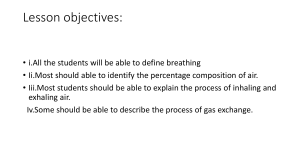
Pursed-lip Breathing - StatPearls - NCBI Bookshelf 2/20/23, 9:17 AM NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Pursed-lip Breathing John D. Nguyen; Hieu Duong. Author Information and Affiliations Last Update: July 25, 2022. Definition/Introduction The major drive for respiration originates in the central and peripheral chemoreceptors. The central chemoreceptors are located anterior medulla in the brainstem and predominantly responds to a decrease in pH from the accumulation of carbon dioxide in the cerebral spinal fluid. The blood-brain barrier protects the central nervous system from external stimuli. Carbon dioxide is lipid-soluble, which allows it to quickly diffuse across the protective barrier and influence the respiratory drive. Unlike the central chemoreceptors, the peripheral chemoreceptors are more sensitive to changes in oxygen levels. The peripheral chemoreceptors consist of the carotid and aortic bodies. The aortic bodies are located at the aortic arch while the carotid bodies are situated at the common carotid artery bifurcation. Hypoxia stimulates cranial nerve IX to send signals to the nucleus tractus solarius which triggers ventilation. However, the central chemoreceptors normally override the peripheral receptors as it originates from the central control system of the body.[1] Purse-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow controlled flow. The expiratory phase of respiration is going to prolonge when compared to inspiration to expiration ratio in normal breathing. The maneuver presents as a controlled breath directed through the nostril then exhalation directed through lips having a puckered or pursed appearance. This technique creates a back pressure producing a small amount of positive endexpiratory pressure (PEEP). During exhalation, the forces cause the airways that lack cartilage to drag inward towards the lumen obstructing airflow by increasing airway resistance which could lead to carbon dioxide trapping.[2] When there is an increased in carbon dioxide levels the central chemoreceptors are triggered to immediately increase the rate of respiration in an attempt to bring the body’s pH back to a baseline range of roughly 7.4 in a normal individual.[3][4] While the increase in the rate of respiration is effective in clearing carbon dioxide, it can potentially cause more air trapping and fatigue of the respiratory muscles.[5] PEEP mitigates the increase in work by creating an artificial splint that supports the patency of the airways and alveoli, increasing surface area and recruiting more alveoli to participate in gas exchange.[6] The positive pressure created opposes the forces exerted on the airways from the flow of exhalation. As a result, pursed-lip breathing helps support breathing by the opening of the airways during exhalation and increasing excretion of volatile acids in the form of carbon https://www.ncbi.nlm.nih.gov/books/NBK545289/ Page 1 of 5 Pursed-lip Breathing - StatPearls - NCBI Bookshelf 2/20/23, 9:17 AM dioxide preventing or relieving hypercapnia. Through purse-lip breathing, people can have relief of shortness of breath, decrease the work of breathing, and improve gas exchange. They also regain a sense of control over their breathing while simultaneously increasing their relaxation. Issues of Concern With purse-lip breathing, the action of breathing initiates voluntarily. For purse-lip breathing to be effective, the individual must be able to perform the technique correctly. The technique requires proper coordination to maintain prolonged exhalation. As for the therapeutic effects, they are short-lived. The technique is limited to 3 to 5 breaths since prolonging the duration of the technique causes fatigue of the respiratory muscles and significantly lower than normal levels of carbon dioxide in a normal individual potentially leading to a decrease perfusion pressure in the brain causing syncope. Without the proper use of purse-lip breathing, an individual could exacerbate air trapping and carbon dioxide retention. Clinical Significance Clinically, purse-lip breathing when done correctly, can be beneficial in individuals suffering from dyspnea and air trapping. With proper teaching and coaching the technique can be easily taught by a trained professional. The benefits of purse-lip breathing may extend beyond its effects on the relief of carbon dioxide retention and improvement in oxygenation. Patients in mild respiratory distress may be able to regain control of their respiration through the technique. It is also an excellent tool for relaxation. Purse lip breathing commonly helps patients with chronic obstructive pulmonary disease (COPD). With these patients, purse-lip breathing may not be a voluntary action, but rather a compensatory mechanism to help splint open the airways.[7][8] COPD individuals may have chronic obstruction of their airways from mucus plugging, loss of integrity of the airways, or enlargement of the airways. These changes in the airways can prevent the appropriate driving pressure and flow of air to maintain an adequate clearance of carbon dioxide due to an increase in airway resistance.[9] The increase in airway resistance also affects inhalation preventing enough oxygen from reaching the alveoli to create a sufficient partial pressure of oxygen needed to drive the diffusion of oxygen across the alveoli-capillary interface adequately. The defected driving pressure for oxygenation is further exacerbated due to the retention of carbon dioxide, causing less carbon dioxide to diffuse from the blood into the alveoli for excretion. The blunting of the proper mechanism to excrete carbon dioxide and adequate oxygenation leads to a constant stimulus to the central chemoreceptors to increase respiration until the point of exhaustion. Chronic hypercapnia decreases the sensitivity of the central chemoreceptors, allowing peripheral receptors sensing oxygen levels to become the predominantly drive for respiration.[10][11] Increased purse lip breathing in these patients may be a sign of impending respiratory failure. Nursing, Allied Health, and Interprofessional Team Interventions When it comes to the proper teaching of a new technique such as purse-lip breathing the trained individual should explain the benefits and potential adverse effects. The physiology of the https://www.ncbi.nlm.nih.gov/books/NBK545289/ Page 2 of 5 Pursed-lip Breathing - StatPearls - NCBI Bookshelf 2/20/23, 9:17 AM technique requires explanation, followed by a demonstration. After teaching, the trainer should ensure that the trainee has learned the technique properly by asking the trainee to perform the technique or explain the technique to the trainer; this can ensure proper technique and correction of any mistakes that may occur during the learning process.[12][13] Physicians, nurses, and health care professionals can incorporate the technique to help calm the patient. Patients with COPD, congestive heart failure, or panic attack may use the technique to relieve their dyspnea. This method could help reduce the need for noninvasive mechanical ventilation.[14][15] Nurses that can recognize COPD patients in respiratory distress through signs such as increase purse-lip breathing, dyspnea, and accessory muscles use will allow rapid initiation of a response team to assist the patient before they deteriorate.[16][17] [Level III] Nursing, Allied Health, and Interprofessional Team Monitoring When it comes to monitoring, nursing staff should be able to teach pursed-lip breathing and explain to the trainee when this technique would be useful. The risk and benefits of the technique should be thoroughly explained with all questions and concerns addressed. The nursing staff often spends the most time with patients of all health professionals. Nurses should be able to identify any patients that are in respiratory distress. With the knowledge of the common signs and symptoms of respiratory distress, nurses can effectively alert the appropriate response team and physicians to intervene before they deteriorate. Since the compensatory pursed-lip breathing is common to COPD patients, nursing should monitor COPD for the fatigue of respiratory muscles. Promptly alerting the physician can prevent patients from requiring mechanical ventilation. Review Questions Access free multiple choice questions on this topic. Comment on this article. Figure Pursed lip breathing. Image courtesy O.Chaigasame References 1. Brinkman JE, Toro F, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 8, 2022. Physiology, Respiratory Drive. [PubMed: 29494021] 2. Seadler BD, Toro F, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 8, 2022. Physiology, Alveolar Tension. [PubMed: 30969647] 3. Hopkins E, Sanvictores T, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Sep 12, 2022. Physiology, Acid Base Balance. [PubMed: 29939584] https://www.ncbi.nlm.nih.gov/books/NBK545289/ Page 3 of 5 Pursed-lip Breathing - StatPearls - NCBI Bookshelf 2/20/23, 9:17 AM 4. Keir DA, Duffin J, Millar PJ, Floras JS. Simultaneous assessment of central and peripheral chemoreflex regulation of muscle sympathetic nerve activity and ventilation in healthy young men. J Physiol. 2019 Jul;597(13):3281-3296. [PubMed: 31087324] 5. Lomax M, Kapus J, Webb S, Ušaj A. The effect of inspiratory muscle fatigue on acid-base status and performance during race-paced middle-distance swimming. J Sports Sci. 2019 Jul;37(13):1499-1505. [PubMed: 30724711] 6. Gonçalves-Ferri WA, Jauregui A, Martins-Celini FP, Sansano I, Fabro AT, Sacramento EMF, Aragon DC, Ochoa JM. Analysis of different levels of positive end-expiratory pressure during lung retrieval for transplantation: an experimental study. Braz J Med Biol Res. 2019;52(7):e8585. [PMC free article: PMC6644527] [PubMed: 31314854] 7. Vatwani A. Pursed Lip Breathing Exercise to Reduce Shortness of Breath. Arch Phys Med Rehabil. 2019 Jan;100(1):189-190. [PubMed: 30033163] 8. Sakhaei S, Sadagheyani HE, Zinalpoor S, Markani AK, Motaarefi H. The Impact of Pursedlips Breathing Maneuver on Cardiac, Respiratory, and Oxygenation Parameters in COPD Patients. Open Access Maced J Med Sci. 2018 Oct 25;6(10):1851-1856. [PMC free article: PMC6236030] [PubMed: 30455761] 9. Haghighi B, Choi S, Choi J, Hoffman EA, Comellas AP, Newell JD, Lee CH, Barr RG, Bleecker E, Cooper CB, Couper D, Han ML, Hansel NN, Kanner RE, Kazerooni EA, Kleerup EAC, Martinez FJ, O'Neal W, Paine R, Rennard SI, Smith BM, Woodruff PG, Lin CL. Imaging-based clusters in former smokers of the COPD cohort associate with clinical characteristics: the SubPopulations and intermediate outcome measures in COPD study (SPIROMICS). Respir Res. 2019 Jul 15;20(1):153. [PMC free article: PMC6631615] [PubMed: 31307479] 10. Docio I, Olea E, Prieto-LLoret J, Gallego-Martin T, Obeso A, Gomez-Niño A, Rocher A. Guinea Pig as a Model to Study the Carotid Body Mediated Chronic Intermittent Hypoxia Effects. Front Physiol. 2018;9:694. [PMC free article: PMC5996279] [PubMed: 29922183] 11. Benner A, Lewallen NF, Sharma S. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 19, 2022. Physiology, Carbon Dioxide Response Curve. [PubMed: 30844173] 12. Feinberg I, Ogrodnick MM, Hendrick RC, Bates K, Johnson K, Wang B. Perception Versus Reality: The Use of Teach Back by Medical Residents. Health Lit Res Pract. 2019 Apr;3(2):e117-e126. [PMC free article: PMC6610032] [PubMed: 31294313] 13. Yen PH, Leasure AR. Use and Effectiveness of the Teach-Back Method in Patient Education and Health Outcomes. Fed Pract. 2019 Jun;36(6):284-289. [PMC free article: PMC6590951] [PubMed: 31258322] 14. Sha J, Worsnop CJ, Leaver BA, Vagias C, Kinsella P, Rahman MA, McDonald CF. Hospitalised exacerbations of chronic obstructive pulmonary disease: adherence to guideline recommendations in an Australian teaching hospital. Intern Med J. 2020 Apr;50(4):453-459. [PubMed: 31157943] 15. Avdeev SN, Truschenko NV, Gaynitdinova VV, Soe AK, Nuralieva GS. Treatment of exacerbations of chronic obstructive pulmonary disease. Ter Arkh. 2018 Dec 30;90(12):6875. [PubMed: 30701836] 16. Charlton PH, Pimentel M, Lokhandwala S. MIT Critical Data. Secondary Analysis of https://www.ncbi.nlm.nih.gov/books/NBK545289/ Page 4 of 5 Pursed-lip Breathing - StatPearls - NCBI Bookshelf 2/20/23, 9:17 AM Electronic Health Records [Internet]. Springer; Cham (CH): Sep 10, 2016. Data Fusion Techniques for Early Warning of Clinical Deterioration; pp. 325–338. [PubMed: 31314272] 17. Cui L, Liu H, Sun L. Multidisciplinary respiratory rehabilitation in combination with noninvasive positive pressure ventilation in the treatment of elderly patients with severe chronic obstructive pulmonary disease. Pak J Med Sci. 2019 Mar-Apr;35(2):500-505. [PMC free article: PMC6500851] [PubMed: 31086540] Copyright © 2022, StatPearls Publishing LLC. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Bookshelf ID: NBK545289 PMID: 31424873 https://www.ncbi.nlm.nih.gov/books/NBK545289/ Page 5 of 5