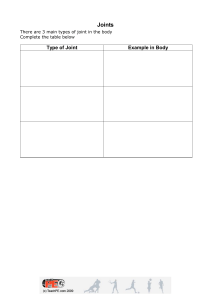
Musculoskeletal System: Bone and connective Tissue Disease Rheumatic Diseases: Affects joints, muscles, and soft tissue. S/S: Most common s/s are arthritis & pain. Clinical Manifestations: Pain, joint swelling, limited ROM, stiffness, weakness, fatigue. Medical Management: MEDS TO TARGET o Inflammation (aspirin, NSAIDS) o Management of s/s: DMARDs (disease, modifying, antirheumatic drugs/ suppress immune system. o Pain: non opioid o Nonpharm: hat, assistive devices/ braces, exercise, TENS. Nursing Management: Functional modifications, pain, psychological status. LABS: ERS & CRP (ELEVATED DUE TO INFLAMMATION). Rheumatic Arthritis: Autoimmune disease originated in the soft tissue of the distal joints. (WRISTS, HANDS, ELBOW, KNEE, ANKLES) Cycles of exacerbation and remission. HAVE FLAIR UPS DUE TO TRIGGERS. Risk factors: pollution, smoking, family hx. Scoring system: has to be greater than 6!! Joint involvement, blood studies, elevated ESR & CRP, and duration of s/s, and RF Factor. Clinical manifestation: symmetrical joint pain, morning stiffness, redness, warmth, decreased ROM. HALLMARK SIGN: SWAN-NECK DEFORMITIY & ULNAR DEVIATION. Underwight. Medical Management: Reduce pain, swelling, achieve remission, prevent/ decrease joint deformity, minimize disability. PT/ OT. o Meds: DMARD (methotrexate) get , corticosteroids, NSAIDS, opioids. o Labs: Baseline of liver function and reassess periodically ( r/t methotrexate use). CBC to monitor WBC for infection. Systemic Lupus Erythematosus: (LUPUS) Inflammation autoimmune disease, AFFECTING NEARLY ALL ORGANS!! Clinical Manifestation: Fever, fatigue, weight loss, anorexia, butterfly shaped rash across bridge of nose. Cardiac System manifestations: Pericarditis, myocarditis, HTN, arrhythmias. Medical management: Goal is to prevent progressive loss of organ function, minimize disfunction, and preventing complications. Medical management: o Hydroxychloroquine: tx cutaneous, musculoskeletal, and system features. o Monoclonal antibodies ( Belimumab): Reduces disease activity & flare ups. Nursing Management: Pt teaching for smoking cessation & light exposure, routine follow- ups, monitor for infection & osteoporosis. Gout: Acute inflammatory arthritis caused by INCREASED URIC ACID LEVELS ( ↑ 6.8). Clinical manifestation: Tophi (crystal deposits), urinary stones, nighttime onset (red/ swollen/ warm joints. MAINLY COMMON IN THE BIG TOE!! Risk factors: Increased BMI, regular consumption of alcohol, red meat/shellfish, high fructose drinks, diuretic use, aspirin. Medication management: DURING ATTACK ADMIN. Colchicine, CAUSES N/V & DIARRHEA!! Indocin, corticosteroids o Following acute attack: Administer allopurinol, febuxostat. o Lifestyle changes: weight loss, diet modification (reduces intake of alcohol, red meat, shellfish, and sugary drinks. FIBROMYALGIA: Chronic pain syndrome (muscle aching, stiffness, sleep disturbance, functional impairment. OSTERO-ARTHRITIS: (Degenerative Joint disease) Non-inflammatory degenerative disease. ONLY AFFECTS THE JOINTS, NO SYSTEMIC SYMPTOMS. Risk Factors: Increased age, obesity, female, occupational selection, genetics. S/S: Pain stiffness, functional impairment, crepitus, HERBERDEN’S & BOUCHARD’S NODES. NON-SYMMETRICAL! Medical Management: Symptom management & pain control. Tylenol, opiods, topical agents (diclofenac gel). Diet & exercise, PT/OT, improve & maintain functionality. Arthroplasty: Total hip replacement & total knee replacement: Rest & exercise balance, heat therapy, ice therapy. Total hip: no bending at the hip, no crossing the legs, do not turn on affected side. Septic Arthritis: Joint becomes infected. S. aureus common cause. S/S: Warm, painful, swollen joints, decreased ROM. o Systemic: fever, chills, leukocytosis o Musculoskeletal trauma & Orthopedic Surgery Fractures: Complete or incomplete disrupted in the continuity of bone structure. S/S: Pain, loss of function, deformity, shortening, crepitus, localized edema or ecchymosis. Management: Immobilize, check pulses and sensation distal to the site, OPEN FRACTURE: SPLINT & APPLY STERILE DRESSING. Open Reduction: IV antibiotics & tetanus shot, wound irrigation and wound vacs Cast: Tx of choice for fractures, used to correct/ prevent deformity & immobilize fracture. Will feel a warm sensation while cast is drying Splints & Braces: performed in acute care setting with plans to cast eventually. Assessment: 5 Ps- Pain, Pallor, pulselessness, paresthesia, paralysis. Nursing Management: Apply ice over fracture site. Elevate the extremity for 24-48 H. Move joints above and below cast regularly. Assess for hot spot, pulselessness, drainage, pressure injury. DO NOT: Get plaster cast wet, insert any objects inside the cast, bear weight, cover cast with plastic for prolonged periods. Complications: Compartment syndrome: increased pressure withing confined space, compromises, blood flow and tissue perfusion. Can be reversible if caught soon enough. o Remove cast, hold cast at heart level to promote blood flow, fasciotomy Disuse disorder: muscle atrophy, loss of strength because of prolonged immobilization Cast syndrome: GI distress due to having a body or spica cast. External fixator: Manage fractures with soft tissue damage, corrects defects, nonunion, and lengthens limbs. Advantages: Immediate immobilization, minimal blood loss, pt comfort, early mobilization. Disadvantages: pin site loosening and infection, risk for osteomyelitis. Nursing Management: assess for pressure injuries, sensation/ cap refill in ext, adhere to weight baring restrictions, encourage exercising withing approved limits Traction: Pulling force to promote and maintain alignment to injured body part. CONTINOUS, WITH WEIGHT HANGING FREELY. Goals: decrease muscle spasms and pain, realign bone fracture, correct/ prevent deformities. Complications: Shock, compartment syndrome, VTE, PE, delayed complications (union, avascular necrosis. Fat emboli S/S OF FAT EMBOLI: SOB, LOW O2 SAT, INITIAL INCREASES HR, PETECHIAE ON THE CHEST, CHEST PAIN, MORE COMMON CAUSED FROM FEMUR FRACTURE. Management: IVF, vasopressors, oxygen, steroids to reduce inflammation. Compartment syndrome: Impaired perfusion leading to necrosis and permanent dysfunction s/s: unrelenting pain worsening with ROM. Assess 5 Ps.