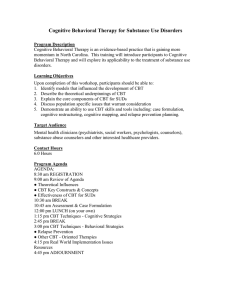
1 Cognitive Behavioral Therapy and Depression Jeremy Arnold Department of Counseling and Pastoral Care, Asbury Theological Seminary CO740: Counseling Theories and Techniques Dr. Marcus Kilian April 21, 2023 2 Abstract The increasing numbers of people struggling with depression worldwide makes it crucial that Mental Health Providers are equipped with tools to provide real relief to those seeking help. The current landscape is of Mental Health is impacted by the COVID19 pandemic as well as a growing trend of non-traditional forms of therapy. Cognitive Behavior Therapy was created to deal with depression in the 1960s. This paper will analyze the CBT approach to depression considering today’s challenges. The research done here confirms that Cognitive Behavior Therapy continues to be an effective treatment of depression in our context today. 3 Cognitive Behavioral Therapy and Depression General overview of the approach The World Health Organization’s (WHO) latest exhaustive worldwide study reported that 322 million people were living with Depression in 2015, making it among the most common problems experienced globally (World Health Organization, 2017). The high prevalence of depression also makes it the highest cause of disability worldwide (Ezawa, 2021). Not only is Depression extremely common, but its prevalence is also rising. Research shows the rates of depression increased from 2005-2015, specifically in younger populations (APA, 2022). To make matters worse, the WHO released a scientific brief in March of 2022 revealing that the COVID19 pandemic led to a massive 27.6% increase in cases of Major Depressive Disorder (MDO) (WHO, 2022). The prevalence and growing concern make it crucial that all mental health practitioners have effective strategies to help clients struggling with depression. Cognitive Behavioral Therapy (CBT) can be used to treat many different disorders, but it is especially effective in treating depression. While there are different diagnoses within the general term “depression”, each of them shares the common trait of an individual having negative thoughts and feelings about themselves or the situation they find themselves in. CBT provides a way to focus on these cognitions and gives the depressed person tools to change. Starting with Assessment and Case conceptualization, the therapist evaluates the client’s suitability for CBT (Wright et al., 2017). After forming a hypothesis, the therapist begins to introduce basic CBT concepts outlined in detail later in this paper. Using Cognitive and Behavioral techniques the therapist and client work together over the course of treatment to change the negative thoughts, and problematic behaviors contributing to the depression. 4 Understandings of clinical problems & health Within the Depressive Disorders, there are six different specified diagnosis, and many of them can also have modifiers to indicate the more specific symptoms being experienced (APA, 2022). Therefore, each client that walks into a mental health clinicians office with “depression” must be assessed. It cannot be assumed that all clients with depressive symptoms have the same issue that can be treated with the exact same techniques as if they were all the same. A 2021 study done in England showed that various subtypes of depression respond differently to CBT (Simmonds‐Buckley, 2021). While CBT was shown to be effective, it was more effective in patients whose symptoms fell in a category they labelled the cognitive/affective subtype. Patients whose symptoms were also somatic experienced some, but less relief from symptoms. A contributing factor was that somatic patients also showed a higher probability of dropping out of the treatment. For these reasons, assessment of patient’s symptoms and compatibility with CBT is essential. Cognitive Behavior Therapy is based on the belief that emotions and behaviors are strongly influenced by cognitions, and that the ways a person behaves can reciprocally effect patterns of thought (Wright et al., 2017). In treating depression, CBT uses this influencing factor to target the cognitions and behaviors to decrease the depressive symptoms. This process of the interaction between cognitions, behaviors, and emotions is depicted in the figure 1 below: Figure 1. Basic CBT Model 5 CBT recognizes that the cognitive process is subject to making mistakes, called cognitive distortions (Beck et al., 1979). When a cognitive distortion enters the paradigm, it follows that the emotions and behaviors of the person will be impacted by the distorted thinking. Depressed persons experience the world around them in ways that make it difficult to function. A helpful way of understanding this is through the concept of depressed persons attribution style (Wright et al., 2017). This involves three distorted domains. First, the depressed person views problems internally instead of externally. Because of this, a depressed person puts blame on themselves even when there is no evidence that a problem is their fault. Second, a depressed person views problems as global rather than specific. This contributes to them believing problems are affecting things way beyond their actual scope. And third, depressed persons view problems as fixed rather than changeable. When a depressed person sees a problem, they view it as something they will always have to deal with without hope of change. Counselor’s stance/role While CBT is known for its techniques and homework exercises, another highly important component is the therapeutic relationship. From its beginnings, Beck’s Cognitive Therapy (CT) acknowledged the importance of the collaborative therapeutic relationship (Beck et al., 1979). In contrast with Albert Ellis’ more direct and brash style, Beck warned that the techniques in CT could end up being administered in a robotic sort of way where the counselor views the client like a computer. There are some important characteristics for the counselor to bring to the table to establish this healthy therapeutic relationship. From Beck’s perspective, the three common traits that Cognitive counselors needed to be successful were “warmth, accurate empathy, and genuineness” (Beck et al., 1979, p. 45). Others have added positive regard to this list, borrowing from Carl Rogers ( Wright et al., 2017). The term Collaborative Empiricism (CE) is often used to 6 describe the way the counselor and client work together throughout treatment (Wright et al., 2017). Within this counselor and client team, the client comes with the raw data of their thoughts, feelings and desires as the counselor helps the client learn what data is important to collect and what to do with it throughout treatment (Beck et al., 1979). While positive regard has been borrowed from Carl Rogers, CBT departs from his PersonCentered Theory because the counselor will often take on the role of Psychoeducator (Wright et al., 2017). CBT requires the teaching of various models and techniques the client will be using outside of the therapy sessions making it important for counselors to be adept in the role of teacher. Major components of treatment Cognitive Behavior Therapy is a short term, problem-focused approach (Wright et al., 2017). Moderately depressed patients typically receive treatment for 5-20 sessions. While CBT counselor pay attention to the history of their client in forming their case conceptualization, the major focus is on the problem as it is being experienced in the present. Assessing a client and forming a conceptualization of their case is a major component of Cognitive Behavior Therapy. The initial assessment takes the form of an interview utilizing Socratic questioning to help gather the client’s relevant information (Wright et al., 2017). Here the counselor is looking first for the client’s level of compatibility with CBT. The counselor evaluates several things in determining the client’s suitability for CBT. This can be organized into seven separate dimensions. These dimensions evaluate the severity of the problem, the client’s optimism about success, willingness to participate in the change process, the client’s view of the CBT as negative or positive, the client’s aptitude in evaluating their cognitions and emotions, ability to be in relationship with the counselor, and the client’s ability to focus in a problem-oriented way. 7 Once a counselor has determined a client is suitable for CBT, they begin to form a case conceptualization (Wright et al., 2017). The case conceptualization helps the counselor to form a hypothesis about what is causing the client’s depressive symptoms. This hypothesis becomes a working hypothesis as various CBT interventions are employed. The hypothesis can change as the therapy progresses. Another major component of Cognitive Behavior Therapy with any client, including those presenting for depression, is building a healthy therapeutic alliance. Basic helping skills should be utilized in gathering the client’s initial story and forming a case conceptualization, but these skills also help foster the relationship as it is beginning. Attending to this relationship throughout the counseling process is an important component that helps the other components of therapy produce successful outcomes (Wright et al., 2017). While some therapy approaches involve the counselor following the client’s lead wherever they take the session offering little direction, CBT uses collaborative structuring methods to increase the efficiency of the session (Wright et al., 2017). Each session involves setting an agenda, often with the help of the client, and the counselor works to keep the session on the agreed upon items. This structure is not without flexibility if something comes up in discussion that the counselor sees as important enough to deviate from the agenda. Session progression will be discussed further below. There is an abundance of techniques the client will be invited to participate in throughout the therapy, and it is important for the client to understand what they are, and why they are helpful. Homework, or take-home exercises are a staple of CBT and cannot be effective if they are not fully understood. Therefore, psychoeducation is an important component of CBT (Wright 8 et al., 2017). Through psychoeducation clients are taught the main concepts of CBT, and exercises to put them into practice outside of the session. Perhaps the most unique component of CBT is the concept of Cognitive Restructuring. Cognitive Restructuring is done through various techniques to help clients uncover maladaptive thoughts (Wright et al., 2017). These can be automatic thoughts, core beliefs, or schemas. Often take-home exercises are utilized to help the client do much of this work outside of the therapy sessions. Some of these specific techniques will be discussed further below. CBT grew out of strict Behavior Therapy which focused solely on behavioral interventions to address the client’s problem. While CBT includes cognitive techniques, it still utilizes behavioral methods. For depression, the best place to begin is with behavioral activation (described more fully below) (Wright et al., 2017). Beginning with this behavioral method helps the client to start with something small to see change in their life. Experiencing a successful change can increase the client’s belief that change is possible and provide motivation to participate more fully in larger goals. Other behavioral methods such as Graded Task Assignment and Behavioral Rehearsal can also be helpful when working with depressed clients. Finally, the last major component of CBT is the idea that clients learn skills that prevent them from relapsing back into their symptoms (Wright et al., 2017). CBT does not only help clients solve their problems, but it also gives them the tools to solve their future problems as well. Typical progression of sessions As mentioned briefly above, the structured nature of CBT is an important component. While the sessions towards the end of treatment can alter slightly, and this general template varies from counselor to counselor it can serve as a typical progression of a session (Wright et al., 2017): 9 1. Greeting: This provides space for the counselor and the client to engage each other in small talk and acclimate themselves to the space. 2. Assess symptoms: Here the counselor is looking for signs of the severity of the client’s depression. Is he or she suicidal? Do they seem to be better or worse than last week? 3. Collaboratively set the agenda for today’s session: The counselor and client will work together to set the agenda for the work they will do. The counselor will come into the session with ideas in mind, but should include the client when possible, in setting the agenda. This will reinforce the collaborative relationship. 4. If take home exercises have already been introduced, it is reviewed. Was the exercise completed? How was the experience for the client? Did they experience problems? If so and they overcame them, how? If not, how might they have overcome them? 5. Do in session CBT work on issues from the agenda. For a depressed person who is overwhelmed by the thought of calling a friend, this might include something like role play to help them feel what it is like to make the call. 6. Psychoeducation: Here the counselor teaches a CBT skill related to the depression. Early in the treatment of depression introducing the concept of automatic thoughts and their relationship with emotions and behaviors is common. The diagram in figure 1 above can be used as a template for adding specific thoughts and behaviors helping the client to see the connection between their own thoughts and behaviors. 7. Create a take home exercise: The counselor may have an exercise in mind, but it is often helpful for the counselor and client to work together to create a meaningful exercise for the client to complete during the week. As treatment progresses, clients should be more involved in creating the exercises (Beck, 1979). Often the counselor 10 will have a technique in mind but invite the client into the process to apply it to their specific context. In the example previously used of calling a friend, the counselor could have behavioral activation in mind and simply ask, “what is one thing you can do this week?” If the client comes up with calling a friend, it is then narrowed down to a specific friend, at a specific time. Socratic questioning is used to help the think through potential barriers and solutions. 8. Review and Feedback: A summary is provided giving the counselor an opportunity to make sure the client understands the work they have done together and assess how the client feels the session has gone. Towards the middle phase of treatment, there will likely be less psychoeducation and towards the end of treatment the counselor will begin to introduce relapse prevent techniques to prepare for the termination of treatment. Techniques and their therapeutic purposes Cognitive Behavior therapists working with depressed patients draw from numerous techniques each with specific purposes. More could be mentioned but the ones focused on here will be Socratic Questioning, Behavioral Activation, Examining the Evidence, Thought Change Records, and Coping Cards. Socratic Questioning is a staple of CBT and is utilized throughout the therapeutic process. It is a form of questioning the client in line with the commitment to collaborative empiricism (Wright et al., 2017). The goal is to help the client uncover their unhelpful thought patterns. A form of Socratic questioning that is often used in CBT is the Downward Arrow Technique which uses a series of (often repetitive) Socratic questions to help the client dig deeper to uncover deeper levels of thought patterns. A 2022 study evaluated the use of Socratic Questioning on depressed 11 clients receiving CBT (Vittorio, 2022). Previously, it was theorized that Socratic Questioning was a productive technique, but very little research had been done to support this assumption. In studying 123 clients diagnosed with Major Depressive Disorder, they concluded “Our findings support the theorized effects of Socratic questioning as a procedure which achieves symptom reductions through the promotion of cognitive change in CBT” (Vittorio, 2022). Depressed clients often have a difficult time engaging in activities that would lift their mood. This can result in a cycle of inactivity producing more and more depressive symptoms (Wright et al., 2017). For this reason, Behavioral Activation is often the first technique employed in CBT with depressed clients. The counselor and client work together (reinforcing collaborative empiricism) to identify 1 or 2 activities that would produce a better mood in the client. The counselor, still using Socratic questioning, helps the client to narrow down activities to something small that is very achievable. Then they work together to create a plan and evaluate what barriers might exist to the success of completing the plan. Other techniques like role play can help assist in the preparation to complete the activity. Research supports the use of Behavioral Activation. A network meta-analysis in 2021 evaluated the effectiveness of Behavioral Activation, Cognitive Restructuring, and full CBT (Ciharova, 2021). The results show that Behavioral Activation alone is effective even without other CBT interventions. As discussed above, a major component of CBT is modifying negative thought patterns, whether they are automatic thoughts, core beliefs, or schemas. CBT employs a number of techniques aimed to help the client modify their unhelpful thought patterns. Examining the Evidence is a technique used to help clients modify identified automatic negative thoughts (Wright et al., 2017). Once an automatic negative thought, or unhelpful core belief is identified, Examining the Evidence is the process of rationally thinking through the evidence that supports 12 the thought and the evidence that contradicts the thought. The counselor and client work together to create lists for each side to determine if there is enough evidence to support believing the thought. This process can be done in an organized way through a worksheet, or in a more informal way without writing the lists down. Another technique used to help clients modify automatic thoughts is a Thought Change Record. Beck et al. created a 5-column chart to help clients to record a situation, their emotional reaction and automatic thoughts related to that situation, a more rational response to the situation, and the emotional and behavioral outcome (Beck, 1979). This is a powerful self-monitoring take home exercise that helps the depressed person to capture and analyze the validity of their automatic thoughts (Wright et al., 2017). It brings together many of the other cognitive techniques, like examining the evidence and identifying cognitive distortions that would have been previously taught to the client. A staple of CBT is giving clients tools to be their own therapists outside of the sessions and after the termination of treatment. A helpful technique in accomplishing this is the use of Coping Cards (Wright et al., 2017). The skills learned from the Thought Change Record can be applied to assist the client to react differently in future situations. In session, the counselor, and the client work together to think of rational responses to future events and write them down on a card, or a note app on their smartphone. The client then keeps these cards with them when the situation may occur and refers to the card when they start having negative automatic thoughts. The card will help them to instead evaluate the situation with realistic rational thoughts. There are numerous other techniques that also assist in the treatment of depression, but these are some of the most effective tools and staples of CBT. 13 Relevant Christian insights and implications During the sermon on the mount, Jesus makes it clear that human sinfulness is not just about behavior. He says, “You have heard that it was said to the people long ago, ‘You shall not murder, and anyone who murders will be subject to judgment.’ But I tell you that anyone who is angry with a brother or sister will be subject to judgment. Again, anyone who says to a brother or sister, ‘Raca,’ is answerable to the court. And anyone who says, ‘You fool!’ will be in danger of the fire of hell” (NIV, Matthew 5:21-22). After he speaks about the connection between murder and anger he goes on to make the same connection between adultery and lust. In both cases Jesus is saying the cognitions of humans are subject to judgment as well as their behaviors. CBT works out of a model that assumes cognitions, behaviors, and emotions are all intertwined. A model that provides avenues for change in our cognitions certainly is aligned with this aspect of the Christian faith. The Apostle Paul writes, “Do not conform to the pattern of this world, but be transformed by the renewing of your mind” (Romans 12:2). Paul is calling for real change in the lives of the Roman Christians. In this sentence he uses imperative verb forms that communicate the command of an authority figure. This type of change is not merely a suggestion, it is a requirement. The mode through which this change should occur is through the “renewing of your mind”. At first glance this seems to connect to the work done in CBT. CBT therapists seek to change the way people’s minds are operating, so many Christians have pointed to it as a form of therapy to help deal with sin. This connection between CBT and Romans 12:2 is valid, but with an important caveat. Paul uses the verb μεταμορφοῦσθε in a passive form which translates into English as “be transformed”. The more active form of μεταμορφόω would have been translated as “I transform”, or in the imperative, “transform yourself”. But Paul clearly uses the passive form of the verb 14 meaning the transformation is coming from somewhere outside of the person being transformed. While not explicitly stated, it is safe to conclude from the context that Paul is implying God is the one who does the transforming of Christians. God alone is the one who brings about the type of change Paul is talking about in the phrase “renewing of your mind”. So, what does this mean for the Christian CBT therapist? It makes doing CBT even more meaningful. In creation God invites Adam to name the animals he has created (Gen. 2:19). From the beginning God has invited humans into his creative activity. The CBT therapist operating out of a Christian perspective can enter the creative activity of God as God renews the minds of his people. The connection between CBT and faith also makes it possible for religious practices to be integrated into the therapy with the consent of the client (Tan, 2007). Christian CBT practices such as prayer, inner healing prayer, and the use of scripture can be extremely effective techniques added to traditional CBT. Empirical support for the effectiveness of the approach It was mentioned in the introduction that depression is the largest reason for disability around the world. For CBT to be considered effective, it should not only be effective at decreasing symptoms, but it should also be helping people get back to being able to function within society. In 2021 a study was done to evaluate the effectiveness of CBT in increasing job rates for those who were not working due to depression, and for increasing productivity at work for those who were already working but were experiencing depression. The study concluded that CBT proved to be effective in both getting people back to work, and increasing productivity (Ezawa, 2021). 15 Another project evaluated the levels of cognitive change in depressed clients by looking at two types of affect: negative affect and positive affect (Whelen, 2021). They concluded that the cognitive change was more pronounced in the reduction of negative affect, but they also recorded a significant improvement in positive affect as well. It is also important to note that CBT was proven to be an effective tool against depression during the COVID19 pandemic (Zamiri-Miandoab, 2022). A network meta-analysis pulled together research from 14 different studies to determine the effectiveness of CBT on anxiety and depression during the pandemic. They study concluded, “Based on the overall results of metaanalysis, CBT had a significant effect on reducing anxiety and depression.” Finally, another area it is important to understand the effectiveness of CBT is in the growing demand for avenues for therapy other than face to face, in person counseling. The field of counseling exists in a world that is increasingly operating in digital spaces and effective means of counseling outside of the traditional form is crucial moving forward. Another meta-analysis was done in 2022 to evaluate the effectiveness of in-person and virtual CBT with depressed clients (Charron, 2022). Their hypothesis was that virtual CBT is equally as effective as in person CBT. The study confirmed their hypothesis. Not only is CBT empirically proven to be an effective form of treatment, but it has also proven it was effective during a global crisis, and it is effective through various digital modes of counselling. This is important moving forward. CBT has proven it can be adaptable to changing circumstances. A personal critique of the approach Personally, I believe Cognitive Behavioral Therapy is an excellent model to work from when doing therapy with depressed clients. I took this class because when I first learned about 16 CBT in the basic theories class, it seemed like a great tool, specifically for treating depression and anxiety. I plan to use it as a go to model when working with depressed clients. CBT leaves open the door to view people through a Christian lens. Even though it grew out of the behavioral assumptions of naturalism, it now has plenty of space for Christian worldviews. Another significant draw to CBT is that it is short-term. People living in poverty are at a higher risk of depression (WHO, 2017). The short-term approach to helping people translates to it being more accessible to those without means. One of the biggest critiques I have of some of the early theories of counseling is the extreme length, making it only accessible to the wealthy elite. However, even though I have yet to begin practicing in the field, I can see the temptation for CBT to become a mechanical approach to counseling. It is important for clinicians to remember they are not treating a disorder; they are treating a person experiencing a problem. A criticism I have recently come to have about CBT comes from my being exposed to the Internal Family Systems model which views people in terms of their “parts”. I worry that work could be done in session to help a client when their “self” is in charge, but when their “anxious part” or their “depressed part” takes over I worry that those parts will not be as accepting of the CBT interventions. Overall, the overwhelming empirical support for CBT far outweighs my concerns. 17 References American Psychiatric Association. (2022). Depressive Disorders. In Diagnostic and statistical manual of mental disorders (5th ed., text rev.). Beck, A. T., Rush, A. J., Shaw, B. F., Emery, G. (1979). Cognitive Therapy of Depression. The Guilford Press Charron, Carly M., Gorey, Kevin M. (2022). Virtual versus Face-to-Face Cognitive Behavioral Treatment of Depression: Meta-Analytic Test of a Noninferiority Hypothesis and Men’s Mental Health Inequities Depression Research and Treatment 2022 https://doi.org/10.1155/2022/2972219 Ciharova, M. et al. (2021). Cognitive restructuring, behavioral activation and cognitivebehavioral therapy in the treatment of adult depression: A network meta-analysis. Journal of Consulting and Clinical Psychology, 89(6) 563–574. DOI 10.1037/ccp0000654 Ezawa, I. D., Bartels, G. C., Strunk, D. R. (2021) Getting down to business: an examination of occupational outcomes in cognitive behavioral therapy for depression. Cognitive Behaviour Therapy, 50(6) 479–491. DOI 10.1080/16506073.2021.1875039 Simmonds, B. M., Catarino, A., Delgadillo, J. (2021). Depression subtypes and their response to cognitive behavioral therapy: A latent transition analysis. Depression & Anxiety, 38(9) 907–916. DOI 10.1002/da.23161 Tan, S. (2007). Use of Prayer and Scripture in Cognitive-Behavioral Therapy. Journal of Psychology and Christianity, 26(2), 101-111. Vittorio, Lisa N., Murphy, Samuel T., Braun, Justin D., Strunk, D.R. (2022). Using Socratic Questioning to promote cognitive change and achieve depressive symptom reduction: 18 Evidence of cognitive change as a mediator, Behaviour Research and Therapy,150 https://doi.org/10.1016/j.brat.2022.104035 Whelen, M. L., Strunk, D. R. (2021). Does cognitive behavioral therapy for depression target positive affect? Examining affect and cognitive change session-to-session. Journal of Consulting and Clinical Psychology, 89(9) 742–750. DOI 10.1037/ccp0000679 World Health Organization. (2017). Depression and Other Common Mental Disorders, Global Health Estimates https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSDMER-2017.2-eng.pdf World Health Organization (2022, March 2). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. The World Health Organization https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-inprevalence-of-anxiety-and-depression-worldwide Wright, J. H., Brown, G. K., Thase, M. E., Basco, M. R. (2017). Learning Cognitive-Behavior Therapy: An Illustrated Guide. American Psychological Association Zamiri-Miandoab, N., Hassanzade, R. & Mirghafourvand, M. (2022). The effect of cognitive behavior therapy on anxiety and depression during COVID-19 pandemic: a systematic review and meta-analysis. Annals of General Psychology, 21(40) https://doi.org/10.1186/s12991-022-00417-y