Telemedicine Impact Analysis: Future Prospects & Healthcare Delivery
advertisement

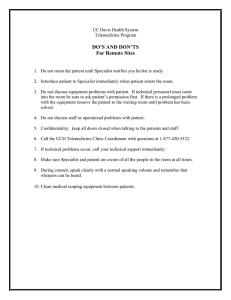
Title: "Revolutionizing Healthcare Delivery: A Comprehensive Analysis of the Impact and Future Prospects of Telemedicine" Abstract: This thesis explores the transformative role of telemedicine in the contemporary healthcare landscape, investigating its impact on accessibility, quality of care, and the overall efficiency of healthcare delivery. Through an in-depth analysis of the technological advancements, regulatory frameworks, and user perspectives, this study aims to provide a comprehensive understanding of the evolving nature of telemedicine and its potential to reshape the future of healthcare. The thesis also delves into the challenges and ethical considerations associated with telemedicine, offering insights into how stakeholders can collaborate to address these issues and maximize the benefits of this revolutionary approach to healthcare delivery. Aims and Objectives: Aim: The overarching aim of this research project is to comprehensively analyse the impact and future prospects of telemedicine on healthcare delivery, exploring its potential to revolutionize the way healthcare services are accessed and provided. Objectives: To examine the historical evolution of telemedicine: Investigate the origins and development of telemedicine to provide a foundation for understanding its trajectory in healthcare delivery. To explore the technological foundations of telemedicine: Analyse the key technologies that enable telemedicine, including communication tools, data exchange platforms, and remote monitoring devices. To assess the current regulatory landscape of telemedicine: Examine existing regulations governing telemedicine practices to identify their impact on adoption, scalability, and interoperability. To categorize and analyse different telemedicine models and modalities: Classify and critically evaluate various telemedicine approaches, including synchronous and asynchronous models, remote patient monitoring, and mobile health applications. To understand patient and provider perspectives on telemedicine: Investigate the attitudes, preferences, and concerns of both patients and healthcare providers regarding the adoption and use of telemedicine. To identify challenges and ethical considerations associated with telemedicine: Explore potential obstacles, such as privacy concerns, security issues, and disparities in access, and assess the ethical implications of telemedicine practices. To evaluate the impact of telemedicine on accessibility and geographical reach: Analyse how telemedicine contributes to improving access to healthcare services, especially in underserved or remote areas. To assess the impact of telemedicine on the quality of care: Examine the effectiveness of telemedicine in maintaining or enhancing the quality of healthcare delivery, including diagnostic accuracy, treatment outcomes, and patient satisfaction. To analyse the cost-effectiveness of telemedicine: Investigate the economic implications of telemedicine adoption, considering potential cost savings for both healthcare providers and patients. To examine patient outcomes associated with telemedicine use: Investigate the impact of telemedicine on health outcomes, patient adherence to treatment plans, and overall patient well-being. To explore the satisfaction levels of healthcare providers utilizing telemedicine: Assess the experiences and satisfaction levels of healthcare professionals who incorporate telemedicine into their practice. To investigate emerging technologies and innovations in telemedicine: Explore the latest technological advancements in telemedicine, such as artificial intelligence integration, virtual reality, and wearable devices. To propose recommendations for addressing challenges and ethical considerations: Develop practical recommendations for policymakers, healthcare providers, and technology developers to mitigate challenges and uphold ethical standards in telemedicine. To present case studies highlighting successful telemedicine implementations: Showcase examples of successful telemedicine implementations, extracting lessons learned and best practices for future endeavours. To provide policy implications and identify regulatory trends for telemedicine: Assess the potential policy implications and identify emerging regulatory trends that could shape the future of telemedicine. To offer insights into the future prospects of telemedicine: Provide a forward-looking analysis of the potential disruptions, innovations, and future developments in the field of telemedicine. To contribute to a comprehensive understanding of telemedicine's potential impact globally: Synthesize the findings to contribute valuable insights to academia, policymakers, healthcare practitioners, and technology developers, fostering a deeper understanding of telemedicine's global impact. Chapter 1: Introduction 1.1 Background 1.2 Rationale 1.3 Objectives 1.4 Scope and Limitations Chapter 2: Literature Review 2.1 Historical Evolution of Telemedicine 2.2 Technological Foundations 2.3 Regulatory Landscape 2.4 Telemedicine Models and Modalities 2.5 Patient and Provider Perspectives 2.6 Challenges and Ethical Considerations Chapter 3: Methodology 3.1 Research Design 3.2 Data Collection 3.3 Data Analysis Chapter 4: Impact of Telemedicine on Healthcare Delivery 4.1 Accessibility and Geographical Reach 4.2 Quality of Care 4.3 Cost-effectiveness 4.4 Patient Outcomes 4.5 Provider Satisfaction Chapter 5: Future Prospects and Innovations 5.1 Emerging Technologies in Telemedicine 5.2 Integration with Artificial Intelligence 5.3 Potential Disruptions and Innovations 5.4 Policy Implications and Regulatory Trends Chapter 6: Addressing Challenges and Ethical Considerations 6.1 Privacy and Security Concerns 6.2 Inequality in Access 6.3 Establishing Trust in Telemedicine 6.4 Ethical Guidelines for Telehealth Practitioners Chapter 7: Case Studies 7.1 Successful Implementation Stories 7.2 Lessons Learned from Failures Chapter 8: Recommendations 8.1 Policymakers 8.2 Healthcare Providers 8.3 Technology Developers 8.4 Future Research Directions Chapter 9: Conclusion 9.1 Summary of Findings 9.2 Implications for Healthcare Practices 9.3 Concluding Remarks -----------------------------------------------------------------------------------------------------------------------------------------------------------------Chapter 1: Introduction Introduction: In the rapidly evolving landscape of modern healthcare, technological advancements have become integral catalysts for transformative change. Among these innovatimodels anddicine has emerged as a groundbreaking paradigm, challenging traditional healthcare delivery models, and ushering in a new era of patient-centric and accessible services. This thesis embarks on a comprehensive exploration of the profound impact and prospects of telemedicine, aiming to dissect the intricate interplay between technology, healthcare, and societal needs. 1.1 Background Over the past decades, telemedicine has transcended its initial conceptualization, evolving from a niche practice into a mainstream solution with the potential to revolutionize the way healthcare is accessed and delivered. Enabled by advancements in telecommunications, information technology, and healthcare systems, telemedicine extends beyond geographical constraints, bridging the divide between patients and healthcare providers. The confluence of these factors not only addresses challenges related to healthcare accessibility but also opens avenues for improving the quality, efficiency, and affordability of healthcare services. 1.2 Rationale The rationale for undertaking this comprehensive analysis stems from the urgent need to understand the multifaceted implications of telemedicine on the healthcare ecosystem. As telemedicine gains traction globally, it is imperative to scrutinize its historical evolution, technological foundations, and the diverse models and modalities it encompasses. By doing so, we can discern the potential benefits and pitfalls, ensuring that the integration of telemedicine aligns with the overarching goal of enhancing healthcare outcomes and experiences for diverse populations. 1.3 Objectives This research project seeks to achieve a set of well-defined objectives. These include investigating the historical evolution of telemedicine, exploring its technological foundations, assessing the current regulatory landscape, categorizing diverse telemedicine models, and understanding the perspectives of both patients and healthcare providers. Additionally, the study aims to evaluate the impact of telemedicine on accessibility, quality of care, and cost-effectiveness, while addressing challenges and ethical considerations associated with its implementation. Furthermore, the project endeavours to identify emerging technologies, propose recommendations for addressing challenges, and offer insights into the future prospects and policy implications of telemedicine. 1.4 Scope and Limitations While the scope of this research project is extensive, acknowledging its limitations is essential for a nuanced interpretation of the findings. The study primarily focuses on telemedicine in the context of its impact on healthcare delivery, leaving aside broader discussions on healthcare policy and system-level considerations. Additionally, the dynamic nature of technology and healthcare introduces inherent challenges in capturing real-time developments. However, by adopting a rigorous methodology and drawing upon existing literature, this research aspires to provide a timely and insightful contribution to the ongoing discourse on telemedicine's transformative potential. Chapter 2: Literature Review 2.1 Historical Evolution of Telemedicine The historical roots of telemedicine can be traced back to the early experiments with telegraphy and telephony in the late 19th century. However, it was not until the latter half of the 20th century that advancements in communication technologies paved the way for telemedicine's practical applications. The seminal work of pioneers like Walter Reed and the establishment of the Space Technology Applied to Rural Papago Advanced Health Care (STARPAHC) project marked significant milestones in the early development of telemedicine. Over time, telemedicine has evolved from simple audio-visual consultations to sophisticated platforms integrating real-time data exchange, remote monitoring, and artificial intelligence. 2.2 Technological Foundations The technological underpinnings of telemedicine have undergone a paradigm shift, propelled by advancements in information technology, high-speed internet, and mobile communication. The integration of secure and interoperable platforms has enabled seamless communication between patients and healthcare providers, fostering the expansion of telemedicine beyond traditional boundaries. Cloud computing, data analytics, and Internet of Things (IoT) devices play pivotal roles in facilitating remote consultations, diagnostics, and treatment monitoring. As telemedicine continues to evolve, emerging technologies such as virtual reality and augmented reality are poised to further enhance the immersive healthcare experience. 2.3 Regulatory Landscape The widespread adoption of telemedicine is intricately linked to the regulatory frameworks governing its implementation. The regulatory landscape varies globally, with countries grappling to strike a balance between ensuring patient safety, fostering innovation, and addressing ethical considerations. Key issues include licensure, reimbursement policies, and data privacy. Notable initiatives, such as the Telemedicine Modernization Act in the United States and the European Union's efforts to harmonize telemedicine regulations, reflect ongoing endeavours to create an enabling environment for telemedicine practitioners. 2.4 Telemedicine Models and Modalities Telemedicine encompasses diverse models and modalities tailored to meet specific healthcare needs. Synchronous models involve real-time interactions between patients and healthcare providers through video conferencing or phone calls, offering immediacy in diagnosis and consultation. Asynchronous models, on the other hand, involve the exchange of patient information, such as images and medical records, allowing for flexibility in communication timing. Remote patient monitoring, teleconsultation kiosks, and mobile health applications further contribute to the versatility of telemedicine, catering to a spectrum of medical specialties and patient demographics. 2.5 Patient and Provider Perspectives Understanding the perspectives of both patients and healthcare providers is paramount to the successful integration of telemedicine into mainstream healthcare delivery. Patient acceptance, satisfaction, and perceived benefits influence the adoption of telemedicine services. Likewise, healthcare providers' attitudes towards telemedicine, encompassing concerns about technology reliability, diagnostic accuracy, and the doctor-patient relationship, play a pivotal role in shaping its implementation. Studies examining these perspectives contribute valuable insights into optimizing telemedicine practices to meet the needs and expectations of diverse stakeholders. 2.6 Challenges and Ethical Considerations The widespread adoption of telemedicine is not without challenges and ethical considerations. Privacy and security concerns regarding patient data, the potential for misdiagnosis in virtual consultations, and the exacerbation of healthcare disparities are critical issues that demand careful consideration. Striking a balance between innovation and safeguarding patient welfare requires the development of robust ethical guidelines, transparent communication, and ongoing efforts to address the evolving challenges associated with telemedicine. Chapter 3: Methodology 3.1 Research Design The research design for this thesis employs a mixed-methods approach to ensure a comprehensive and nuanced exploration of the impact and future prospects of telemedicine on healthcare delivery. The combination of qualitative and quantitative methods allows for a triangulation of data, enhancing the validity and reliability of the study. 3.2 Data Collection 3.2.1 Literature Review: A thorough review of academic literature, peer-reviewed articles, and relevant conference proceedings will provide a foundational understanding of the historical evolution, technological foundations, regulatory landscape, and diverse models of telemedicine. This literature review will be continuously updated to incorporate the latest research findings. 3.2.2 Surveys and Interviews: Surveys will be distributed to both healthcare providers and patients to gather quantitative data on their experiences, perceptions, and preferences regarding telemedicine. Additionally, in-depth interviews with a subset of participants will be conducted to extract qualitative insights into the nuanced aspects of telemedicine adoption and use. 3.2.3 Case Studies: Case studies will be conducted to analyse successful telemedicine implementations. This qualitative research method will provide valuable real-world examples, lessons learned, and best practices, offering a practical perspective on the impact of telemedicine in diverse healthcare settings. 3.2.4 Document Analysis: Relevant documents, such as regulatory policies, industry reports, and telemedicine guidelines, will be analysed to understand the broader policy context and regulatory trends shaping the implementation of telemedicine. 3.3 Data Analysis 3.3.1 Quantitative Data: Survey data will be analysed using statistical methods to identify patterns, trends, and correlations. Descriptive statistics will provide a quantitative overview, while inferential statistics will be employed to draw meaningful conclusions about the relationships between variables. 3.3.2 Qualitative Data: Thematic analysis will be applied to interview transcripts and case study findings to identify recurring themes, patterns, and divergent perspectives. Qualitative data analysis software will assist in organizing and interpreting textual data. 3.3.3 Cross-Method Analysis: The integration of quantitative and qualitative findings will enable a cross-method analysis, providing a more holistic understanding of the research questions. This approach aims to triangulate data, enhance the robustness of conclusions, and generate comprehensive insights. 3.4 Ethical Considerations 3.4.1 Informed Consent: Participants will be provided with clear and detailed information about the study's purpose, procedures, and potential risks. Informed consent will be obtained from all participants before their involvement in surveys, interviews, or case studies. 3.4.2 Confidentiality and Anonymity: Measures will be implemented to ensure the confidentiality and anonymity of participants. Identifiable information will be securely stored, and findings will be presented in aggregate to prevent the identification of individual participants. 3.4.3 Ethical Review: The research protocol will undergo ethical review by the relevant institutional review board (IRB) to ensure compliance with ethical guidelines and standards for research involving human participants. Chapter 4: Impact of Telemedicine on Healthcare Delivery 4.1 Accessibility and Geographical Reach Telemedicine has emerged as a potent tool in breaking down geographical barriers, significantly improving healthcare accessibility. Virtual consultations and remote monitoring enable patients to connect with healthcare providers regardless of their physical location. This chapter examines the extent to which telemedicine enhances accessibility, especially in remote or underserved areas, and explores the implications of increased geographical reach on healthcare delivery. 4.2 Quality of Care The integration of telemedicine into healthcare delivery holds implications for the quality of patient care. By enabling timely consultations, remote diagnostics, and continuous monitoring, telemedicine has the potential to enhance healthcare outcomes. This section investigates the impact of telemedicine on diagnostic accuracy, treatment efficacy, and patient satisfaction, aiming to discern how it contributes to maintaining or improving the overall quality of healthcare services. 4.3 Cost-effectiveness A critical aspect of healthcare delivery is the economic efficiency of services. Telemedicine has been heralded as a cost-effective solution, potentially reducing the financial burden on both healthcare providers and patients. This chapter assesses the economic implications of telemedicine adoption, exploring the potential cost savings, resource optimization, and improved healthcare resource allocation associated with its integration into the healthcare system. 4.4 Patient Outcomes Effective healthcare delivery is measured not only by the process but also by tangible patient outcomes. Telemedicine interventions, including remote monitoring and virtual consultations, influence patient adherence to treatment plans, recovery rates, and overall well-being. This section delves into empirical evidence and studies that illuminate the impact of telemedicine on various patient outcomes, providing insights into the effectiveness of these interventions. 4.5 Provider Satisfaction Telemedicine's impact extends beyond patients to the healthcare providers who adopt and utilize these technologies. This chapter explores the experiences and satisfaction levels of healthcare professionals engaging in telemedicine practices. Understanding the perspectives of providers is crucial for gauging the success and sustainability of telemedicine integration into routine healthcare delivery and identifying areas for improvement. Chapter 5: Future Prospects and Innovations 5.1 Emerging Technologies in Telemedicine The landscape of telemedicine is continually evolving, driven by rapid advancements in technology. This chapter explores the emerging technologies poised to shape the future of telemedicine. Innovations such as artificial intelligence (AI) integration, machine learning algorithms for diagnostics, virtual reality (VR) applications in telehealth, and the Internet of Things (IoT) for remote patient monitoring will be scrutinized. An in-depth analysis will be conducted to understand how these technologies may redefine the capabilities and potential applications of telemedicine in the coming years. 5.2 Integration with Artificial Intelligence Artificial intelligence is increasingly becoming a transformative force in healthcare. This section investigates how the integration of AI into telemedicine platforms can enhance diagnostic accuracy, personalize treatment plans, and optimize healthcare workflows. The exploration encompasses AI-driven chatbots for initial consultations, predictive analytics for proactive healthcare interventions, and the ethical considerations surrounding the use of AI in telemedicine. 5.3 Potential Disruptions and Innovations Beyond incremental advancements, this chapter explores potential disruptive innovations that could reshape the telemedicine landscape. From decentralized healthcare platforms built on blockchain technology to the integration of genomics data in telehealth consultations, the study delves into visionary concepts that may redefine the fundamental paradigms of healthcare delivery. Through scenario analyses and expert opinions, the chapter aims to provide insights into the potential game-changers on the horizon. 5.4 Policy Implications and Regulatory Trends As telemedicine continues to evolve, policy frameworks and regulatory environments must adapt to ensure safe, ethical, and efficient practices. This section investigates the evolving policy landscape, examining recent developments and anticipated trends in telemedicine regulations. The analysis extends to considerations of cross-border telehealth services, data privacy regulations, and the implications of regulatory frameworks on the adoption and integration of emerging telemedicine technologies. Chapter 6: Addressing Challenges and Ethical Considerations 6.1 Privacy and Security Concerns Telemedicine's expansion raises critical issues related to the privacy and security of patient data. This chapter delves into the challenges surrounding the confidentiality of electronic health records, secure data transmission, and the potential vulnerabilities in telemedicine platforms. Strategies and technologies employed to mitigate privacy and security risks, as well as the evolving regulatory landscape addressing these concerns, will be examined. The goal is to provide a comprehensive understanding of the measures required to establish a secure telemedicine environment. 6.2 Inequality in Access While telemedicine has the potential to enhance healthcare accessibility, disparities in access persist. This section explores the challenges associated with the digital divide, socioeconomic barriers, and disparities in healthcare infrastructure. The study investigates initiatives and policies aimed at addressing these issues, ensuring that telemedicine contributes to equitable healthcare access across diverse populations. 6.3 Establishing Trust in Telemedicine Trust is paramount in healthcare, and establishing trust in telemedicine encounters unique challenges. This chapter examines the factors influencing patient and provider trust in telemedicine, such as technology reliability, data accuracy, and the virtual doctorpatient relationship. Strategies for building and maintaining trust in telehealth interactions, including transparent communication and user education, will be analysed to provide insights into fostering confidence in telemedicine practices. 6.4 Ethical Guidelines for Telehealth Practitioners Telemedicine introduces ethical considerations that require careful attention. This section explores the development and implementation of ethical guidelines for telehealth practitioners, encompassing issues such as informed consent in virtual consultations, the ethical use of emerging technologies, and the preservation of patient autonomy. The study aims to contribute to the formulation of ethical frameworks that ensure the responsible and ethical practice of telemedicine across diverse healthcare settings. Chapter 7: Case Studies 7.1 Successful Implementation Stories This section of the thesis delves into real-world case studies that highlight successful implementations of telemedicine. Each case study explores the unique challenges faced, strategies employed, and outcomes achieved by healthcare organizations or practitioners leveraging telemedicine technologies. Case studies may include examples from various healthcare settings such as urban and rural clinics, specialty care, and integrated health systems. Analysing these success stories provides valuable insights into the practical applications of telemedicine and the factors contributing to its effectiveness. 7.2 Lessons Learned from Failures In contrast to success stories, this part of the chapter focuses on case studies where telemedicine implementations faced challenges or did not achieve the desired outcomes. By examining these less successful or failed attempts, the research aims to identify common pitfalls, barriers, and lessons learned. Understanding the factors that contribute to telemedicine implementation failures is crucial for refining strategies, improving adoption rates, and informing future initiatives. Chapter 8: Recommendations 8.1 Policymakers Telemedicine's successful integration into healthcare systems requires a supportive policy environment. Recommendations for policymakers include: Developing and updating telemedicine-specific regulations to address emerging technologies and modalities. Establishing reimbursement models that incentivize telemedicine adoption while ensuring cost-effectiveness and quality of care. Promoting research and development initiatives to continually assess the impact of telemedicine and inform policy decisions. Collaborating with stakeholders to create standardized interoperability and data exchange frameworks. 8.2 Healthcare Providers For healthcare providers looking to adopt or optimize telemedicine practices, the following recommendations are proposed: Investing in comprehensive training programs for healthcare professionals to enhance their proficiency in telemedicine technologies. Implementing user-friendly telemedicine platforms and ensuring seamless integration with existing electronic health record systems. Conducting regular assessments of patient and provider satisfaction to identify areas for improvement. Collaborating with technology vendors to stay abreast of emerging innovations and updates in telemedicine solutions. 8.3 Technology Developers Technology developers play a crucial role in shaping the future of telemedicine. Recommendations for this sector include: Prioritizing the development of secure, interoperable, and user-friendly telemedicine platforms. Incorporating artificial intelligence and machine learning capabilities to enhance diagnostic accuracy and treatment recommendations. Engaging in continuous research and development to explore innovative technologies that can further improve telemedicine outcomes. Collaborating with healthcare providers and organizations to tailor telemedicine solutions to specific healthcare contexts and specialties. 8.4 Future Research Directions To guide future research efforts in the field of telemedicine, the following recommendations are suggested: Investigating the long-term impact of telemedicine on patient outcomes, including chronic disease management and preventive care. Exploring the sociocultural factors influencing the adoption and acceptance of telemedicine across diverse populations. Assessing the economic implications of widespread telemedicine adoption on healthcare systems, insurers, and patients. Conducting comparative studies to evaluate the effectiveness of different telemedicine modalities in various healthcare settings. Chapter 9: Conclusion 9.1 Summary of Findings During this comprehensive exploration into the impact and prospects of telemedicine on healthcare delivery, a myriad of insights has been uncovered. From its historical evolution to its current technological foundations, regulatory landscapes, and diverse models, this research has provided a holistic understanding of telemedicine's multifaceted nature. The impact of telemedicine on accessibility, quality of care, cost-effectiveness, patient outcomes, and provider satisfaction has been scrutinized, shedding light on both its promises and challenges. 9.2 Implications for Healthcare Practices The findings presented in this thesis have significant implications for healthcare practices. The success stories detailed in case studies underscore the potential for telemedicine to improve healthcare accessibility, especially in underserved areas, and enhance the overall quality of patient care. Furthermore, the lessons learned from both successful and unsuccessful implementations provide valuable guidance for healthcare providers seeking to integrate telemedicine into their practices. 9.3 Concluding Remarks As we stand at the intersection of technological innovation and healthcare transformation, telemedicine emerges not merely as a tool but as a catalyst for redefining the very fabric of healthcare delivery. The successful implementation of telemedicine is contingent upon the collaborative efforts of policymakers, healthcare providers, technology developers, and researchers. It necessitates the continuous refinement of regulations, the cultivation of trust among patients and providers, and a commitment to addressing challenges related to privacy, security, and access disparities. In conclusion, telemedicine holds tremendous potential to democratize healthcare, providing equitable access to quality services while optimizing resource utilization. However, realizing this potential requires a conscientious and collaborative approach from all stakeholders. As we navigate the evolving landscape of healthcare delivery, let the insights garnered from this thesis serve as a compass, guiding us toward a future where telemedicine is seamlessly woven into the fabric of accessible, efficient, and patient-centric healthcare practices. -----------------------------------------------------------------------------------------------------------------------------------------------------------------Question Checklist 1.1 Identify the area for the research project. 1.2 Develop the aims and objectives of the research project. 1.3 Explain ethical considerations that apply to the area of the research project. 1.4 Complete a literature review of chosen area of research. 2.1 2.2 2.3 2.4 Critically compare different types of research. Evaluate a range of methods that can be used to collect data. Identify a range of tools that can be used to analyse data. Explain the importance of validity and reliability of data used within research. 3.1 Identify sources of support whilst conducting research project. 3.2 Formulate a detailed plan for research project. 3.3 Select research methods for the project. 3.4 Develop research questions to be used within project. 3.5 Conduct the research using identified research methods. 3.6 Record and collate data. 4.1 Use data analysis methods to analyse the data. 4.2 Draw conclusions from findings 4.3 Reflect how own research findings substantiate initial literature review.