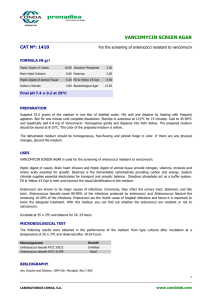
INFECTIVE ENDOCARDITIS Pathophysiology: Alteration of endothelial surfaces of heart valves, allowing organism attachment and colonization. Factors leading to endothelial alterations: inflammatory processes (e.g., rheumatic heart disease) or injury from turbulent blood flow. Platelets and fibrin deposit on damaged valves, forming NBTE Nonbacterial Thrombotic Endocarditis. Bacteremia facilitates bacteria adherence and colonization on NBTE, forming a vegetation. Further deposits of platelets and fibrin cover bacteria, creating a protective coating. Develops a conducive environment for continued organism and vegetation progression. Destruction of underlying tissue may occur, leading to valve leaflet perforation or rupture of chordae tendineae, interventricular septum, or papillary muscle. Portions of friable vegetation break loose, forming septic emboli. Right-sided IE (tricuspid and pulmonary valves) often leads to pulmonary abscesses. Left-sided IE (mitral and aortic valves) may cause emboli to various organs (kidneys, spleen, brain). Immune Complex Deposition: o Occurs in organs, particularly kidneys, causing abscesses, infarction, or glomerulonephritis. o Extracardiac manifestations include skin manifestations (petechiae, Osler nodes, Janeway lesions) and eye involvement (Roth spots). Prosthetic Valve Endocarditis (PVE): o Causative organisms in early PVE are typically nosocomial and often drugresistant. Clinical Presentation Symptoms: Fever (≥ 100.4°F) Chills Night sweats Generalized weakness Dyspnea Unexplained weight loss Myalgia or arthralgias Signs: Fever (most common sign of IE) New or changing/worsening heart murmur (occurs in 48% or 20%, respectively) Embolic phenomena (emboli affect the heart, lungs, abdomen, or extremities) Skin manifestations (ie, petechiae, splinter hemorrhages, Osler nodes, Janeway lesions) Splenomegaly Mycotic aneurysms Clubbing of extremities. Laboratory Tests: Blood cultures (most important laboratory test) Hematologic tests for anemia (normochromic, normocytic) WBC count may be elevated in acute disease but could be normal in subacute IE Nonspecific findings such as thrombocytopenia, elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), and abnormal urinalysis (ie, proteinuria or microscopic hematuria) Imaging Studies: Transthoracic echocardiogram (TTE) and/or transesophageal echocardiogram (TEE); key imaging to identify presence of vegetations CT or MRI may be used to assess involvement of other organ systems (ie, lungs, kidneys, and brain Acute phase staph Sub acute phase strep (less violent) Treatment Treatment considerations Selection of an appropriate antimicrobial agent must combine characteristics such as the ability to penetrate into the vegetation, the ability to achieve adequate drug concentrations, and the ability to be minimally affected by high bacterial inoculum to achieve adequate kill rates. To accomplish this, parental, bactericidal antimicrobials are typically required to ensure optimal treatment, with an extended treatment course of 4 to 6 weeks (in most cases). Empirical Treatment: Evaluate risk factors for likely causative organism. Empirical therapy: Primarily cover Gram-positive bacteria (S. aureus, viridans group streptococci, enterococci). Vancomycin is a reasonable empiric therapy; consider daptomycin if needed. Adjust coverage based on suspected pathogens; monitor response until cultures and susceptibilities determined. Organism-Specific Treatment: Streptococci: o Majority susceptible to penicillin; penicillin G or ceftriaxone preferred. o Duration: 4 weeks; shorter for uncomplicated cases with highly penicillinsusceptible strains. o Adjust treatment based on penicillin MICs. Staphylococci: o Identify methicillin susceptibility and valve type. o NVE: PRP or cefazolin for methicillin-susceptible; vancomycin or daptomycin for methicillin-resistant. o PVE: Prolonged treatment, consider addition of gentamicin and rifampin. Enterococci: o Determine specific species; dual beta-lactam regimen for susceptible strains. o Resistance to vancomycin: Consider daptomycin, linezolid, or combination therapy for at least 6 weeks. Gram-Negative Bacteria: Identify the pathogen; use aminoglycoside or fluoroquinolone in combination with appropriate β-lactam. Treatment duration: Minimum of 6-8 weeks; may involve surgical intervention. Consult infectious diseases specialist or endocarditis team. HACEK Group: Difficult to isolate; initiate empirical treatment with ceftriaxone or ampicillin-sulbactam. Fluoroquinolones may be used for intolerance. Treatment duration: 4 weeks (NVE) or 6 weeks (PVE). Culture-Negative IE: Empiric regimens based on patient characteristics, risk factors, and presentation. Consider vancomycin and cefepime (NVE, acute presentation) or vancomycin plus ceftriaxone (late PVE). Consult infectious diseases specialist or endocarditis team for management. Fungi: Treatment challenging; amphotericin B common, valve replacement often necessary. High-dose intravenous antifungal therapy for at least 6 weeks, followed by oral suppression. Newer antifungals (caspofungin, voriconazole) may be effective, depending on organism and susceptibilities. Prophylaxis: Presence of prosthetic valves or material, prior IE, select forms of congenital heart disease, and cardiac transplant patients with cardiac valvulopathy. No prophylaxis advised for other patients with cardiac dysfunction. Procedures Requiring Prophylaxis: Dental procedures involving manipulation of gingival tissue or periapical region. GI surgeries primarily targeting enterococci.