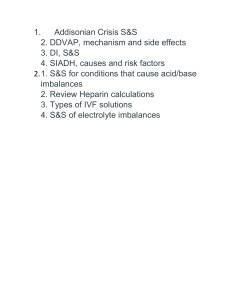
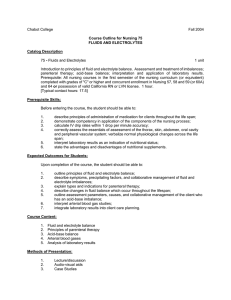
Fluid, Electrolyte, Acid-Base Imbalances: Textbook Chapter
advertisement

Chapter 16 Fluid, Electrolyte, and Acid-Base Imbalances KEY POINTS HOMEOSTASIS • Body fluids and electrolytes play an important role in maintaining a stable internal environment of the body. • A variety of adaptive responses keep the composition and volume of body fluids and electrolytes within the narrow limits of normal to maintain homeostasis and promote health. • Many diseases and their treatments could affect fluid and electrolyte balance and alter homeostasis. WATER CONTENT OF BODY • Water is the primary component of the body, accounting for about 50-60% of the body weight in the adult. • The 2 major fluid compartments in the body are intracellular fluid (ICF), or inside the cells, and extracellular fluid (ECF), or outside the cells. ECF is composed of interstitial fluid, plasma, and transcellular fluids. ELECTROLYTES • Electrolyte composition varies between the ECF and ICF, though the overall concentration of the electrolytes is nearly the same in the 2 compartments. • The measurement of electrolytes is important in evaluating electrolyte balance, as well as in determining the composition of electrolyte preparations. MECHANISMS CONTROLLING FLUID AND ELECTROLYTE MOVEMENT Copyright © 2020 by Elsevier, Inc. All rights reserved. • Many different processes are involved in the movement of electrolytes and water between the ICF and ECF. Some of these include osmosis, simple diffusion, facilitated diffusion, and active transport. Two forces drive water movement: hydrostatic pressure and osmotic pressure. • Osmotic pressure is the amount of pressure required to stop the osmotic flow of water. Measuring osmolality is important because it indicates the water balance of the body. • The tonicity of the fluid surrounding cells affects them. Fluids with the same osmolality compared to plasma are isotonic. Solutions which have a lower osmolality comparatively with plasma are hypotonic; those with an increased osmolality compared to plasma are hypertonic. • Hydrostatic pressure is the force of fluid within a compartment and is the major force that pushes water out of the vascular system at the capillary level. • Oncotic pressure (colloidal osmotic pressure) is osmotic pressure exerted by colloids in solution. The major colloids in the vascular system contributing to osmotic pressure are proteins, such as albumin. FLUID MOVEMENT IN CAPILLARIES • The amount and direction of fluid movement between the interstitial space and the capillary is determined by the interaction of (1) capillary hydrostatic pressure, (2) plasma oncotic pressure, (3) interstitial hydrostatic pressure, and (4) interstitial oncotic pressure. • When capillary or interstitial pressures are altered, fluid may abnormally shift from one compartment to another, resulting in edema or dehydration. FLUID SPACING • Fluid spacing describes the distribution of body water. • First spacing describes the normal distribution of fluid in the ICF and ECF compartments. • Second spacing refers to an abnormal accumulation of interstitial fluid (i.e., edema). Copyright © 2020 by Elsevier, Inc. All rights reserved. • Third spacing occurs when fluid accumulates in a part of the body and it cannot be exchanged easily with the rest of the ECF (e.g., burns, blisters). REGULATION OF WATER BALANCE • Water balance is maintained among water intake, use, and excretion. • An intact thirst mechanism is important for fluid balance. The patient who cannot recognize or act on the sensation of thirst is at risk for fluid deficit and hyperosmolality. • An increase in plasma osmolality or a decrease in circulating blood volume stimulates antidiuretic hormone (ADH) secretion. • Glucocorticoids and mineralocorticoids secreted by the adrenal cortex help regulate water and electrolytes. Aldosterone, a mineralocorticoid, has potent sodium-retaining and potassiumexcreting capability. • The kidneys are the primary organs for regulating fluid and electrolyte balance through adjusting urine volume and composition. • Insensible water loss, which is invisible vaporization from the lungs and skin, helps regulate body temperature. • The older adult has normal physiologic changes that increase his or her susceptibility to fluid and electrolyte imbalances. Functional changes may occur that affect the ability to obtain fluids independently. FLUID AND ELECTROLYTE IMBALANCES • Fluid and electrolyte imbalances are classified as either deficits or excesses. • Fluid volume deficit can occur with abnormal loss of body fluids (e.g., diarrhea, drainage, hemorrhage, polyuria), inadequate intake, or a plasma-to-interstitial fluid shift. Copyright © 2020 by Elsevier, Inc. All rights reserved. • Fluid volume excess may result from excess fluid intake, abnormal retention of fluids (e.g., heart failure, renal failure), or interstitial-to-plasma fluid shift. • The goals of treatment in fluid imbalances are to correct the underlying cause and to restore fluid and electrolyte balance. SODIUM IMBALANCES • Sodium is the major ECF cation and plays a major role in maintaining the concentration and volume of the ECF. • Hypernatremia, high serum sodium, may occur with inadequate water intake, water loss or, rarely, sodium gain. • Symptoms include those of dehydration and any accompanying ECF volume deficit, such as postural hypotension, weakness, and tachycardia. • Treatment is treated based on the cause. With water deficits, volume is replaced. If sodium excess occurs, dilution is achieved with sodium-free IV fluids. • Hyponatremia is a low serum sodium level. Common causes include a loss of sodiumcontaining fluids or water excess in relation to the amount of sodium. • Symptoms of hyponatremia are related to cellular swelling and are primarily manifested in the central nervous system. • In hyponatremia from water excess, fluid restriction is often the only treatment. If fluid loss is the cause, replacement with sodium-containing solutions is indicated. POTASSIUM IMBALANCES • Potassium is the major ICF cation and the major factor in the resting membrane potential of nerve and muscle cells. Changes in potassium balance cause several clinical problems. • Hyperkalemia is a high serum potassium level. Copyright © 2020 by Elsevier, Inc. All rights reserved. • The most common cause is renal failure. Hyperkalemia also occurs with massive cell destruction (e.g., burn or crush injury, tumor lysis); metabolic acidosis; and catabolic states (e.g., severe infections). • The most clinically significant manifestations of hyperkalemia are changes in cardiac conduction. Other manifestations include confusion, tetany, muscle cramps, and paresthesias, followed by weakness or paralysis of skeletal muscles. Monitor the ECG of all patients with hyperkalemia to detect potentially fatal dysrhythmias and monitor the effects of therapy. • The patient with dangerous cardiac dysrhythmias should receive IV calcium gluconate. • Hypokalemia is a low serum potassium level. • The most common causes are from abnormal losses from either the kidneys or the gastrointestinal tract. • Hypokalemia can cause potentially lethal ventricular dysrhythmias. Skeletal muscle weakness and paralysis, including the respiratory muscles, leading to shallow respirations and respiratory arrest, can occur. • Patients taking digoxin have increased digoxin toxicity if their serum potassium level is low. • Treat hypokalemia by giving oral or IV potassium chloride and increasing dietary potassium intake. CALCIUM IMBALANCES • The functions of calcium include transmission of nerve impulses, myocardial contractions, blood clotting, formation of teeth and bone, and muscle contractions. • Hypercalcemia is a high serum calcium level. • Hyperparathyroidism causes two thirds of the cases. The rest are caused by malignancy, especially from hematologic, breast, or lung cancers. Copyright © 2020 by Elsevier, Inc. All rights reserved. • Manifestations include fatigue, lethargy, confusion, weakness, seizures, and cardiac dysrhythmias. • Treatment consists of restricting dietary calcium, promoting urinary calcium excretion with loop diuretics, and hydrating the patient with isotonic saline infusions. • Hypocalcemia is a low serum calcium level. • The most common cause is a decrease in the production of parathyroid hormone. • Hypocalcemia causes increased muscle excitability resulting in tetany, paresthesia, and circumoral numbness. • Observe a patient who has had neck surgery, particularly a thyroidectomy, for signs of hypocalcemia. • Treatment of hypocalcemia is usually oral or IV calcium supplementation. PHOSPHATE IMBALANCES • Phosphorus is a primary anion in the ICF and is essential to the function of muscle, red blood cells, and the nervous system. • Hyperphosphatemia is a high serum phosphorus level. It is usually associated with acute kidney injury or • chronic kidney disease. • Symptoms include neuromuscular irritability, tetany, and calcified deposits in soft tissues. • The primary management is treating the underlying cause. • Hypophosphatemia is a low serum phosphorus level. • It most often occurs in a patient who is malnourished or has a malabsorption syndrome. • It is often asymptomatic. If symptoms occur, they are typically severe, requiring treatment with oral or IV phosphorus. MAGNESIUM IMBALANCES Copyright © 2020 by Elsevier, Inc. All rights reserved. • Magnesium plays an important role in many essential cellular processes. • Hypermagnesemia is a high serum magnesium level. It usually occurs only when a patient with renal insufficiency or failure has an increased magnesium intake. • Initial clinical manifestations include hypotension, facial flushing, lethargy, and nausea and vomiting. With rising levels, deep tendon reflexes are lost, followed by somnolence, then respiratory and cardiac arrest. • Treatment focuses on avoiding magnesium-containing medications and foods. Severe manifestations require treatment with IV calcium. • Hypomagnesemia, a low serum magnesium level, is associated with malnutrition states, such as fasting or starvation and increased GI or kidney losses. • Clinical manifestations are related to neuromuscular and CNS irritability and include hyperactive deep tendon reflexes, tremors, seizures, and confusion. • Treatment involves replacing magnesium with oral or IV supplements. ACID-BASE IMBALANCES • Patients with clinical conditions frequently develop acid-base imbalances. Always consider the possibility of acid-base imbalance in patients with serious illnesses. • The body has 3 main mechanisms by which it regulates acid-base balance to maintain the arterial pH between 7.35 and 7.45. These mechanisms are the buffer system, respiratory system, and renal system. • Buffering is the primary regulator of acid-base balance. Buffers act chemically to change strong acids into weaker ones or bind acids to neutralize them. Copyright © 2020 by Elsevier, Inc. All rights reserved. • Blood is slightly alkaline and has a normal arterial pH of 7.35 to 7.45. Medically, if the pH drops below 7.35, a person has acidosis. If the blood pH is greater than 7.45, the person has alkalosis Alterations in Acid-Base Balance • Acid-base imbalances are classified as respiratory or metabolic. Respiratory imbalances affect carbonic acid concentrations; metabolic imbalances affect the base bicarbonate. • Respiratory acidosis (carbonic acid excess) occurs whenever there is hypoventilation. • Respiratory alkalosis (carbonic acid deficit) occurs whenever there is hyperventilation. • Metabolic acidosis (base bicarbonate deficit) occurs when an acid other than carbonic acid accumulates in the body or when bicarbonate is lost from body fluids. • Metabolic alkalosis (base bicarbonate excess) occurs when a loss of acid (prolonged vomiting or gastric suction) or a gain in bicarbonate occurs. • Arterial blood gas (ABG) values provide valuable information about a patient’s acid-base status, the underlying cause of the imbalance, the body’s ability to regulate pH, and the patient’s overall oxygen status. • In cases of acid-base imbalances, the clinical manifestations are generalized and nonspecific. The treatment is directed toward correction of the underlying cause. ASSESSMENT OF FLUID, ELECTROLYTE, AND ACID-BASE IMBALANCES • Assess for the specific clinical manifestations of fluid, electrolyte, and acid-base imbalances throughout this chapter. Copyright © 2020 by Elsevier, Inc. All rights reserved. • Other health history data consist of assessment of past health history, medications, surgery, or other treatments, and a review of systems using functional health patterns. • Assessment of serum electrolyte values is the best starting point for identifying imbalances. Other useful tests include osmolality, glucose, BUN, creatinine, and specific gravity. ORAL FLUID AND ELECTROLYTE REPLACEMENT • In all cases, treatment is directed toward correcting the underlying cause. • Mild deficits can be corrected using the appropriate oral rehydration or electrolyte solution. IV FLUID AND ELECTROLYTE REPLACEMENT • Fluid replacement therapy is used to correct many fluid and electrolyte imbalances. The amount and type of solution used is determined by patient requirements and laboratory results. • Hypotonic solutions, such as 0.45% NaCl, provide more water than electrolytes, diluting the ECF and producing movement of water from the ECF to the ICF. • An isotonic solution, such as lactated Ringer’s and 0.9% NaCl, expands only the ECF. There is no net loss or gain from the ICF. • A hypertonic solution initially increases the osmolality of the ECF and results in expansion of the ECF. It is used in the treatment of hyponatremia and trauma patients with head injury. • KCl, CaCl, MgSO4, and HCO3– are common additives to the basic IV solutions. • Colloids increase oncotic pressure, pulling fluid into the vascular space. Central venous access devices • Central venous access devices (CVADs) are placed in large blood vessels of people who need frequent, continuous, rapid, or intermittent administration of fluids or medications. Copyright © 2020 by Elsevier, Inc. All rights reserved. • Three different methods are used to achieve central venous access: centrally inserted catheters, peripherally inserted catheters, or implanted infusion ports. • The major disadvantage of CVADs is an increased risk of systemic infection. • Nursing management of CVADs includes assessment, dressing change and cleansing, injection cap changes, and maintenance of catheter patency. Copyright © 2020 by Elsevier, Inc. All rights reserved.