impaired arousal responsiveness to increased carbon dioxide or decreased oxygen. SLEEP APNEA IS NOT THE CAUSE OF SIDS. SUEND – Occurs in the first week of life. SUID – Death in the postneonatal period. SIDS: Epidemiology Peak Age – 2 to 3 months, 95% occur by 6 months 2F Sex – Higher % are Boys Time of Death – During sleep Time of Year – Increased incidence in winter. Socioeconomic – Lower socioeconomic class. Birth – Higher % in preterm infants → ELBW and VLBW; multiple births; low APGAR; Genetic Predisposition – To SIDS has been postulated as a cause, chromosome 6q was positively linked to a syndrome of SIDS and dysgenesis of the testis. Risk Factors for SIDS: a) Underlying infant vulnerability factor o Brain abnormality – A critical incident in the fetal developmental period or in early neonatal life and an environmental stressor such as prone sleep positioning. b) Maternal Smoking – Major factor in SIDS. MINGUITO, SHANIA D. | BSN 2-B 10 2F – SICK GROWING CHILD c) Maternal Alcohol Use d) Cosleeping – Infant sharing a bed with an adult or older child on a noninfant bed. e) Prone Sleeping – Causes oropharyngeal obstruction or affect thermal balance or arousal state. f) Side-Lying Position – No longer recommended for infants sleeping at home, day care, or hospitals (unless medically indicated). g) Soft Bedding – Such as waterbeds, sheepskins, beanbags, pillows, and quilts should be avoided for infant sleeping surfaces. h) Viral respiratory or botulism infection. i) Pulmonary Edema j) Brainstem Abnormalities k) Neurotransmitter Deficiencies l) Heart Rate Abnormalities m) Distorted familial breathing patterns. n) Decreased arousal responses. o) Possible lack of surfactant in alveoli. Protective Factors for SIDS: a) Breastfeeding – First 16 weeks of life. b) Pacifier Use c) Supine Position d) Updated Immunization Status Infant Risk Factors for SIDS: a) Low birth weight or preterm birth (<37 weeks’ gestation) b) Low APGAR Scores c) Recent Viral Illness d) Siblings of two or more SIDS victims e) Male Gender f) Infants of Native American or AfricanAmerican Ethnicity 2F HOME MONITORING IS NOT RECOMMENDED FOR THIS GROUP OF CHILDREN. SIDS: Nursing Care Management 1. Educating families about the risk of prone sleeping position in infants from birth to 6 months of age, use of appropriate bedding surfaces, association with maternal smoking, and the dangers of cosleeping on noninfant surfaces. 2. Nurses have an important role in modeling behaviors for parents to foster practices that decrease the risk of SIDS, including placing infants in a supine sleeping position in the hospital. 3. Promote supine sleep positions at home. (Can also be side-lying positions) 4. Nurses must be proactive in further decreasing the incidence of SIDS; postpartum discharge planning, newborn discharges, follow-up home visits, well-baby clinic visits, and immunization visits provide excellent opportunities to educate parents about safe sleep environment for infants and other protective factors for SIDS. 5. Nurses must continue to take every opportunity to advocate for infants by providing information for parents and caretakers about the modifiable risk factors for SIDS that can be implemented to prevent its occurrence across all sectors of the population. 6. Parents should be counseled by a nurse or someone else trained in counseling at the time of the infant’s death. It helps if they can talk to this same person periodically for however long it takes to resolve their grief. 7. Autopsy reports should be given to parents asap. 8. Reading that their child’s death was unexplained can help to reassure parents the death was not their fault. MINGUITO, SHANIA D. | BSN 2-B 11 2F – SICK GROWING CHILD TAKE NOTE! Practices that may reduce the risk of SIDS: ✓ Avoid smoking during pregnancy and near the infant. ✓ Using supine sleeping position. ✓ Avoiding soft, moldable mattresses, blankets, and pillows. ✓ Avoid bed sharing. ✓ Breastfeeding ✓ Avoid overheating during sleep hypoxemia hypoxia hypercapnia RESPIRATORY FAILURE URGENT RESPIRATORY THREATS An inadequate supply of oxygen results in blood hypoxemia and tissue hypoxia; inadequate carbon dioxide removal causes hypercapnia. Often both gases may be insufficiently exchanged. Respiratory Insufficiency – applied to two conditions: a) When there is increased work of breathing but gas exchange function remains near normal. b) When normal blood gas tensions cannot be maintained and hypoxemia and acidosis develop secondary to carbon dioxide retention. Respiratory Failure – Inability of the respiratory apparatus to maintain adequate gas exchange. o This process involves pulmonary dysfunction that generally results in impaired alveolar-capillary gas exchange, which can lead to hypoxemia or hypercapnia. 2F Respiratory Arrest – Cessation of respiration. 12 Apnea – Cessation of breathing for more than 20 seconds, or for a short period when associated with hypoxemia or bradycardia. Effective pulmonary gas exchange requires: ✓ Clear airways ✓ Normal lungs and chest wall ✓ Adequate pulmonary circulation Diagnosis of Respiratory Failure Is determined by the combined application of three sources of information: 1. Presence or history of a condition that might predispose to respiratory failure. 2. Observation of respiratory failure. 3. Measurement of ABGs. Predisposing Factors: Obstructive Lung Disease – There is increased resistance to airflow in either the upper or the lower respiratory tract. ✓ Obstruction ▪ Tracheomalacia Strached collapse) ▪ Choanal Atresia ▪ Vocal Paralysis ✓ Aspiration ▪ Meconium ▪ Mucus ▪ Vomitus ▪ FB ✓ Infection ▪ Epiglottis ▪ Pneumonia ▪ Pertusis ▪ Severe Tonsillitis ✓ Laryngospasm from local irritation ▪ Intubation ▪ Drowning ▪ Aspiration S & MINGUITO, SHANIA D. | BSN 2-B 2F – SICK GROWING CHILD Restrictive Lung Disease – Impaired lung expansion results from loss of lung volume, decreased distensibility, or chest wall disturbance. Causes: RDS Pulmonary Edema Pleural Effusion Near Drowning Congenital Diaphragmatic Hernia Abdominal Distention Muscular Dystrophy Paralytic Conditions (e.g., poliomyelitis, botulism) ✓ Severe Structural Obstructions (e.g., sever scoliosis) ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ Primary Inefficient Gas Transfer – Insufficient alveolar ventilation for carbon dioxide removal or impaired oxygenation of pulmonary capillary blood as a result of dysfunction of the respiratory control mechanism. Causes of respiration center depression include: ✓ Cerebral trauma (e.g., birth injuries, shaken baby syndrome) ✓ Intracranial tumors ✓ CNS Infection (e.g., meningitis, encephalitis, sepsis) ✓ Overdose with barbiturates, opioids, or benzodiazepines ✓ Sever Asphyxia (e.g., hypercapnia, hypoxemia) ✓ Tetanus 2F Recognition of Respiratory Failure: 1. Insufficient alveolar ventilation leads to hypoxemia and hypercapnia. 2. Evaluation of respiratory adequacy is based on both clinical assessment and laboratory studies. 3. In clinical situations in which impaired ventilation can be anticipated or clinical manifestations indicate impending hypoxemia, serial measurements of blood gases should be obtained and monitored to detect impending respiratory failure, and therapy should be implemented before respiratory acidosis becomes extreme. Respiratory Management Failure: Nursing Care 1. Recognize the situation and immediately initiate resuscitative measures, such as opening the airway and positioning, administering supplemental oxygen and positive pressure ventilation, suctioning, performing CPR, or intubating if the child’s status continues to deteriorate. 2. When the situation is not an arrest, the suspicion of respiratory failure is confirmed by assessment, and the severity is defined by capillary or arterial blood gas analysis. 3. When severity is established, an attempt is made to determine the underlying cause by thorough evaluation. Specific Therapies – Directed reversal of the causative factors. toward Nonspecific Therapies – Necessary to maintain oxygenation and enhance carbon dioxide removal until specific methods take effect. MINGUITO, SHANIA D. | BSN 2-B 13 2F – SICK GROWING CHILD The major reasons for implementing nonspecific treatments are: 1. Unknown etiology 2. Lack of specific treatment for a known cause. 3. Lack of time for a specific treatment to take effect, and 4. Need for specialized personnel or equipment for specific treatment. The principles of management are to: 1. Maintain ventilation and maximize oxygen delivery. 2. Correct hypoxemia and hypercapnia. 3. Treat the underlying cause. 4. Minimize extra-pulmonary organ failure. 5. Apply specific and nonspecific therapy to control oxygen demands, and 6. Anticipate complications. Monitoring the patient’s condition is critical. Observation and Monitoring: ✓ Nurse monitors the child to anticipate respiratory failure, determine a course of action, and assess the patient’s response to treatment. ✓ If close, continuous monitoring is required, the child is transferred to a pediatric intensive care unit. Observation is geared toward general appearance, responsiveness, pulse oximetry, and vital signs. ✓ Prone positioning improves oxygenation and lung mechanics. ✓ Nurse monitors the child’s cardiac and respiratory status by observation and electronic means. ✓ Goal of therapy is to control the body’s oxygen demands, assessments of fever and pain should be frequent. ✓ Measure oxygenation by the use of pulse oximetry or blood gas monitoring. 2F Clinical Failure Manifestations of 14 Respiratory Cardinal Signs: o Restlessness o Tachypnea o Diaphoresis Early but Less Obvious Signs: o Mood changes o Headache o Altered depth and pattern of respirations o Hypertension o Exertional dyspnea o Anorexia o Increased cardiac output and urinary output o CNS Symptoms o Nasal Flaring o Expiratory Grunting o Wheezing Signs of More Severe Hypoxia: o o o o o o o o o o Hypotension Depressed respirations Dimness of Vision Bradycardia Arrythmias Somnolence (drowsy , sleepy) Cyanosis Stupor (near Coma Dyspnea unconsciousness) Nursing Observation for the Child with Respiratory Failure: Observation of respiratory effort or distress – Nasal flaring, grunting, gasping, retractions, agonal respirations. Observation of diaphragmatic movement, lung expansion, and use of accessory muscles – Depth, symmetry, inspiration/expiration ratio. MINGUITO, SHANIA D. | BSN 2-B 2F – SICK GROWING CHILD Auscultation of chest to assess: ✓ Breath sounds – presence, intensity, quality, symmetry ✓ Abnormal sounds – stridor, wheezes, crackles, rhonchi, increase or decrease in sounds ✓ Endotracheal tube placement and need for suction Visual inspection of skin color, capillary refill. Observation of activity level and level of consciousness. CROUP SYNDROME REACTIVE AIRWAY DISORDERS Croup – General term applied to a group of symptoms characterized by hoarseness, a resonant cough described as “barking” or “brassy” (croupy), varying degrees of inspiratory stridor, and varying degrees of respiratory distress resulting from swelling or obstruction in the region of the larynx. 1. Acute Epiglottitis 2. Acute LTB 3. Acute Spasmodic Laryngitis 4. Acute Tracheitis ➔ H. influenza type B o Parainfluenza virus o Influenza types A and B o Human coronavirus o Rhinoviruses o Enteroviruses o Metapneumoviruses o Adenoviruses o RSV o Measles ➔ Mycoplasma pneumonia – can also cause coup. 2F CROUP: Acute Epiglottitis (2 to 5 years old) ➔ Noninfectious ➔ Obstructive inflammatory process. o Causative Agent: H. influenza o Caustic Agents: Hot foods, smoke inhalation, foreign bodies, and exposure to crack cocaine. ➔ Three clinical observations that are predictive of epiglottis are absence of spontaneous cough, presence of drooling, and agitation. ➔ Manifestations: Child is irritable, restless, voice is thick and muffled, froglike croaking sound on inspiration. Not hoarse, suprasternal and substernal retractions may be visible. ➔ Struggles to breathe, slow, quiet breathing provides better air exchange. ➔ Throat is red and inflamed, and a distinctive, large, cherry red, edematous epiglottis is visible on careful throat inspection. o Throat inspection should only be performed when immediate endotracheal intubation or emergency tracheotomy can be performed if needed. CROUP: Acute Epiglottitis Therapeutic Management, Prevention, and Nursing Care Management ➔ Progressive obstruction leads to: o hypoxia o hypercapnia o acidosis o decreased muscular tone o reduced level of consciousness o sudden death ➔ Lateral neck radiograph of the soft tissues is indicated for diagnosis. ➔ Nasotracheal intubation → for RDS ➔ Swelling decreases after 24 hours of antibiotic therapy. ➔ Corticosteroids for reducing edema. MINGUITO, SHANIA D. | BSN 2-B 15 2F – SICK GROWING CHILD ➔ Recommended to receive H. influenzae type B conjugate vaccine beginning at 2 months of age. ✓ Act quickly but calmly and provide support without unduly increasing anxiety. ✓ Child is allowed to remain in the position that provides the most comfort and security. ✓ Droplet isolation precautions are indicated for 24 hours after initiation of effective antibiotic therapy to control spread of respiratory organisms. ✓ Nurses who suspect epiglottitis should not attempt to visualize the epiglottitis directly with a tongue depressor or take a throat culture but should have the child seen by the primary care provider immediately. ✓ Resuscitation equipment and suction should be immediately available and ready at the child’ bedside. CROUP: Acute Laryngitis Causative Agents: Viruses Therapeutic and Nursing Care Management The disease is almost always self-limiting without long-term sequelae. Treatment is supportive with fluids and humidified air. CROUP: Acute Laryngotracheobronchitis AKA LTB → Affects children less than 5 years of age. 2F Organisms responsible: 1. parainfluenza virus types 1 and 2 2. parainfluenza virus type 3 3. RSV 4. influenza types A and B 5. measles 6. M. pneumoniae ➔ Onset of low-grade fever. Child wakes up with barky, brassy cough at times inspiratory stridor. ➔ Symptoms got worse at night, and agitation and crying tend to exacerbate the symptoms. ➔ Manifested by nasal flaring, intercostal retractions, tachypnea, and continuous stridor. ➔ Develops the classic barking or seallike cough and acute stridor after several days of rhinitis. ➔ Can lead to respiratory acidosis or respiratory failure. LTB Therapeutic Management and Nursing Care Management ➔ Major Objective: Maintain an airway and providing for adequate respiratory exchange. ➔ Cool mist, cool air vaporizer, cool temperature therapy. ➔ Nebulized epinephrine is used in children with croup that is not alleviated with cool mist. ➔ Corticosteroids – decrease subglottic edema. ➔ Severe Cases → helium + oxygen (heliox) may reduce the work of breathing and relieve the airway obstruction. ➔ Continue to drink beverages they like. ➔ Children with severe respiratory distress (traditionally, a respiratory rate >60 breaths/min for infants) should not be given anything by mouth to prevent aspiration and increased work of breathing. ✓ Monitor, observe, and proper assessment. – Cardiac, respiratory, and pulse oximetry. ✓ Early signs of impending airway obstruction include increased pulse and respiratory rate; substernal, suprasternal, and intercostal MINGUITO, SHANIA D. | BSN 2-B 16 2F – SICK GROWING CHILD retractions; nasal flaring; and increased restlessness. ✓ Rest, sit upright, or children wanted to be held. CROUP: Acute Spasmodic Laryngitis AKA MIDNIGHT CROUP or TWILIGHT CROUP – Characterized by paroxysmal attacks of laryngeal obstruction that occur at night. Child awakes suddenly with the characteristic barking, metallic cough; hoarseness; noisy inspirations; and restlessness. Therapeutic Management and Nursing Care ✓ Managed at home. Cool mist is recommended. ✓ Warm mist provided by steam from hot running water may be helpful. ✓ Hospitalized for moderate to severe symptoms. ✓ Corticosteroid therapy. CROUP: Bacterial Tracheitis (5 to 7 years old) Infection of the mucosa and soft tissues of the upper trachea. o Complication of LTB. o Thick, purulent tracheal secretions. o May develop a life-threatening upper airway obstruction, respiratory failure, ARDS, and multiple organ dysfunction. Organism responsible: - Staphylococcus aureus M. catarrhalis S. pneumoniae S. pyogenes H. influenzae 2F Therapeutic Management and Nursing Care ✓ Antipyretics, fluid status, and antibiotics (10-day course) ✓ Endotracheal intubation and mechanical ventilation ASTHMA REACTIVE AIRWAY DISORDERS Chronic inflammatory disorder of the airways characterized by recurring symptoms, airway obstruction, and bronchial hyperresponsiveness. Atopy – Genetic predisposition for the development of an IgE-meditated response to common aeroallergens, is the strongest identifiable predisposing factor for developing asthma. Exaggerated response of bronchi to a trigger such as URI, dander, cold air, exercise. - bronchospasm, exudation, and edema of bronchi - infancy to adolescence or adulthood - wheezing, chest tightens, cough, labored respirations - Treatment: inhaled corticosteroids, bronchodilators, leukotriene modifiers, allergen, and control of triggers. Organisms responsible: - viruses – RSV in infants, variety of URI pathogens AIM MINGUITO, SHANIA D. | BSN 2-B 17 2F – SICK GROWING CHILD STATUS ASTHMATICUS REACTIVE AIRWAY DISORDERS Medical emergency that can result in respiratory failure and death if unrecognized and untreated. ➔ therapy for status asthmaticus is aimed at improving ventilation, decreasing airway resistance and reliving bronchospasm, correcting dehydration and acidosis, allaying child and parent anxiety related to the severity of the event, and treating any concurrent infection 18 NEONATAL RESPIRATORY DISTRESS SYNDROME LOWER AIRWAY DISORDERS Surfactant deficiency immaturity of the thorax. and physiologic ➔ chronic intrauterine stress (e.g., maternal preeclampsia or hypertension) ➔ nonpulmonary cause – sepsis, cardiac defects More details on Module 1F. BRONCHOPULMONARY DYSPLASIA Asthma & S. Asthmaticus: NCM: ✓ acute asthma care ✓ pulse oximetry is monitored along with rate and depth of breathing ✓ auscultation of air movement, adventitious sounds, and any signs of respiratory distress ✓ child w/ s. asthmaticus should be placed on continuous cardio-respiratory (including BP) and pulse oximetry monitoring ✓ avoid allergens ✓ relieve bronchospasm ✓ promote self-care and normalization ✓ child and family support 2F LOWER AIRWAY DISORDERS Chronic lung disease, is a pathologic process that develops primarily in ELBW and VLBW interstitial edema infants with RDS. epithelial swelling thickening& Fibrotic walls More details on Module 1F. C T prolif of alveolar . CYSTIC FIBROSIS LOWER AIRWAY DISORDERS Exocrine (mucus-producing) gland dysfunction that produces multisystem involvement. - autosomal recessive trait - inherits defective gene from both parents - Cystic Fibrosis Transmembrane Regulator (CFTR) → codes a protein of 1480 amino acids - mechanical obstruction caused by increased viscosity of mucous gland secretions - produces thick, heavy mucoprotein that accumulates and dilates - small organs like pancreas and bronchioles become obstructed - retained mucus serves as an excellent medium for bacterial growth - viscous and tenacious secretions are difficult to expectorate and gradually obstruct the bronchi and bronchioles, causing scattered areas of MINGUITO, SHANIA D. | BSN 2-B 2F – SICK GROWING CHILD bronchiectasis, hyperinflation ateltectasis, and TAKE NOTE: REINFORCEMENT Is a disease of exocrine gland function that involves multiple organ systems but results in chronic respiratory infection. Common symptoms are: - progressive chronic obstructive lung disease associated with infection - maldigestion from exocrine pancreatic insufficiency - growth failure from malabsorption and anorexia - diabetes symptoms of hyperglycemia, polyuria, glycosuria and weight loss from pancreatic insufficiency -salty sweat Signs of a pneumothorax are usually nonspecific and include tachypnea, tachycardia, dyspnea, pallor, and cyanosis. A subtle drop in oxygen saturation (measured by pulse oximetry) may be an early sign of pneumothorax. 2F Therapeutic Management and Nursing Care ✓ prevent or minimize pulmonary complications ✓ ensure adequate nutrition for growth ✓ encourage appropriate physical activity ✓ promote reasonable quality of life ✓ Pulmonary Assessment – special attention to lung sounds, observation of cough, and evidence of decreased activity or fatigue ✓ Gastrointestinal Assessment – Observing the frequency and nature of the stools and abdominal distention ✓ must be alert to evidence of growth failure or failure to thrive ✓ determine the child’s eating and eliminating habits and confirm a history of frequent respiratory tract infections or bowel obstruction in infancy ✓ assess newborn for feeding and stooling patterns ✓ nurse anticipates diagnostic testing such as initial newborn screening, immunoreactive trypsinogen, DNA analysis, or sweat chloride test Flutter mucus clearance device – Small, handheld plastic pipe with a stainless-steel ball on the inside. Acapella provides highfrequency oscillation as well as PEP. MINGUITO, SHANIA D. | BSN 2-B 19 2F – SICK GROWING CHILD Patent Ductus Arteriosus BRONCHITIS PDA LOWER AIRWAY DISORDERS CHD - ACYANOTIC DEFECTS NON-OBSTRUCTIVE LESIONS Inflammation of the large airways (trachea and bronchi) that is frequently associated with a URI. dry, hacking, nonproductive cough worsens at night first 4 years of life productive in 2 or 3 days requires only symptomatic treatment including analgesics, antipyretics, and humidity - Treatment: Cough suppressants - Organisms responsible: ✓ viral ✓ M. pneumoniae ✓ bacteria, fungi, airborne irritants Failure of the fetal ductus arteriosus (artery connecting the aorta and pulmonary artery) to close within the first weeks of life. The continued patency of this vessel allows blood to flow from the higher-pressure aorta to the lower-pressure pulmonary artery, which causes a left-to-right shunt. ➔ machinery-like murmur ➔ widened pulse pressure and bounding pulses result from runoff of blood from the aorta to the pulmonary artery Treatment: allergic disorders, BRONCHIOLITIS LOWER AIRWAY DISORDERS Most common infectious disease of lower airways. Acute viral infection with maximum effect at bronchiolar level. - occurs in winter and spring - 2-12 mos. of age; rare after 2 years - labored respirations, poor feeding, cough, tachypnea, retractions, flaring nares, emphysema, increased nasal mucus, wheezing, may have fever - Treatment: Provide supplemental oxygen if saturations ≤90%; bronchodilators (optional), suction nasopharynx, ensure adequate fluid intake, maintain adequate oxygenation. 2F Organisms responsible: ✓ caused by RSV, adenoviruses, and parainfluenza viruses, human metapneumovirus, Mycoplasma pneumoniae Medical – Administer indomethacin. Surgical – Surgical division/ligation, videoassisted thoracoscopic surgery. Nonsurgical – Coils to occlude the PDA. Atrial Septal Defect ASD CHD - ACYANOTIC DEFECTS NON-OBSTRUCTIVE LESIONS Abnormal opening between the atria, allowing blood from the higher-pressure left atrium to flow into the lower-pressure right atrium. There are three types of atrial septal defect (ASD). ➔ Ostium primum (ASD 1) – Opening at lower end of septum; may be associated with mitral valve abnormalities. ➔ Ostium secundum (ASD 2) – Opening near center of septum. ➔ Sinus Venosus Defect – Opening near junction of superior vena cava and right atrium; may be associated with partial anomalous pulmonary venous connection. ➔ Left atrial pressure slightly exceeds right atrial pressure, blood flows from the left to the right atrium, causing an increased flow of oxygenated blood into the right side of the heart. MINGUITO, SHANIA D. | BSN 2-B 20 2F – SICK GROWING CHILD ➔ Asymptomatic, may develop heart failure, characteristic murmur ➔ RISK FOR ATRIAL DYSRHYTHMIAS ATRIOVENTRICULAR SEPTAL CHD - ACYANOTIC DEFECTS NON-OBSTRUCTIVE LESIONS Incomplete fusion of the endocardial cushions. Consists of a low ASD that is continuous with a high VSD and clefts of the mitral and tricuspid valves, which creates a large central atrioventricular (AV) valve that allows blood to flow between all four chambers of the heart. ➔ the directions and pathways of flow are determined by pulmonary and systemic resistance, left and right ventricular pressures, and the compliance of each chamber ➔ flow is generally from LEFT TO RIGHT ➔ most common cardiac defect in children DOWN SYNDROME ➔ MINIMUM SHUNTING OF BLOOD – left-to-right shunting occurs and pulmonary blood flow increases VENTRICULAR SEPTAL CHD - ACYANOTIC DEFECTS NON-OBSTRUCTIVE LESIONS Abnormal opening between the right and left ventricles. May be classified according to location: membranous (accounting for 80%) or muscular. May vary in size from a small pinhole to absence of the septum, which results in a common ventricle. ➔ VSDs – most likely occur during the first year of life in children having small or moderate defects. ➔ because of the higher pressure within the LEFT VENTRICLE and because the systemic arterial circulation offers more resistance than the pulmonary circulation ➔ blood flows through the DEFECT INTO THE PULMONARY ARTERY 2F PULMONIC STENOSIS CHD - ACYANOTIC DEFECTS OBSTRUCTIVE LESIONS Narrowing at the entrance to the pulmonary artery. Resistance to blood flow causes right ventricular hypertrophy and decreased pulmonary blood flow. Pulmonary atresia is the extreme form of pulmonic stenosis (PS) is that there is total fusion of the commissures and no blood flows to the lungs. The right ventricle may be hypoplastic. ➔ PS is present = resistance to blood flow causes right ventricular hypertrophy ➔ result in reopening of the foramen ovale, shunting of unoxygenated blood into the left atrium, and systemic cyanosis ➔ newborns w/ severe narrowing are cyanotic AORTIC STENOSIS CHD - ACYANOTIC DEFECTS OBSTRUCTIVE LESIONS Narrowing or stricture of the aortic valve, causing resistance to blood flow in the left ventricle, decreased cardiac output, left ventricular hypertrophy, and pulmonary vascular congestion. ➔ the prominent anatomic consequence of aortic stenosis (AS) – is hypertrophy of the LEFT VENTRICULAR WALL ➔ left ventricular hypertrophy also interferes with coronary artery perfusion and may result in myocardial infarction ➔ VALVULAR STENOSIS – most common type usually caused by malformed cusps VALVULAR STENOSIS is a serious defect because: 1. Obstruction tends to be progressive. 2. Sudden episodes of myocardial ischemia/low cardiac output, can result in sudden death. 3. Surgical repair rarely results in a normal valve. MINGUITO, SHANIA D. | BSN 2-B 21 2F – SICK GROWING CHILD narrow part of aorta COARCTATION OF THE AORTA CHD - ACYANOTIC DEFECTS OBSTRUCTIVE LESIONS Localized narrowing near the insertion of the ductus arteriosus, which results in increased pressure proximal to the defect (head and upper extremities) and decreased pressure distal to the obstruction (body and lower extremities). ➔ narrowing within the aorta is increased pressure proximal to the defect (upper extremities) and decreased pressure distal to it (lower extremities) ➔ high blood pressure and bounding pulses in arms, weak or absent femoral pulses, cool lower extremities with lower blood pressure TRANSPOSITION OF THE GREAT ARTERIES CYANOTIC DEFECTS Pulmonary artery leaves the left ventricle, and the aorta exists from the right ventricle, with no communication between the systemic and pulmonary circulations. ➔ SEPTAL DEFECTS/PDA must be present to permit blood to enter the systemic circulation or the pulmonary circulation for mixing of saturated and desaturated blood ➔ MOST COMMON DEFECT = Patent Foramen Ovale ➔ severely cyanotic Atresia - not normal opening HYPOPLASTIC LEFT HEART SYNDROME (4) TETRALOGY OF FALLOT CYANOTIC DEFECTS The classic form includes four defects: USD 1. ventricular septal defect (VSD) stenosis BSA 2.3. pulmonic overriding aorta RVH 4. right ventricular hypertrophy ➔ an example of acyanotic heart defect ➔ if pulmonary vascular resistance is higher than systemic resistance, the shunt is from RIGHT TO LEFT ➔ if systemic resistance is higher than pulmonary resistance the shunt is LEFT TO RIGHT ➔ cyanosis, characteristic murmur, hypoxia – blue spells, emboli, seizures, loss of consciousness/SID 2F LESS COMMON CONGENITAL HEART DEFECT Underdevelopment of the left side of the heart, resulting in a hypoplastic left ventricle and aortic atresia. Most blood form the left atrium flows across the patent foramen ovale to the right atrium, to the right ventricle, and out the pulmonary artery. ➔ descending aorta receives blood from the patent ductus arteriosus supplying systemic blood flow ➔ the amount of blood flow to the pulmonary and systemic circulations depends on the relationship between the pulmonary and systemic vascular resistances ➔ the coronary and cerebral vessels receive blood by RETROGRADE FLOW through the HYPOPLASTIC ASCENDING AORTA. ➔ mild cyanosis, dec. cardiac output, CVC ➔ FATAL IN FIRST MONTHS OF LIFE WITHOUT INTERVENTION MINGUITO, SHANIA D. | BSN 2-B 22 2F – SICK GROWING CHILD TAP VR TRICUSPID ATRESIA/PULMONARY ATRESIA TOTAL ANOMALOUS PULMONARY VENOUS RETURN LESS COMMON CONGENITAL HEART DEFECT LESS COMMON CONGENITAL HEART DEFECT The tricuspid valve fails to develop. ➔ no communication from the RIGHT ATRIUM to the RIGHT VENTRICLE ➔ blood flows through an ATRIAL SEPTAL DEFECT (ASD) / patent foramen ovale to the left side of the heart ➔ COMPLETE MIXING OF UNOXYGENATED AND OXYGENATED BLOOD IN THE LEFT SIDE OF THE HEART ➔ VSD – right ventricle and out to the lungs ➔ cyanosis, tachycardia, dyspnea Rare defect characterized by failure of the pulmonary veins to join the left atrium. Instead, the pulmonary veins are abnormally connected to the systemic venous circuit via the right atrium or various veins draining toward the right atrium, such as the superior vena cava. ➔ MIXED BLOOD BEING RETURNED to the RIGHT ATRIUM and shunted from the right to the left through an ASD – Atrial Septal Defect. ➔ TAPVC – Total Anomalous Pulmonary Venous Connection ➔ cyanosis, asymptomatic ➔ w/o intervention = CF / death "common truncus" TRUNCUS ARTERIOSUS LESS COMMON CONGENITAL HEART DEFECT Failure of normal septation and division of t he embryonic bulbar trunk into the pulmonary artery and the aorta. TAPVC classified as follows: 1. Supracardiac – Attachment above the diaphragm, such as to the superior vena cava. 2. Cardiac – Direct attachment to the heart, such as to the right atrium or coronary sinus. 3. Infradiaphragmatic – Attachment below to the diaphragm, such as to the inferior vena cava (most severe form). ➔ PREFERENTIAL BLOOD FLOW TO THE LUNGS ➔ results in development of SINGLE VESSEL that OVERRIDES both ventricles ➔ blood from both ventricles MIXES in the COMMON GREAT ARTERY – leads to desaturation and hypoxemia ➔ Symptomatic, Mod. – Severe HF, cyanosis, poor growth, activity intolerance 2 common vessel instead of - single Type 1 – A single pulmonary trunk arises near the base of the truncus and divides into the left and right pulmonary arteries. 2F Type 2 – The left and right pulmonary arteries arise separately but in close proximity and at the same level from the back of the truncus. Type 3 – The pulmonary arteries arise independently from the sides of the truncus. MINGUITO, SHANIA D. | BSN 2-B 23 2F – SICK GROWING CHILD SBE RHEUMATIC FEVER ACQUIRED HEART DISEASE Occurs after pharyngitis caused by group A Bhemolytic streptococci (GABHS). Self-limiting illness that involves the joints, skin, brain, serous surfaces, and heart. Rheumatic Heart Disease – Cardiac valve damage, most significant complication of RF. - Ages 5 to 14 years old - principal manifestations are observed in the heart, joints, skin, and central nervous system - major cardiac manifestation involves valvular endocardium, pericardium, and myocardium - most commonly associated in mitral valve Aschoff Bodies – Inflammatory hemorrhagic bullous lesions are formed which cause swelling, fragmentation, and alterations in the connective tissue. - these lesions occur at the heart, blood vessels, brain, and serous surfaces of the joints and pleura ↳ - Subacute Endocarditis ✓ 10-day course for initial therapy of Penicillin or an alternative antibiotic. ✓ SBE prophylaxis is NOT RECOMMENDED. ✓ Salicylates are used to reduce fever and discomfort and to control the inflammatory process, especially in the joints. ✓ Prednisone administration may be indicated in some patients with heart failure. INFECTIOUS ENDOCARDITIS ACQUIRED HEART DISEASE ➔ infection of the valves and inner lining of the heart ➔ potentially damage or destroy the heart valves with high morbidity and mortality for affected pts. ➔ children with CONGENITAL ANOMALIES OF HEART/GREAT VESSELS ➔ children with indwelling catheters are also at risk – affecting the mitral/aortic valve ➔ fever, malaise, murmur Organisms responsible: Rheumatic Fever: Therapeutic and Nursing Care Management ✓ eradication of GABHS (primary prevention) ✓ prevention of permanent cardiac damage ✓ palliation of the other symptoms ✓ encourage compliance with drug regimens ✓ facilitate recovery from the illness ✓ provide emotional support ✓ prevention of recurrences (secondary prevention) ✓ Penicillin (PO or IM) remains drug of choice, with macrolides or cephalosporins as a substitute in penicillin-sensitive children. 2F ✓ ✓ ✓ ✓ 24 Prophylaxis Streptococcus viridans Staphylococcus aureus Gram-negative bacteria, enterococcus Fungi – Candida albicans Therapeutic & NCM: ✓ administration of high-dose antibiotics IV 2-8 weeks ✓ blood culture ✓ counsel parents of high-risk children concerning the need for prophylactic antibiotic therapy ✓ must maintain highest level of oral health to reduce the chance of bacteremia from oral infections MINGUITO, SHANIA D. | BSN 2-B 2F – SICK GROWING CHILD ✓ educate pts. and families to bring unexplained fever, weight loss, change in behavior Nursing Goals: 1. Preparation of child for IV infusion, usually with an intermittent-infusion device, and performance of several venipunctures to draw blood for culture and laboratory values. 2. Use of sterile technique when administering IV antibiotics. 3. Observation for side effects of antibiotics, especially inflammation along venipuncture sites, along with assessments of renal function. 4. Observation for complications, including embolism and HF. 5. Education regarding the importance of follow-up visits for cardiac evaluation, echocardiographic monitoring, and blood culturing. KAWASAKI DISEASE ACQUIRED HEART DISEASE Acute systemic vasculitis of unknown cause. resolves in 6 to 8 weeks damage to the coronary arteries dilation of the coronary arteries winter and early spring outbreak KD involves inflammation of the small and medium-sized blood vessels → coronary arteries being the most susceptible to damage - Inflammatory markers: C-reactive protein level and erythrocyte sedimentation rate - 2F Acute Phase of KD – Begins with an abrupt onset of high fever that is unresponsive to antibiotics and antipyretics. Subacute Phase of KD – Begins with resolution of the fever and lasts until all outward clinical signs of KD have disappeared. If changes in the coronary arteries occur, some enlargement or dilation is generally evident by echocardiography during the second week of illness. Convalescent Phase of KD – Clinical signs of KD have mostly resolved, but the laboratory values are still abnormal. This phase is complete when all blood values return to normal (6 to 8 weeks after onset). At the end of this stage, parents report that the child appears to have returned to normal in terms of temperament, energy, and appetite. Kawasaki Disease: Therapeutic Nursing Care Management and ✓ Salicylate therapy ✓ Steroids, infliximab, cyclosporine ✓ Aspirin is given initially to control fever and symptoms of inflammation. ✓ Additional anticoagulation therapy, such as clopidogrel or warfarin administration, may be indicated in children with moderate or giant coronary enlargement, respectively. ✓ Nurse must focus on symptomatic relief, emotional support, diagnostic assistance, medication administration, and education of the child and family. TAKE NOTE: REINFORCEMENT It causes swelling and inflammation in the walls of small to medium-sized blood vessels that carry blood throughout the body. MINGUITO, SHANIA D. | BSN 2-B 25 2F – SICK GROWING CHILD ANEMIA 1. Replacement of bone marrow by fibrous tissue or by neoplastic cells, as in leukemia. 2. Depression of marrow activity by irradiation, chemicals, or drugs; and 3. Interference with bone marrow activity caused by systemic disorders such as severe infection, chronic renal disease, widespread malignancy, collagen disease, or hypothyroidism. IRON DEFICIENCY ANEMIA ANEMIA - ALTERATIONS IN HEMATOLOGIC FUNCTION Caused by an inadequate supply or loss of iron. inadequate supply of iron impaired iron absorption blood loss excessive demands for iron required for growth - At birth the full-term infant has approx. 0.5 supply or iron. - Average of 0.8mg of iron must be absorbed each day during the first 15 years of life. - During the last trimester of pregnancy, iron is transferred from the mother to the fetus at the rate of 4mg/day. - IDA enhances the leakage of plasma proteins, which causes edema; retarded growth; and decreased serum concentration of the proteins album, gamma globulin, and transferrin. - Iron supplements are administered in two divided doses between meals, when the presence of free hydrochloric acid is greatest, and are accompanied by a citrus fruit or juice, which helps reduce iron to its most soluble state. 2F IDA: Therapeutic Management and Nursing Care ✓ Prevention is the primary goal. – Proper nutrition and more iron supplements. ✓ Use only breast milk for the first 12 months. ✓ Iron suppl. of 1mg/kg/day should be provided by 4 to 6 months of age in a full-term infant. While, 2 mg/kg/day by 2 months of age in preterm infants. ✓ Administer iron drops. ✓ Limit the amount of formula to no more than 1 L/day. ✓ Iron medication must continue for 2 to 3 months after blood values normalize to replenish the body’s iron stores. ✓ Iron ingested in excessive quantities is toxic, even fatal, parents should keep no more than a 1-month supply in the home and store it safely away from the reach of children. NORMOCYTIC ANEMIA ANEMIA - ALTERATIONS IN HEMATOLOGIC FUNCTION Normochromic (normal color) or normocytic (normal cell size) anemia occur because of impaired production of erythrocytes by the bone marrow or by abnormal or uncompensated loss of circulating red blood cells, as with acute hemorrhage. The red blood cells appear normal in both color and size; however, there are simply too few of them for effective oxygen transport. Etiology: ➔ breaking up of red blood cells ➔ decreased RBC production ➔ increased RBC destruction ➔ blood loss, or other etiologies ➔ acute blood loss ➔ bone marrow failure ➔ chronic disease o Kidney disease, Rheumatoid arthritis and thyroiditis o Destruction (hemolysis) MINGUITO, SHANIA D. | BSN 2-B 26 2F – SICK GROWING CHILD Acute Blood-Loss Anemia – which can occur from trauma such as an automobile accident with internal bleeding from acute nephritis in which blood is lost in the urine o in the newborn from disorders such as placenta previa, premature separation of the placenta, maternal-fetal or twin-to-twin transfusion, or trauma to the cord or placenta. Risk Assessment: - fatigue - getting tired so much easily - dizziness - SOB (shortness of - lack of energy - weakness breath) S/S: - pale, dizziness, SOB, fatigue, weakness, lack of energy, irritability Diagnostic Evaluation: CBC, reticulocyte test, bone marrow biopsy Therapeutic & NCM: ✓ Discontinue any drug or chemical suspected of causing the bone marrow dysfunction and remove the substance from the child’s environment to avoid exposure. ✓ Monitor the vital signs. ✓ History of alcohol intake. ✓ Provide an adequate nutritional diet. ✓ Blood transfusion ✓ Erythropoietin ✓ ATG IV Anti Thymocyte Globulin) ✓ Bone marrow biopsy 2F SICKLE-CELL ANEMIA ANEMIA - ALTERATIONS IN HEMATOLOGIC FUNCTION Group of hereditary disorders, all of which are related to the presence of HgbS. Administration of pneumococcal, H. influenzae type B, and meningococcal vaccines is recommended. TAKE NOTE: REINFORCEMENT Is an inherited disorder characterized by defective hemoglobin and affects the shape of the cells. Correct term: SCA are HgBSS Disease and Homozygous Sickle Cell Disease - SCA – The homozygous form of the disease (HgbSS), in which valine, an amino acid, is substituted for glutamic acid at the sixth position of the B chain. - Sickle Cell C Disease – A heterozygous variant of SCD (HgbSC), characterized by the presence of both HgbS and hemoglobin C (HgbC), in which lysine is substituted for glutamic acid at the sixth position of the B chain. - Sickle Thalassemia Disease – Combination of sickle cell trait and Bthalassemia trait. - Mode of Transmission: Genes One of a group of diseases collectively termed hemoglobinopathies. Basic defect responsible for the sickling of erythrocytes is contained in the globin fraction of hemoglobin, which is composed of 574 amino acids. Hemoglobinopathies – Normal adult hemoglobin (HgbA) is partly or completely replaced by abnormal sickle hemoglobin (HgbS). MINGUITO, SHANIA D. | BSN 2-B 27 2F – SICK GROWING CHILD Manifestations of SCA: B-THALASSEMIA 1. Obstruction caused by the sickled RBCs. 2. Vascular inflammation 3. Increased RBC destruction. Diagnostic Evaluation: & Nursing Care ✓ Prevent sickling phenomenon. ✓ Prevent stroke. ✓ Hypoxia prevented when surgery is necessary. ✓ Assessment of the child in sickle cell crisis includes all areas and systems. ✓ Minimize tissue deoxygenation. ✓ Encourage screening and genetic counseling. ✓ Promote hydration. ✓ Bed rest to minimize energy expenditure and to improve oxygen utilization. ✓ Hydration through oral and IV therapy. ✓ Electrolyte replacement, since hypoxia results in metabolic acidosis, which also promotes sickling. ✓ Analgesia for severe pain from vasoocclusion. ✓ Blood replacement to treat anemia and to reduce the viscosity of the sickled blood. ✓ Antibiotic therapy to treat any existing infection. – Penicillin 2F Thalassemia, Greek of “Thalassa” → Sea Inherited blood disorders characterized by deficiencies in the rate of production of specific globin chains in hemoglobin. Refers to people Mediterranean sea. 1. Stained blood smear 2. Sickle Turbidity Test (Sickledex) 3. Hemoglobin Electrophoresis SCA: Therapeutic Management: ANEMIA - ALTERATIONS IN HEMATOLOGIC FUNCTION living near the Thalassemia → Excess of hemosiderin, the iron-containing pigment from the breakdown of hemoglobin, results from decreased hemoglobin synthesis and increased hemolysis of transfused erythrocytes. - autosomal recessive disorder TAKE NOTE: REINFORCEMENT Is an autosomal recessive anemia associated with abnormalities with the b chain of adult hemoglobin. Manifestations: - anemia (before diagnosis) - progressive anemia o chronic hypoxia o headache o bone pain o decreased exercise tolerance o listlessness o anorexia - small stature - delayed sexual maturation - bone changes Hemosiderosis – Excess iron storage in various tissues of the body. Hemochromatosis – Excess iron storage that results in cellular damage. MINGUITO, SHANIA D. | BSN 2-B 28 2F – SICK GROWING CHILD B-Thalassemia: Therapeutic and Nursing Care Management ✓ promote compliance with transfusion and chelation therapy ✓ assist the child in coping with the anxiety-provoking treatments and the effects of the illness ✓ foster the child’s and family’s adjustment to a chronic illness ✓ observe for complications of multiple blood transfusions ✓ all families with a child with thalassemia should be tested for the trait and referred for genetic counseling ✓ improved physical and psychologic well-being because of the ability to participate in normal activities ✓ decreased cardiomegaly and hepatosplenomegaly ✓ fewer bone changes ✓ normal or near-normal growth and development until puberty, and ✓ fever infections ✓ Vit C – only to pt. who are ascorbate depleted ✓ Deferoxamine 2F APLASTIC ANEMIA ANEMIA - ALTERATIONS IN HEMATOLOGIC FUNCTION Production of the formed elements of the blood is simultaneously depressed. - can be congenital, or present at birth, or acquired - human parvovirus infection, hepatitis, or overwhelming infection - decreased platelet count - bone marrow → red bone marrow to yellow, fatty bone Diamond-Blackfan Syndrome – Congenital condition, marked by complete or almost complete absence of all cells of the erythroid series. Fanconi Syndrome – Pancytopenia, hypoplasia of the bone marrow, and patchy brown discoloration of the skin due to the deposition of melanin. Aplastic Anemia: Therapeutic and Nursing Care Management: ✓ must restore the function of the narrow o immunosuppressive therapy – counter presumed immunologic responses that prolong aplasia o bone marrow transplantation ✓ prepare the child and family for diagnostic and therapeutic procedures, preventing complications from severe pancytopenia, and emotionally supporting the family in the face of potentially fatal outcome MINGUITO, SHANIA D. | BSN 2-B 29 2F – SICK GROWING CHILD HEMOPHILIA CLOTTING DISORDERS - ALTERATIONS IN HEMATOLOGIC FUNCTION Refers to a group of bleeding disorders resulting from congenital deficiency, dysfunction, or absence of specific coagulation proteins or factors. - transmitted as an x-linked recessive disorder - prolonged bleeding anywhere from or in the body - Hemarthrosis – Refers to the bleeding into the joint cavities. RICE → Elevation Rest, Ice, Compression, and VON WILLEBRAND DISEASE CLOTTING DISORDERS - ALTERATIONS IN HEMATOLOGIC FUNCTION Severe: <1% - Spontaneous bleeding without trauma Moderate: 1% to 5% - Bleeding with trauma Mild: >5% to 40% - Bleeding with severe trauma or surgery Hemophilia: Therapeutic and Nursing Care Management: ✓ recognize the signs that indicate bleeding ✓ prevent bleeding ✓ bleeding episodes treated early with factor replacement ✓ exercise and physical therapy ✓ nurse must maintain a high level of suspicion when a child with hemophilia shows signs such as headache; slurred speech; loss of consciousness; bleeding, and black tarry stools ✓ primary therapy is to replace the missing clot factor ✓ AVOID aspirin and NSAIDs because they inhibit platelet function ✓ However, Ibuprofen are effective in relieving pain caused by synovitis and must be used with caution. 2F Hereditary bleeding disorder characterized by a deficiency of or defect in a protein called Von Willebrand factor (vWF). vWF Protein → Contributes to the adherence of platelets to damaged endothelium and serves as a carrier protein for factor VIII. ➔ results in prolonged bleeding time because platelets fail to adhere to the walls of the ruptured vessel to form a platelet plug ➔ s/s: frequent nosebleeds, gingival bleeding, easy bruising, excessive menstrual bleeding (menorrhagia) VWD: Nursing Care Management: ✓ be calm, to alleviate anxiety and promote child’s cooperation ✓ nosebleed – child must breathe from the mouth Epistaxis Management: 1. Sit up and lean forward (do not lie down). 2. Apply pressure to nose with thumb and forefinger for at least 10 minutes. MINGUITO, SHANIA D. | BSN 2-B 30 2F – SICK GROWING CHILD 3. Insert cotton into each nostril and apply ice to bridge of nose if bleeding persists. 4. Keep child calm and quiet. DISSEMINATED INTRAVASCULAR COAGULATION CLOTTING DISORDERS - ALTERATIONS IN HEMATOLOGIC FUNCTION Diffuse fibrin deposition in the microvasculature, consumption of coagulation factors, and endogenous generation of thrombin and plamin. ➔ secondary disorder ➔ complication of a number of pathologic processes ➔ hallmark signs: bleeding and clotting – occurs simultaneously ➔ petechiae, purpura, bleeding from openings in the skin, bleeding from umbilicus, trachea, GI bleeding, hypotension, organ dysfunction DIC: Therapeutic Management: and Nursing Care ✓ platelets and fresh frozen plasma may be needed to replace lost plasma components ✓ recognize the signs that might indicate its presence ✓ monitor IV infusion and blood transfusions 2F IDIOPATHIC THROMBOCYTOPENIC PURPURA CLOTTING DISORDERS - ALTERATIONS IN HEMATOLOGIC FUNCTION Purpura – Infrequent sign at presentation. ➔ hemorrhagic disorder by thrombocytopenia, absence to severe signs of bleeding (e.g., easy bruising, mucosal bleeding, petechiae, menorrhagia), and normal bone marrow with a normal or increased number of immature megakaryocytes and esinophils Types: - Acute – URT (MMR, or chickenpox; after infection with human parvovirus) - Self-Limiting Course (Chronic) - >12 months’ duration. ITP: Therapeutic Management: ✓ ✓ ✓ ✓ and Nursing Care activity is restricted prevent serious bleeding episodes treatment administered w/o SEs anti-D antibody → after administration of anti-D antibody, observe the child for a min. of 1 hr. and maintain a patent IV line. Obtain baseline VS measurements before the infusion and again 5, 20, and 60 minutes after beginning the infusion. If fever, chills, or headache occurs during or shortly after the infusion, the nurse should administer acetaminophen, diphenhydramine, and/or hydrocortisone. Observe the patient for an additional hr. after the anti-D antibody infusion is complete. MINGUITO, SHANIA D. | BSN 2-B 31 2F – SICK GROWING CHILD NEUROBLASTOMA ALTERATIONS IN CELLULAR GROWTH Most common extracranial solid tumor of childhood and the most common cancer diagnosed in infancy. ➔ originate from embryonic neural crest cells that normally give rise to the adrenal medulla and the sympathetic nervous system ➔ adrenal gland or retroperitoneal sympathetic chain ➔ Primary Site: Within abdomen; include head and neck region, chest, and pelvis. Manifestations: - firm, nontender, irregular mass in the abdomen that crosses the midline - compression of kidney, ureter, or bladder may cause urinary frequency or retention Stages of Neuroblastoma: Stage 1 – Localized tumor that is confined to the area of origin capable of complete gross excision; representative ipsilateral lymph nodes negative for tumor microscopically (nodes that are attached to and removed with the primary tumor may be positive). Stage 2-A – Unilateral tumor with incomplete gross resection; representative ipsilateral nonadherent lymph nodes and contralateral lymph nodes negative for tumor microscopically. Stage 2-B – Unilateral tumor with or without complete gross excision, with ipsilateral nonadherent lymph nodes positive for tumor; enlarged contralateral lymph nodes must be negative microscopically. 2F Stage 3 – Tumor infiltrating across the midline, with or without regional lymph node involvement; or localized unilateral tumor with contralateral regional lymph node involvement; or midline tumor with bilateral lymph node involvement. Stage 4 – Dissemination of tumor to distant lymph nodes, bone, bone marrow, liver, skin, and/or other organs. Stage 4-S – Localized primary tumor (as defined for stage 1, 2-A, or 2-B) with dissemination limited to liver, skin, or bone marrow but not to bone. Neuroblastoma: Therapeutic and Nursing Care Management: ✓ remove as much of the tumor as possible and to obtain biopsies ✓ chemotherapy – mainstay of therapy ✓ prevent postop. complications for abdominal, thoracic, or cranial surgery ✓ parents need much support in dealing with these feelings and expressing them to the appropriate people WILM’S TUMOR (NEPHROBLASTOMA) ALTERATIONS IN CELLULAR GROWTH Common kidney tumor of childhood. - painless swelling/mass within abdomen hematuria, anemia, hypertension weight loss and fever dyspnea, cough, SOB, pain in the chest Staging of Wilms Tumor: Stage 1 – Tumor is limited to one kidney and completely resected. Stage 2 – Tumor extends beyond kidney but is completely resected; lymph nodes do not contain tumor. Stage 3 – Residual tumor confined to abdomen that may have disease in nearby lymph nodes or abdominal space. Stage 4 – Hematogenous metastases with disease spread to the lung, liver, bone, brain, or distant lymph nodes. MINGUITO, SHANIA D. | BSN 2-B 32 2F – SICK GROWING CHILD Stage 5 – Bilateral renal involvement is present at diagnosis. WILMS: Therapeutic and Nursing Care Management: ✓ surgery + chemotherapy ✓ same nursing care to other cancers treated with surgery, irradiation, and chemotherapy EWING’S SARCOMA (BONE TUMOR) ALTERATIONS IN CELLULAR GROWTH Primitive neuroectodermal tumor of the bone, are the second most common malignant bone tumor. ➔ arises in the marrow spaces of the bone rather from the osseous tissue ➔ tumor originates from the shaft of long and trunk bones, most often affecting the pelvis, femur, tibia, fibula, humerus, ulna, vertebra, scapula, ribs, and skull OSTEOSARCOMA (BONE TUMOR) ALTERATIONS IN CELLULAR GROWTH Most common bone cancer in children and most commonly affects patients in the second decade of life during their growth spurt. Therapeutic & Nursing Care Management: ✓ surgical biopsy ✓ limb salvage procedure ✓ all gross and microscopic tumors must be resected ✓ chemotherapy plays a vital role in treatment of osteosarcoma ✓ straightforward honesty is essential in gaining the child’s cooperation and trust ✓ nurse should be present at the discussion ✓ nurse must be careful not to overwhelm children with information ✓ nurse must be considerate and mindful of the child’s feelings 2F Ewing’s: Therapeutic and Nursing Care Management: ✓ limb salvage might be feasible ✓ radiotherapy and chemotherapy ✓ prepare the client and the family on the different tests ✓ child should wear loose-fitting clothes over the irradiated area t o minimize additional skin irritation ✓ protect the area from sunlight and sudden changes in temperature (heating pads/ice packs) – due to increased sensitivity ✓ encourage child to use the extremity as tolerated MINGUITO, SHANIA D. | BSN 2-B 33 2F – SICK GROWING CHILD LEUKEMIA ALTERATIONS IN CELLULAR GROWTH Cancer that starts in blood-forming tissue, such as the bone marrow, and causes large numbers of abnormal blood cells to be produced and enter the bloodstream. Types: 1. Acute Lymphocytic Leukemia (ALL) – This is the most common type of leukemia in young children. All can also occur in adults. This type of leukemia begins in the B or T lymphocytes, which are immature white blood cells. Lymphocytes are the building blocks of the lymphoid tissues that make up the immune system. antchen 2. Acute Myelogenous Leukemia (AML) – AML is the most common type of acute leukemia in adults. Myeloid stem cells usually mature in to abnormal myeloblasts, or white blood cells. But, they sometimes become abnormal red blood cells or platelets. As they multiply, they overwhelm the normal cells in the bone marrow and blood. The cancer cells can also spread to other parts of the body. adults Signs & Symptoms: - fever/chills persistent fatigue, weakness frequent or severe infections losing weight w/o trying swollen lymph nodes enlarged liver/spleen easy bleeding/bruising recurrent nosebleeds tiny red spots in your skin (petechiae) excessive sweating, esp. at night bone pain/tenderness Diagnostic Tests: PE, CBC, bone marrow test Therapeutic & NCM: ✓ Obtain health history which may reveal some symptoms reported by the patient before problem is detected on PE. ✓ Conduct a physical assessment. ✓ Monitor lab results. ✓ Provide emotional support, education, listen, help in decision making. ✓ Chemotherapy – Tr for Leukemia HODGKIN’S DISEASE SOFT TISSUE TUMORS - ALTERATIONS IN CELLULAR GROWTH 3. Chronic Lymphocytic Leukemia (CLL) – Begins in the B lymphocytes. As the abnormal cells proliferate, they crowd out the normal cells. Originates in the lymphoid system and primarily involves the lymph nodes. 4. Chronic Myelogenous Leukemia (CML) – Occurs when a genetic change turns the myeloid cells into immature cancer cells. These cells then grow slowly and overwhelm the healthy cells in the bone marrow and blood. Classified into Four Histologic Types: 2F - spleen, liver, bone marrow, lungs, and mediastinum 1. lymphocytic predominance 2. nodular sclerosis 3. mixed cellularity 4. lymphocytic depletion MINGUITO, SHANIA D. | BSN 2-B 34 2F – SICK GROWING CHILD Staging of Hodgkin Disease: Stage 1 – Lesions are limited to one lymph node area or only one additional extralymphatic site (I-E), such as the liver, lungs, kidney, or intestines. Stage 2 – Two or more lymph node regions on the same side of the diaphragm or one additional extralymphatic site or organ (II-E) on the same side of the diaphragm is involved. Stage 3 – Lymph node regions on both sides of the diaphragm and has spread to one extralymphatic site (III-3), spleen (III-S), or both (III-SE). Stage 4 – Cancer has metastasized diffusely throughout the body to one or more extralymphatic sites with or without involvement of associated lymph nodes. - complete blood count uric acid levels liver function tests C-reactive protein radiographic tests Hodgkin’s: Therapeutic and Nursing Care Management: ✓ follow-up care of children no longer receiving therapy is essential to identify relapse and second malignancies ✓ immunizations against pneumococci and meningococci are recommended before the splenectomy ✓ explain the treatment side effects – child and family support ✓ nurse should discuss a feasible school schedule with the parents and child 2F NON-HODGKIN’S DISEASE SOFT TISSUE TUMORS - ALTERATIONS IN CELLULAR GROWTH - Disease is usually diffuse rather than nodular. - Cell type is evenly split between B-cell and T-cell lineages. - Dissemination occurs earlier, more often, and more rapidly. Staging of Non-Hodgkin Lymphoma: Stage 1 – Disease is limited to one lymph node area or only one additional extralymphatic site (I-E). Stage 2 – Two or more lymph node regions on the same side of the diaphragm or one additional extralymphatic site or organ (II-E) on the same side of the diaphragm. Stage 3 – Tumor on both sides of abdomen and may have spread to an area or organ next to the lymph nodes (IIIE), spleen (IIIS), or both (IIISE). Stage 4 – Tumor has spread into any organ that is not right next to an involved node, and/or the tumor has spread to the central nervous system or bone marrow. Non-Hodgkin’s: Therapeutic and Nursing Care Management: ✓ irradiation and chemotherapy ✓ lymphoblastic lymphoma → chemotherapeutic drugs – cyclophosphamide ✓ nonlymphoblastic lymphoma – cyclic drug combinations → cyclophosphamide and high-dose methotrexate ✓ administered 6 to 24 months ✓ nursing care is similar to cancer MINGUITO, SHANIA D. | BSN 2-B 35 2F – SICK GROWING CHILD RHABDOMYOSARCOMA SOFT TISSUE TUMORS - ALTERATIONS IN CELLULAR GROWTH Most common soft tissue sarcoma in children. Arises from embryonic mesenchyme with three recognized subtypes. - occurs in the head and neck - more common in males – 6 years or younger - originate from: o muscles o tendons o bursae o fascia o fibrous o connective o lymphatic o vascular tissue TAKE NOTE: REINFORCEMENT Is a rare type of cancer that forms in soft tissue specifically skeletal muscle tissue or hollow organs such as bladder or uterus. Staging of Rhabdomyosarcoma: Group 1 – Localized disease; tumor completely resected and regional nodes not involved. Rhabdomyosarcoma: Therapeutic Nursing Care Management: and ✓ complete removal of tumor ✓ radical procedures with high morbidity should be avoided ✓ careful assessment for signs of the tumor ✓ supportive care during each stage of therapy ✓ emotional support of the family RETINOBLASTOMA SOFT TISSUE TUMORS - ALTERATIONS IN CELLULAR GROWTH Arises from the retina, most common intraocular malignancy of childhood. Whitish “glow” in the pupil → cat’s eye reflex or leukocoria - caused by genetic alterations Rb gene - germ-line mutation - chromosomal deletion (chromosome 13) - increased incidence of cognitive impairment and congenital malformations Group 2 – Localized disease with microscopic residual that may have spread into nearby lymph nodes. Group 3 – Incomplete resection with gross residual disease; disease may have spread into nearby lymph nodes but not into distant organs. Group 4 – Metastatic disease present at diagnosis. 2F - indirect ophthalmoscopy, ultrasound, CT, and MRI scans MINGUITO, SHANIA D. | BSN 2-B 36 2F – SICK GROWING CHILD International Classification for Intraocular Retinoblastoma: Group A – Small (3 mm or less) intraretinal tumors away from the optic disc and foveola. Group B – All remaining tumors that are larger than 3 mm and/or close to the optic disc or foveola but remain confined to the retina. Group C – Discrete local disease with minimal amounts of disease under the retina (subretinal seeding) or into the gelatinous material of the eye (vitreous seeding). Group D – Large or poorly defined tumors with significant vitreous or subretinal seeding; retina may have become detached from the back of the eye. Group E – Tumor is very large, extending near the front of the eye, is bleeding or causing glaucoma, or has other features that indicate there is no means to save the eye. Retinoblastoma: Therapeutic and Nursing Care Management: ✓ enucleation – no salvage of vision ✓ irradiation – for vitreous seeding ✓ chemotherapy – decrease the tumor size (plaque brachytherapy) ✓ photocoagulation – destroy retinal blood vessels that supply nutrition to the tumor ✓ cryotherapy – freezing the tumor, which destroys microcirculation to the tumor and the cells themselves through microcrystal formation ✓ prepare the family for diagnostic and therapeutic procedures and home care ✓ child may not see clearly after procedure → SENSITIVE TO LIGHT ✓ encourage the parents to participate in dressing changes – eye patches and etc. ✓ safety measures should be practiced at all times 2F CLEFT LIP AND CLEFT PALATE ALTERATIONS IN GASTROINTESTINAL FUNCTION Most common birth defect. ➔ exposure to environmental factors or teratogens may be responsible for clefts at a critical point in embryonic development ➔ alcohol use, cigarette smoking, and prescription drugs, including anticonvulsants, steroids, and retinoids ➔ FOLIC ACID supplements may protect against clefting CLEFT LIP - multifactorial inheritance, environmental factors, familial occurrence - male predominance - unilateral/bilateral - external nose, nasal cartilages, nasal septum, maxillary alveolar ridges, dental anomalies - 2-3 mos. surgical repair, early use of orthodontics - nasal alveolar molding - feeding and weight gain CLEFT PALATE - associated w/ syndromes (chromosomal), familiar occurrence, environmental factors such as maternal alcohol ingestion, smoking, or teratogens - female predominance - soft palate/hard palate - midline/posterior palate - may involve nostril and absence of nasal septal development (communication with oral and nasal cavity) - surgical repair for isolated Cp between 6-12 months; infants with CL/CP between 9-15 months - feeding efficiency; growth failure MINGUITO, SHANIA D. | BSN 2-B 37 2F – SICK GROWING CHILD - feeding cup, syringe feeding, special needs feeder, pigeon bottle, cleft palate nurser; avoid spoon, fork Therapeutic & NCM: ✓ cleft/craniofacial multidisciplinary team ✓ plastic surgery, otolaryngology, orthodontics, speech-language, pediatrics, nursing, audiology, social work, psychology ✓ surgical closure of the cleft ✓ nurse must address not only the infant’s physical needs but also the parents’ emotional needs ✓ nurse should encourage expression of parental grief and fears ESOPHAGEAL ATRESIA & TRACHEOESOPHAGEAL FISTULA ALTERATIONS IN GASTROINTESTINAL FUNCTION Rare malformations that represent a failure of the esophagus to develop as a continuous passage and a failure of the trachea and esophagus to separate into distinct structures. ➔ EA – frothy saliva in the mouth & nose, drooling, choking, and coughing, mild/significant respiratory distress ➔ EA – if fed, the infant may swallow normally but suddenly cough and gag, with return of fluid through the nose and mouth, the infant may become cyanotic and apneic because of aspiration of formula or saliva ➔ EA w/ TEF (Type C) – stomach becomes distended with air, and thoracic and abdominal compressions (especially during crying) cause the gastric contents to be regurgitated through the fistula and into the trachea, producing chemical PNEUMONITIS ➔ NG-orogastric (OG) catheter into the esophagus ➔ When EA w/ TEF is suspected, the infant is IMMEDIATELY DEPRIVED OF ORAL INTAKE. 2F 38 Polyhdramnios – Accumulation of 2000 mL of amniotic fluid. Tracheomalacia – May occur as a result of weakness in the tracheal wall that exists when a dilated proximal pouch compresses the trachea early in fetal life. EA & TEF: Therapeutic & NCM: ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ maintenance of a patent airway prevention of pneumonia gastric/blind pouch decompression supportive therapy surgical repair of the anomaly IV fluids are initiated and the infant is positioned to facilitate drainage of secretions and decrease the likelihood of aspiration accumulated secretions are suctioned frequently from the mouth and pharynx infants head is kept UPRIGHT to facilitate removal of fluid collected nursing responsibility for detection of this serious malformation begins immediately after birth assist in pre-op care, post-op care, special problems, family support, discharge planning, and home care. Esophagus-failure todevelop passage Esophagus &trachea-failure toseparate MINGUITO, SHANIA D. | BSN 2-B 2F – SICK GROWING CHILD PYLORIC STENOSIS ALTERATIONS IN GASTROINTESTINAL FUNCTION Occurs when the ferential muscle of the pyloric sphincter becomes thickened, resulting in elongation and narrowing of the pyloric canal. This produces an outlet obstruction and compensatory dilation, hypertrophy, and hyperperistalsis of the stomach. ➔ develops in the first few weeks of life, causing nonbilious vomiting (occurs after feeding) Cregurgitation) ➔ projectile vomiting may develop if the infant is fussy and hungry after vomiting ➔ if not diagnosed asap → dehydration, metabolic alkalosis, and failure to thrive may occur ➔ common in FIRSTBORN MALES ➔ inheritance is polygenic, with an increased risk in the siblings and offspring of affected persons Pyloromyotomy (Fredet-Ramstedt Operative Procedure) – Performed by laparoscope and consists of a longitudinal incision through the circular muscle fibers of the pylorus down to, but not including, the submucosa. incision to wall of . . PYLOMS Therapeutic & NCM: ✓ surgical relief of the pyloric obstruction by pyloromyotomy is the standard therapy ✓ pre-op → infant must be rehydrated and metabolic alkalosis corrected with parenteral fluid and electrolyte administration ✓ replacement fluid therapy usually delays surgery for 24 to 48 hours ✓ stomach is decompressed with an NG tube if the infant continues with vomiting ✓ infant = no evidence of fluid & electrolyte imbalance → surgery is performed without delay ✓ nurse must observe for clinical features that help establish the diagnosis 2F ✓ careful regulation of fluid therapy ✓ reestablishment of normal feeding patterns ✓ nurses must be alert to signs of HPS in infants and refer them for medical evaluation ✓ HPS should be considered a possibility in the very young infant who appears alert but fails to gain weight and has a history of vomiting after feedings ✓ assessment should be based on observation of eating behaviors, evidence of characteristic clinical manifestations, hydration, and nutritional status ✓ careful monitoring of the IV fluids and strict monitoring of intake and output are important ✓ observe VS – fluid/electrolyte imbalances GASTROESOPAGEAL REFLUX ALTERATIONS IN GASTROINTESTINAL FUNCTION Transfer of gastric contents into the esophagus. This phenomenon is physiologic, occurring throughout the day, most frequently after meals and at night. ➔ peak: 4 months of age ➔ PASSIVE REGURGITATION (18 mos.) ➔ failure to thrive, respiratory problems, dysphagia develops ➔ prone to develop GER o premature infants o bronchopulmonary dysplasia o tracheoesophageal/esophageal atresia repairs o neurologic disorders o scoliosis o asthma o cystic fibrosis o cerebral palsy ➔ avoid caffeine, citrus, tomatoes, alcohol, peppermint, spicy/fried foods ➔ thickened feedings & upright positioning MINGUITO, SHANIA D. | BSN 2-B 39 2F – SICK GROWING CHILD Nissen Fundoplication – Most common surgical procedure. This surgery involves passage of the gastric fundus behind the esophagus to encircle the distal esophagus. GER: Therapeutic & NCM: ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ adequate weight gain limited spitting up or vomiting good sleep habits no recurrent pneumonias educate parents regarding home care – including feeding, positioning, and medications when indicated care for child undergoing surgical intervention parents should not place infants on their sides as an alternative to fully supine sleeping avoid of soft bedding and soft objects in the bed is important if severe – NG tube feedings may decrease the amount of emesis and provide constant buffering of gastric acid OMPHALOCELE ALTERATIONS IN GASTROINTESTINAL FUNCTION True failure of embryonic development. Occurs when there is failure of the caudal or lateral infolding of the abdominal wall. Post-op: ✓ mechanical ventilation ✓ parenteral nutrition ✓ intraabdominal compression – prevents effective respiration and restrict blood flow to the lower extremities & abdominal organs ✓ feedings may resume once adequate bowel function is established ✓ observe for infection, evisceration, intestinal volvulus, obstruction, and ventral hernia Long-term complications include: ✓ ✓ ✓ ✓ GER failure to thrive ventral hernia feeding issues ➔ 3rd week of gestation ➔ usually covered only by a translucent peritoneal sac ➔ the sac may contain only a small portion of the bowel or most of the bowel and other abdominal viscera such as the liver 2F TAKE NOTE: REINFORCEMENT Is a congenital abnormality in which some of the abnormal organs protrude through an opening in the abdominal muscles of the umbilical cord. MINGUITO, SHANIA D. | BSN 2-B 40 2F – SICK GROWING CHILD INTUSSUSCEPTION ALTERATIONS IN GASTROINTESTINAL FUNCTION Most common cause of intestinal obstruction in children. Occurs when a proximal segment of the bowel telescopes into a more distant segment, pulling the mesentery with it. Mesentery is compressed and angled, resulting in lymphatic and venous obstruction. TAKE NOTE: REINFORCEMENT Is a condition in which part of the intestine slides into an adjacent part of the intestine. ➔ 3 mos. – 6 years ➔ more common in males ➔ ILEOCECAL VALVE (common site) ➔ sudden acute abdominal pain ➔ child screaming and drawing the knees onto the chest ➔ child appearing normal and comfortable between episodes of pain ➔ vomiting, lethargy ➔ passage of red, current jelly-like stools ➔ tender, distended abdomen ➔ palpable SAUSAGE-SHAPED mass in upper right quadrant ➔ empty lower right quadrant → DANCE SIGN ➔ eventual fever, prostration, and other signs of peritonitis Therapeutic & NCM: ✓ air enema, saline enema ✓ IV fluids, NG decompression, and antibiotic therapy ✓ nurse can help establish a diagnosis by listening to the parent’s description of the child’s physical and behavioral symptoms ✓ nurse prepares the parents for the immediate need for hospitalization ✓ maintenance of NPO status, routine lab testing (CBC and urinalysis), signed parental consent, and pre-anesthetic sedation are performed ✓ children with perforation → IV fluids, systemic antibiotics, bowel decompression before undergoing surgery ✓ observe VS, BP, intact sutures and dressing, and the return of bowel sounds Passage of a normal brown stool usually indicates that the intussusception has reduced itself. This is immediately reported to the practitioner, who may choose to alter the diagnostic and therapeutic care plan. The classic signs and symptoms of intussusception may not be present; a more chronic picture may occur, characterized by diarrhea, anorexia, weight loss, occasional vomiting, and periodic pain. The older child may have pain without other signs or symptoms. Because this condition is potentially life threatening, be aware of such signs, and closely observe and refer these children for further medical investigation. 2F MINGUITO, SHANIA D. | BSN 2-B 41 2F – SICK GROWING CHILD HIRSCHSPRUNG’S DISEASE ALTERATIONS IN GASTROINTESTINAL FUNCTION Congenital anomaly that results in mechanical obstruction from inadequate motility of part of the intestine. TAKE NOTE: REINFORCEMENT A birth defect characterized by the absence of a particular nerve cells in a segment of a bowel. ➔ more common in males ➔ SHORT-SEGMENT DISEASE ➔ relates due to the absence of GANGLION cells in the affected areas of the intestine, resulting in a loss of the rectosphincteric reflex and an abdominal microenvironment of the cells ➔ CONGENITAL AGANGLIONIC MEGACOLON – primary defect, which is the absence of ganglion cells in the myenteric plexus of Auerbach and the submucosal plexus of Meissner ➔ LONG-SEGMENT HD – entire colon or part of the small intestine may be involved ➔ TOTAL CLONIC AGANGLIONOSIS – there is no innervation of the large and small intestine from the anus to the ileocecal valve 2F Therapeutic & NCM: ✓ soave pull-through, Swenson procedure, Duhamel procedure ✓ main objectives are to help the parents adjust to a congenital defect in their child, foster infant-parent bonding ✓ prep the parents for med-surg intervention ANORECTAL MALFORMATIONS ALTERATIONS IN GASTROINTESTINAL FUNCTION Rectal Atresia – Complete obstruction (inability to pass stool) and requires immediate surgical intervention. Rectal Stenosis – May not become apparent until later in infancy when the infant has a history of difficult stooling, abdominal distention, and ribbonlike stools. Persistent Cloaca – Complex anorectal malformation in which the rectum, vagina, and urethra drain into a common channel opening into the perineum. PSARP – common surgical procedure for the repair of anorectal malformations POSTERIOR SAGGITAL ANORECTOPLASTY MINGUITO, SHANIA D. | BSN 2-B 42 2F – SICK GROWING CHILD Therapeutic & NCM: ✓ primary management – surgical ✓ first nursing responsibility is assisting in identification of anorectal malformations ✓ a newborn who does not pass stool within 24 hours after birth or has meconium that appears at a location other than the anal opening requires further assessment ✓ pre-op care: diagnostic evaluation, GI decompression, bowel preparation, IV fluids ✓ (for perineal fistula) Anoplasty is performed – involves moving the fistula opening to the center of the sphincter and enlarging the rectal opening ✓ feedings are started soon after the surgical repair ✓ breastfeeding is encouraged because it causes less constipation ✓ Cloaca (female), recto-urethral prostatic fistula (male), and vestibular fistula (female) → DESCENDING COLOSTOMY is performed, to allow fecal elimination and avoid fecal contamination ✓ PSARP – common surgical procedure for the repair of anorectal malformations 2F CONGENITAL DIAPHRAGMATIC HERNIA ALTERATIONS IN GASTROINTESTINAL FUNCTION CDH results when the diaphragm does not form completely, resulting in an opening between the thorax and the abdominal cavity. ➔ diaphragm forms at 4-8 weeks gestation ➔ BOCHDALEK HERNIA or AKA LEFT POSTEOLATERAL DEFECT (most common type of CDH) ➔ Bochdalek – intestines and other abdominal structures, such as the liver, can enter the thoracic cavity, compressing the lung ➔ lung hypoplasia, ventilation is compromised ➔ pulmonary hypertension ➔ acute RDS is present, dyspneic, cyanotic, scaphoid abdomen, impaired cardiac output, shock Therapeutic & NCM: ✓ fetal surgery ✓ proper assessment, prompt recognition of neonatal respiratory distress, cyanosis, scaphoid abdomen, mediastinal shift would alert the nurse to investigate further ✓ any infant with a scaphoid abdomen, moderate to severe respiratory distress, decreased breath sounds unilaterally, and a history of polyhydramnios should be suspected of having a CDH ✓ ventilation should not be given with bag and mask to prevent further intestinal air and subsequent respiratory compromise ✓ pre-op care involves prompt recognition, resuscitation, and stabilization of the infant, including ventilatory support, blood gas monitoring, fluid volume maintenance, and administration of IV fluids and electrolytes MINGUITO, SHANIA D. | BSN 2-B 43 2F – SICK GROWING CHILD ✓ post-op → routine obs, detect signs of RDS/fluid/electrolyte imbalances ✓ monitor mediastinal shift signs, pulmonary air leak, and infection UMBILICAL HERNIA ALTERATIONS IN GASTROINTESTINAL FUNCTION Hernia – Protrusion of a portion of an organ or organs through an abnormal opening. Umbilical Hernia – Common hernia observed in infants. Occurs when fusion of the umbilical ring is incomplete at the point where the umbilical vessels exit the abdominal wall. Incarceration – Hernia is constricted and cannot be reduced manually, is rare. (3 to 5 years) Nursing Care Management: ✓ Need reassurance that the defect usually is not harmful. ✓ Taping or strapping the abdomen to flatten the protrusion does not aid in resolution and can produce skin irritation. ✓ Observe the child for complications related to a hematoma or infection. Therapeutic & NCM: ✓ investigation of possible organic causes such as CMA, intussusception, or other GI problem ✓ PO – Lactobacillus reuteri ✓ antispasmodics ✓ antihistamines ✓ antiflatulents Areas that should be stressed include: 1. infant’s diet 2. diet of the breastfeeding mother 3. time of day when crying occurs 4. relationship of crying to feeding time 5. presence of specific family members during crying and habits of family members, such as smoking 6. activity of the mother or usual caregiver before, during, and after crying 7. characteristics of the cry (e.g., duration, intensity) 8. measures used to relieve crying and their effectiveness 9. infant’s stooling, voiding, and sleeping patterns RUMINATION COLIC (PAROXYSMAL ABDOMINAL PAIN) ALTERATIONS IN GASTROINTESTINAL FUNCTION Abdominal pain or cramping that is manifested by loud crying and drawing t he legs up to the abdomen. Star anise tea is a remedy used by some to treat colic. Numerous cases of star anise tea toxicity have been recorded in the literature. Inform parents that this remedy should not be used in infants to treat colic. 2F ALTERATIONS IN GASTROINTESTINAL FUNCTION Is a behavioral problem which causes a regurgitation of readily eaten food. Etiology: Unknown Risk Factors: - gastric distention w/ food - abdominal pressure - relaxation of lower esophageal sphincter - gastric contents regurgitated - food expelled/re-swallowed depending on social circumstances MINGUITO, SHANIA D. | BSN 2-B 44 2F – SICK GROWING CHILD Risk Assessment: - abdominal pain - indigestion - repeatedly bringing up (regurgitating food) - attempt to force back food into the oropharynx - spitting up/vomiting S/S: re-chewing of the food, repeated regurgitation, bad breath, raw & chapped lips, malnutrition, delayed growth development DT: endocrine hormone functions, test for anemia, serum electrolytes Therapeutic & NCM: ✓ Restore a nurturing environment. ✓ Provide a primary care of nursing staff to feed the child. ✓ Talking away distractions during feeding. ✓ Making feeding a more relaxing and pleasurable experience. ✓ Maintain a calm and even temperament when feeding the infant or child throughout the meal. CELIAC DISEASE ALTERATIONS IN GASTROINTESTINAL FUNCTION Permanent intestinal intolerance to dietary gluten. A protein present in wheat, barley, rye, and oats, that causes damage to the villi in the small intestine. Risk Assessment: - 1st degree relative with celiac disease Northern European background T1 DM Down Syndrome/Turner Syndrome Autoimmune Thyroid Disease microscopic colitis addison’s disease IgA deficiency S/S: abdominal bloating & pain, chronic diarrhea, vomiting, constipation, pale, foulsmelling, fatty stool, IDA, weight loss, fatigue, irritability & behavioral issues, dental enamel defects of the permanent teeth, delayed growth & puberty DT: PE, CBC, HLA Genetic Test, Endoscopy Therapeutic & NCM: ✓ gluten-free diet ✓ help the child adhere to the dietary regimen ✓ nurse must give advise to parents of the necessity of reading all label ingredients carefully to avoid hidden sources of gluten ✓ nurse can be instrumental in allowing the child to express concerns and frustration while focusing on ways in which the child can still feel normal Also known as: 2F ✓ gluten-induced enteropathy ✓ gluten-sensitive enteropathy ✓ celiac sprue MINGUITO, SHANIA D. | BSN 2-B 45 2F – SICK GROWING CHILD SHORT BOWEL SYNDROME ALTERATIONS IN GASTROINTESTINAL FUNCTION Malabsorptive disorder that occurs as a result of decreased mucosal surface area, usually because of extensive resection of the small intestine. ➔ decreased intestinal surface area for absorption of fluid, electrolytes, and nutrients ➔ need for parenteral nutrition (PN) Therapeutic & NCM: ✓ preserve as much length of bowel as possible during surgery ✓ maintain optimum nutritional status, growth, and development while intestinal adaptation occurs ✓ stimulate intestinal adaptation with enteral feeding ✓ minimize complications related to the disease process and therapy ✓ most important components of nursing care are administration and monitoring of nutritional therapy Therapeutic & NCM: ✓ Maintain hygiene of the bladder area to prevent infection and excoriation of the surrounding tissue. ✓ Adding a sterile, nonadherent, moist dressing is placed over the exposed bladder area to prevent infection and to avoid the diaper form adhering to mucosa. ✓ Inspect periodically for evidence of pressure necrosis. ✓ Apply fluid management, IV access should be applied early on. ✓ Preserve pelvic immobility. ✓ Maintain ureteric catheter patency. ✓ Avoid having the baby cry to decrease chances of abdominal distention. ✓ Maintain skin hygiene. HYPOSPADIAS ALTERATIONS IN GENITOURINARY FUNCTION Hypospadias – Urethral opening is located below the glans penis or anywhere along the ventral surface (underside) of the PENILE SHAFT. BLADDER EXSTROPHY ALTERATIONS IN GENITOURINARY FUNCTION Is a more severe defect characterized by externalization of the bladder, splaying of the urethra with failure of tubular formation. Etiology: Exstrophy results from failure of the abdominal wall and underlying structures, including the ventral wall of the bladder, to fuse in utero. As a result, the lower urinary tract is exposed and the everted bladder appears bright red through the abdominal opening. 2F S/S: bladder is visible, smaller-capacity bladder, lower-than-usual belly button, anus is lower than usual, separated pelvic bones, undescended testicles Chordee – Ventral curvature of the penis, results from the replacement of normal skin with a fibrous band of tissue and usually accompanies more sever forms of hypospadias. TAKE NOTE: REINFORCEMENT Is a birth defect in which the opening of the urethra is not located at the tip of the penis. MINGUITO, SHANIA D. | BSN 2-B 46