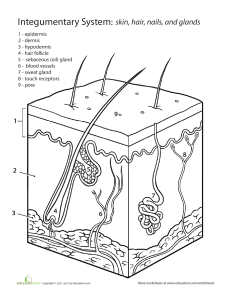
UNIT II: THE INTEGUMENTARY SYSTEM - LAB OUTLINE I. II. III. IV. V. VI. VII. VIII. OVERVIEW ANATOMY OF THE SKIN, HAIR, AND NAILS THE SKIN A. Epidermis: 4 or 5 Layers 1. Layers of Cells in the Epidermis 2. Thick and Thin Skin 3. Cells of the Epidermis B. Dermis 1. Two Tissue Layers 2. Subcutaneous Tissue 3. Fibers 4. Nutrition 5. Nerve Endings GLANDS A. Major Glands of the Skin 1. Types of Sweat Glands 2. Other Glands HAIR A. Hair Structure 1. Hair Follicle B. Three Types of Hair C. Hair Color and Texture D. Hair Growth 1. Hair Growth Follicle NAILS PHYSIOLOGY OF THE INTEGUMENTARY SYSTEM A. Functions of the Skin B. Injuries to the Skin C. Diagnostic Tests used to Diagnose Integumentary System Disorders D. Integumentary System Disorders 1. Disorders ADDITIONAL REPRESENTATIVE DISEASES AND DISORDERS OF THE INTEGUMENTARY SYSTEM ● damage from abrasion on the skin’s surface ■ reduces water loss through the skin ○ Deep layer: dermis ■ Loose/areolar connective tissue over dense irregular connective tissue ■ responsible for most of the strength of the skin The hypodermis is adipose connective tissue; it is not part of the skin, but it attaches the skin to the body (muscle or bone) ○ Subcutaneous tissue, a layer of loose connective tissue THE SKIN ● ● ● ● ● ● ● In the adult human body, the skin makes up about 16% of the body weight and covers an area of 1.5-2m2. Largest organ system in the human body. Protects the inner organ, in need of daily care and protection to maintain its health. The skin’s primary role is to help protect the rest of the body’s tissues and organs from physical damage (such as abrasions), chemical damage (such as detergent), and biological (such as microorganism). Cutaneous membrane - Is the technical term for the skin. Made up of 3 general layers: ● Epidermis ○ Contains cells that produce pigment and protect immune system ● Dermis ○ Contains nerve endings oil and sweat glands, and hair follicles ● Subcutaneous layer/hypodermis ○ Made up of fat, connective tissue and larger blood vessels Accessory structures: ● Hair ● Gland ● Nails OVERVIEW ● ● The integumentary system is composed of the skin, hair, nails, and cutaneous glands. its appearance can also indicate physiological imbalances not just for vanity’s sake ANATOMY OF THE SKIN, HAIR, AND NAILS ● The skin is the largest organ of the body. ● It is composed of two layers: ○ Superficial layer: epidermis ■ Stratified squamous epithelial tissue ■ multiple cell layers of the epidermis protects against the potential Fig. Skin anatomy Page 1 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB EPIDERMIS: 4 OR 5 LAYERS ● ● ● ● Stratified squamous epithelium (multiple layers of cube-shaped cells in the basal layer and progressively flattened toward the surface). ○ Though the epidermis is stratified, it is not as thick as the dermis. ○ The Epithelium can be non-keratinized (moist) or keratinized. ■ Non-keratinized - the surface cells retain new clues and are attached to the cytoplasm. ■ Keratinized - the cytoplasm at the surface is replaced by a protein called “keratin”, and the cells are dead. It is separated from the underlying dermis by the basement of the membrane. ● Called “keratinocytes” ● It makes cells durable. It is the durability of the keratinocytes that gives the epidermis its ability to resist abrasion and reduce water loss. Other cells in epidermis: melanocytes, Langerhans cells, and Merkel cells ○ Melanocytes produce the pigment melanin, which contributes to skin color. ○ Langerhans cells are part of the immune system. ○ Merkel cells are specialized epidermal cells associated with the nerve endings responsible for detecting light touch and superficial pressure. Contains no blood vessels ○ The living cells of the dermis receive nutrients and excrete waste products by the diffusion of the substances between the epidermis and the capillaries of the dermis. 4-5 strata (regions) (stratum: singular) ○ The number of strata of the skin varies depending on the location in the body. Fig. Layers of the epidermis LAYERS OF CELLS IN THE EPIDERMIS Stratum basale/germinativum ● simple cuboidal epithelial tissue. ● The deepest stratum of the epidermis ● A single layer of simple cuboidal or columnar epithelial cells. ○ Actively divides to make new epidermis ○ Deepest layer of the epidermis ● So cells have structures that hold them to on another or to the basement membrane by hemidesmosomes; while desmosomes hold the keratinocytes together ○ The connections formed by the hemidesmosomes and desmosomes provide structural strength to the epidermis. ○ Keratinocytes are strengthened internally by keratin fibers (intermediate filaments) that insert into the desmosomes ● Functions: ○ Mechanically bind the cells together. ○ Help form a permeability barrier. ○ Provide a mechanism for intercellular communications. ● Keratinocyte stem cells of the stratum basale undergo mitotic divisions approximately every 19 days. ○ One (1) daughter cell remains a stem cell in the stratum basale and divides again. ○ But other daughter cells are pushed toward the surface and become keratinized. ○ It takes approximately 50-56 days for the cell to reach the epidermal surface and will cast off. Page 2 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB Stratum spinosum ● superficial to the basale ● Consists of 8-10 layers of many-sided cells ○ The cells of this stratum are pushed to the surface, they flatten, then the desmosomes break apart and new desmosomes are formed. This particular desmosome is an epithelial cell that has cell surface glycoprotein which attaches to other glycoproteins located on adjacent cells and on the basement membrane. Among these glycoprotein connections between cells, there are some relatively strong adhesive structures called “desmosomes”. ○ Desmosomes - consist of adhesive glycoproteins that bind cells together and intracellular proteins attached to the immediate filaments that extend in the cytoplasm of the cells. Many desmosomes are found in the epithelial tissues that are subjected to stress such as of the stratified squamous epithelium of the skin. They hold the keratinocytes together. ○ Hemidesmosome - similar to the one-half of the desmosomes attached to the epithelial cells to the basement membrane. During this preparation for microscopic observation, the cells usually shrink from one another except where they are attached by desmosomes causing the cells to appear spiny, hence the name Stratum Spinosum. ● During preparation for microscopic observation, the cells usually shrink from one another, except where they are attached by desmosomes, causing the cells to appear spiny—hence the name stratum spinosum. ● As keratinocytes progressed through this stratum additional keratin fiber and lipid defiled membrane-bound organelles known as the Lamellar bodies formed inside the cells. Stratum granulosum ● Consists of 2-5 layers of somewhat flattened, diamond-shaped cells. ● The long access of these cells is oriented parallel to the surface of the skin. ● So this stratum derived its name from the presence of protein granules of Keratohyalin which accumulate in the cytoplasm of the keratinocytes. The lamellar bodies which formed as the cells pass through the stratum Spinosum move to the plasma membrane, and release their lipid contents into the extracellular space. ● Inside the keratinocyte, a protein envelope formed beneath the plasma membrane. So in the most superficial layers of the stratum granulosum, the new clues and other organelles degenerate and the keratinocytes die. Unlike other organelles, the keratin fibers and keratohyalin granules within the cytoplasms do not degenerate. Stratum lucidum ● Found only in thick skin ● Is a thin, clear zone above the stratum granulosum, found only in thick skin ● Consists of several layers of dead keratinocytes with indistinct boundaries. ○ so the keratin fibers are present but the keratohyalin which was evident has dispersed around the keratin fiber and the cells appear somewhat transparent. ● The stratum lucidum is present only in a few areas of the body. Page 3 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB THICK AND THIN SKIN ● Stratum corneum ● composed of dead, keratin-filled cells that flake off (exfoliate) ● The last and most superficial stratum of the epidermis is the stratum corneum. ● Composed of 25 or more layers of dead overlapping squamous cells joined by the desmosomes. ○ Eventually, the desmosomes break apart, and the cells are shed from the surface of the skin. ■ Excessive shedding of the stratum corneum of the scalp results in dandruff. ■ Skin cells are continually shed from other areas as others rub against the body or as the skin is washed. ● Consist of cornified cells which are dead keratinocytes with a hard protein envelope and filled with protein keratin ○ Keratin: mixture of keratin fibers and keratohyalin. ○ The envelope and keratin are responsible for the structural strength of the stratum corneum. ● The type of keratin found in that skin is soft keratin. ● Another type of keratin is hard keratin, which can be found in nails and the external part of the hair. ○ Cells containing hard keratin are more durable than cells with soft keratin, and they are not shed off. ● Lipids are released from the lamellar bodies surrounding the skin cells. ○ Lipids are responsible for many of the skin’s permeability characteristics. ● ● ● ● ● Skin is characterized as thick or thin based on the structure of the epidermis. THICK SKIN - has all 5 epithelial strata ○ Can be found in areas subject to the pressure of friction such as the palm of the hands, soles of the feet, and the fingertips. THIN SKIN - covers the rest of the body and is more flexible than the thick skin. The stratum lucidum is generally absent in the thin skin. ○ Each stratum in the thin skin contains fewer layers of cells than found in the thick skin. ○ Example: Stratum granulosum frequently consists of only 1 or 2 layers of cells, than the 3-5 layers of cells in thick skin. ○ Hair can only be found in thin skin. The entire skin (both the epidermis and dermis) varies in thickness from 0.5 mm on eyelids to 5mm on the back of the shoulders. The term “thick and skin” only refers to the epidermis and should not be used when total skin thickness is considered. ○ It is actually the variation in the thickness of the dermis that accounts for most of the difference in total thickness. ■ For example, the skin of the back is thin, whereas that of the palm of the hand is thick skin. However, because the dermis of the skin of the back is greater than that of the palm. If the skin is subjected to friction or pressure, an area called “Calluses” often forms when the stratum corneum of the epidermis increases in thickness. ○ The increased number of cell layers provides added protection to the area that experiences more mechanical stress. The skin over bony prominences developed a cone-shaped structure called a “corn”. The base of the corn is at the surface, but the apex extends deep on the epidermis, and the pressure on the acorn may be painful. ○ Calluses and corns can be developed in thin and thick skin. Page 4 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ● soles of the feet, contain less melanin ○ To produce melanin, the enzyme tyrosinase converts the amino acid tyrosine to dopaquinone. ■ Dopaquinone can be converted to a variety of related molecules, most of which are brown to black pigments but some of which are yellowish or reddish Tactile Cells ○ ○ CELLS OF THE EPIDERMIS ● ● Keratinocytes ○ KERATINIZATION: As keratinocytes move from the deeper epidermal layers to the surface, the cells change shape and chemical composition ■ the cells eventually die and produce an outer layer of dead, hard cells that resists abrasion and forms a permeability barrier ■ IMPORTANCE: determining skin disease which result from malfunction ○ Make up the majority of epidermal cells ○ Grow and divide pushing the older cells up toward the surface ○ Produce and fill themselves with keratin (a hard, waterproof protein) as they move toward the surface ○ Stratum corneum contains the keratinocytes that have completely filled with keratin and died ○ This process is called cornification. Melanocytes ○ irregularly shaped cells with many long processes that extend between the keratinocytes of the stratum basale and the stratum spinosum ■ Cells stay in the stratum basale ○ Produce skin pigments called melanin. ■ provides protection against ultraviolet light from the sun ■ MELANIN PRODUCTION: determined by genetic factors (primarily responsible for the variations in skin color among different races and among people of the same race), exposure to light, and hormones ○ NOTE that the number of melanocytes in the skin is relatively the same for all humans, regardless of race. ○ Keratinocytes take in melanin-filled vesicles called melanosomes by endocytosis ○ Melanocytes may not be evenly distributed across the skin, and denser patches of these cells account for freckles and moles ■ Large amounts of melanin are found in certain regions of the skin, such as freckles, moles, the nipples, the areolae of the breasts, the axillae, and the genitalia ■ Other areas of the body, such as the lips, palms of the hands, and ● Receptors for fine touch Found in the stratum basale associated with nerve cells in the underlying dermis Dendritic Cells ○ Immune system cells found in the stratum spinosum and the stratum granulosum ○ Alert the body’s immune system to the invasion of pathogens Fig. Melanin concentration visual difference Fig. Epidermis cells visual DERMIS ● ● Referred to as "true skin." Connective tissue Page 5 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ● ● ● ● The dermis contains: ○ Fibers ■ Collagen: main type of protein fiber of the extracellular matrix, but elastic and reticular fibers ○ Nerve endings (varied in structure and function) ■ (1) free nerve endings for pain, itch, tickle, and temperature sensations ■ (2) hair follicle receptors for light touch ■ (3) Pacinian corpuscles for deep pressure ■ (4) Meissner corpuscles for detecting simultaneous stimulation at two points on the skin ■ (5) Ruffini end organs for sensing continuous touch or pressure ○ Cutaneous glands ○ Hair follicles ○ papillae ○ Blood vessels ■ allow for nutrient and waste exchange to the cells of the dermis and the living cells of the epidermis Cells of the dermis: ○ Fibroblasts ○ a few adipocytes ○ Macrophages If the skin is overstretched, the dermis may rupture and leave lines that are visible through the epidermis ○ These lines of scar tissue, called stretch marks, can develop in the skin of individuals who have experienced rapid growth Composed of two tissue layers : ○ Superficial papillary TWO TISSUE LAYERS 1. Dermal Papillae ○ ○ ○ ○ ○ ○ 2. ○ Deeper reticular layer papillary layer derives its name from projections that extend toward the epidermis Cone-like projections of dermis that fit into recesses of epidermis Possess blood vessels, touch receptors Loose connective tissue with thin fibers that are somehow loosely arranged Contain blood vessels that: ■ supply the overlying epidermis with oxygen and nutrients ■ Remove waste products ■ aid in regulating body temperature Under the thick skin of the palm of the hands and sole of the feet lie in parallel curving ridges ■ Ridges shape the overlying epidermis into pattern called friction ridges ■ The impressions left on surfaces by this friction form fingerprints and footprints and this Improve grip of hands and feet ■ Everyone has unique friction ridge patterns, even identical twins. Reticular Layer ○ Main layer of dermis ■ Composed of dense irregular tissue connective tissue ○ Continuous with the subcutaneous tissue and forms a mat of irregularly arranged fibers that is resistant to stretching on many directions ○ The elastic and collagen fibers are oriented more in some directions than in others and produce cleavage lines, or tension lines, in the skin ■ important for health professionals to understand cleavage line directions because an incision made parallel to the cleavage lines is less likely to gap than an incision made across them ■ The development of infections and the formation of scar tissue are Page 6 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ○ ○ reduced in wounds where the edges are closer together. Intramuscular injections are used for injecting most vaccine and certain antibiotic Subcutaneous injection - insulin injection SUBCUTANEOUS TISSUE ● ● ● ● ● ● ● Sometimes called as hypodermis ○ Not part of the skin ○ Deep to the skin Attaches the skin to underlying bone and muscles and supplies the skin with blood vessels and nerves ○ Consists of loose connective tissue with collagen and elastic fibers Main type of cells within the subcutaneous tissue are: ○ fibroblasts, adipocytes, and macrophages Half of the body’s stored lipids are the subcutaneous tissues ○ Function in insulation and padding and as a source of energy Can be used to estimate total body fat by pinching the skin at selected locations and measuring the thickness of the skin fold and underlying subcutaneous tissue ○ The thicker the fold, the greater the amount of total body fat Amount of adipose tissue in the subcutaneous tissue varies with age, sex, and diet ○ responsible for some of the differences in body shape between individuals of the same sex ■ Children - more adipose “chubby baby”because they have proportionately more adipose tissue than adults ■ Adult male - less adipose than female ■ Adult female - more adipose than male; over thighs, buttocks & breast Types of Injections: ○ Intradermal injection - used for the tuberculin skin test, goes into the dermis. It is administered by drawing the skin taut and inserting a small needle at a shallow angle into the skin. ○ Subcutaneous injection - extends into the subcutaneous tissue; an insulin injection is one example. A subcutaneous injection is achieved by pinching the skin to form a “tent,” into which a short needle is inserted. ○ Intramuscular injection - reaches a muscle deep to the subcutaneous tissue. It is accomplished by inserting a long needle at a 90-degree angle to the skin. Intramuscular injections are used for injecting most vaccines and certain antibiotics. FIBERS ○ Composed of fibrous connective tissue made by fibroblasts ■ Collagen: strength and toughness ■ Elastic fibers: extensibility and elasticity NUTRITION ○ ○ ○ ○ ○ ○ Nutrition is one of the many factors required for the maintenance of overall skin health. Am impaired nutritional status alters the structural integrity and biological functions of skin resulting in an abnormal skin barrier and/or dry skin. The importance of micro nutrients such as certain vitamins and minerals for skin health has been highlighted in cell culture, animal and clinical studies. These micro nutrients are employed not only as active compounds in therapeutic agents for treating certain skin diseases but also as ingredients in cosmetic products. There are nutritional status dependent on both macro and micronutrients as vital for skin health. Proper nutritional intake compliments factors in regulating skin barrier function. Vitamin A and vitamin C are important for healthy skin because they are necessary for collagen production. Vitamin A ■ Green and yellow vegetables, dairy products, and liver Vitamin C ■ Fruits and green vegetables. ■ Calcium is responsible for the differentiation of keratinocytes as a major cell type in epidermis. Page 7 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB NERVE ENDINGS ○ ○ ○ ○ ● Estrogen and production. testosterone increase sebum Pressure, pain, warm, and cold receptors are in deeper parts of the dermis. Lamellated and tactile corpuscles are for pressure and touch. Free nerve endings are for pain. Receptor nerve endings may surround a hair follicle. Sweat Glands ● ● Also known as sudoriferous glands Two types: ○ ○ TYPE OF SWEAT GLANDS GLANDS MAJOR GLANDS OF THE SKIN ○ ○ Sebaceous glands produce sebum (oil) Sweat glands Sebaceous Glands ● Located in the dermis ● oil-producing ● simple or compound produce sebum ○ ● ● ● Apocrine sweat gland Eccrine/Merocrine sweat gland ● Eccrine/Merocrine sweat glands ○ Most common type of sweat gland ○ ○ ○ alveolar glands that SEBUM: oily, white substance rich in lipids which is associated during puberty where various hormones cause to produce lot of sebum and this contributes to oily skin ■ If a duct of sebaceous glands is clogged with sebum, a white heads result. If allowed to dry and oxidize, it will become darker forming a black head. ■ If the sebaceous glands are infected, it will result in a moderate/severe form of acne. ● Excess sebum can block or plug the ducts of the glands forming a comedo (pimple). The condition is called acne. ● Most common occurrence is during puberty when sex hormone levels rise. Classified as Holocrine glands ○ Because sebum is released by the lysis and death of secretory cells Empty sebum into hair follicles ○ release their secretions into the upper part of the hair follicles through a duct Functions to moisturize the skin and hair ○ secretion of sebum onto the hair and surrounding skin prevents drying and protects against some bacteria ○ ○ ○ ○ ○ Simple, coiled, tubular glands that open directly onto the surface of the skin through sweat pores. distributed over the majority of the areas of the body ■ most numerous in the palms of the hands and soles of the feet not found on the margin of the lips, the labia minora, and the tips of the penis and clitoris Secrete sweat onto skin surface directly Clear, watery perspiration Activated with increase in body temperature Functions to cool the body through evaporation Divided into two parts: ■ Deep coil portion (located in the dermis) ● Produces an isotonic fluid that is mostly water but also contains some salts (NaCl), and small amounts of ammonia, uric acid, urea, and lactic acid. ■ Duct (passes to the skin surface) ● Asthis fluid moves through the duct, sodium chloride moves by active transport from the duct back into the body thereby conserving salts. ● so the resulting hypo osmotic fluid that leaves the duct is called sweat. So when the body temperature starts to rise above normal the sweat glands produce sweat Page 8 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ● ● which evaporates and cools the body. (thermoregulation) sweat can also be released in the palms soles and axillary as a result of emotional stress. Apocrine sweat gland ○ ○ ○ ○ ○ ○ ○ ○ Simple, coiled, tubular glands that open into the hair follicle superficial to the opening of the sebaceous glands. Typically larger and more productive than eccrine glands Characterized by a simple cuboidal epithelium Secretion contains protein, lipid, carbohydrates, ammonium, and other organic compounds. ■ Contains 3 Methyl-2 hexanoic acid ● essentially odorless body odor due to bacterial decomposition when first released but are quickly metabolized by bacteria to cause body odor. ● Many mammals use scent as a means of communication Becomes active in puberty as a result of sex hormones ■ Physiology says that the activity of apocrine sweat glands may signal sex maturity. Empty secretion into hair follicle Located in axillary and genital regions (scrotum,labia majora, and around the anus) Milky sweat due to proteins and fats ● Mammary gland ○ ○ ○ ○ Modified apocrine sweat glands located in the breast (In breast tissue) normally only functional in lactating women ■ Produces milk (in female); ■ Nourishes an infant non functional form (in males) Regulated in the endocrine system and becomes functional in response to the hormonal changes associated in giving birth. OTHER GLANDS ● HAIR Ceruminous gland ○ ○ ○ Produce cerumen or earwax Found in external auditory canal ■ Keep foreign particles and insects out of auditory canal Modified eccrine sweat glands located in the ear canal. ■ Ear wax is composed of the combined secretions of ceruminous glands and sebaceous glands. ■ Cerumen and hair in the ear canal protect the tympanic membrane by preventing dirt and small insects from moving too deeply into the ear canal ● However, an accumulation of cerumen can block the ear canal and make hearing more difficult. ● ● ● presence of hair is one of the characteristics of all mammals ○ if the hair is dense and covers most of the body surface, it is called fur ○ In humans, hair is found everywhere on the skin except the palms, the soles, the lips, the nipples, parts of the external genitalia, and the distal segments of the fingers and toes. The three types of hair are lanugo, vellus, and terminal. A hair can be divided into three sections: the bulb, the root, and the shaft. HAIR STRUCTURE ● ● change as a person ages There are three layers to a hair : ○ the inner medulla - central acces of the hair. Consist of two or three layers of cells containing soft keratin ○ the cortex - cells constrain hard keratin., Surrounds medula. Contains the bulk of the hair. Covered by the cuticle Page 9 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ○ the cuticle- single layer of cells that constrain hard keratin. The Edges are overlapping. ○ ○ Keratinocytes: produce the hair and form the hair matrix Melanocytes: provide pigment for the hair HAIR FOLLICLE ● ● ● ● ● ● ● tube-like invaganiation of the epidermins that extends to the dermis Hair develops and grows with each hair follicle Consists of dermal root shift and epithelial root shifts ○ Dermal root shift is the portion of the dermis that surrounds the epithelial root shift. ○ The Epithelial root shift is divided into external and internal parts. ■ EXTERNAL: At the opening of the follicle, the external epithelial root shift, has all the starta found in the thin skin.The deeper in the hair follicle, the number of cells decreases until the hair bulb, only stratum basale is present. This arrangement of epidermal cells has important consequences for skin repair. So if the epidermis and superficial part dermis are damaged, the keratinocyte stem cells in the stratum basale of the undamaged part of the hair follicle can be the source of the hair epithelium ■ INTERNAL: has raised edges that mesh closely with the raised edges of the hair cuticle and this arrangement holds the hair in place. When a hair is pulled out, the internal epithelial root sheath usually comes out as well and is plainly visible as whitish tissue around the root of the hair. Contains the hair root Formed by the stratum basale Arrector pili muscle ○ Associated with each hair follicle are these smooth muscle cells ■ extend from the dermal root sheath of the hair follicle to the papillary layer of the dermis ○ The hair follicle and the hair inside it are at an oblique angle to the surface of the skin ○ Contracts and raises the hair in the follicle on end ■ PROCESS: When the arrector pili muscles contract, however, they pull the follicle into a more perpendicular position, causing the hair to “stand on end.” ■ Movement of the hair follicles produces raised areas which causes “goose bumps” ● common response to cold temperatures as well as strong emotional responses ○ Little value for human survival ■ But in other mammals, arrector pili muscle contractions are important for warmth as well as communication of aggression or fear The dermal papilla has a blood vessel, which feeds hair follicle cells: Fig. Hair Follicle Page 10 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB THREE TYPES OF HAIR ● Lanugo Hair ○ ○ ● ○ ○ ○ ○ Vellus hair is the body hair on most women and children Prepubertal stage At puberty, terminal hair esp in pubic and axillary region replaces much of the vellus hair Terminal Hair ○ Thick, coarse, and heavily pigmented, ○ ○ ○ ● ○ Vellus Hair ○ Unpigmented and very fine ○ replaces lanugo hair around the time of birth ○ ● ○ Very fine, delicate and unpigmented (colorless) type of hair seen in developing fetus ■ Forms on a fetus during the last three months of its development (By the fifth or sixth month of fetal development) Lanugo hair is usually replaced by birth forms the eyebrows, eyelashes, and hair on the scalp. Adult stage At puberty, terminal hair forms in the axillary and pubic regions of both sexes. It also forms on the face and possibly on the trunk and limbs of men. ■ These changes in hair type at puberty are universal and have biological significance ■ The beard, pubic, and axillary hair are visible signs of sexual maturity ● Pubic and axillary hair may function as wicks for dispersing odors produced by secretions from specialized glands in the pubic and axillary regions acting as olfactory signals to others. It also has been suggested that pubic hair protects against abrasion during intercourse and axillary hair reduces friction when the arms move against the body. Chest, leg and arm hair is approximately 90% terminal hair in male and 35% in female ■ In males, terminal hairs replace the vellus hairs of the face to form the beard All types of human hair can be divided into three sections (shown in Figure 3.9): ○ (1) The bulb is a thickening of the hair at the end of the hair follicle. ■ Base of the root is expanded to form hair bulb; an expanded knob at the base of the hair root ■ Inside the hair bulb is a mass of undifferentiated epithelial cells called the matrix. ● MATRIX: produces both the hair and the internal epithelial root sheath ● The dermis of the skin projects into the hair bulb as a hair papilla. Within the hair papilla are blood vessels that provide nourishment to the cells of the matrix. (2) The root extends from the bulb to the skin’s surface; located below the surface (3) The shaft is the section of the hair extending out from the skin’s surface. It protrudes above the surface of the skin. most of the root and the shaft are composed of column of dead keratinized epithelial layers arranged in three concentric layers: ■ (1) the medulla: central axis of the hair, and it consists of two or three layers of cells containing soft keratin ■ (2) the cortex: surrounds the medulla and forms the bulk of the hair. The cells of the cortex contain hard keratin ■ (3) the cuticle: covers the cortex, a single layer of cells also containing hard keratin. The edges of the cuticle cells overlap like shingles on a roof. HAIR COLOR AND TEXTURE ● ● ● Hair color is the result of the melanin production by the melanocytes and the distribution of melanin to the cells of the hair ○ Similar to how melanocytes of the epidermis produce melanin and pass it to the keratinocytes of the skin. ○ Melanocytes within the hair bulb matrix produce melanin and pass it to the keratinocytes in the hair cortex and medulla. The skin having varying amounts and types of melanin cost different shades of hair color. ○ The blonde hair has a little black brown melanin. ○ Jet black hair has the most intermediate amount of melanin accounting for the different shades of brown. ○ Red hair is caused by varying amounts of the red type of melanin. ○ Hair sometimes contains both black brown or red melanin. Hair color is controlled by several genes and dark hair color is not necessarily dominant over light. Page 11 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ● ● ■ With age the amount of melanin in hair can decrease causing hair color to fade or become white. ○ Gray hair is usually a mixture of faded and unfaded and white hair. The development of high resolution Digital microscopes allow researchers to obtain more accurate measurements of hair features. There are studies that have been done using a digital microscopy and to explore variants within the cortical texture color and density characteristics throughout hair strands. ○ Changes in your hair's thickness, texture and growth location (too little in some places, too much in others) can also occur. ● ● Regrowth of hair occurs in many individuals, but some experience permanent hair loss. ● the most common kind of permanent hair loss is “pattern baldness” wherein hair follicles shrink and revert to producing vellus hair, which is very short, transparent, and for practical purposes invisible. . Eventually, hair production in these smaller follicles may completely cease ● Baldness is more common and more pronounced in certain men, it can also occur in women. Genetic factors and the hormone testosterone are involved in causing pattern baldness. The length of each stage depends on the hair: ○ EYELASHES: grow for approximately 30 days and rest for 105 days ○ SCALP HAIR: grow for 3 years and rest for 1–2 years Maximum hair length is determined by the rate of hair growth and the length of the growing phase ○ scalp hair can become very long ○ eyelashes stay short HAIR GROWTH CYCLE ● HAIR GROWTH ● ● Hair goes through a growing stage and a resting stage, and then it falls out. Not all of the hairs on the head cycle are on the same schedule. ○ Each hair grows about a half inch per month, and its growth stage lasts for approximately three years ○ average rate of hair growth is approximately 0.3 mm per day ■ Cutting, shaving, or plucking hair does not alter the growth rate or the character of the hair ● But hair can feel coarse and bristly shortly after shaving because the short hairs are less flexible ○ Roughly 90 percent of the hairs on your head are somewhere in the growing stage at any given time ○ Normally lose about 100 hairs from your scalp every day ■ Hair loss can be more extensive than the normal 100 hairs per day. ■ ALOPECIA AREATA: often called spot baldness, involves varying degrees of hair loss and can affect all areas of the body. ● most likely due to an autoimmune response, where the defense cells of the body destroy normal, healthy cells. ● PROCESS: ○ During the growth stage, a hair increases in length as new matrix cells are produced, differentiate, become keratinized, and die. ○ The hair grows longer as cells are added at the base of the hair root. ○ Eventually, hair growth stops; the hair follicle shortens and holds the hair in place. ○ A resting period follows. Each hair then goes into a one to two year resting stage, and then it falls out ○ After which a new cycle begins. ○ With this new cycle, a new hair forms to replace the old hair, which falls out of the hair follicle. Thus, losing a hair normally means that the hair is being replaced. PHASES: 1. Anagen (Growth phase) ● Nourishment of hair follicle via blood supply enables hair growth 2. Catagen (Transition phase) ● Hair follicle detaches from the nourishing blood supply. 3. Telogen (Resting phase) ● Without nourishment, the hair dies and falls out. NAILS ● ● ● ● Thin plate consisting of layers of dead stratum corneum cells that contain a very hard type of keratin. Located at the distal ends of the digits (fingers and toes). protect the ends of the fingers and toes, aid in grasping small objects, and are used for scratching. Consist of proximal nail root and distal nail body. ○ Nail Root - covered by skin Page 12 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ○ ○ ○ ○ ○ ○ ○ ○ ○ ○ ○ ● Nail Body - visible portion of the nail. It lies on the nail bed Nail Fold - covers the Lateral and Proximal edges of the nail. Nail Groove - hold the edges of the nail in place Cuticle/Eponychium - stratum corneum of the nail fold which grows into the nail body. Hyponychium - skin under the free edge of the nail. Thicken region of the stratum corneum. Nail root extends distally from the nail matrix which is growth center at the root of the nail is composed of active keratinocytes in the stratum basale The nail also attaches into the underlying nail bed, which is located between the nail matrix and the hyponychium. ■ The nail matrix and the bed is composed of the epithelial tissue, with a stratum basale that gives rise to the cells that form the nail, both contributing to the growth of the nail ■ The nail matrix is thicker than the nail bed and produces nearly all of the nail. ■ The nail bed is visible through the clear nail and appears pink because of the blood vessels in the underlying dermis A small part of the nail matrix (lunula), is seen through the nail body as a whitish crescent shaped area at the base of the nail. ■ The lunula, seen best on the thumb, appears white because the blood vessels do not show through the thicker nail matrix. The free edge of the nail and the nail body make up the nail plate. As the nail forms in the nail matrix and bed, it slides over the nail bed towards the distal end of the digit. The nails grow at an average rate of 0.5 to 1.2 mm per day. ■ fingernails grow more rapidly than toenails. ■ Unlike hair, they grow continuously throughout life and do not have a resting phase PHYSIOLOGY OF THE INTEGUMENTARY SYSTEM FUNCTIONS OF THE SKIN The functions of the integumentary system include: 1. 2. 3. 4. 5. 6. 7. Protection from pathogens and UV light Vitamin D production Temperature regulation Water retention Sensation Nonverbal communication Excretion Protection from pathogens and UV light ● ● ● ● ● ● ● Anatomy of a nail ● ● ● Integumentary system is the body’s outer barrier which defends it from harm. Hence, it is the body’s first line of defense. Difficult for pathogens to penetrate Dry, acidic surface is unfriendly to bacteria Melanin absorbs and protects underlying cells from UV light damage. The skin protects underlying structures from mechanical damage. Both the dermis and the epidermis play roles in this line of defense, but in different ways. ○ The dermis, particularly the irregular dense connective tissue of the reticular layer, provides structural strength, preventing tearing of the skin. ○ The stratified epithelium of the epidermis protects against abrasion. As the outer cells of the stratum corneum slough off, they are replaced by cells from the stratum basale. Calluses develop in areas subject to heavy friction or pressure. The skin prevents microorganisms and other foreign substances from entering the body. ○ Secretions from skin glands produce an environment unsuitable for some microorganisms. ○ The skin also contains components of the immune system that act against microorganisms Hair provides protection in several ways. ○ The hair on the head acts as a heat insulator and protects against ultraviolet light and abrasion. ○ The eyebrows keep sweat out of the eyes, ○ Eyelashes protect the eyes from foreign objects ○ Hair in the nose and ears prevents dust and other materials from entering. ○ Axillary and pubic hair protect against abrasion. Nails protect the ends of the fingers and toes from damage and can be used in defense. The intact skin plays an important role in reducing water loss because its lipids act as a barrier to the diffusion of water. Some lipid-soluble substances readily pass through the epidermis. ○ Lipid-soluble medications can be administered by applying them to the skin, after which the medication slowly diffuses through the skin into the blood. ○ For example, nicotine patches are applied to help reduce withdrawal symptoms in people attempting to quit smoking. Page 13 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB Vitamin D production ● ● ● ● Important for the regulation of calcium and phosphate homeostasis PRIMARY ROLE: stimulate the uptake of calcium and phosphate from the small intestine ○ Adequate levels of these minerals are necessary for normal bone metabolism and calcium is required for normal nerve and muscle function. Vitamin D synthesis begins in skin when it is exposed to ultraviolet light. UV light encourages skin to produce vitamin D. ○ People can produce all the vitamin D they require by this process if enough ultraviolet light is available. ■ However, because people live indoors and wear clothing, their exposure to ultraviolet light may not be adequate for the manufacture of sufficient vitamin D. This is especially likely for people living in cold climates because they remain indoors or are covered by warm clothing when outdoors. ■ Fortunately, vitamin D can also be ingested and absorbed in the small intestine. Natural sources of vitamin D are liver (especially fish liver), egg yolks, and dairy products (e.g., butter, cheese, and milk). In addition, the diet can be supplemented with vitamin D in fortified milk or vitamin pills Vitamin D synthesis involves a precursor molecule, 7-dehydrocholesterol, which is stored in the skin. ○ When exposed to ultraviolet light, the precursor molecule is converted into cholecalciferol. ○ Cholecalciferol is released into the blood and modified first by the liver and later by the kidneys to form active vitamin D3, also called calcitriol. ■ Calcitriol is an important hormone, a chemical messenger that travels through the blood, regulating calcium homeostasis. ○ ○ Water Retention ● The skin’s epidermis waterproofs the body by keeping water from the environment out and body fluids in. Sensation ● ● ● ● ● Nerve endings are located in the stratum basale, and dermis respond to stimuli Receptors in the skin can detect: ○ Temperature (heat & cold) ○ Pain ○ Touch ○ Pressure The epidermis and dermal papillae are well supplied with touch receptors The dermis and deeper tissues contain pain, heat, cold, touch, and pressure receptors Hair follicles (but not the hair) are well innervated, and sensory receptors surrounding the base of hair follicles can detect hair movement Nonverbal communication ● ● ● Blushing when embarrassed Pale when frightened Color, texture, silkiness, and other qualities of the skin and hair can all be indicative of overall health Additional function: Excretion ● Excretion is the removal of waste products from the body. ○ Temperature Regulation ● ● ● Body temperature is affected by blood flow through the skin When blood vessels (arterioles) in the dermis dilate, more warm blood flows from deeper structures to the skin, and heat loss increases. In other words, it dilate to increase blood flow to the skin so that heat can radiate out of the body. ○ Body temperature tends to increase as a result of exercise, fever, or a rise in environmental temperature. ○ In order to maintain homeostasis, this excess heat must be lost. ■ The body accomplishes this by producing sweat. ● The sweat spreads over the surface of the skin; as it evaporates, the body loses heat. Blood vessels in the dermis constrict, less warm blood flows from deeper structures to the skin, and heat loss decreases. In other words, it constricts to preserve heat for the body’s core. If body temperature begins to drop below normal, heat can be conserved by a decrease in the diameter of dermal blood vessels. Contraction of the arrector pili muscles causes hair to stand on end, but this does not significantly reduce heat loss in humans because so little hair covers the body. ■ However, the hair on the head is an effective insulator. In addition to water and salts, sweat contains a small amount of waste products, including urea, uric acid, and ammonia. However, even when large amounts of sweat are lost, the quantity of waste products eliminated in the sweat is insignificant because the urinary system excretes most of the body’s waste products. INJURIES TO THE SKIN ● Regeneration versus fibrosis ○ ○ ○ Skin can heal by regeneration or fibrosis. In regeneration, normal function returns. ■ •The stratum basale cells reach contact inhibition before the fibroblasts fill the area with scar tissue. In fibrosis, normal functioning tissue is replaced by scar tissue. ■ Fibroblasts’ collagen fibers produce granulation tissue to fill in the wound’s clot. ■ Fibroblasts reach contact inhibition before the cells of the stratum basale cells. Page 14 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ■ ■ ● Burns ○ ○ ○ ○ It is an injury to a tissue caused by heat, cold, friction, chemicals, electricity, or radiation Burns can be classified by degree. (considering the (1) extent of surface area involved and the (2) depth of the burn) ■ In adults, the rule of nines is used to determine the extent of a burn. ● which divides the body into areas that are approximately 9%, or multiples of 9%, of the body surface area ■ For younger patients, surface area relationships are different. ● For example, in an infant, the head and neck are 21% of BSA, whereas in an adult they are 9%. ● For burn victims younger than age 15, a table specifically developed for them should be consulted. On the basis of depth, burns are classified as either partial thickness or full-thickness burns. ■ Partial thickness are subdivided into first and second degree burns ■ Full thickness are called third-degree burns. Degrees: ■ First-degree burns involve only the epidermis. It may result in redness, pain, and swelling. They can be caused by sunburn or brief exposure to hot or cold objects, ■ and they heal in a week or so without scarring. Second-degree burns involve the epidermis and dermis. Symptoms include redness, pain, edema, swelling, and blisters. Healing takes approximately 2 weeks, and no scarring results. ● However, if the burn goes deep into the dermis, the wound appears red, tan, or white; may take several months to heal; and might scar. ● In all second-degree burns, the epidermis regenerates from epithelial tissue in hair follicles and sweat glands, as well as from the edges of the wound Third-degree burns involve the epidermis, dermis, and hypodermis. The epidermis and dermis are completely destroyed, and tissue just below the skin may be involved. Third-degree burns are often surrounded by first- and second-degree burns. ● Although the areas that have first- and second-degree burns are painful, the region of third-degree burn is usually painless because the sensory receptors have been destroyed. ● Third-degree burns appear white, tan, brown, black, or deep cherry-red. Skin can regenerate only from the edges, and skin grafts are often necessary. ● Symptoms include charring and no pain at the burn site Fourth-degree burns are extremely severe burns that affect tissues deeper than the subcutaneous tissue, often damaging tendons, fascia, muscle, and bone. ● Like third-degree burns, fourth-degree burns are painless due to the destruction of sensory receptors. ● Because of the severity of tissue damage, fourth-degree burns often require amputation or removal of damaged tissue. Death may occur due to the increased likelihood of infection. Page 15 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB /GRAPHIC CONTENT WARNING! Some images may be disturbing to some individuals./ ● ● ● DIAGNOSTIC TESTS USED TO DIAGNOSE INTEGUMENTARY SYSTEM DISORDERS ● Three diagnostic tests are commonly used: ○ Skin biopsy: the removal of a piece of tissue or a sample of cells from a body so that it can be analyzed in a laboratory ○ Skin scraping: the taking of skin cell scrapings so that the cells can be viewed under a microscope ○ Wood’s light: the use of a black light to view pigment changes in the skin ● the subcutaneous tissue cause the skin to sag and wrinkle. Retin-A is a vitamin A derivative that appears to be effective in treating fine wrinkles on the face, such as those caused by long-term exposure to the sun; it is not effective in treating deep lines. ○ One ironic side effect of Retin-A use is increased sensitivity to the sun’s ultraviolet rays. Doctors prescribing this cream caution their patients to always use a sunblock when they are going to be outdoors. The skin also becomes drier with age as sebaceous gland activity decreases. ○ Decreases in the activity of sweat glands and the blood supply to the dermis result in a reduced ability to regulate body temperature. ■ Elderly individuals who do not take proper precautions may experience heat exhaustion, which can even lead to death. The number of functioning melanocytes generally decreases; however, in some localized areas, especially on the hands and face, melanocytes increase in number, producing age spots. (Age spots are different from freckles, which are caused by an increase in melanin production, not an increase in melanocyte numbers.) White or gray hairs also appear because of a decrease in or lack of melanin production. Skin that is exposed to sunlight appears to age more rapidly than non exposed skin. ○ This effect is observed on areas of the body that receive sun exposure, such as the face and hands. ○ However, the effects of chronic sun exposure on the skin are different from the effects of normal aging. In skin exposed to sunlight, normal elastic fibers are replaced by an interwoven mat of thick, elastic-like material, the number of collagen fibers decreases, and the ability of keratinocytes to divide is impaired. DISORDERS ● Skin cancer ○ ○ Skin cancer is the most common cancer, and it is associated with sun exposure. Basal cell carcinoma is the most common skin cancer, and it tends not to metastasize. INTEGUMENTARY SYSTEM DISORDERS ● ● As the body ages, the skin is more easily damaged because the epidermis thins and the amount of collagen in the dermis decreases. Skin infections are more likely, and skin repair occurs more slowly. ○ A decrease in the number of elastic fibers in the dermis and a loss of adipose tissue from ○ Squamous cell carcinoma results from keratinocytes in the stratum spinosum. They commonly form on the face, hands, ears, and neck and can metastasize. Page 16 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ○ ○ ○ Malignant melanoma is the rarest form of skin cancer. It is the most deadly because it metastasizes easily. Usually begins in a mole. ● Skin infections ● Bacterial skin infections ○ ○ ○ ● Fungal skin infections ● Parasitic skin infections ○ Tinea Infections ■ Contact with an infected person, damp surfaces ■ Includes ringworm, athlete’s foot, and jock itch. ■ a circular rash that clears from the center, giving it a ringlike appearance Skin can be infected by a type of bacteria, a virus, fungus, or parasite. Impetigo: caused by the bacterium Staphylococcus or Streptococcus. Appears as a cluster of vesicles that burst and crust over, which may cause pain and itching. Cellulitis: infection of the skin’s dermis or hypodermis and is frequently caused by Streptococcus or Staphylococcus bacteria. Commonly occurs on the face and lower legs, characterized by redness and swelling of an area of the skin that increases in size rapidly. ○ ● Herpes Simplex Virus (HSV): small, painful blisters that appear on the skin and on the mucous membranes of the mouth (HSV-1) or genitals (HSV-2). Contagious. Herpes Varicella Zoster: causes chickenpox in children and shingles in adults. Scabies ■ Caused by an infestation of mites ■ Causes small red bumps on the skin that itch severely Viral skin infections ○ Warts: growth caused by HPV. Page 17 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB ● Other common skin disorders ○ Psoriasis ■ Characterized by an overgrowth of skin cells and improper keratinization of the epidermis and nails ■ It is an autoimmune disorder that runs in families ○ Scleroderma ■ It involves the accumulation of ■ ■ ○ excess connective tissue in the skin and various organs. The excess collagen causes hardening of the skin and organs, with decreased elasticity; this leads to a decrease in function. It can be caused by exposure to certain chemicals or can be associated with autoimmune diseases such as lupus. Atopic Dermatitis (Atopic Eczema) ■ It is an allergic reaction that causes an infection ADDITIONAL REPRESENTATIVE DISEASES AND DISORDERS OF THE INTEGUMENTARY SYSTEM (FROM BOOK TABLE 5.2) ■ ○ It can cause the skin to have a leathery appearance and be discolored Hives (Urticaria) ■ It is a skin reaction that can be caused by insect bites or by contact with substances that can cause an allergic reaction, such as certain foods or drugs. ■ The symptoms include raised areas of the skin, redness, and itching. CONDITION DESCRIPTION Birthmarks Congenital (present at birth) disorders of the dermal capillaries Ringworm Fungal infection that produces patchy scaling and inflammatory response in the skin Eczema and dermatitis Inflammatory conditions of the skin caused by allergy, infection, poor circulation, or exposure to chemical or environmental factors Frostbite - Psoriasis Chronic skin disease characterized by thicker-than-normal epidermal layer (stratum corneum) that sloughs to produce large, silvery scales; bleeding may occur if the scales are scraped away Vitiligo Development of patches of white skin where melanocytes are destroyed, apparently by an autoimmune response Alopecia areata - Skin cancer Page 18 of 19 UNIT II: THE INTEGUMENTARY SYSTEM - LAB BACTERIAL INFECTIONS Impetigo Small blisters containing pus; easily rupture to form a thick, yellowish crust; usually affects children Erysipelas Swollen patches in the skin caused by the bacterium Streptococcus pyogenes Decubitus ulcers (bedsores, pressure sores) Develop in people who are bedridden or confined to a wheelchair; compression of tissue and reduced circulation result in destruction of the skin and subcutaneous tissue, which later become infected by bacteria, forming ulcers Acne Develops when sebum — an oily substance that lubricates your hair and skin — and dead skin cells plug hair follicles. Bacteria can trigger inflammation and infection resulting in more severe acne Fig. ingrown VIRAL INFECTIONS Rubeola (measles) Skin lesions; caused by a virus contracted through the respiratory tract; may develop into pneumonia or infect the brain, causing damage Rubella (German measles) Skin lesions; usually mild viral disease contracted through the respiratory tract; may be dangerous if contracted during pregnancy because the virus can cross the placenta and damage the fetus Chickenpox Skin lesions; usually mild viral disease contracted through the respiratory tract Shingles Painful skin lesions; caused by the chickenpox virus after childhood infection; can recur when the dormant virus is activated by trauma, stress, or another illness Cold sores (fever blisters) Skin lesions; caused by herpes simplex I virus; transmitted by oral or respiratory routes; lesions recur Genital herpes Genital lesions; caused by herpes simplex II virus; transmitted by sexual contact Page 19 of 19