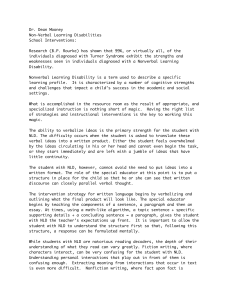
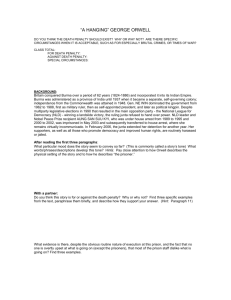
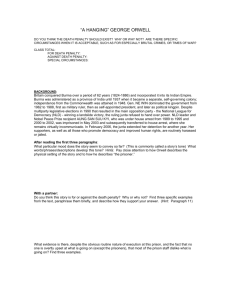
This article was downloaded by: [University of Birmingham] On: 19 September 2013, At: 12:47 Publisher: Routledge Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered office: Mortimer House, 37-41 Mortimer Street, London W1T 3JH, UK Developmental Neuropsychology Publication details, including instructions for authors and subscription information: http://www.tandfonline.com/loi/hdvn20 Neuropsychological Differences Among Children With Asperger Syndrome, Nonverbal Learning Disabilities, Attention Deficit Disorder, and Controls a b Margaret Semrud-Clikeman Ph.D. , Jenifer Walkowiak , Alison c Wilkinson & Gina Christopher d a Departments of Psychology and Psychiatry, Michigan State University, East Lansing, Michigan b Children's National Medical Center, Washington, DC c Children's Medical Center Dallas, Dallas, Texas d Department of Educational Psychology, University of Texas at Austin, Austin, Texas Published online: 16 Aug 2010. To cite this article: Margaret Semrud-Clikeman Ph.D. , Jenifer Walkowiak , Alison Wilkinson & Gina Christopher (2010) Neuropsychological Differences Among Children With Asperger Syndrome, Nonverbal Learning Disabilities, Attention Deficit Disorder, and Controls, Developmental Neuropsychology, 35:5, 582-600, DOI: 10.1080/87565641.2010.494747 To link to this article: http://dx.doi.org/10.1080/87565641.2010.494747 PLEASE SCROLL DOWN FOR ARTICLE Taylor & Francis makes every effort to ensure the accuracy of all the information (the “Content”) contained in the publications on our platform. However, Taylor & Francis, our agents, and our licensors make no representations or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of the Content. Any opinions and views expressed in this publication are the opinions and views of the authors, and are not the views of or endorsed by Taylor & Francis. The accuracy of the Content should not be relied upon and should be independently verified with primary sources of information. Taylor and Francis shall not be liable for any losses, actions, claims, proceedings, demands, costs, expenses, damages, and other liabilities whatsoever or howsoever caused arising directly or indirectly in connection with, in relation to or arising out of the use of the Content. This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden. Terms & Downloaded by [University of Birmingham] at 12:47 19 September 2013 Conditions of access and use can be found at http://www.tandfonline.com/page/termsand-conditions DEVELOPMENTAL NEUROPSYCHOLOGY, 35(5), 582–600 Copyright © 2010 Taylor & Francis Group, LLC ISSN: 8756-5641 print / 1532-6942 online DOI: 10.1080/875656412010494747 Downloaded by [University of Birmingham] at 12:47 19 September 2013 Neuropsychological Differences Among Children With Asperger Syndrome, Nonverbal Learning Disabilities, Attention Deficit Disorder, and Controls Margaret Semrud-Clikeman Departments of Psychology and Psychiatry, Michigan State University, East Lansing, Michigan Jenifer Walkowiak Children’s National Medical Center, Washington, DC Alison Wilkinson Children’s Medical Center Dallas, Dallas, Texas Gina Christopher Department of Educational Psychology, University of Texas at Austin, Austin, Texas Confusion is present as to possible diagnostic differences between Asperger syndrome (AS) and Nonverbal learning disabilities (NLD) and the relation of these disorders to attentional difficulties. Three-hundred and forty-five children participated in this study in 5 groups; NLD, AS, attention deficit hyperactivity disorder (ADHD): Combined type, ADHD: Inattentive type, and controls. The NLD group showed particular difficulty on visual-spatial, visual-motor, and fluid reasoning measures compared to the other groups. There was also a significant verbal-performance IQ split in this group related to difficulty in social functioning. This study extends the findings from previous studies and extends these findings to differences between AS and NLD groups. Previous studies have evaluated the neuropsychological functioning of children with nonverbal learning disabilities (NLD) (2000), Asperger disorder (AS) (Ozonoff & Griffith, 2000), or attention deficit hyperactivity disorder (ADHD) (Nigg, Blaskey, Huang-Pollock, & Rappley, 2002) Few studies have compared the neuropsychological functioning of children across these diagnoses in the domains of intelligence, achievement, motor, perception, and fluid reasoning. The purpose of this study was to evaluate possible differences among these groups on measures of verbal ability, fluid reasoning, and visual-motor skills. Correspondence should be addressed to Margaret Semrud-Clikeman, Ph.D., Michigan State University, Psychology Building, 321 A West Fee Hall, East Lansing, MI 48824. E-mail: semrudcl@msu.edu NEUROPSYCHOLOGICAL DIFFERENCES 583 Downloaded by [University of Birmingham] at 12:47 19 September 2013 NONVERBAL LEARNING DISABILITY The original concept of nonverbal learning disabilities was introduced by Johnson and Myklebust (1967) and included children who had difficulty with social perception. Subsequently Rourke and colleagues later suggested that the combined deficits of visual-spatial learning, tactile and motor skills, and mathematics make up a syndrome they termed a nonverbal learning disability (NLD) (Rourke, 1989; Rourke & Tsatsanis, 1996). An area of controversy in the area of NLD has been the definition of this disorder. Many studies utilize an approach where the child must meet a selection of symptoms from an array of possibilities in order to qualify for a diagnosis of NLD. Although the NLD subtype continues to be refined, it is currently characterized by three broad areas of dysfunction including motoric skills, visual/spatial organizational skills, and social abilities (Semrud-Clikeman, 2007). Children with NLD often show excellent single word reading skills and spelling ability but have difficulty with inferential thinking, complex reading comprehension, and mathematics (Semrud-Clikeman & Glass, 2008). Executive functioning for these children generally may be problematic as they often have difficulty in understanding situations that involve cause–effect reasoning, generating solutions to problems, and learning new material that is complex or novel (Rourke, 1995; Semrud-Clikeman, 2003). Many clinicians and researchers suggest that children with NLD have difficulty in correctly perceiving social relations and with social judgment (Semrud-Clikeman, 2007). Some have suggested that these social difficulties are secondary to difficulties with visual-spatial development (Rourke, 2000) while others suggest that there are significant perceptual problems that contribute to problems with understanding facial expressions, voice intonation, and the speaker’s intent (Forrest, 2007; Guli, Wilkinson, & Semrud-Clikeman, 2008; Pennington, 1991, 2008; SemrudClikeman, 2007). It is unclear from the empirical literature whether this hypothesis is accurate and further research that evaluates whether these perceptual and visual-spatial deficits underlie the social-emotional functioning of children with NLD is needed. ASPERGER SYNDROME A defining feature of AS is difficulty with social relationships. Particular difficulties are present in nonverbal behaviors (eye contact, facial expression, and body gestures), successful peer relationships, and with social reciprocity. Children with AS often have interests that are circumscribed and intense and may be inflexible in their adherence to routines. Neuropsychologically, children with AS show strong verbal skills, poor visual-spatial ability, and problems with executive functioning (Klin, Sparrow, Cicchetti, & Rourke, 1995). As some researchers have questioned the findings of visual-spatial difficulties in AS (Edgin & Pennington, 2005), this area of inquiry remains open. While diagnostic criteria for AS is contained within the DSM-IV-TR (American Psychiatric Association, 2000) structure, there is no commensurate manual for a diagnosis of NLD. There are several similarities between AS and NLD. In both disorders, problems with social communication and reciprocity, nonverbal communication, pragmatic language, and visual-spatial skills appear to be present (Gunter, Ghaziuddin, & Ellis, 2002; Voeller, 1995). Stronger verbal compared to performance skills on cognitive testing were found for children with AS or NLD (Gillberg & 584 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER Billstedt, 2000; Klin et al., 1995). It is important to note that the many of the symptoms of NLD may be present in children with AS. However, differences between children with AS and those with NLD include the presence of stereotyped and restricted patterns of interest and the need to adhere to routines present in children with AS but not NLD (Semrud-Clikeman, 2007). Downloaded by [University of Birmingham] at 12:47 19 September 2013 ADHD, AS, AND NLD Of interest for this study is the co-occurrence of ADHD in children with AS and NLD (Gillberg & Billstedt, 2000). Studies have found a high co-occurrence of ADHD in a sample of children with AS with 33% to 50% of the samples showing significant difficulties in inattention and 7% showing problems with overactivity (Gadow, DeVincent, & Pomeroy, 2006; Ghaziuddin, WeidmerMikhail, & Ghaziuddin, 1998; Leyfer et al., 2006; Nyden, Gillberg, Hjelmquist, & Heiman, 1999). Similar to children with AS those with NLD also show a tendency to have attentional difficulties. Children with NLD are often identified as having problems with attention and tend to be diagnosed with ADHD: Predominately Inattentive type (ADHD–PI) (Semrud-Clikeman, 2007). Some have suggested that the attentional problems found in children with NLD are due to visual perceptual and tactile difficulties (Rourke, 2000) while others suggest these difficulties are separate but that visual attentional issues may be related to problems with social functioning (Corbett & Constantine, 2006; Fine, Semrud-Clikeman, Butcher, & Walkowiak, 2008). Rourke (2000) suggested that deficits in visual perceptual skills may be related to attentional difficulty seen in many of these children rather than a true diagnosis of ADHD. Thus, these visual attentional issues may have a differential effect on social functioning for children with NLD apart from the difficulties found for children with ADHD; an area of inquiry that requires further research. Given the hypothesis that children with AS or NLD may have attentional differences, it was felt important to control for significant attentional problems for these children on the neuropsychological measures in this study. For this reason we included a group of children with ADHD–PI and Attention Deficit Hyperactivity Disorder: Combined type (ADHD–C) to attempt to control the effect attentional difficulties have on the ability to complete tasks that require executive functions. The main hypotheses of this study were that children with AS and NLD would show significant problems on measures of executive functioning, visual perception, and performance abilities compared to the children with ADHD or the control group. It was also hypothesized that children with NLD would show a difference in Verbal-Performance IQ skills compared to the other four groups as suggested by the literature. Moreover, it was hypothesized that children with NLD would show right-sided difficulties on measures of motor dexterity while these problems would not be present in the children with AS, ADHD–C, ADHD–PI, or controls. METHOD Participants Participants were children referred by parents, teachers, psychologists, psychiatrists, pediatricians, and community organizations to a large university for participation in a larger eight-year study examining the neuropsychological functioning of children with developmental disorders. The final sample included 345 children ranging in age from 9.1 years to 16.5 years. There were 242 males and Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 585 103 females in the sample with 18% of the sample self-identified as a minority (Hispanic, African American, and Asian). There were five groups of children identified for the purpose of this study; control (N = 113), AS (N = 50), NLD (N = 26), ADHD–C (N = 76), and ADHD–PI (N = 80). Reflecting the general rates of AS and ADHD comorbidity 27 of the AS group also had a secondary diagnosis of ADHD; 14 with ADHD–C and 13 with ADHD–PI. For the NLD group 22 also had a secondary diagnosis of ADHD; 6 with ADHD–C and 16 with ADHD–PI. Doctoral-level graduate students trained in administering a comprehensive neuropsychological battery individually assessed the participants. These graduate students were blind to the diagnosis of the child. Diagnoses were determined by consensus of two independent sources; licensed psychologists within the community or university, and advanced doctoral students. Participants for whom a diagnosis was not unanimous were not included in the study (N = 5). Exclusionary criteria included a history of a reading disability, seizure disorder, progressive neurological problems, traumatic brain injury, or any other serious medical condition. Those with comorbid psychopathology were also excluded from the sample, including participants with severe mood or conduct disorders. Only children with a FSIQ above 80 were included in the sample. Children with a diagnosis of ADHD were diagnosed by either private practitioners (psychiatrists or psychologists) or through the neuropsychology clinic at the university. Our confirmation of a diagnosis for ADHD required a T-score of 65 or higher on the Behavior Assessment Scale for Children–2 (BASC–2)(Reynolds & Kamphaus, 2004) inattention and/or hyperactivity scale as well as meeting criteria for DSM-IV-TR (American Psychiatric Association, 2000) diagnosis of ADHD using a parent semi-structured interview. Children in the control group had no history of learning, behavioral, or attentional difficulties both by parent and teacher report and an interview completed prior to participation. No child in this group met criteria for AS, NLD, or reading disability. The Autism Diagnostic Interview (ADI–R) (Le Couteur, Lord, & Rutter, 2003) or the Autism Diagnostic Observational System (ADOS)(Lord, Rutter, DiLavore, & Risi, 1999) were administered to children in the AS group through a private practitioner to determine the presence of autistism spectrum disorders (ASD). These results were not generally available for the study from these private practitioners. No child met the criteria for autism using the ADI–R. The children were diagnosed with AS partly based on the results of one of these measures with the diagnosis of AS confirmed using DSM-IV-TR (American Psychiatric Association, 2000) criteria for this study. An AS screener based on DSM-IV-TR Asperger syndrome criteria developed at the clinic and completed by the child’s primary caretaker was used for tertiary confirmation. The cutoff score on this measure was 6 as defined by DSM-IV-TR criteria. There were three children excluded from the study who did not meet all of these criteria. Of the children with AS approximately 25% would also have met criteria for NLD. An independent licensed psychologist evaluated approximately half of the sample of children diagnosed with a nonverbal learning disability. This diagnosis was confirmed through review of previous testing if current or through an updated assessment. Agreement among the two first authors and any previous diagnosis was required for inclusion in the study. There were six children who were found to not qualify under the following criteria or who met criteria for significant depression or anxiety disorder diagnoses. Consistent with the recommendations from research criteria (Rourke & Tsatsanis, 1996), children with NLD qualified for this group if they met all of the following criteria: (1)Scores 1 standard deviation below average on the parent form of the Social Skills Rating Scale (SSRS) (Gresham & Elliott, 1990); (2) Math calculation skills below the 15th percentile on the math calculation subtest of the Woodcock-Johnson Achievement Test III Downloaded by [University of Birmingham] at 12:47 19 September 2013 586 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER (WJ-Ach III) (Woodcock, McGrew, & Mather, 2001b); (3) Average scores on the letter-word identification subtest from the WJ-Ach III (Woodcock et al., 2001b); (4) Average estimated verbal IQ of at least 85 standard score points on the Wechsler Abbreviated Scale of Intelligence (WASI) (Psychological Corporation, 1999); (5) Scores at least one standard deviation below average on the Visual Motor-Integration Test (VMI) (Beery, Buktenica, & Beery, 2006); and (6) Below average scores on the Purdue Pegboard (Tiffin, 1968). We decided to use a more conservative approach to diagnosis and to view the disorder as a syndrome which incorporated the main areas of visual-motor skills, motor skills, social functioning, and good verbal ability. It is important to mention here that children with AS may have many symptoms that are consistent with a diagnosis of NLD. For the current study, however, children with AS were selected apart from similarities with the NLD group when one of more of the following symptoms were found during the parent interview: a stereotyped and restricted pattern of interests, inflexible adherence to nonfunctional routines, stereotyped and repetitive motor mannerisms, preoccupation with parts of objects, and a lack of spontaneous seeking to share enjoyment, interests, or achievements with others. The children in the AS group also were not required to show the same symptoms as detailed above. Inclusionary Instruments WASI (Psychological Corporation, 1999). The WASI is an abbreviated scale of intelligence with measures of similarities, vocabulary, block design, and matrix reasoning. As discussed earlier, there are research findings that indicate the performance IQ may be impacted in children with NLD. For this reason, the VIQ was used as an estimate of ability. WJ-Ach III (Woodcock et al., 2001b). Three subtests from the WJ-Ach III were administered; letter-word identification, calculation, and mathematics reasoning. VMI (Beery et al., 2006). The VMI requires the child to copy increasingly more difficult geometric figures within a grid. It provides a measure of visual-motor skills. Purdue Pegboard (Tiffin, 1968). The Purdue Pegboard requires the child to place pegs in holes as quickly as possible first with the dominant hand, then the nondominant hand, and then both hands together for 30 seconds each. This measure has been found to be a good measure of manual dexterity but not necessarily useful for determining lateralization (Reddon, Gill, Gauk, & Maerz, 1988). The Structured Interview for Diagnostic Assessment of Children (SIDAC) (Puig-Antich & Chambers, 1978). The SIDAC is a formal interview based on DSM-IV diagnoses, modified and updated from the Kiddie-Schedule of Affective Disorders and Schizophrenia (K-SADS) developed by Puig-Antich and Chambers (1978). The ADHD portion of the SIDAC interview was used in this study to determine the presence of ADHD symptoms with severity based on the number of symptoms reported. Symptoms related to inattention, hyperactivity, and impulsivity were included. This measure was also used as partial confirmation of parent-reported diagnosis of ADHD, as noted earlier. Behavior Assessment System for Children–2 (BASC–2) (Reynolds & Kamphaus, 2004). Two subtests from the BASC–2 parent rating scale were used as a measure of attention and hyperactivity. The BASC–2 is an omnibus behavioral rating scale that provides normative data for specific behaviors. It has excellent psychometric properties. NEUROPSYCHOLOGICAL DIFFERENCES 587 Social Skills Rating Scale (SSRS) (Gresham & Elliott, 1990). The SSRS is a behavioral rating scale completed by the child’s main caretaker. It measures total social skills through a Likert scale of three options (never, sometimes, and very often). Downloaded by [University of Birmingham] at 12:47 19 September 2013 Study Measures Woodcock-Johnson Cognitive Battery III (WJ-Cog III) (Woodcock, McGrew, & Mather, 2001a). Two subtests that make up the Fluid Reasoning index were utilized from the WJ-Cog III; analysis/synthesis and concept formation. These tests require the child to look at a problem and utilize the information present to solve the item. Analysis and synthesis requires the child to solve picture equations while concept formation requires cognitive flexibility and skill in evaluating problems to determine what is similar between the stimuli. Rey-Osterreith Complex Figure (Osterreith, 1944). The Rey-Osterreith complex figure test requires the child to copy a complex figure as accurately as possible and is a measure of perceptual organization (Lezak, Howieson, & Loring, 2004). The scoring system used is the one developed by Osterreith and translated by Corwin and Bylsma (1993) involving the widely used 18-item, 36-point scoring system. Judgment of Line Orientation (JLO) (Benton, Sivan, Hamsher, Varney, & Spreen, 2004). The JLO is a measure of spatial ability without a motor component. The child is asked to look at an array of lines and then is shown two lines. He/she is then asked to match the two lines to the array. Grooved Pegboard (Klove, 1963). The grooved pegboard measures complex finger coordination. It consists of a board with slotted holes angled in various directions. Each peg has a groove and only fits in one way in each hole. The child uses first the dominant hand and then the nondominant hand to place the pegs as quickly as possible. It has been recommended as a good measure of lateralized impairment (Lezak et al., 2004) Finger Tapping Test (Reitan & Wolfson, 1985). The Finger Tapping test requires the child to tap a key as quickly as possibly first with the dominant hand and then with the nondominant. Analyses Multivariate analysis of variance (MANOVA) with multiple post-hoc comparisons was used to determine whether there were group differences based on age or verbal IQ in the sample. The general linear model (GLM) with post-hoc comparisons was used to evaluate group differences among the behavioral, cognitive, and neuropsychological measures. RESULTS Table 1 presents the group means and standard deviations for the sample age, estimated Verbal IQ measure, and group selection measures. There were no significant differences among groups for 588 11.1 46.9 49.7 53 111.9 106.4 112.5 101.3 .04 –.24 –.11 BASC-attn9 SSRS10 VIQ11 Reading Mathematics Calculation VMI12 Purdue RH13 Purdue LH14 Purdue Both Hands –.97 101 –1.14a –1.3 107.8 97.1 107.3 64.7 37.1 64.1 10.6 10.3 10.2 Mean 1.9 17 1.8 1.7 17 17.4 17.6 11 11.2 13.8 4.1 28.8 2.3 SD AS2 (N = 50) –1.29 87.5 –1.33 –.98 102.2 90.8 109.7 65.7 38.7 64.3 10.2 11.3 5.3 Mean 1.4 11.7 1.5 1.2 15.2 19.7 16.7 8.9 8.5 12.3 3.4 26.1 2.3 SD NLD3 (N = 26) –.45 96.6 –.68 –.44 106.7 101.1 110 67.9 40 72 14.3 10 5.7 Mean 1.2 15.5 1.3 1.2 13.2 17.9 16.6 8.2 8.7 11.9 2.4 24.4 3.7 SD ADHD-C4 (N = 76) –.57 97 –.61 –.42 108.25 100 106.1 67.7 44.1 55.4 10.7 10.8 5.6 Mean 1.2 8.7 1.2 1.4 14.6 20.7 11.7 7.6 10.9 10.8 5.2 25.4 3.2 SD ADHD-PI5 (N = 80) N.S. NLD < ADHD-C (p = .007), ADHD-PI (p = .04) C > All (p < .0001) NLD < All (p < .02) C < All (p < .03) AS < C (p = .001), ADHD-C (p = .01), ADHD-PI (p = .01) NLD < C (p = .04) NLD, AS < C (p < .001), NLD < ADHD-C (p = .03) N.S.6 AS > C (p < .0001), NLD (p < .0001) , ADHD-C (p < .0001), ADHD-PI (p < .0001) C < NVLD, ADHD-C, ADHD-PI (p < .0001) AS, NLD, ADHD-PI > C (p < .0001) ADHD-C > All (p < .0001) ADHD-C > ADHD-PI , AS, NLD (p < .0001) C < AS, NLD, ADHD-C, ADHD-PI (p < .0001) C < All (p < .0001) AS, NLD < ADHD-C (p < .022) ADHD-PI> AS (p < .0001), NLD (p = .022), ADHD-C (p = .014) C < All (p < .0001) N.S. Group Significance 1Standard deviation; 2Asperger Syndrome; 3Nonverbal Learning Disability; 4Attention deficit hyperactivity disorder–Combined type; 5Attention deficit hyperactivity disorder—Predominately Inattentive Type; 6Not significant; 7Structured interview; 8Social Skills Rating Scale; 9Behavior Assessment System for Children–Hyperactivity scale; 10Behavior Assessment System for Children–Attention scale; 11Verbal IQ; 12Visual-Motor Integration Test; 13Right hand; 14Left hand. 1.04 12.5 1.04 1.3 12.3 15 14.3 9.3 10.8 3 2.7 SIDAC Total7 BASC-hyper8 25.1 1.4 SD1 10.4 .9 Mean Age AS screener Variable Control (N = 113) TABLE 1 Significant Group Differences for Group Selection Measures; Means and Standard Deviations Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 589 age (p = .18). As expected due to selection criteria, there was not a significant difference in estimated Verbal IQ among the groups (p = .085, partial eta squared = .024). Analyses of Group Selection Measures Downloaded by [University of Birmingham] at 12:47 19 September 2013 Membership in groups was partially determined by scores on selected psychological measures. Preliminary analyses were conducted to determine whether the expected group differences were present. These results are provided in Table 1. Visual-Spatial Measures. Scores from the VMI were evaluated using a one way ANOVA. A significant group difference was present for the VMI (F(4,290) = 5.68, p < .0001, partial eta squared = .07). Post-hoc comparisons found that the NLD group differed from all of the other groups (p < .02). These findings were expected for the NLD group as it was a variable involved in the selection for the group. A preliminary analysis of the right (RH), left (LH), and both hands results of the Purdue Pegboard found a significant main group effect difference for all conditions (F(12, 418) = 2.45, p = .004, partial eta squared = .058). Follow-up analyses found that there were significant group differences for all conditions (p < .008). Post-hoc analysis found that Control group scored better with the RH compared to the clinical groups (p < .03). Among the clinical groups there were no differences for the RH. For the LH, the AS and NLD groups scored significantly worse than the control group but not from each other (p = .44). This finding was predicted by the selection criteria for the NLD group. This finding was not predicted for the AS group. For the both hands condition, the AS and NLD groups were significantly less successful than the control group (p < .001) but did not differ from each other. The NLD group also scored worse compared to the ADHD–C group (p = .03). Behavioral Measures On the semi-structured interview (SIDAC) a significant main effect for group was found (F(4, 337) = 124.6, p < .0001) for total symptoms of attention/impulsivity/hyperactivity. Post-hoc comparisons found that the control group scored significantly lower than all clinical groups (p < .0001). Clinical group comparisons found the ADHD–C group to score lower than all other clinical groups (p < .0001). There were no significant differences between the AS, NLD, or ADHD–PI groups. A preliminary analysis of the hyperactivity and attention scales of the BASC–2 was completed using a 2 × 5 MANOVA. As expected significant findings were present for the main effect for group (F(8, 656) = 47.2, p < .0001, partial eta squared = .37). Follow-up analyses found significant group differences for attention (p < .0001) and hyperactivity (p < .0001). For the hyperactivity measure, post-hoc analyses found that the ADHD–C group differed significantly from all of the other groups (p = .005). When the clinical groups were compared, the ADHD–C showed significantly higher scores on the hyperactivity measure from all of the other clinical groups (p < .0001) while the AS, NLD, and ADHD–PI groups did not differ from each other. For the attention measure all clinical groups were less successful than the control group (p < .0001). No significant differences were found among the clinical groups on the attention measure. 590 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER Downloaded by [University of Birmingham] at 12:47 19 September 2013 Social Skills Selection Measure On the SSRS there was a significant main effect for group (F(4, 329) = 30.2, p < .0001) with the control group scoring significantly higher than all of the clinical groups (p < .0001). There were significant differences between the NLD and ADHD–C group (p = .022) with the NLD group scoring significantly worse than the ADHD–C group. There was no significant difference between the NLD and AS groups (p = .54). The ADHD–PI group was rated better on this measure compared to the ADHD–C (p = .014), AS (p < .0001) and NLD (p = .022) groups. For the AS screener an ANOVA found a significant group difference (p < .0001). Post-hoc analyses found that all of the clinical groups scored higher than the control group (p < .0001). Clinical group comparisons found that the AS group scored higher than the NLD and ADHD groups (p < .0001). No difference was found among the NLD and ADHD groups (p > .05). Table 1 provides these findings Analysis of Measures of Interest Evaluation of the estimated verbal and performance IQs using a 2 (verbal, performance) × 5 (group) MANOVA found a significant main effect for group (F (8, 678) = 5.769, p < .0001, partial eta = .064). Table 2 provides these results. Follow-up analysis found no significant difference for the verbal estimated IQ among groups (p = .085, partial eta = .024) with a significant difference present for the performance estimated IQ among groups (p < .0001, partial eta = .095). Post-hoc analysis found that the NLD group scored significantly worse than the control group (p < .0001), AS group (p = .001), and both ADHD groups (p < .0001). The AS group scored worse compared to the control group (p = .018) but not the ADHD groups. To evaluate whether the difference between verbal and performance estimated IQ differed among the groups, a one way ANOVA was conducted. A significant group difference was found (F(4, 337) = 6.8, p < .0001, partial eta squared = .075). Post hoc comparisons indicated significant differences among the NLD group and all of the other groups with the NLD group showing the largest split (p < .006). No other group differences were found. A significant main effect for group was found for academic achievement (F(12, 804) = 6.97, p < .0001, partial eta squared = .084). (See Table 2.) Follow-up analysis found no significant difference for reading recognition among the groups (p = .16) while mathematics calculation (p < .0001) and mathematics reasoning (p < .0001) were significant. Post-hoc analysis found significant differences among all of the clinical groups and the control group for mathematics calculation (p < .0001) with the control group scoring better. Analysis of the clinical groups found that the NLD group performed significantly worse than the ADHD–C (p = .007) and ADHD–PI group (p = .04) on mathematics calculation but not the AS group (p = .16). The ADHD groups did not differ from each other (p = .39). The finding of differences for the NLD was not unexpected as it was one of the criteria for selection for that group. For mathematics reasoning, the control group performed significantly better than all of the clinical groups (p < .04). Among the clinical groups the NLD group was less successful than the ADHD–C group (p < .0001) and the ADHD–PI group (p = .001) but not the AS group (p = .1). The ADHD groups did not differ from each other significantly (p = .84). 591 13.7 1.5 114.0 112.6 113.8 110.1 V-P7 Split Mathematics Reasoning Fluid Reasoning AnalysisSynthesis Concept Formation .9 1.2 1.5 1.3 1.7 1.3 –.16 –.14 –.82 –.59 –.26 .2 13.7 19.2 13.5 –.8 –.7 –2.4 –.08 –1.64 –.71 102.5 104.1 100.4 3.4 103.0 103.9 Mean 1.9 1.7 2.8 1.6 2.6 .85 17.9 12.5 23.1 18.4 18.7 18.9 SD AS2 (N = 50) –1.4 –.8 –2.9 –1.8 –4.5 –1.7 96.4 98.5 96.7 18.8 97.4 90.9 Mean 1.7 .95 3.5 1.9 6.9 2.5 16.8 13.6 15.1 19.8 19.1 18.1 SD NLD3 (N = 26) .3 .34 –1.2 –.13 –.9 –.25 105.5 108.5 108 .71 108.3 109.1 Mean 1.2 1.1 1.6 1.5 1.5 .9 18.1 16.6 14.7 16 16.4 12.7 SD ADHD-C4 (N = 76) –.2 –.07 –1.1 –.3 –.96 –.14 106.1 105.9 107.1 –2.5 109.1 109.5 Mean 1.3 1 1.8 1.2 1.9 1.4 13.4 17.6 13.4 14.7 12.3 14.6 SD ADHD-PI5 (N = 80) N.S.11 N.S. NLD < All (p < .001) NLD < C (p = .001), ADHD-C (p = .008), ADHD-PI (p = .004) AS, NLD < C (p = .01) NLD < C (p < .0001) AS < C (p < .005) NLD < ADHD-C, ADHD-PI (p < .01) NLD < All (p < .01) AS < C (p = .018) NLD < C. ADHD groups (p < .0001) NLD < AS (p < .001) NLD > All (p < .006) NVLD < ADHD-C (p < .0001), ADHD-PI (p = .001) C > All clinical groups (p < .04) AS, NLD < C (p < .0001) AS < ADHD-C (p = .01), ADHD-PI (p = .03) NLD < ADHD-C (p .003), ADHD-PI (p = .006) AS, NLD, ADHD-PI <C (p < .03) Group Significance 1Standard deviation; 2Asperger Syndrome; 3Nonverbal Learning Disability; 4Attention deficit hyperactivity disorder–Combined type; 5Attention deficit hyperactivity disorder–Predominately Inattentive Type; 6Performance IQ; 7Verbal-Performance; 8Judgment of Line Orientation; 9Right hand; 10Left hand; 11Not significant. Rey Osterreith JLO8 Grooved Peg RH9 Grooved Peg LH10 Tapping RH Tapping LH 13.6 110.4 PIQ6 17.4 Mean Measure SD1 Control (N = 113) TABLE 2 Significant Group Differences on Neuropsychological Measures: Means and Standard Deviations Downloaded by [University of Birmingham] at 12:47 19 September 2013 592 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER Downloaded by [University of Birmingham] at 12:47 19 September 2013 Fluid Reasoning Cluster A significant main effect for group was found on the fluid reasoning measures (F(4, 305) = 8.28, p < .0001, partial eta squared = .1). (See Table 2.) Post-hoc analyses found that the NLD (p < .0001), AS (p < .0001), and ADHD–PI (p = .026) performed significantly worse than the control group on this measure. Within the clinical groups the NLD group performed significantly worse than the ADHD–C (p = .003) and ADHD–PI (p = .006) groups but not the AS group (p = .35). In addition, the AS group differed significantly from the ADHD–C (p = .010) and ADHD–PI (p = .03) groups. The ADHD groups did not differ from each other (p = .72). When the individual subtests from the fluid reasoning cluster were evaluated a significant difference was found for the analysis/synthesis subtest (p < .0001) and for the concept formation subtest (p = .001). Post-hoc comparisons for the analysis/synthesis subtest found that the AS, NLD, and ADHD–PI all performed significantly worse than the controls (p < .03) while the ADHD–C group did not differ significantly from the control group (p = .06). The NLD group scored more poorly compared to the ADHD–C group (p = .01) with no other clinical group differences found. On the concept formation subtest there was a significant difference between the AS (p = .005) and NLD (p < .0001) groups and the control group. The NLD group scored significantly more poorly compared to the ADHD–C (p = .01) and ADHD–PI (p = .01) but not from the AS group (p = .12). Visual-Spatial Abilities To evaluate group differences on visual-motor and visual-spatial skills a 2 (JLO, Rey-Osterreith) × 5 (group) MANOVA was conducted. A significant main effect for group was present (F(8, 308) = 3.9, p < .0001, partial eta squared = .1). Follow-up analyses found that there was a group difference for the Rey-Osterreith (p = .001) and the JLO (p < .0001). Post-hoc analysis found that the NLD group performed significantly worse than the control (p < .0001), AS (p = .01), and both ADHD groups (p < .0001) on the Rey-Osterreith Complex Figure. There was no significant difference among the other groups. Similarly for the JLO the NLD group performed significantly worse than all of the groups (p < .001) with no differences found among the other groups. These findings indicate significantly poorer performance on all measures of visual-organization and visual-spatial skills as predicted. To evaluate the relation among the level of social skill development and these visual-spatial abilities, a correlation was performed. There was a significant overall correlation between the JLO and the SSRS social skills rating (p = .013). Similarly there was a significant overall correlation between the Rey-Osterreith and the SSRS (p = .017). Motor Skills To evaluate complex motor skills a 4 (Grooved Pegboard RH, Grooved Pegboard LH, Tapping RH, Tapping LH) × 5 (group) MANOVA found a significant main effect for group (F(16, 336) = 2.56, p = .001, partial eta squared = .08). Follow-up analyses found significant differences present for the Grooved Pegboard RH (p = .002), Grooved Pegboard LH (p = .002), Tapping RH (p = .05), and Tapping LH (p =.02). Post-hoc analyses found that for the Grooved Pegboard RH the NLD group was significantly slower than the control group (p = .001) with no significant difference found among the ADHD Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 593 groups, AS group, and the control group (p > .3). The NLD group performed significantly worse than the ADHD–C (p = .008) and ADHD–PI group (p = .004) with no significance difference from the AS group (p = .056). For the Grooved Pegboard LH a significant differences was present for the AS (p = .01) and NLD (p = .01) groups compared to the control group. Post-hoc analysis found that for Tapping LH the AS (p = .009) and NLD (p = .027) groups performed significantly worse than the control group. No significant differences were found between the ADHD groups and the control group (p > .4). The AS group performed significantly worse than the ADHD–C group (p = .01) but not the ADHD–PI group (p = .1) or the NLD group (p = .9). The NLD group performed significantly worse than the ADHD–C group (p = .03) but not the ADHD–PI group (.13). No difference was present between the ADHD groups (p = .31). DISCUSSION One of the main aims of this study was to determine whether there are neuropsychological differences among children with NLD, AS, or ADHD. A main research question was to explore skills on measures of visual-spatial, fluid reasoning, and motor skills compared to children with AS or ADHD. It was hypothesized those children with ADHD–C and ADHD–PI would not show problems in these areas. Cognitive Differences The hypothesis that the NLD group would score more poorly on the Performance IQ measure compared to the other groups was confirmed. The AS group scored more poorly than the control group but not the ADHD groups and there was no difference among the ADHD groups and the control groups on this measure. The NLD group also scored more poorly than the AS group on the Performance IQ of the WASI. In addition the Verbal-Performance IQ split was found to be significantly larger only for the NLD group. No significant difference between verbal and performance abilities was present among the other groups. These findings are consistent with those from the literature suggesting the V-P split in children with NLD. Our study did not select subjects based on this split. We utilized this procedure in order to determine whether this split is indeed present in this population. In the NLD sample 74% of the individuals had a V > P split of more than 15 standard score points and 40% had a split of 25 standard score points or higher (range from 15 to 55). This finding was different for the AS group where 63% showed verbal and performance IQs within 15 of each other. However, 37% showed VIQ > PIQ in the AS group. This finding indicates that while children with NLD are more likely to show a VIQ > PIQ split; there is a sizable minority of children who do not. While this study does find that most children with NLD in our sample did show such a split, this finding is not sufficient to provide a distinction between a diagnosis of NLD and that of AS. Other researchers have reached a similar conclusion when looking at children with NLD (Pelletier, Ahmad, & Rourke, 2001). Conversely, for the AS group there is a sizable minority of children who also show a VIQ > PIQ split. Recently, Black, Wallace, Sokoloff, and Kenworthy (2009) found that children with autism with a discrepantly high verbal or performance IQ showed significantly more difficulties with social functioning. Others have found that when the nonverbal IQ was higher than the verbal Downloaded by [University of Birmingham] at 12:47 19 September 2013 594 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER IQ more social difficulties were present (Joseph, Tager-Flusberg, & Lord, 2002). In the current study a discrepancy between verbal and performance IQ in children with AS was also found with higher verbal scores related to fewer social difficulties. A future study that evaluated children with NLD may evaluate whether less discrepant measures of ability are related to better outcomes or severity of the disorder. Academic findings were also similar to previous studies in that none of the children demonstrated a reading disability. Given that mathematics calculation skills were part of the inclusionary criteria for our NLD group, it was not surprising that our NLD group scored more poorly on this subtest (Drummond, Ahmad, & Rourke, 2005; Rourke, Ahmad, Collins, Hayman-Abello, & Warriner, 2002). This finding was also present for the mathematics reasoning subtest and is consistent with previous research studies (Pelletier et al., 2001; Strang & Rourke, 1985). Findings from the measure of fluid reasoning indicated that the control group scored better than all of the clinical groups. Of more interest was the finding that both the NLD and AS groups performed significantly more poorly compared to the ADHD groups and did not differ from each other on this measure. Behavioral difficulties are often present for children with NLD or AS when they are faced with a novel situation. It may well be that the deficit in fluid reasoning compromises their already limited ability to function in unfamiliar or complex situations. Previous studies have suggested difficulties in concept-formation and novel problem-solving skills (Rourke & Tsatsanis, 2000). Other researchers have begun to suggest that the difficulty some children with NLD have in social functioning is due to problems with executive functioning (Forrest, 2007). Some studies have found that children with ASD may show good to excellent abilities on a measure of matrix reasoning (Dawson, Soulieres, Gernsbacher, & Mottron, 2007; Hayashi, Kato, Igarashi, & Kashima, 2008). The Raven’s Standard Progressive Matrices Test (Raven, Raven, & Court, 1993) requires the child to solve geometric designs by supplying the missing element by choosing one of 6 to 8 alternatives that best match the design. This test differs from the WJ-Cog III measures utilized in the current study. The fluid reasoning portion of the WJ-Cog III requires not only solving of geometric designs but also the use of categorical reasoning, inductive and deductive logic, and the ability to shift set (Strauss, Sherman, & Spreen, 2006). In contrast the Raven’s has been found to be a unidimensional estimate of reasoning ability (Raven, Raven, & Court, 2000). The relation of the WJ-Cog III fluid reasoning test to social functioning is likely stronger than that found for the Raven’s because of the multidimensional nature of social reasoning. Our findings of difficulty with fluid reasoning for both NLD and AS groups support the suggestion that these difficulties complicate the child’s ability to solve novel, visually complex problems. These difficulties may contribute to problems with perspective-taking as well as with the ability to adapt to changing environmental demands. Children with ADHD were not found to have significant difficulties on this task. This finding suggests that problems encoding visual stimuli for children with AS and NLD contributes to social problems while for children with ADHD social difficulties may not be due to inaccurate perception but rather to impulsivity and inattention (Fine et al., 2008). Further study is necessary to untangle the relation of executive functioning and attention to social competence. Denckla (2000) suggests that there is a “cognitive overlap zone” of executive functions in NLD and ADHD due to overlapping neural regions. Neuroimaging provides some support for this theory. Structural and functional magnetic resonance imaging (fMRI) studies have found differences in right hemispheric frontal and striatal networks as well as in white matter structures (i.e., corpus callosum) in children with ADHD (Castellanos et al., 1994; Castellanos et al., 1996; Giedd et al., Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 595 1994; Hynd et al., 1993; Semrud-Clikeman et al., 2000). Similarly, Rourke (1995) suggested that difficulty was present in the right-hemispheric white matter in NLD. Differences have also been found in the smaller volume of the corpus callosum for children with AS despite control for white matter volume (Chung, Dalton, Alexander, & Davidson, 2004), higher volumes of white matter (Filipek, 1999), and increased volume in the caudate regions (Sears et al., 1999). While the emerging MRI research in AS suggests white matter involvement in the disorder, the findings are not conclusive. Prospective research in imaging for children with NLD has not been published but findings from existing neurological cases does suggest involvement of the right hemisphere and possibly of white matter (Voeller, 1995). Further study is needed to determine the validity of the right hemispheric white matter hypothesis in NLD. Visual-spatial differences. The NLD group showed significantly more difficulty compared to the other groups on the Rey-Osterreith Complex Figure test. Impairment on this test is thought to reflect problems with planning, organization, and visual-spatial reasoning as well as visual-motor skills. These findings are consistent with previous studies for children with NLD (Wilkinson & Semrud-Clikeman, 2008; Woods, Weinborn, Ball, Tiller-Nevin, & Pickett, 2000; Worling, Humphries, & Tannock, 1999). For the children with AS no significant differences were found compared to the other three groups. This finding is consistent with that of Edgin and Pennington (2005) who found few problems in spatial cognition in children with AS while others have found problems with visual organization (Kenworthy et al., 2005). These findings indicated that copying a complex figure may be an area of specific difficulty for children with NLD. Reviewing the individual scores supports this hypothesis to some extent. In the NLD sample 63% showed scores in the below average range while for the AS sample 39% scored in the below average range. Similarly the JLO, a measure of spatial reasoning without a motor component, was found to differ among the groups. The NLD group scored more poorly compared to the other groups. Children with AS were found to show, as a group, average to above average performance on the JLO (79% of the sample scored within the average to above average range). These visual-spatial measures were among the few that differentiated children with NLD from those with AS. Motor. The literature suggests that a right hemispheric deficit is present in children with NLD and as such more difficulty would be seen with the left hand than the right hand measures. It has also been hypothesized that children with NLD show bilateral difficulties in fine motor skills (Rourke, 1995). We found only partial support for this hypothesis. While our findings indicated that the NLD and AS groups performed more poorly on a measure of complex fine motor functioning compared to controls with the left hand and bilaterally for the NLD group, these measures did not differ significantly from the scores obtained by the ADHD groups and as such may not be specific to AS or NLD. Limitations of the Study There are several limitations to this study. One limitation was the lower number of children with a diagnosis of NLD. It required several years to find sufficient numbers of children who met criteria for NLD who did not also meet criteria for AS. The sample for this study did not include children with genetic or other disorders that have been associated with NLD (velocardiofacial syndrome, Williams syndrome) and these results may not be generalizable to groups of children with medical Downloaded by [University of Birmingham] at 12:47 19 September 2013 596 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER and/or genetic disorders. An additional issue is the possible confound between the visual fluid reasoning tests of the WJ-Cog III and the visual-perceptual difficulties found in the children with NLD and many of those with a diagnosis of AS. These results should be interpreted in light of these problems and our findings are consistent with previous research, also using visual tasks that find problems with concept formation and executive functioning (Fisher, DeLuca, & Rourke, 1997; Sikora, Haley, Edwards, & Butler, 2002) Another limitation of the study was that we were not able to obtain the scores from the ADOS or ADI–R. These measures were obtained in a private clinic setting with the results were not available to our study. In the future selection of subjects using these measures would provide for better diagnostics and the ability to evaluate performance based on number of symptoms reported on the ADI–R. Finally, our sample of children with NLD did show significant difficulties on the estimated performance test from the WASI. It was elected not to use covariate procedures to control for this group difference. There are several articles that question the use of covariate procedures to equate groups (Adams, Brown, & Grant, 1985; Miller & Chapman, 2001) while others suggest that ANCOVAs are appropriate when evaluating treatment decisions (van Breukelen, 2006). In the case of this study there were no differences in verbal estimated IQ—one of the selection criteria. We elected not to covary for Full Scale estimated IQ which did significantly differ among the groups due to the group differences on performance estimated IQ given the concerns voiced in these various articles. Conclusion Taken together, these findings indicate that the theoretical model suggested by Rourke (1988) provides a backdrop for our understanding of NLD. The performance deficits seen on the motor tasks also suggest bilateral involvement of the brain with the NLD group scoring more poorly on both right and left hands compared to the other groups. In contrast the AS group only showed differences with the LH. These findings do suggest difficulties in motor coordination for the NLD and AS groups with poorer performance present for the right hemisphere than for the left. Some have suggested that children with NLD may appear to be clumsy and uncoordinated (Rourke, 1988), while others have found a wide variation in bimanual motor coordination in children with AS (Gunter et al., 2002). Our study suggests that there is a wide variation in these skills for both groups and problems with coordination may not be an area specifically different for children with NLD (Wilkinson & Semrud-Clikeman, 2008). Findings of differences in visual-spatial skills were strongly present for children with NLD even when motor disability was not present. The finding of differences in visual-spatial skills and performance abilities implicate the posterior regions of the brain. These difficulties, however, were present only for the NLD group. No difference was found among the AS, ADHD, or control groups on visual-spatial ability. This finding suggests that there may be differences between the NLD and AS groups in these areas; an issue that has been the subject of debate in the literature. It may well be that the discriminating difference between NLD and AS is in visual-spatial ability, thus it is strongly recommended that these measures to be included in the neuropsychological battery when evaluating these children. A comparison between children with NLD and those diagnosed with pervasive developmental disorder, not otherwise specified (PDD-NOS) has not been conducted to determine what commonality may be present. One issue with such a comparison is Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 597 the lack of definition for the diagnosis of PDD-NOS; basically this diagnosis is provided when the child does not meet criteria for any other diagnosis in the autistic spectrum but has significant social difficulty. The difference between verbal and performance abilities was found specifically for children with NLD even though the selection criteria had not required such a split. These findings support clinical reports of larger than expected Verbal-Performance IQ splits in children with NLD. It is important to note that a sizable minority of children with AS also showed such a split; thus, the split alone is not sufficient for discriminating between NLD and AS for diagnostic purposes. With larger numbers in our study these findings may have been more robust. It is difficult, however, to recruit sufficient numbers of well-diagnosed NLD children as it required 7 years of recruiting to obtain our sample size in a large metropolitan region. While attention is an important issue for children with AS or NLD, it was not strongly related to our measures. One of the issues for our study was attempting to control for attentional problems frequently found in children with AS or NLD for which we utilized ADHD–C and ADHD–PI groups. In the future, other studies may wish to contrast children with AS and comorbid ADHD symptoms, those with AS without ADHD symptomatology, as well as that combination for children with NLD. We cannot rule out that attentional issues may have played a role in some of our findings. REFERENCES Adams, K. M., Brown, G. G., & Grant, I. (1985). Analysis of covariance as a remedy for demographic mismatch of research subject groups: Some sobering simulations. Journal of Clinical and Experimental Neuropsychology, 7, 445–464. American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. Beery, K. E., Buktenica, N. A., & Beery, N. A. (2006). Developmental Test of Visual-Motor Integration-5. San Antonio: Pearson. Benton, A. L., Sivan, A. B., Hamsher, K., Varney, N. R., & Spreen, O. (2004). Contributions to neuropsychological assessment: A clinical manual (2nd ed.). New York: Oxford University Press. Black, D. O., Wallace, G. L., Sokoloff, J. L., & Kenworthy, L. (2009). Brief report: IQ split predicts social symptoms and communication abilities in high-functioning children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 1613–1619. Castellanos, F. X., Giedd, J. N., Eckburg, W. L., Marsh, A. C., Kaysen, D., Hamburger, S. D., et al. (1994). Quantitative morphology of the caudate nucleus in attention deficit hyperactivity disorder. American Journal of Psychiatry, 151(1212), 1791–1796. Castellanos, F. X., Giedd, J. N., Marsh, W. L., Hamburger, S. D., Vaiturzis, A. C., & Dickstein, D. P. (1996). Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Archives of General Psychiatry, 53(7), 607–616. Chung, M. K., Dalton, K. M., Alexander, A. L., & Davidson, R. J. (2004). Less white matter concentration in autism: 2D voxel-based morphometry. NeuroImage, 23(1), 242–251. Corbett, B. A., & Constantine, L. J. (2006). Autism and Attention Deficit Hyperactivity Disorder: Assessing attention and response control with the integrated visual and auditory continuous performance test. Child Neuropsychology, 12, 335–348. Corwin, J., & Bylsma, F. W. (1993). The Clinical Neuropsychologist, 7(9–15). Dawson, M., Soulieres, I., Gernsbacher, M. A., & Mottron, L. (2007). The level and nature of autistic intelligence. Psychological Science, 18, 657–662. Denckla, M. B. (2000). Learning disabilities and attention-deficit/hyperactivity disorder in adults: Overlap with executive dysfunction. In T. E. Brown (Ed.), Attention-deficit disorders and comorbidities in children, adolescents, and adults (pp. 297–318). Washington, DC: American Psychiatric Press, Inc. Downloaded by [University of Birmingham] at 12:47 19 September 2013 598 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER Drummond, C. R., Ahmad, S. A., & Rourke, B. P. (2005). Rules for the classification of younger children with nonverbal learning disabilities and basic phonological processing disabilities. Archives of Clinical Neuropsychology, 20, 171–182. Edgin, J. O., & Pennington, B. F. (2005). Spatial cognition in Autism Spectrum Disorders: Superior, impaired, or just intact? Journal of Autism and Developmental Disorders, 35, 729–745. Filipek, P. A. (1999). Neuroimaging in the developmental disorders: The state of the science. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 40(1), 113–128. Fine, J. G., Semrud-Clikeman, M., Butcher, B., & Walkowiak, J. (2008). Brief report: Attention effect on a measure of social perception Journal of Autism and Developmental Disorders, 38, 1797–1802. Fisher, N. J., DeLuca, J. W., & Rourke, B. P. (1997). Wisconsin Card Sorting Test and Halstead Category Test performances of children and adolescents who exhibit the syndrome of Nonverbal Learning Disabilities. Child Neuropsychology, 3, 61–70. Forrest, B. (2007). Diagnosing and treating right hemisphere disorders. In S. J. Hunter & J. Donders (Eds.), Pediatric neuropsychological intervention (pp. 175–192). Cambridge, MA: Cambridge University Press. Gadow, K. D., DeVincent, C. J., & Pomeroy, J. (2006). ADHD symptom subtypes in children with pervasive developmental disorder. Journal of Autism and Developmental Disorders, 36(2), 271–283. Ghaziuddin, M., Weidmer-Mikhail, E., & Ghaziuddin, N. (1998). Comorbidity of Asperger syndrome: A preliminary report. Journal of Intellectual Disability Research, 42(4), 279–283. Giedd, J. N., Castellanos, F. X., Casey, B. J., Kozuch, P., King, A. C., Hamburger, S. D., et al. (1994). Quantitative morphology of the corpus callosum in attention deficit hyperactivity disorder. American Journal of Psychiatry, 151(5), 665–669. Gillberg, C., & Billstedt, E. (2000). Autism and Asperger syndrome: Coexistence with other clinical disorders. Acta Psychiatrica Scandinavica, 102(5), 321–330. Gresham, F. M., & Elliott, S. N. (1990). Social Skills Rating System. Circle Pines, MN: American Guidance Service, Inc. Guli, L. A., Wilkinson, A., & Semrud-Clikeman, M. (2008). Social Competence Intervention Program. Champaign, IL: Research Press. Gunter, H. L., Ghaziuddin, M., & Ellis, H. (2002). Asperger syndrome: Tests of right hemisphere functioning and interhemispheric communication. Journal of Autism and Developmental Disorders, 32(4), 263–281. Hayashi, M., Kato, M., Igarashi, K., & Kashima, H. (2008). Superior fluid intelligence in children with Asperger’s disorder. Brain and Cognition, 66, 306–310. Hynd, G. W., Hern, K. L., Novey, E. S., Eliopulos, D., Marshall, R., Gonzalez, J. J., et al. (1993). Attention deficit-hyperactivity disorder and asymmetry of the caudate nucleus. Journal of Child Neurology, 8(4), 339–340. Johnson, D. J., & Myklebust, H. R. (1967). Learning disablities: Educational principles and practices. New York: Grune & Stratton. Joseph, R. M., Tager-Flusberg, H., & Lord, C. (2002). Cognitive profiles and social-communicative functioning in children with autism spectrum disorder. Journal of Child Psychology and Psychiatry, 46, 807–821. Kenworthy, L. E., Black, D. O., Wallace, G. L., Ahluvalia, T., Wagner, A. E., & Sirian, L. M. (2005). Disorganization: The forgotten executive dysfunction in High-Functioning Autism (HFA) Spectrum Disorders. Developmental Neuropsychology, 28, 809–827. Klin, A., Sparrow, S. S., Cicchetti, D. V., & Rourke, B. P. (1995). Validity and neuropsychological characterization of Asperger syndrome: Convergence with nonverbal Learning Disabilities syndrome. Journal of Child Psychology and Psychiatry, 36(1127–1140). Klove, H. (1963). Clinical neuropsychology. In F. M. Forster (Ed.), The medical clinics of North America (pp. 1647–1658). New York: Saunders. Le Couteur, A., Lord, C., & Rutter, M. (2003). Autism Diagnostic Interview-Revised. Los Angeles, CA: Western Psychological Services. Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with Autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, V36(7), 849–861. Lezak, M. D., Howieson, D. B., & Loring, D. W. (2004). Neuropsychological assessment (Fourth ed.). New York: Oxford University Press. Lord, C., Rutter, M., DiLavore, P. C., & Risi, S. (1999). Autism Diagnostic Observation Schedule. Los Angeles, CA: Western Psychological Services. Miller, G. M., & Chapman, J. P. (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110, 40–48. Downloaded by [University of Birmingham] at 12:47 19 September 2013 NEUROPSYCHOLOGICAL DIFFERENCES 599 Nigg, J. T., Blaskey, L. G., Huang-Pollock, C. L., & Rappley, M. D. (2002). Neuropsychological executive functions and DSM-IV ADHD subtypes. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 59–66. Nyden, A., Gillberg, C., Hjelmquist, E., & Heiman, M. (1999). Executive function/attention deficits in boys with Asperger syndrome, attention disorder and reading/writing disorder. Autism, 3(3), 213–228. Osterreith, P. A. (1944). Le test de copie d’une figure complexe. Archives de Psychologie, 30(206), 356. Ozonoff, S., & Griffith, E. M. (2000). Neuropsychological function and the external validity of Asperger syndrome. In A. Klin, F. R. Volkmar, & S. S. Sparrow (Eds.), Asperger syndrome (pp. 72–96). New York: Guilford Press. Pelletier, P. M., Ahmad, S. A., & Rourke, B. P. (2001). Classification rules for basic phonological processing disabilities and nonverbal learning disabilities: Formulation and external validity. Child Neuropsychology, 7(2), 84–98. Pennington, B. F. (1991). Diagnosing learning disorders: A neuropsychological framework. New York: The Guilford Press. Pennington, B. F. (2008). Diagnosing learning disorders: A neuropsychological framework (2nd ed.). New York: Guilford. Psychological Corporation. (1999). Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Harcourt Assessment, Inc. Puig-Antich, J., & Chambers, W. J. (1978). The Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS). New York: New York Psychiatric Press. Raven, J., Raven, J. C., & Court, J. H. (1993). Raven manual: Section 1: General overview. Oxford, England: Psychologists Press. Raven, J., Raven, J. C., & Court, J. H. (2000). Raven manual research supplement 3: American norms, neuropsychological applications. Oxford, England: Oxford Psychologists Press, Ltd. Reddon, J. R., Gill, D. M., Gauk, S. E., & Maerz, M. D. (1988). Purdue pegboard: Test-retest estimates. Perceptual and Motor Skills, 66, 503–506. Reitan, R. M., & Wolfson, D. (1985). The Halstead-Reitan Neuropsychological Test Battery: Theory and Interpretation. Tucson, AZ: Neuropsychology Press. Reynolds, C. R., & Kamphaus, R. W. (2004). Behavior Assessment System for Children-2. Circle Pines, MN: Pearson Assessments. Rourke, B. P. (1988). The syndrome of nonverbal learning disabilities: Developmental manifestations in neurological disease and dysfunction. The Clinical Neuropsychologist, 4, 293–330. Rourke, B. P. (1989). Nonverbal learning disabilities: The syndrome and the model. New York: Guilford Press. Rourke, B. P. (1995). The NLD syndrome and the white matter model. In B. P. Rourke (Ed.), Syndrome of nonverbal learning disabilities: Neurodevelopmental manifestations (pp. 1–26). New York: Guilford Press. Rourke, B. P. (2000). Neuropsychological and psychosocial subtyping: A review of investigations within the University of Windsor laboratory. Canadian Psychology, 41(1), 34–51. Rourke, B. P., Ahmad, S. A., Collins, D. W., Hayman-Abello, B. A., & Warriner, E. M. (2002). Child clinical/pediatric neuropsychology: Some recent advances. Review of Psychology, 53, 309–339. Rourke, B. P., & Tsatsanis, K. D. (1996). Syndrome of nonverbal learning disabilities: Psycholinguistic assets and deficits. Topics in Language Disorders, 16(2), 30–44. Rourke, B. P., & Tsatsanis, K. D. (2000). Nonverbal learning disabilities. In A. Klin, F. R. Volkmar, & S. S. Sparrow (Eds.), Asperger syndrome (pp. 231–253). New York: The Guilford Press. Sears, L. L., Vest, C., Mohamed, S., Bailey, J., Ranson, B. J., & Piven, J. (1999). An MRI study of the basal ganglia in autism. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 23, 613–624. Semrud-Clikeman, M. (2003). Executive functions and social communication disorders. Perspectives, 29, 20–22. Semrud-Clikeman, M. (2007). Social competence in children. New York: Springer. Semrud-Clikeman, M., & Glass, K. L. (2008). Comprehension of humor in children with Nonverbal Learning Disabilities, Verbal Learning Disabilities and without Learning Disabilities. Annals of Dyslexia, 58, 163–180. Semrud-Clikeman, M., Steingard, R., Filipek, P. A., Bekken, K., Biederman, J., & Renshaw, P. F. (2000). Neuroanatomical-neuropsychological correlates of ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 477–484. Sikora, D. M., Haley, P., Edwards, J., & Butler, R. W. (2002). Tower of London test performance in children with poor arithmetic skills. Developmental Neuropsychology, 21, 243–254. Strang, J. D., & Rourke, B. P. (1985). Arithmetic disability subtypes: The neruopsychological significant of specific arithmetical impairment in childhood. In B. P. Rourke (Ed.), Neuropsychology of learning disabilities: Essentials of subtype analysis (pp. 167–183). New York: Guilford Press. Downloaded by [University of Birmingham] at 12:47 19 September 2013 600 SEMRUD-CLIKEMAN, WALKOWIAK, WILKINSON, CHRISTOPHER Strauss, E., Sherman, E. M. S., & Spreen, O. (2006). A compendium of neuropsychological tests (Third ed.). New York: Oxford University Press. Tiffin, J. (1968). Purdue Pegboard: Examiner Manual. Chicago: Science Research Associates. van Breukelen, G. J. P. (2006). ANCOVA versus change from baseline had more power in randomized studies and more bias in nonrandomized studies. Journal of Clinical Epidemiology, 59, 920–925. Voeller, K. K. (1995). Clinical neurological aspects of the right hemisphere deficit syndrome. Journal of Child Neurology, 10, 16–22. Wilkinson, A., & Semrud-Clikeman, M. (2008). Motor speed in children and adolescents with nonverbal learning disabilities. Paper presented at the International Neuropsychological Society, February 2008, Waikoloa, HI. Woodcock, R. W., McGrew, K. S., & Mather, N. (2001a). Woodcock-Johnson III Test of Cognitive Abilities. Rolling Meadows, IL: Riverside Publishing. Woodcock, R. W., McGrew, K. S., & Mather, N. (2001b). Woodcock-Johnson III Tests of Achievement. Itasca, IL: Riverside. Woods, S. P., Weinborn, M., Ball, J. D., Tiller-Nevin, S., & Pickett, T. C. (2000). Periventricular leukomalacia (PVL): An identical twin case study illustration of white matter dysfunction and nonverbal learning disability (NLD). Child Neuropsychology, 6, 274–285. Worling, D. E., Humphries, T., & Tannock, R. (1999). Spatial and emotional aspects of language influencing in nonverbal learning disabilities. Brain and Language, 70, 220–239.