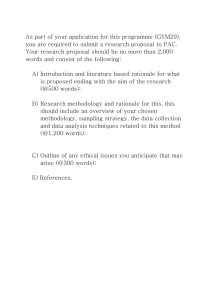
Normal Spontaneous Delivery & Essential Intrapartum Newborn Care (NSD & EINC) RLE & Lecture Integrated By H.P.M. Makiling Expected Outcomes: • Cognitive o Define what is NSD & EINC. o Learn the concepts and rationale of doing NSD & EINC. • Psychomotor o Demonstrate Essential Intrapartum Newborn Care through Return Demonstration. What is Normal Spontaneous Delivery? ❖ The delivery of the baby through the birth canal without any surgery. What is Essential Intrapartum Newborn Care? ❖ is a package of evidence-based practices recommended by the Department of Health (DOH), Philippine Health Insurance Corporation (PhilHealth), and the World Health Organization (WHO) as the standard of care in all births by skilled attendants in all government and private hospitals. Why is EINC implemented? ❖ The purpose is to lessen or possibly eliminate the mortality rate of infants, which was high during the early 2000s, and is a part of the MDGs & SDGs solution to lessen mortality rate. Paraphernalia needed in Normal Spontaneous Delivery: ❖ Sterile Gloves (2pcs) ❖ Cord clamp ❖ Mosquito Tip forceps ❖ Kelly forceps ❖ Bandage scissors ❖ Leggings ❖ Sterile towel (3pcs) ❖ Bonnet ❖ 4x4 Sterile Gauze ❖ 10cc syringe ❖ Oxytocin ❖ Bedpan Steps in doing Normal Spontaneous Delivery: 1. 2. Provide warmth: Check the environment (Room temperature at 25-28). ❖ Eliminate air drafts, turn off the aircon. ❖ Rationale: To prevent hypothermia and humidity inside delivery room. Perform medical handwashing. ❖ 3. A primary prevention that should be done by all health care workers. Prepare all the necessary materials. Separate clean and sterile materials. Arrange the instruments in proper order. ❖ Rationale: clean materials are away from the delivery table while sterile materials are near the nurses and physician’s vicinity. ❖ Arrangement of sterile materials: 4X4 gauze, cord clamp, Kelly forceps, mosquito tip forceps, sterile bandage scissors, sterile towel, bonnet, blanket. 4. Assist the client in fowlers/sitting position in delivery table. ❖ 5. Provide perineal hygiene. ❖ 6. Rationale: The patient is secured in position and not be in discomfort in position. Rationale: To provide a sterile environment for delivering the fetus. Don sterile gloves (double gloving) then place the sterile towel under the buttocks, followed by leggings and 1 towel in the abdomen. ❖ Rationale: the purpose of double gloving is to maintain sterility within the delivery table. ❖ Rationale: the purpose of putting sterile towel under the buttocks prevents soiling the delivery table. ❖ Rationale: the purpose of putting leggings for the client is for easier putting of undergarment after delivery of the infant. ❖ Rationale: the purpose of putting sterile towel in the client’s abdomen is done so that the secretions that is in the infants’ skin will not be contacted by the skin of the client during the process of skin-toskin contact and colostrum feeding in the delivery room. 7. Observe for signs of crowning, advice patient to bear down and perform proper panting. ❖ Rationale: once vaginal tear is at 8-10cm that is a sign of crowning. ❖ Rationale: advising and teaching proper panting to client prevents overfatigue and lessens the risk of the client being exhausted during delivery of the fetus. 8. During delivery of the head, encourage the patient to breathe rapidly with mouth open. ❖ Primipara: the physician will perform episiotomy, hand over the bandage scissors and gauze. ❖ Rationale: assist the physician, you will not do the episiotomy itself. ❖ Multipara: Perform Ritgen’s maneuver – place a sterile gauze in the perineum ❖ Rationale: use your dominant hand to assist the fetal head to be delivered, and instruct the mother to do proper panting and rapid breathing. 9. Immediately after birth of the head wipe the mouth and nose. ❖ Rationale: to remove secretions blocking the mouth and nose for infant to start breathing. 10. Assess for cord coil to determine if there is loop of cord encircling the neck. ❖ If CORD COIL is LOOSE: Loosened and drawn down over the fetal head. ❖ Rationale: so fetal head can breathe using mouth and nose once delivered. ❖ If CORD COIL is TIGHT: Clamp and cut the cord before shoulders are delivered. ❖ Rationale: to reduce the risk of the infant dying during delivery. 11. After expulsion of fetal head, the nurse should assist the baby during external rotation. ❖ Rationale: since the fetus itself knows how to rotate, you should just assist if there is problem during external rotation of the fetus. 12. Assist in downward pull to deliver the anterior shoulder and upward pull to deliver the rest of the body. ❖ Rationale: instruct client for the final push during delivery of the anterior shoulder, once anterior shoulder is out and upward pull is done the mother can stop doing proper panting. 13. State the time of delivery and the gender of the baby. ❖ Rationale: Shout the time and gender of the newborn so everyone in the delivery room is aware of the infants’ details. 14. Place the newborn in mother's abdomen in prone position, dry the newborn’s back and start the APGAR Scoring. ❖ Rationale: 1st APGAR score that the nurse should give is always and should be abnormal (4-6 score) and not at risk (0-3 score). 15. Perform thorough drying for at least 30 seconds (do not wipe off the vernix caseosa [spread] then remove the soiled towel). ❖ Rationale: Wipe off just the excess secretions in the skin of the infant, and do not wipe off the vernix caseosa because it is the natural coating of the newborn infant once delivered out of the uterus. 16. Cover the newborn with another sterile towel and place a bonnet to the head to conserve heat. ❖ Rationale: by doing so lessens the risk of the infant having hypothermia. 17. Administer oxytocin 10 IU (IM) to mother as ordered 1minute after the baby is born and second baby is ruled out. ❖ Rationale: by administering oxytocin to the patient intramuscularly, there should be uterine contraction that is a sign for placental separation. 18. Remove the 1st gloves before touching the umbilical cord then place it in the decontamination solution (normal saline + HCL) ❖ Rationale: Immediately dispose of the 1st layer of sterile gloves, you will not put the sterile gloves in the decontamination solution. ❖ Rationale: during this stage the decontamination solution should already be prepared for the placental separation and for decontaminating used sterile materials. 19. Wait until the pulsation stop, then clamp the plastic cord at least 2cm above the umbilical base and clamp again at 5cm from the base. Cut the cord close to the plastic clamp. ❖ Rationale: delayed cord clamping is an evidence-based practice that improves the chance of the infant not to be unalive. 20. Place the bandage scissors in the kidney basin with decontamination solution (normal saline + HCL [hydrochloric acid]) ❖ Rationale: by putting the bandage scissors can the people inside the delivery room ascertain that that bandage scissor is used for cord clamping. 21. Observe for signs of placental separation. ❖ Rationale: once signs of placental separation, after delivery of the fetus and administration of oxytocin, is manifesting; prepare for the expulsion of the placenta. ❖ Signs and symptoms of placental separation: ➢ When fundus is palpated, the nurse will feel globular mass in the uterine fundus. ➢ Lengthening of the umbilical cord. ➢ Gushing of blood out of the vagina. ➢ There are still signs of uterine contractions. 22. If there is lengthening of the cord, the nurse should perform Crede's maneuver (during strong uterine contraction perform controlled cord traction and counter traction until placenta is out). ❖ Rationale: Crede’s maneuver is done by doing up, down, right, and left movements during wringing of the umbilical cord; during strong uterine contraction and performing proper controlled counter contraction to pull placenta out the uterus. 23. Observe and note for the time of placental delivery, inspect for the completeness of placenta and cotyledons. ❖ Rationale: shout the time of placental expulsion, same manner when newborn infant is declared out of the client’s uterus. ❖ Rationale: normal number of cotyledons should be 30 and above, if cotyledons are finished being counted and less than what is normal and placenta is losing some parts; immediately report it the physician for expulsion of remaining parts of the placenta inside the client’s uterus. ❖ Rationale: If placenta is complete and the number of cotyledons is complete, it is a Schultze placenta; while if the placenta is incomplete and is missing parts and the number of cotyledons is also incomplete, it is a Duncan placenta, also known in other terms as “dirty Duncan placenta. 24. Place the placenta in the kidney basin. ❖ Rationale: putting placenta in the decontamination solution for further examination. 25. Perform perineal hygiene, if perineal stitching is performed, assist the physician. ❖ Rationale: so that there will be no secretions left in the vagina and perineum and to inhibit the growth of microorganisms that can develop infections. 26. Place the patient in comfortable position ❖ Rationale: so that when you are transferring client to recovery room there will be no discomfort. 27. Observe for feeding cues at 20–90 minutes, encourage the mother for full breastfeeding, once feeding cues are present. ❖ Rationale: by encouraging client for breastfeeding will there be the time for the family to have their first interaction with a child. APGAR Score ➢ The Apgar score describes the condition of the newborn infant immediately after birth and, when properly applied, is a tool for standardized assessment. ➢ It also provides a mechanism to record fetal-to-neonatal transition. ➢ Apgar scores do not predict individual mortality or adverse neurologic outcome. Materials for Newborn Care: ➢ Tuberculin syringe (3pcs ➢ Bacille-Guerin Calmette Vaccine ➢ Vitamin K ➢ Hepatitis B Vaccine ➢ Newborn clothes (onesies, baby gloves, booties, bonnet) ➢ Newborn Diaper ➢ Dry cotton balls ➢ Micropore tape ➢ Blanket ➢ Manual tape measure w/o metal ➢ Identification Band Steps in doing Essential Intrapartum Newborn Care: 1. After full breastfeeding is completed, the nurse may perform eye care. ❖ Performing eyecare prevents of the infant having conjunctival infection. 2. Administer ophthalmic ointment, gently pull down the lower eyelid and apply the medication from inner to outer canthus. ❖ Application of ophthalmic erythromycin lessens the risk of the infant having ophthalmia neonatorum, a type of congenital conjunctival infection caused by STIs. 3. Close the newborn’s eyes and wipe the excess ointment. ❖ Rationale: use cotton, gauze or gloves to remove excess ointment, avoid skin-to-skin contact with infant to lessen risk of contact with your skin flora/bacteria. 4. 5. Administer Vitamin K in left vastus lateralis, if the newborn is: ❖ Premature: 0.05ml/IM ❖ Term: 0.1ml/IM ❖ Administering Vit. K improves blood coagulation, and lessens risks of blood thinning. Administer Hepatitis B vaccine in right vastus lateralis at 0.5ml/IM ❖ 6. Administer BCG in the upper deltoid at 0.05ml/ID ❖ 7. Administering Hepatitis B vaccine lessens the risk of the infant having Hepatitis B. Administering BCG can lessen the risk of the infant having respiratory infections. Measure the NB length (48-54cm), head circumference (33 35cm), chest and abdomen (31-33cm) Weight (2,500-4000grams/5 8lbs/8oz-13oz.) then place the NB identification tag ❖ When measuring newborn length make sure to start at the crown and end in the sole of the feet. ❖ After measuring the infant, place identification band (color of band [either blue or pink], last name of parent indicated, date and time of birth, and physician/nurses that assist the labor of client). 8. Assess the VS and perform 2nd APGAR SCORING ❖ Temperature: use rectal thermometer to check for patency (check if infant has anal hole). ❖ Respirations: should be 20-40 c/pm, if bradycardic or tachycardic report to pediatrician ❖ Pulse: should be 130-160 b/pm, if infant shows signs of bradypnea or tachypnea report to pediatrician ❖ 9. Rationale: the 2nd APGAR score should be normal (7-10 score) Postponed bathing at least 6 hrs. the mother is place in the stretcher together with her baby and move in the recovery room or ward. ❖ Rationale: prevents the infant having hypothermia. 10. Encourage for continued breastfeeding ❖ Rationale: prevents the infant having hypoglycemia. ❖ Continued breastfeeding for at least a year has wonderful effects for the infant’s development. 11. Perform after care. ❖ By meaning of after care; assess VS of mother & infant during recovery process, observe the mother & infant during recovery process and/or provide cord care for infant. ❖ Educate the client the benefits of breastfeeding and to have follow-up check-ups during post-partum period and check-up of the infant during its 1st year. ❖ Once the infant has pooped in the next 24 hours (meconium) the mother and the infant can be discharged. ❖ It is an EBP to release both mother and infant after meconium, so that both cannot contact the microorganisms that is within the hospital’s premises, and expose the infant to the immediate family. References: https://www.unionwomancare.org/pdf/ONG-09e.pdf https://caro.doh.gov.ph/wp-content/uploads/2014/09/EINC.pdf Maternal & Child Nursing 9th Editon by JoAnne Silbert-Flagg Kozier & Erb’s Fundamentals of Nursing Concepts, Process, and Practice, 11th Edition Nursing_CS_Newborn-Apgar-Scores-and-Implications; Lecturio Nursing Further Readings: Checklist for NSD & NBC Maternal & Child Nursing 9th Editon by JoAnne Silbert-Flagg