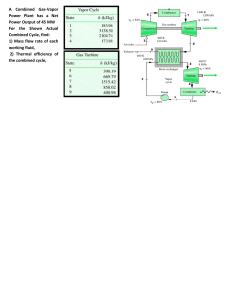
Algorithms for IV fluid therapy in adults Algorithm 1: Assessment Using an ABCDE (Airway, Breathing, Circulation, Disability, Exposure) approach, assess whether the patient is hypovolaemic and needs fluid resuscitation Assess volume status taking into account clinical examination, trends and context. Indicators that a patient may need fluid resuscitation include: systolic BP <100mmHg; heart rate >90bpm; capillary refill >2s or peripheries cold to touch; respiratory rate >20 breaths per min; NEWS ≥5; 45o passive leg raising suggests fluid responsiveness. Yes No Algorithm 2: Fluid Resuscitation Initiate treatment Identify cause of deficit and respond. Give a fluid bolus of 500 ml of crystalloid (containing sodium in the range of 130–154 mmol/l) over less than 15 minutes. Assess the patient’s likely fluid and electrolyte needs History: previous limited intake, thirst, abnormal losses, comorbidities. Clinical examination: pulse, BP, capillary refill, JVP, oedema (peripheral/pulmonary), postural hypotension. Clinical monitoring: NEWS, fluid balance charts, weight. Laboratory assessments: FBC, urea, creatinine and electrolytes. Yes Can the patient meet their fluid and/or electrolyte needs orally or enterally? Ensure nutrition and fluid needs are met Also see Nutrition support in adults (NICE clinical guideline 32). No Reassess the patient using the ABCDE approach Does the patient still need fluid resuscitation? Seek expert help if unsure Yes Does the patient have complex fluid or electrolyte replacement or abnormal distribution issues? Look for existing deficits or excesses, ongoing abnormal losses, abnormal distribution or other complex issues. No No Does the patient have signs of shock? Yes Yes >2000 ml given? Yes Algorithm 3: Routine Maintenance Algorithm 4: Replacement and Redistribution Existing fluid or electrolyte deficits or excesses Check for: dehydration fluid overload hyperkalaemia/ hypokalaemia Estimate deficits or excesses. No Seek expert help Give maintenance IV fluids Normal daily fluid and electrolyte requirements: 25–30 ml/kg/d water 1 mmol/kg/day sodium, potassium*, chloride 50–100 g/day glucose (e.g. glucose 5% contains 5 g/100ml). No Give a further fluid bolus of 250–500 ml of crystalloid Reassess and monitor the patient Stop IV fluids when no longer needed. Nasogastric fluids or enteral feeding are preferable when maintenance needs are more than 3 days. Ongoing abnormal fluid or electrolyte losses Redistribution and other complex issues Check ongoing losses and estimate amounts. Check for: vomiting and NG tube loss biliary drainage loss high/low volume ileal stoma loss diarrhoea/excess colostomy loss ongoing blood loss, e.g. melaena sweating/fever/dehydration pancreatic/jejunal fistula/stoma loss urinary loss, e.g. post AKI polyuria. Check for: gross oedema severe sepsis hypernatraemia/ hyponatraemia renal, liver and/or cardiac impairment. post-operative fluid retention and redistribution malnourished and refeeding issues Seek expert help if necessary and estimate requirements. Prescribe by adding to or subtracting from routine maintenance, adjusting for all other sources of fluid and electrolytes (oral, enteral and drug prescriptions) Monitor and reassess fluid and biochemical status by clinical and laboratory monitoring *Weight-based potassium prescriptions should be rounded to the nearest common fluids available (for example, a 67 kg person should have fluids containing 20 mmol and 40 mmol of potassium in a 24-hour period). Potassium should not be added to intravenous fluid bags as this is dangerous. ‘Intravenous fluid therapy in adults in hospital’, NICE clinical guideline 174 (December 2013. Last update December 2016) © National Institute for Health and Care Excellence 2013. All rights reserved. Algorithms for IV fluid therapy in adults Algorithm 1: Assessment Yes Algorithm 2: Fluid Resuscitation Using an ABCDE (Airway, Breathing, Circulation, Disability, Exposure) approach, assess whether the patient is hypovolaemic and needs fluid resuscitation Assess volume status taking into account clinical examination, trends and context. Indicators that a patient may need fluid resuscitation include: systolic BP <100mmHg; heart rate >90bpm; capillary refill >2s or peripheries cold to touch; respiratory rate >20 breaths per min; NEWS ≥5; 45o passive leg raising suggests fluid responsiveness. No Assess the patient’s likely fluid and electrolyte needs History: previous limited intake, thirst, abnormal losses, comorbidities. Clinical examination: pulse, BP, capillary refill, JVP, oedema (peripheral/pulmonary), postural hypotension. Clinical monitoring: NEWS, fluid balance charts, weight. Laboratory assessments: FBC, urea, creatinine and electrolytes. Can the patient meet their fluid and/or electrolyte needs orally or enterally? Yes Ensure nutrition and fluid needs are met Also see Nutrition support in adults (NICE clinical guideline 32). No Does the patient have complex fluid or electrolyte replacement or abnormal distribution issues? Look for existing deficits or excesses, ongoing abnormal losses, abnormal distribution or other complex issues. Yes Algorithm 4: Replacement and Redistribution No Algorithm 3: Routine Maintenance ‘Intravenous fluid therapy in adults in hospital’, NICE clinical guideline 174 (December 2013. Last update December 2016) © National Institute for Health and Care Excellence 2013. All rights reserved. © National Institute for Health and Care Excellence 2013. All rights reserved. Algorithms for IV fluid therapy in adults Using an ABCDE (Airway, Breathing, Circulation, Disability, Exposure) approach, assess whether the patient is hypovolaemic and needs fluid resuscitation Assess volume status taking into account clinical examination, trends and context. Indicators that a patient may need fluid resuscitation include: systolic BP <100mmHg; heart rate >90bpm; capillary refill >2s or peripheries cold to touch; respiratory rate >20 breaths per min; NEWS ≥5; 45o passive leg raising suggests fluid responsiveness. Yes Algorithm 2: Fluid Resuscitation Initiate treatment Identify cause of deficit and respond. Give a fluid bolus of 500 ml of crystalloid (containing sodium in the range of 130–154 mmol/l) over less than15 minutes. Reassess the patient using the ABCDE approach Does the patient still need fluid resuscitation? Seek expert help if unsure No Yes Does the patient have signs of shock? Yes No Assess the patient’s likely fluid and electrolyte needs (Refer algorithm 1 box 3) Yes >2000 ml given? Seek expert help No Give a further fluid bolus of 250–500 ml of crystalloid ‘Intravenous fluid therapy in adults in hospital’, NICE clinical guideline 174 (December 2013. Last update December 2016) © National Institute for Health and Care Excellence 2013. All rights reserved. Algorithms for IV fluid therapy in adults Using an ABCDE (Airway, Breathing, Circulation, Disability, Exposure) approach, assess whether the patient is hypovolaemic and needs fluid resuscitation Assess volume status taking into account clinical examination, trends and context. Indicators that a patient may need fluid resuscitation include: systolic BP <100mmHg; heart rate >90bpm; capillary refill >2s or peripheries cold to touch; respiratory rate >20 breaths per min; NEWS ≥5; 45o passive leg raising suggests fluid responsiveness. No Yes Algorithm 2: Fluid Resuscitation Assess the patient’s likely fluid and electrolyte needs History: previous limited intake, thirst, abnormal losses, comorbidities. Clinical examination: pulse, BP, capillary refill, JVP, oedema (peripheral/pulmonary), postural hypotension. Clinical monitoring: NEWS, fluid balance charts, weight. Laboratory assessments: FBC, urea, creatinine and electrolytes. No Yes Can the patient meet their fluid and/or electrolyte needs orally or enterally? No Does the patient have complex fluid or electrolyte replacement or abnormal distribution issues? Yes Look for existing deficits or excesses, ongoing abnormal losses, abnormal distribution or other complex issues. Ensure nutrition and fluid needs are met Also see Nutrition support in adults (NICE clinical guideline 32). Algorithm 4: Replacement and Redistribution No Algorithm 3: Routine Maintenance Give maintenance IV fluids Normal daily fluid and electrolyte requirements: 25–30 ml/kg/d water 1 mmol/kg/day sodium, potassium*, chloride 50–100 g/day glucose (e.g. glucose 5% contains 5 g/100ml). Reassess and monitor the patient Stop IV fluids when no longer needed. Nasogastric fluids or enteral feeding are preferable when maintenance needs are more than 3 days. * Weight-based potassium prescriptions should be rounded to the nearest common fluids available (for example, a 67 kg person should have fluids containing 20 mmol and 40 mmol of potassium in a 24-hour period). Potassium should not be added to intravenous fluid bags as this is dangerous. ‘Intravenous fluid therapy in adults in hospital’, NICE clinical guideline 174 (December 2013. Last update December 2016) © National Institute for Health and Care Excellence 2013. All rights reserved. Algorithms for IV fluid therapy in adults Using an ABCDE (Airway, Breathing, Circulation, Disability, Exposure) approach, assess whether the patient is hypovolaemic and needs fluid resuscitation Assess volume status taking into account clinical examination, trends and context. Indicators that a patient may need fluid resuscitation include: systolic BP <100mmHg; heart rate >90bpm; capillary refill >2s or peripheries cold to touch; respiratory rate >20 breaths per min; NEWS ≥5; 45o passive leg raising suggests fluid responsiveness. No Assess the patient’s likely fluid and electrolyte needs History: previous limited intake, thirst, abnormal losses, comorbidities. Clinical examination: pulse, BP, capillary refill, JVP, oedema (peripheral/pulmonary), postural hypotension. Clinical monitoring: NEWS, fluid balance charts, weight. Laboratory assessments: FBC, urea, creatinine and electrolytes. No Yes Can the patient meet their fluid and/or electrolyte needs orally or enterally? Ensure nutrition and fluid needs are met Also see Nutrition support in adults (NICE clinical guideline 32). No Does the patient have complex fluid or electrolyte replacement or abnormal distribution issues? Look for existing deficits or excesses, ongoing abnormal losses, abnormal distribution or other complex issues. Yes Algorithm 4: Replacement and Redistribution Existing fluid or electrolyte deficits or excesses Check for: dehydration fluid overload hyperkalaemia/ hypokalaemia Estimate deficits or excesses. Ongoing abnormal fluid or electrolyte losses Check ongoing losses and estimate amounts. Check for: vomiting and NG tube loss biliary drainage loss high/low volume ileal stoma loss diarrhoea/excess colostomy loss ongoing blood loss, e.g. melaena sweating/fever/dehydration pancreatic/jejunal fistula/stoma loss urinary loss, e.g. post AKI polyuria. Redistribution and other complex issues Check for: gross oedema severe sepsis hypernatraemia/ hyponatraemia renal, liver and/or cardiac impairment. post-operative fluid retention and redistribution malnourished and refeeding issues Seek expert help if necessary and estimate requirements. Prescribe by adding to or subtracting from routine maintenance, adjusting for all other sources of fluid and electrolytes (oral, enteral and drug prescriptions) Monitor and reassess fluid and biochemical status by clinical and laboratory monitoring ‘Intravenous fluid therapy in adults in hospital’, NICE clinical guideline 174 (December 2013. Last update December 2016) © National Institute for Health and Care Excellence 2013. All rights reserved. .