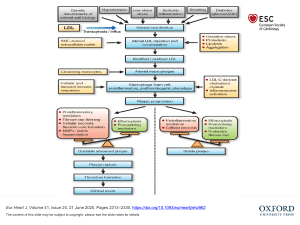
VIEWPOINT European Heart Journal (2024) 00, 1–3 https://doi.org/10.1093/eurheartj/ehae110 Interventional cardiology Emanuele Barbato 1 *, Margaret McEntegart2, and Tommaso Gori 3 1 Department of Clinical and Molecular Medicine, Sapienza University, Piazzale Aldo Moro 5, 00185 Rome, Italy; 2Department of Cardiology, Columbia University Medical Center, New York, NY, USA; and 3Kardiologie I, Center for Cardiology, University Medical Centre Mainz and DZHK Standort Rhein-Main, Mainz, Germany Graphical Abstract Ten interventional cardiology papers from 2023 that may change our practice Coronary artery disease ORBITA-2 PCI versus placebo improves outcome FIRE Physiology-guided PCI in older patients improves outcomes ILUMIEN-IV OCT reduces stent thrombosis but does not change other outcomes Resistant hypertension Peripheral interventions PARTNER-3 TAVI vs SAVR in intermediate risk SIMPLICITY-3 Catheter-based renal artery denervation more Meta-analysis DCBs associated with higher patency rate than POBA outcomes at 5 years sham at 3 years Cardiogenic shock Valve disease ECLS-SHOCK Increased bleeding and peripheral complications TRILUMINATE Percutaneous therapy of regurgitation mproves Qol OCTOBER OCT improves outcome in bifurcation lesions DAPT de-escalation Reduces bleeding and ischaemic events Our selected papers. PCI, percutaneous coronary intervention; OCT, optical coherence tomography; DAPT, dual anti-platelet therapy; TAVI, transcatheter aortic valve implantation; SAVR, surgical aortic valve replacement; DCB, drug-coated balloon; POBA, plain old balloon angioplasty; Qol, quality of life. * Corresponding author. Email: emanuele.barbato@uniroma1.it © The Author(s) 2024. Published by Oxford University Press on behalf of the European Society of Cardiology. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehae110/7619355 by guest on 06 March 2024 The year in cardiovascular medicine 2023: the top 10 papers in interventional cardiology 2 The year 2023 brought tremendous innovation in interventional cardiovascular medicine, with numerous publications from long-awaited trials that were designed to provide definitive answers regarding the role of physiology, imaging, novel devices, and novel applications of structural interventions. While the 10 papers presented below admittedly represent an arbitrary choice (Graphical Abstract), there are thousands of other ones equally worthy of mention. setting of acute coronary syndromes, but the concern remains regarding a possible increase in ischaemic events. To address this concern, Kang et al. performed a patient-level meta-analysis of four trials (TROPICAL-ACS, POPular Genetics, HOST-REDUCE-POLYTECHACS, and TALOS-AMI trials) including 10 133 acute coronary syndrome patients.5 De-escalation was found to be superior for both ischaemic [HR 0.76 (95% CI 0.60–0.97), P = .029] and bleeding events [HR = 0.70 (95% CI 0.61–0.81), P < .001]. Cardiogenic shock The primary purpose of percutaneous coronary intervention itself was under investigation in the most recently published trial on this list, ORBITA-2, presented at the 2023 American Heart Association Scientific Sessions.1 In this randomized controlled trial, specifically designed to isolate the treatment effects in patients with stable angina and objective evidence of ischemia not taking anti-anginal medication, interventional therapy significantly reduced the mean angina symptom score compared to a sham placebo procedure [2.9 vs. 5.6; odds ratio 2.21, 95% confidence interval (CI) 1.41–3.47, P < .001]. While coronary interventions have been performed for almost five decades, this trial was the first to formally demonstrate beyond any doubt the effectiveness of PCI in reducing anginal frequency and exercise times. Cardiovascular emergencies are a particularly complex setting for research, with evidence lacking in many aspects of patient care. In the ECLS-SHOCK randomized controlled trial, Thiele et al. assigned 420 patients in cardiogenic shock undergoing early revascularization with or without extracorporeal life support. They reported no impact on 30-day mortality [relative risk 0.98 (5% CI 0.80–1.19); P = .81], but increased bleeding and peripheral complications.6 While this is consistent with previous trials showing no benefit of systematic use of intra-aortic balloon pumps and microaxial devices, the use of these costly devices in selected cases of advanced instability can hardly be investigated. Coronary physiology and imaging The treatment of valvular heart diseases is becoming the domain of interventionalists. Two of the many papers published in 2023 demonstrate how these indications are continuously expanding. Mack et al. reported the 5-year outcomes of the PARTNER-3 trial, randomizing patients with severe, symptomatic aortic stenosis, and low surgical risk to undergo either transcatheter aortic valve implantation or surgery. Rates of both clinical co-primary endpoints, and parameters of hemodynamic valve performance, were essentially similar between groups.7 Nonetheless, the most innovative field in percutaneous valve intervention consists in the treatment of tricuspid valve regurgitation. Severe tricuspid regurgitation is under-treated and associated with an under-recognized rate of morbidity and poor quality of life. In addition, surgical correction is complex and associated with an elevated rate of complications. While showing effectivity in reducing tricuspid regurgitation, in the TRILUMINATE randomized controlled trial, no difference between transcatheter repair and medical therapy was observed in any of the outcomes, including the incidence of death or tricuspid valve surgery and the rate of hospitalization for heart failure except for an improvement in patient-reported quality of life (Kansas City Cardiomyopathy Questionnaire scores, 12.3 ± 1.8 vs. 0.6 ± 1.8 points, P < .001).8 The second paper of this list reports on the results of the FIRE randomized controlled trial presented at the 2023 European Society of Cardiology Congress.2 The incidence of cardiovascular diseases increases with age, as does the prevalence of comorbidities and frailty in patients with myocardial infarction. Despite that, older patients are poorly represented in clinical trials, and clinical decisions regarding complete revascularization balance an increased risk of complications with technical challenges. In this context, Biscaglia et al. enrolled 1445 patients with a median age of 80 (interquartile range 77–84) years presenting with an acute myocardial infarction and multivessel disease. After successful intervention of the culprit lesion, patients were randomized to physiology-guided complete revascularization or no further intervention. During one year follow-up, the composite endpoint (death, myocardial infarction, stroke, or any revascularization) occurred significantly less frequently in the physiology-guided group [hazard ratio (HR) 0.73, 95% CI 0.57–0.93; P = .01], demonstrating a benefit of physiology-guided complete revascularization also in the elderly. Following on from the publications and growing interest in intracoronary imaging in 2022, two eagerly anticipated randomized controlled trials, ILUMIEN IV and OCTOBER, were presented at the 2023 European Society of Cardiology Congress.3,4 While ILUMIEN IV, enrolling patients at higher risk for ischemic events and/or with complex lesions, showed no difference in target lesion failure at 2-year follow-up between optical coherence tomography-guided and angiography-guided interventions despite a larger minimum stent area and a reduced incidence of stent thrombosis in the imaging arm,3 OCTOBER, which specifically focused on bifurcation lesions, reported a significant reduction in major adverse events at 2 years [10% vs. 14%; HR 0.70 (95% CI 0.50–0.98), P = .035] with imaging-guided.4 Dual-antiplatelet therapy De-escalation of dual-antiplatelet therapy has been established itself as a strategy to reduce bleeding risk after coronary interventions in the Structural heart disease Peripheral and hypertension intervention The last two papers selected deal with the expanding field of percutaneous intervention of peripheral artery disease and arterial hypertension. The burden of peripheral artery disease is increasing, and optimal endovascular management remains under-investigated. In a meta-analysis of 51 randomized controlled trials and 8430 patients/lesions, drugcoated balloons demonstrated a higher likelihood of long-term primary patency when used in femoropopliteal disease [odds ratio 2.47 (95% CI 1.93–3.16)] compared with balloon angioplasty. Interestingly, unlike in Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehae110/7619355 by guest on 06 March 2024 Percutaneous coronary intervention Viewpoint 3 Viewpoint Conclusions There were several important publications this year in interventional cardiology, all of which have a direct clinical impact. The selection above, admittedly arbitrary, was drawn by the interventional cardiology editorial team of the Journal among the most quoted papers of the year to reflect the multidisciplinarity of our environment. While there has been confirmation of the treatment effect of coronary interventions, the benefit of imaging and physiology, antiplatelet de-escalation, drugcoated balloon for peripheral disease, and the durability of valve interventions and renal denervation, they also highlight the need for future trials further exploring therapeutic strategies in cardiogenic shock and non-aortic valve interventions. Declarations Disclosure of Interest T.G. has received speaker´s honoraria from Astra Zeneca, Abbott Vascular, Neovasc/Shockwave, Bayer, Novartis, BMS, Insightful/ Lifetech and research funding from Abbott Vascular and Neovasc/ Shockwave. M.M. has received speaker´s honoraria or consulting fees from Shockwave Medical, Teleflex, Boston Scientific, Biosensors, and research funding from Boston Sci. E.B. has received research funding from Insightful Lifetech, Abbott Vascular, and Boston Sci. All are not related to the present work. References 1. Rajkumar CA, Foley MJ, Ahmed-Jushuf F, Nowbar AN, Simader FA, Davies JR, et al. A placebo-controlled trial of percutaneous coronary intervention for stable angina. N Engl J Med 2023;389:2319–30. https://doi.org/10.1056/NEJMoa2310610 2. Biscaglia S, Guiducci V, Escaned J, Moreno R, Lanzilotti V, Santarelli A, et al. Complete or culprit-only PCI in older patients with myocardial infarction. N Engl J Med 2023;389: 889–98. https://doi.org/10.1056/NEJMoa2300468 3. Ali ZA, Landmesser U, Maehara A, Matsumura M, Shlofmitz RA, Guagliumi G, et al. Optical coherence tomography-guided versus angiography-guided PCI. N Engl J Med 2023;389:1466–76. https://doi.org/10.1056/NEJMoa2305861 4. Holm NR, Andreasen LN, Neghabat O, Laanmets P, Kumsars I, Bennett J, et al. OCT or angiography guidance for PCI in complex bifurcation lesions. N Engl J Med 2023;389: 1477–87. https://doi.org/10.1056/NEJMoa2307770 5. Kang J, Rizas KD, Park KW, Chung J, van den Broek W, Claassens DMF, et al. Dual antiplatelet therapy de-escalation in acute coronary syndrome: an individual patient meta-analysis. Eur Heart J 2023;44:1360–70. https://doi.org/10.1093/eurheartj/ehac829 6. Thiele H, Zeymer U, Akin I, Behnes M, Rassaf T, Mahabadi AA, et al. Extracorporeal life support in infarct-related cardiogenic shock. N Engl J Med 2023;389:1286–97. https:// doi.org/10.1056/NEJMoa2307227 7. Mack MJ, Leon MB, Thourani VH, Pibarot P, Hahn RT, Genereux P, et al. Transcatheter aortic-valve replacement in low-risk patients at five years. N Engl J Med 2023;389: 1949–60. https://doi.org/10.1056/NEJMoa2307447 8. Sorajja P, Whisenant B, Hamid N, Naik H, Makkar R, Tadros P, et al. Transcatheter repair for patients with tricuspid regurgitation. N Engl J Med 2023;388:1833–42. https:// doi.org/10.1056/NEJMoa2300525 9. Koeckerling D, Raguindin PF, Kastrati L, Bernhard S, Barker Jo, Quiroga Centeno AC, et al. Endovascular revascularization strategies for aortoiliac and femoropopliteal artery disease: a meta-analysis. Eur Heart J 2023;44:935–50. https://doi.org/10.1093/eurheartj/ ehac722 10. Bhatt DL, Vaduganathan M, Kandzari DE, Leon MB, Rocha-Singh K, Townsend RR, et al. Long-term outcomes after catheter-based renal artery denervation for resistant hypertension: final follow-up of the randomised SYMPLICITY HTN-3 trial. Lancet 2022;400: 1405–16. https://doi.org/10.1016/S0140-6736(22)01787-1 Downloaded from https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehae110/7619355 by guest on 06 March 2024 coronary circulation, mid-term patency rates were similar for bare metal and drug eluting stents.9 Finally, Bhatt et al. reported the long-term outcomes after catheterbased renal artery denervation for resistant hypertension. Of the original 535 patients in the Simplicity-3 randomized controlled trial, 36-month follow-up data were available for 219 patients in the denervation group and 99 patients in the sham group (of whom 63 crossed over to denervation). The change in the office and ambulatory systolic blood pressure was significantly larger in the renal artery denervation group than the sham control group [adjusted treatment difference −22.1 (95% CI −27.2, −17.0) mmHg; P ≤ .0001].10