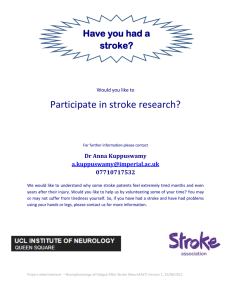
Journal of Psychosomatic Research 173 (2023) 111466 Contents lists available at ScienceDirect Journal of Psychosomatic Research journal homepage: www.elsevier.com/locate/jpsychores Trajectories of post-stroke quality of life and long-term prognosis: Results from an eleven-year prospective study Meijing Hu, Baiyang Zhang, Yidie Lin, Minghan Xu, Cairong Zhu * Department of Epidemiology and Health Statistics, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, People's Republic of China A R T I C L E I N F O A B S T R A C T Keywords: Stroke Quality of life Prognosis Trajectory Purpose: The relationship between quality of life (QoL) and long-term prognosis in stroke patients is still unclear. We explored physical and mental QoL trajectories during the first six months after stroke and determined the associations between trajectories and long-term prognosis in patients with first-ever ischemic stroke. Methods: Included were 733 participants from a prospective study. QoL was assessed with the 12-item Short Form Survey (SF-12) at baseline, 3 and 6 months. Patients' prognoses (stroke recurrence and death) were identified from 2010 to 2021. The latent class growth model (LCGM) was used to identify distinct trajectories of physical and mental QoL measured over the first 6 months. We employed the Cox model or Fine-Gray model for prognoses to examine the associations between QoL trajectories and prognosis. Results: Five trajectories of physical QoL and five trajectories of mental QoL were identified. For physical QoL of the Poor-Improved, and Moderate-Impaired trajectory versus Moderate-Improved trajectory, the hazard ratio (HR) for death was 2.39 (1.14 to 5.02), and 2.03(0.93 to 4.44); the HR for recurrence was 1.56 (0.83 to 2.94) and 2.33 (1.28 to 4.24). For mental QoL of the Moderate-Impaired trajectory versus the Moderate-Improved tra­ jectory, the HR for death was 2.48 (1.21 to 5.07). The results were robust in the sensitivity analysis. Conclusion: QoL during the first six months after ischemic stroke can be categorized into distinct groups. Change in QoL was associated with long-term survival. Secondary prevention of recurrent strokes might rely more on improving patients' physical QoL. 1. Introduction Stroke is a leading cause of death and disability worldwide [1,2]. Poor quality of life (QoL) was reported in stroke survivors due to chal­ lenges like loss of economic sources, disability, and mental difficulties such as depressive symptoms [3]. Compromised QoL in stroke survivors is one of the causes that stroke is regarded as an essential public health problem [4,5]. The support of health personnel and family members can help stroke survivors improve their QoL, including physical, mental, and social aspects [6]. Assessing the QoL for patients in the hospital and survivors living at home might be necessary, which helps healthcare providers ensure that survivors receive adequate community support and medical services to improve their health. In the early stage of stroke, QoL is an appropriate prognostic risk determination tool for planning post-stroke therapy strategies. A short follow-up study proposed that the poor QoL of patients three months after stroke was related to the low 1-year survival rate [7]. The corre­ lation between QoL and survival after stroke was limited because pa­ tients' QoL was investigated at a certain time, resulting in the loss of data information. There has been a growing body of studies evaluating the average change of QoL among individuals with first-ever stroke but reaching inconsistent conclusions. Some studies investigated QoL with a follow-up period of up to 6 months post-stroke and found an improve­ ment in QoL [8–10]. Another study reported different results; substan­ tial gains in QoL during inpatient stroke rehabilitation were followed by declines six months after discharge [11]. A possible explanation of this disparity is the presence of heterogeneity in longitudinal change pat­ terns of post-stroke QoL, and the averaged data masked subgroup in­ formation on QoL changes over time in prior studies. As far as we know, some scholars found QoL of stroke patients in the Netherlands [12] and Italy [13] has changed and can be divided into different trajectories. The QoL of stroke patients in different socioeconomic environments have * Corresponding author at: Department of Epidemiology and Health Statistics, West China School of Public Health and West China Fourth Hospital, Sichuan University, NO.16 Renmin South Road, Chengdu, Sichuan 610041, People's Republic of China. E-mail address: cairong.zhu@hotmail.com (C. Zhu). https://doi.org/10.1016/j.jpsychores.2023.111466 Received 25 November 2022; Received in revised form 14 August 2023; Accepted 15 August 2023 Available online 18 August 2023 0022-3999/© 2023 Elsevier Inc. All rights reserved. M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 different heterogeneous trajectories, but the trajectory pattern of stroke patients in upper-middle-income countries is still unclear. Besides, with the progress of stroke treatment and management, more stroke patients can survive the disease, and the importance of knowledge of the longterm prognosis of health also increases [14]. The evidence on the cor­ relation between QoL and the long-term prognosis of patients with firstepisode stroke is still insufficient. In this context, we hypothesized that QoL trajectory patterns exist in Chinese stroke patients and that these patterns have prognostic signifi­ cance for the risk of subsequent events. Our study objectives were to (1) establish a plausible QoL trajectory pattern within the first six months of stroke patients and (2) elucidate the association of QoL trajectories with subsequent clinical events, including all-cause death and recurrent stroke, until the end of follow-up. and stroke characteristics (TOAST (Trial of Org 10,172 in Acute Stroke Treatment), mRS score > 1 at arrival, side of brain damage). Marital status was divided into two groups, married (in marriage, separated) and single (divorced, widowed, or never married). The classification of smoking or drinking status was based on the question, “Were you a regular smoker/drinker before the stroke?”. Physical activity was clas­ sified according to “Did you participate in physical activity at least once a week for one year before the stroke?”. Following the TOAST criteria, all patients with ischemic stroke were further classified into different stroke subtypes: large-artery atherosclerosis (LAA), cardio-embolism (CE), small-artery occlusion (SAO), other determined etiology (SOE), and undetermined etiology. In the study, the proportion of strokes due to other identified or unidentified causes (i.e., interlayer or other causes) was deficient (only 4 individuals), similar to the previous study [24]. Only three categories of TOAST (LAA, SAO and CE) were included in our study. Side of brain damage includes LHD (left hemisphere damage), RHD (right hemisphere damage), BHD (bilateral hemisphere damage), and Other (side of brain damage is uncertain). 2. Materials and methods 2.1. Participants and procedures Patients diagnosed with first-ever ischemia stroke in the Department of Neurology of West China Hospital of Sichuan University from January 2010 to December 2019 were recruited and followed up to September 2021. Patients were diagnosed according to WHO criteria in combina­ tion with a CT scan and/or MRI [15]. Iatrogenic stroke, such as carotid endarterectomy, cardiac surgery, or angioplasty, and patients with se­ vere cognitive impairment or in critical were excluded. One thousand one hundred twenty-seven stroke patients were included in the participating centers during the study period. For analytical purposes, 394 respondents were excluded for the following reasons: (1) Repeated or invalid enrollment (n = 14), (2) Non-first-ever ischemic stroke (n = 90), (3) TOAST is classified as an interlayer or other reasons (n = 4), (4) Missing values for relevant covariates (n = 59), (5) No follow-up at 3 and 6 months (n = 186), and (6) Recurrence or death in the first 6 months (n = 41). The remaining 733 patients for whom the baseline data sets were complete and at least one reassessment of QoL were conducted were included in the final analyses. 2.3. Survey method Trained graduate students in epidemiology and health statistics are employed as staff for baseline collection and telephone follow-up. The survey included demographic characteristics, health-related behaviors, vascular risk factors, and stroke characteristics. At least four people will visit the ward weekly for a baseline survey. The investigator will explain the study's purpose and significance and introduce the questionnaire's contents to the patients and their families. After questionnaire collection is completed, the survey team will exchange questionnaires for review. If there are incomplete or unclear questionnaires, they should return to the ward immediately to complete the questionnaires. Patients were fol­ lowed up by phone every three months. The score of the SF-12 (Chinese version of the 12-item short-form survey; version 2) and the self-report prognosis (ischemia stroke recurrence and death events) were collected. The survey team exchanged questionnaires for review, and if incomplete or unclear questionnaires were found, the patient or family should be contacted again, and the questionnaires continued to be completed. Double data entry and validation were done using EpiData software. 2.2. Measures 2.2.1. QoL The 12-item Short Form Survey (SF-12) has good reliability and validity [16], which is reliable and sensitive for the Chinese population [17,18], and has been widely used to assess the quality of life of stroke patients [19,20]. The 12-item Short Form Survey performs similarly to the MOS 36-item Short Form Survey (SF-36) [21–23]. It is built with questions extracted from the eight dimensions of SF-36, but the completion time is effectively shortened. The SF-12 includes 12 items about health status and eight health dimensions: Physical function (PF); Role-Physical (RP); Bodily Pain (BP); General Health (GH); Vitality (VT); Social Functioning (SF); Role-Emotional (RE) and Mental Health (MH). According to the American scoring method, two summary scores can be calculated, physical component score (PCS) and mental component score (MCS). Scores above or below 50 are above or below the general population's mean. 2.4. Statistical analysis Continuous variables were represented as Mean ± SD and Median (quartiles), and categorical variables were represented as percentages. We adopted a group-based trajectory modeling approach through the TRAJ procedure in SAS software, version 9.4 (SAS Institute, Inc), to identify trajectories of PCS and MCS during the first 6 months after stroke. This special form of finite mixture modeling fixes the slope and the intercept to equality across individuals within a trajectory. This approach permits all available data to be included in the estimated model, assuming the data were missing randomly. The longitudinal QoL data were fitted by a maximum likelihood method as a mixture of multiple latent trajectories in a censored normal model with a poly­ nomial function of time [25]. We evaluated each trajectory's growth factor (intercept, linear, or quadratic) to obtain the optimal polynomial function forms describing the dynamic QoL change. The best-fitting model is selected by comparing the Bayesian information criterion (BIC) and the Akaike in­ formation criterion (AIC). The model with a lower BIC value and AIC value fits better. In addition, the proportion of each trajectory member needs to be considered to ensure the rationality of the analysis. Each trajectory should hold an approximate trajectory membership proba­ bility of at least 3 % [26,27]. Average posterior probabilities (APP) of trajectory membership >0.70 are taken to indicate that the modeled trajectories are individuals with similar patterns of change and discriminate between individuals with distinct patterns of change. Once the distinct trajectories of physical QoL and mental QoL were 2.2.2. Outcome events Outcome events were all-cause death and recurrent stroke. If the patient relapse repeatedly, the survival time of the recurrent is based on the first recurrence time. Outcome events were collected through structured telephone interviews by trained investigators. 2.2.3. Covariates Covariates included demographic characteristics (age, sex, marital status, education level, annual household income), health-related be­ haviors (smoking status, drinking status, physical activity), vascular risk factors (BMI, hypertension, diabetes, hyperlipidemia, heart disease), 2 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 determined, the Kruskal-Wallis and Chi-square tests were conducted to explore the difference in individual characteristics between distinct trajectories. Cox multivariate model was used to examine the association between QoL trajectories and all-cause mortality. The Fine-Gray model examined the association between trajectories and stroke recurrence, which was applied to correct the possible bias caused by competing risks of death on stroke recurrence [28]. Models included physical trajec­ tories, mental trajectories, and the covariates mentioned above. We started with the unadjusted models and continued to the multivariable models by gradually adding covariates. Sensitivity analyses were performed to test the robustness of the results. We reconstructed trajectory models by including individuals with all three visits of QoL measures at baseline, 3, and 6 months and duplicated the Cox multivariate model and Fine-Gray model analyses. Data analyses were performed using software programs SAS 9.4 (SAS Institute, Inc), and statistical significance was set at P < 0.05 (2-tailed) throughout. Table 1 Baseline Characteristics and Outcomes of Included Subjects (N = 733). Categories Variables Demographics Age (years) Mean ± SD Median(Q1,Q3) 3. Results 3.1. Participants' characteristics Health-related behaviors A total of 733 patients with ischemic stroke met the pre-defined eligibility criteria (Fig. S1). The all-cause mortality and stroke recur­ rence rates during follow-up were 139(19%) and 155(21.2%). The me­ dian follow-up time was 57 months, and the maximum follow-up time was up 138 months. The average age was 61.25 ± 12.99 years, of which 61.7% were men. Table 1 describes the baseline characteristics and outcomes of included subjects. Vascular risk factors 3.2. Trajectories of QoL The specified models considered equally spaced time points. The results of the fit indices for the models with 1–6 physical trajectories are given in Table 2. The 5-trajectory model (1 intercept and 4 quadratic) (Table S1) with physical QoL is the most superior according to BIC, AIC, and average posterior probability: The Persistently Poor trajectory (14.9%) represents those with consistently low scores; the PoorImproved trajectory (20.5%) refers to those whose scores were similar to the Persistently Poor trajectory at initial presentation but steadily increased; the Poor-Acutely Improved trajectory (28.7%) indicates those who initially performance with similar score levels to the Persistently Poor trajectory but with a sharp increase; the Moderate-Impaired tra­ jectory (13.2%) indicates those who scored the same as the ModerateImproved trajectory at initial presentation but declined; and the Moderate-Improved trajectory (22.8%) indicated those who scored slightly below 50 at initial presentation but had a sustained increase to above 50 (Fig. 1 and Supplementary Table S2). The results of the fit indices for the models with 1–6 mental QoL trajectories are given in Table 3. The 5-trajectory model (1 intercept and 4 quadratic) (Table S3) with mental QoL is superior: The Poor-Improved trajectory (9.5%) refers to those who scored low at the initial presen­ tation but steadily increased to near 50; the Moderate-Impaired trajec­ tory (5.2%) indicates those who scored slightly below 50 at first presentation but consistently declined; the Moderate-Improved trajec­ tory (33.4%) indicated those who scored slightly below 50 at initial presentation but had a sustained increase to above 50; the GoodImpaired trajectory (23.9%) indicates those who had scores levels similar to the Persistently Good trajectory at initial presentation but declined; and the Persistently Good trajectory (28.0%) those whose scores had remained stable at about 58 (Fig. 2 and Supplementary Table S4). Stroke characteristics Stroke outcomes Sex, n (%) Male Female Marital status, n (%) Married Single Educational level, n (%) ≤6 years 7–9 years 10–12 years ≥12 years Annual household income, n (%) ≤¥20,000 ¥20,001≥¥50,000 Smoking status, n (%) No Yes Drinking status, n (%) No Yes Physical activity, n (%) No Yes BMI (kg/m2) Mean ± SD Median(Q1,Q3) Hypertension, n (%) No Yes Diabetes, n (%) No Yes Hyperlipidemia, n (%) No Yes Heart disease, n (%) No Yes TOAST, n (%) LAA SAO CE mRS score > 1 at arrival, n (%) No Yes Side of brain damage, n (%) LHD RHD BHD Other Recurrent, n (%) No Yes Mortality, n (%) No Yes Values 61.25 ± 12.99 62.00(53.00, 71.00) 452(61.7) 281(38.3) 641(87.4) 92(12.6) 262(35.7) 216(29.5) 134(18.3) 121(16.5) 219(29.9) 300(40.9) 214(29.2) 417(56.9) 316(43.1) 445(60.7) 288(39.3) 392(53.5) 341(46.5) 23.9 ± 4.2 23.7(21.3, 26) 278(37.9) 455(62.1) 518(70.7) 215(29.3) 500(68.2) 233(31.8) 571(77.9) 162(22.1) 388(52.9) 243(33.2) 102(13.9) 169(23.1) 564(76.9) 244(33.3) 233(31.8) 106(14.5) 150(20.5) 578(78.9) 155(21.2) 594(81.0) 139(19.0) SD: standard deviation; Q1: first quartile; Q3: third quartile; BMI: body mass index; TOAST: trial of org 10,172 in acute stroke treatment; LAA: large-artery atherosclerosis; SAO: small-artery occlusion; CE: cardio-embolism; mRS: modi­ fied rankin score; LHD: left hemisphere damage; RHD: right hemisphere dam­ age; BHD: bilateral hemisphere damage; Other: side of brain damage is uncertain. in each trajectory group for physical and mental QoL. The physical Moderate-Improved group was relatively younger (median, 59 years) with a high proportion of SAO (37.1%), and the group had the lowest proportion of mRS score > 1 at arrival (34.7%). The mental Persistently- 3.3. Trajectory sub-population characteristics Table 4 and Table 5 display the baseline characteristics of individuals 3 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Persistently Poor trajectory, HR: 2.19 (95% CI:1.10,4.34) p = 0.02; in the Moderate-Impaired trajectory of physical QoL, HR: 2.33 (95% CI: 1.28,4.24) p = 0.01. The increased risk of recurrence in the PoorImproved trajectory and the Poor-Acutely Improved trajectory of physical QoL was not observed, HR: 1.56 (95% CI: 0.83,2.94) p = 0.17 and 1.35 ((95% CI: 0.75,2.44) p = 0.32. None of the mental trajectories showed an association with recurrence. Table 2 Fit statistics for trajectories of physical QoL. Number of classes BIC AIC Class proportion APP 1 2 3 − 8125.92 − 7870.73 − 7808.33 − 8116.73 − 7854.64 − 7785.35 100% 33.8%, 66.2% 29.1%, 37.5%,33.4% 4 − 7774.16 − 7739.69 5 ¡7732.00 ¡7690.62 13.8%, 31.0%, 24.6%, 30.7% 14.9%, 13.2%, 20.5%, 28.7%, 22.8% 6 − 7739.03 − 7695.35 1 0.91, 0.94 0.89, 0.81, 0.85 0.88, 0.81, 0.81, 0.87 0.89, 0.77, 0.80, 0.82, 0.88 0.89, 0.76, 0.80, 0.84, 0.88 14.9%, 13.6%, 20.3%, 30.8%, 20.3%, 0.0% 3.5. Sensitivity analyses The shape of each trajectory and the proportion of the sample included varied slightly due to changes in sample size (n = 666) (Sup­ plementary Fig. S2, Fig. S3), the point estimates of QoL are shown in Table S5 and Table S6. Trends in quality-of-life changes in each trajec­ tory and the association of each trajectory with prognosis remained consistent with the primary analysis (Supplementary Table S7). BIC: Bayesian information criteria; AIC: Akaike's information criterion; APP: average posterior probability. 4. Discussion Good age group was similar to others (median, 62 years). This group had the highest proportion of SAO (45.4%), and the group had the relatively lower proportion of mRS score > 1 at arrival (67.8%). Our study suggests distinct trajectories for both physical and mental QoL in stroke patients during the first six months. We identified five physical trajectories: Persistently Poor, Poor-Improved, Poor-Acutely 3.4. Trajectories of QoL after stroke and long-term prognosis Table 3 Fit statistics for trajectories of mental QoL. Patients' physical QoL trajectories and mental QoL trajectories showed different associations with all-cause mortality risk (Table 6). Compared to the Moderate-Improved trajectory of physical QoL, the risk of death was increased in the Persistently Poor trajectory, HR: 2.78 (95% CI: 1.25,6.19) p = 0.01; in the Poor-Improved trajectory of physical QoL, HR: 2.39 (95% CI: 1.14,5.02) p = 0.02. The increased risk of death in the Poor-Acutely Improved trajectory of physical QoL was not observed, HR: 1.53 (95% CI: 0.74,3.19) p = 0.25. Increased risk of death was not observed in the Moderate-Impaired trajectory of physical QoL after adjustment for recurrence, HR: 2.03 (95% CI: 0.93,4.44) p = 0.08. The risk of death was significantly increased in the Moderate-Impaired tra­ jectory of mental QoL, HR: 2.48 (95% CI: 1.21,5.07) p = 0.01. An increased risk of death in the other mental trajectories was not observed. Patients' physical QoL trajectories showed different associations with stroke recurrence (Table 6). Compared to the Moderate-Improved tra­ jectory of physical QoL, the risk of recurrence was increased in the Number of classes BIC AIC Class proportion APP 1 2 3 − 7848.85 − 7753.21 − 7706.53 − 7841.95 − 7734.82 − 7681.24 4 − 7691.21 − 7659.03 5 ¡7665.47 ¡7624.10 100% 14.7%, 85.3% 12.4%, 13.9%, 73.7% 4.2%, 15.8%, 18.1%, 61.8% 5.2%, 9.5%, 23.9%, 33.4%, 28.0% 6 − 7664.09 − 7620.41 1 0.84, 0.95 0.86, 0.78, 0.90 0.79, 0.75, 0.79, 0.87 0.90, 0.77, 0.78, 0.73, 0.78 0.78, 0.98, 0.82, 0.70, 0.69, 0.79 7.0%, 1.0%, 9.3%, 18.6%, 30.4%, 33.8% BIC: Bayesian information criteria; AIC: Akaike's information criterion; APP: average posterior probability. Fig. 1. Trajectory grouping of physical QoL during the first 6 months for 733 participants. QoL means quality of life. 4 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Fig. 2. Trajectory grouping of mental QoL during the first 6 months for 733 participants. QoL means quality of life. physical health. Change in QoL was associated with long-term survival. Failure of the physical QoL score to return to 50 may be associated with an increased risk of all-cause death in patients with first-ever stroke - but only one of 2 trajectory patterns was associated with an increased risk of death. The Poor-Improved trajectory failed to return to the general population level at six months. The risk of all-cause death was increased compared with the Moderate-Improved trajectory. In previous studies on the long-term outcome of stroke, stroke patients with physical difficulties such as poor physical function [37] or physical pain [38]have a higher risk of death. On the other hand, patients with Moderate-Impaired trajectory have not poor basic physical QoL, and the risk of all-cause mortality did not in­ crease (Table 6 and Supplementary Table S7). In a study focusing on the long-term outcome after stroke, the 7-year mortality rate of patients who were judged to be moderately disabled at three months did not increase compared with patients without disabilities [39]. It may be related to the fact that the neurological impairments scores of the two groups of patients at baseline were not poor, which is consistent with our result. The decrease in mental score to a low level is related to the increased risk of all-cause death in stroke patients. The score of the Moderate-Impaired trajectory was moderate at baseline and decreased to about 30 at six months. The risk of all-cause death increased compared with the Moderate-Improved trajectory. Past studies have shown that patients with impaired mental health, such as depression, insufficient energy, and other mental health diagnoses after stroke, have a higher mortality rate [40,41]. Patients with impaired mental health are difficult to get out of the attack of illness, which is bad for the long-term prognosis of patients. The prevention of recurrent strokes might rely more on improving patients' physical QoL. Compared with the Moderate-Improved trajec­ tory, the physical Moderate-Impaired trajectory has an increased risk of recurrence, but the mental Moderate-Impaired trajectory did not show an increased risk of recurrence. We did not observe that the risk of recurrence of any mental trajectory was higher than that of the control trajectory. Previous studies have reported that the prevalence of poststroke anxiety is 25%, and the association between 3-month anxiety and stroke recurrence was not significant during the 10-year follow-up period [42]. Some studies with limited time data (<2 years) have linked post-stroke depression (PSD) with recurrence rates [43,44], but results are not entirely consistent in longer-term and larger sample-size Improved, Moderate-Impaired, and Moderate-Improved. Trajectories identified for mental QoL were: Poor-Improved, Moderate-Impaired, Moderate-Improved, Good-Impaired, and Persistently Good. Short-term improvement in QoL can translate into substantial benefits for the longterm survival of patients. Interventions focused on stroke survivors with impaired physical QoL may reduce poststroke recurrence. The evolution of the health status of stroke patients is often un­ known, especially in the first six months after stroke. The study showed that patients' QoL changed in the first six months after stroke and was more stable after three months. It was aligned with the recovery time frame of physical functions and activities after stroke. Most functional recovery occurs in the first six months after stroke, and the recovery reaches the plateau stage three to six months after stroke [29]. Mental adaptation was in accord with the time frame of healing of physical functions. The tremendous benefits of recovery after injury occur within a limited time window, which can be supported by animal research evidence. An ischemic injury will trigger a series of genetic, molecular, cellular, and electrophysiological events that promote nerve recovery [30,31]. The QoL monitoring conducted by health care providers for patients in the first six months after stroke can obtain sufficient health information to help hospitalized or discharged patients. Still, these data have not been routinely collected [32]. Resilience is common; treatment is still needed, especially the re­ covery of physical health. It can be found by observing the trajectory of physical and mental trajectories that many patients showed a positive promotion and finally maintained a high level. Bonanno et al. proposed that most people can deal with trauma well [33], which was consistent with our results; trajectories were mainly characterized by recovery and resilience [33]. We also observed low and descent QoL trajectories, which made up about 30% of our total patients, which was in keeping with Mierlo at el (30–37%) [12]. There is no decline in stroke patients from Italy, because they focus on survivors with low to moderate dis­ abilities [13]. The mental QoL of stroke patients seems to recover well. Scores of mental QoL (MCS) after stroke are comparable to that in the general population (50 is the score for the general population), whereas scores of physical QoL (PCS) are worse at the six months (the plateau stage), which is consistent with the results of previous studies focusing on QoL for a longer time [34–36]. In order to achieve a substantial improvement in quality of life, patients still need continuous efforts and appropriate treatment, with a particular focus on the recovery of 5 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Table 4 Patients' characteristics by trajectories of physical QoL (N = 733). Characteristic Age (years) Mean ± SD Median(Q1,Q3) Sex, n (%) Male Female Marital status, n (%) Married Unmarried Educational level, n (%) ≤6 years 7–9 years 10–12 years ≥12 years Annual household income, n (%) ≤¥20,000 ¥20,001≥¥50,000 Smoking status, n (%) No Yes Drinking status, n (%) No Yes Physical activity, n (%) No Yes BMI (kg/m2) Mean ± SD Median(Q1,Q3) Hypertension, n (%) No Yes Diabetes, n (%) No Yes Hyperlipidemia, n (%) No Yes Heart disease, n (%) No Yes TOAST, n (%) LAA SAO CE mRS score > 1 at arrival, n (%) No Yes Side of brain damage, n (%) LHD RHD BHD Other Recurrent, n (%) No Yes Mortality, n (%) No Yes Trajectories of physical QoL Persistently Poor(n = 109) Poor-Improved(n = 150) Poor-Acutely Improved (n = 210) Moderate-Impaired(n = 97) Moderate-Improved (n = 167) 65.67 ± 12.78 65.00(56.00,77.00) 62.50 ± 11.51 63.00(56.00,69.00) 60.17 ± 13.31 61.50(50.00,71.00) 61.88 ± 13.10 63.00(54.00,72.00) 58.25 ± 13.10 59.00(49.00,68.00) 45(41.3) 64(58.7) 93(62.0) 57(38.0) 143(68.1) 67(31.9) 62(63.9) 35(36.1) 109(65.3) 58(34.7) 84(77.1) 25(22.9) 134(89.3) 16(10.7) 182(86.7) 28(13.3) 87(89.7) 10(10.3) 154(92.2) 13(7.8) 52(47.7) 26(23.9) 18(16.5) 13(11.9) 59(39.3) 45(30.0) 27(18.0) 19(12.7) 75(35.7) 63(30.0) 39(18.6) 33(15.7) 30(30.9) 37(38.1) 17(17.5) 13(13.4) 46(27.5) 45(26.9) 33(19.8) 43(25.7) 38(34.9) 38(34.9) 33(30.3) 49(32.7) 72(48.0) 29(19.3) 55(26.2) 86(41.0) 69(32.9) 38(39.2) 37(38.1) 22(22.7) 39(23.4) 67(40.1) 61(36.5) 80(73.4) 29(26.6) 84(56.0) 66(44.0) 106(50.5) 104(49.5) 51(52.6) 46(47.4) 96(57.5) 71(42.5) 79(72.5) 30(27.5) 91(60.7) 59(39.3) 117(55.7) 93(44.3) 64(66.0) 33(34.0) 94(56.3) 73(43.7) 53(48.6) 56(51.4) 89(59.3) 61(40.7) 113(53.8) 97(46.2) 49(50.5) 48(49.5) 88(52.7) 79(47.3) 23.6 ± 4.1 23.4(20.8,26) 23.7 ± 4 23.9(21.2,25.5) 24.2 ± 5.1 23.6(21.3,26) 23.7 ± 3.9 23.3(21.1,25.6) 24.1 ± 3.5 23.9(21.8,26.3) 37(33.9) 72(66.1) 65(43.3) 85(56.7) 67(31.9) 143(68.1) 39(40.2) 58(59.8) 70(41.9) 97(58.1) 73(67.0) 36(33.0) 106(70.7) 44(29.3) 151(71.9) 59(28.1) 70(72.2) 27(27.8) 118(70.7) 49(29.3) 80(73.4) 29(26.6) 108(72) 42(28.0) 142(67.6) 68(32.4) 62(63.9) 35(36.1) 108(64.7) 59(35.3) 76(69.7) 33(30.3) 112(74.7) 38(25.3) 166(79.0) 44(21.0) 81(83.5) 16(16.5) 136(81.4) 31(18.6) 66(60.6) 26(23.9) 17(15.6) 85(56.7) 37(24.7) 28(18.7) 103(49.0) 84(40.0) 23(11.0) 47(48.5) 34(35.1) 16(16.5) 87(52.1) 62(37.1) 18(10.8) P value* <0.001 <0.001 0.004 0.01 0.01 0.003 0.03 0.48 0.64 0.13 0.91 0.38 0.08 0.02 <0.001 3(2.8) 106(97.2) 5(3.3) 145(96.7) 25(11.9) 185(88.1) 27(27.8) 70(72.2) 109(65.3) 58(34.7) 31(28.4) 41(37.6) 13(11.9) 24(22.0) 45(30) 47(31.3) 21(14.0) 37(24.7) 67(31.9) 65(31.0) 32(15.2) 46(21.9) 39(40.2) 30(30.9) 15(15.5) 13(13.4) 62(37.1) 50(29.9) 25(15.0) 30(18.0) 80(73.4) 29(26.6) 116(77.3) 34(22.7) 168(80.0) 42(20.0) 68(70.1) 29(29.9) 146(87.4) 21(12.6) 76(69.7) 33(30.3) 109(72.7) 41(27.3) 179(85.2) 31(14.8) 76(78.4) 21(21.6) 154(92.2) 13(7.8) 0.60 0.01 <0.001 SD: standard deviation; Q1: first quartile; Q3: third quartile; QoL: quality of life; BMI: body mass index; TOAST: trial of org 10,172 in acute stroke treatment; LAA: large-artery atherosclerosis; SAO: small-artery occlusion; CE: cardio-embolism; mRS: modified rankin score; LHD: left hemisphere damage; RHD: right hemisphere damage; BHD: bilateral hemisphere damage; Other: side of brain damage is uncertain. * Chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables. studies [45,46]. Depression (HR: 1.68 (1.07 to 2.63)) was reported to be associated with stroke recurrence in a 12-year follow-up study, but no variables representing physical health (the degree of disability, self-care ability, etc) were included in the multivariate model [45]. In another study, the Barthel index, which determine the basic activities of daily living ability of stroke patients, was included in the adjusted model, and no association was found between patients with depression at three months (HR: 0.98 (0.60 to 1.62)) and the risk of recurrence 5 years later, 6 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Table 5 Patients' characteristics by trajectories of mental QoL (N = 733). Characteristic Age (years) Mean ± SD Median(Q1,Q3) Sex, n (%) Male Female Marital status, n (%) Married Unmarried Educational level, n (%) ≤6 years 7–9 years 10–12 years ≥12 years Annual household income, n (%) ≤¥20,000 ¥20,001≥¥50,000 Smoking status, n (%) No Yes Drinking status, n (%) No Yes Physical activity, n (%) No Yes BMI (kg/m2) Mean ± SD Median(Q1,Q3) Hypertension, n (%) No Yes Diabetes, n (%) No Yes Hyperlipidemia, n (%) No Yes Heart disease, n (%) No Yes TOAST, n (%) LAA SAO CE mRS score > 1 at arrival, n (%) No Yes Side of brain damage, n (%) LHD RHD BHD Other Recurrent, n (%) No Yes Mortality, n (%) No Yes Trajectory of mental QoL Poor-Improved (n = 70) Moderate-Impaired (n = 38) Moderate-Improved (n = 245) Good-Impaired (n = 175) Persistently Good(n = 205) 60.14 ± 13.78 61.00(52.00,68.00) 65.37 ± 13.79 66.50(56.00,79.00) 60.54 ± 12.58 61.00(50.00,70.00) 62.26 ± 12.21 63.00(55.00,72.00) 60.85 ± 13.61 62.00(53.00,71.00) 38(54.3) 32(45.7) 24(63.2) 14(36.8) 157(64.1) 88(35.9) 101(57.7) 74(42.3) 132(64.4) 73(35.6) 59(84.3) 11(15.7) 32(84.2) 6(15.8) 215(87.8) 30(12.2) 150(85.7) 25(14.3) 185(90.2) 20(9.8) 31(44.3) 22(31.4) 10(14.3) 7(10.0) 9(23.7) 12(31.6) 10(26.3) 7(18.4) 79(32.2) 82(33.5) 51(20.8) 33(13.5) 69(39.4) 49(28.0) 31(17.7) 26(14.9) 74(36.1) 51(24.9) 32(15.6) 48(23.4) 19(27.1) 26(37.1) 25(35.7) 11(28.9) 14(36.8) 13(34.2) 65(26.5) 118(48.2) 62(25.3) 61(34.9) 61(34.9) 53(30.3) 63(30.7) 81(39.5) 61(29.8) 37(52.9) 33(47.1) 20(52.6) 18(47.4) 141(57.6) 104(42.4) 102(58.3) 73(41.7) 117(57.1) 88(42.9) 44(62.9) 26(37.1) 23(60.5) 15(39.5) 152(62.0) 93(38.0) 114(65.1) 61(34.9) 112(54.6) 93(45.4) 37(52.9) 33(47.1) 23(60.5) 15(39.5) 133(54.3) 112(45.7) 92(52.6) 83(47.4) 107(52.2) 98(47.8) 23.2 ± 4.1 22.9(20.5,25) 25.1 ± 5.4 24.5(21.3,27.4) 24.0 ± 4.4 23.7(21.1,26.1) 23.8 ± 4 23.5(21.3,25.7) 24.0 ± 3.9 23.9(21.9,26) 31(44.3) 39(55.7) 13(34.2) 25(65.8) 90(36.7) 155(63.3) 57(32.6) 118(67.4) 87(42.4) 118(57.6) 49(70.0) 21(30.0) 28(73.7) 10(26.3) 167(68.2) 78(31.8) 117(66.9) 58(33.1) 157(76.6) 48(23.4) 47(67.1) 23(32.9) 25(65.8) 13(34.2) 170(69.4) 75(30.6) 123(70.3) 52(29.7) 135(65.9) 70(34.1) 54(77.1) 16(22.9) 24(63.2) 14(36.8) 184(75.1) 61(24.9) 144(82.3) 31(17.7) 165(80.5) 40(19.5) 47(67.1) 11(15.7) 12(17.1) 21(55.3) 8(21.1) 9(23.7) 124(50.6) 76(31.0) 45(18.4) 103(58.9) 55(31.4) 17(9.7) 93(45.4) 93(45.4) 19(9.3) 12(17.1) 58(82.9) 6(15.8) 32(84.2) 52(21.2) 193(78.8) 33(18.9) 142(81.1) 66(32.2) 139(67.8) 27(38.6) 20(28.6) 17(24.3) 6(8.6) 15(39.5) 13(34.2) 8(21.1) 2(5.3) 88(35.9) 66(26.9) 34(13.9) 57(23.3) 55(31.4) 58(33.1) 24(13.7) 38(21.7) 59(28.8) 76(37.1) 23(11.2) 47(22.9) 58(82.9) 12(17.1) 32(84.2) 6(15.8) 186(75.9) 59(24.1) 138(78.9) 37(21.1) 164(80.0) 41(20.0) 57(81.4) 13(18.6) 23(60.5) 15(39.5) 205(83.7) 40(16.3) 143(81.7) 32(18.3) 166(81.0) 39(19.0) P value* 0.16 0.40 0.56 0.06 0.23 0.92 0.29 0.91 0.26 0.24 0.23 0.88 0.07 <0.001 0.01 0.01 0.60 0.02 SD: standard deviation; Q1: first quartile; Q3: third quartile; QoL: quality of life; BMI: body mass index; TOAST: trial of org 10,172 in acute stroke treatment; LAA: large-artery atherosclerosis; SAO: small-artery occlusion; CE: cardio-embolism; mRS: modified rankin score; LHD: left hemisphere damage; RHD: right hemisphere damage; BHD: bilateral hemisphere damage; Other: side of brain damage is uncertain. * Chi-square tests for categorical variables and Kruskal-Wallis tests for continuous variables. which was consistent with the results of this study [46]. Mental health may not be an independent risk factor for the recurrence of stroke pa­ tients. The omission of physical variables in the multivariable model overestimates the correlation between mental state and recurrence of stroke patients and requires the attention of researchers. To our knowledge, this is the first study to identify trajectories of physical and mental QoL in the first six months after stroke and to determine the associations between distinct trajectories of QoL and long7 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Table 6 The associations between trajectory groups of QoL and prognosis after stroke. Mortality, HR (95%CI) Trajectories of physical QoL Persistently Poor Poor-Improved Poor-Acutely Improved ModerateImpaired ModerateImproved Trajectories of mental QoL Poor-Improved ModerateImpaired ModerateImproved Good-Impaired Persistently Good Recurrent, HR (95%CI) Model 1 Model 2 Model 3 Model 4 Model 5 Model 1 Model 2 Model 3 Model 4 4.26 (2.17,8.35) 3.46 (1.85,6.49) 1.91 (0.996,3.66) 2.71 (1.34,5.48) 3.24 (1.59,6.57) 2.86 (1.50,5.45) 1.74 (0.91,3.36) 2.38 (1.15,4.92) 3.15 (1.55,6.37) 2.85 (1.49,5.46) 1.73 (0.90,3.35) 2.45 (1.18,5.11) 2.87 (1.29,6.34) 2.40 (1.15,5.01) 1.52 (0.74,3.15) 2.24 (1.04,4.84) 2.78 (1.25,6.19) 2.39 (1.14,5.02) 1.53 (0.74,3.19) 2.03 (0.93,4.44) 2.40 (1.34,4.30) 1.62 (0.93,2.85) 1.43 (0.85,2.43) 2.50 (1.43,4.39) 2.19 (1.17,4.08) 1.50 (0.84,2.66) 1.43 (0.83,2.46) 2.30 (1.28,4.13) 2.20 (1.18,4.11) 1.50 (0.84,2.68) 1.39 (0.81,2.39) 2.27 (1.26,4.1) 2.19 (1.10,4.34) 1.56 (0.83,2.94) 1.35 (0.75,2.44) 2.33 (1.28,4.24) Referent Referent Referent Referent Referent Referent Referent Referent Referent 1.31 (0.69,2.48) 2.76 (1.47,5.19) 1.37 (0.71,2.64) 2.14 (1.09,4.22) 1.38 (0.71,2.69) 2.37 (1.18,4.78) 1.12 (0.56,2.24) 2.28 (1.12,4.66) 1.19 (0.60,2.39) 2.48 (1.21,5.07) 0.65 (0.35,1.2) 0.50 (0.22,1.18) 0.69 (0.37,1.30) 0.54 (0.24,1.26) 0.70 (0.37,1.31) 0.54 (0.24,1.25) 0.79 (0.42,1.46) 0.63 (0.27,1.45) Referent Referent Referent Referent Referent Referent Referent Referent Referent 1.06 (0.66,1.71) 1.03 (0.66,1.62) 1.02 (0.63,1.66) 1.09 (0.68,1.73) 1.11 (0.68,1.82) 1.15 (0.72,1.83) 1.1 (0.67,1.80) 1.18 (0.73,1.90) 1.15 (0.70,1.88) 1.23 (0.76,2.00) 0.77 (0.51,1.15) 0.71 (0.48,1.07) 0.74 (0.49,1.13) 0.69 (0.45,1.06) 0.72 (0.47,1.10) 0.71 (0.46,1.10) 0.72 (0.47,1.09) 0.70 (0.44,1.09) Model 1 is unadjusted. Model 2 is adjusted for age, sex, marital status, education level, annual household income, smoking status, drinking status, physical activity. Model 3 is plus adjusted for BMI, hypertension, diabetes, hyperlipidemia, heart disease. Model 4 is plus adjusted for TOAST, mRS score > 1 at arrival, side of brain damage. Model 5 is plus adjusted for recurrent. QoL: quality of life; HR: hazard ratio; CI: confidence interval. term prognosis in Chinese patients with first-ever ischemic stroke. Stroke survivors face multiple obstacles after a stroke, may lack physical activity, and be accompanied by mental trauma. Therefore, it is neces­ sary to cooperate with the medical team and home care to provide early mobilization and continuous mental care for stroke survivors to prevent the deterioration of the condition and obtain an excellent long-term prognosis. This study had several limitations. First, data were collected from a single center in China, limiting the findings' general­ izability to other countries. However, this is one of the few prospective studies focusing on stroke patients with a large sample size, effective information, and long-term follow-up. Furthermore, we controlled for all observed influences as much as possible, but some important factors still affect patients' QoL, such as pre-stroke depression. Finally, some covariates rely entirely on self-reported data, and family members answering questions that some patients could not do may lead to in­ formation bias. Even with these biases, this study is enough to make us realize that the QoL has not been fully utilized. More research is needed to explore the value of this indicator in influencing clinical decisionmaking and policy-making for stroke patients. Contributors MH, BZ, CZ designed the study. YL, MH, MX and BZ collected part of the data. MH and BZ conducted the analysis. All authors critically revised the manuscript for important intellectual content critically. Funding This research was supported by grants from National Natural Science Foundation of China (grant no. 30600511, no. 81673273, and no. 82173618, http://www.nsfc.gov.cn/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The funding agreement ensured the authors' inde­ pendence in designing the study. Ethics approval The study protocol was approved by the Ethics Committee of the West China Hospital, Sichuan University, Chengdu, China (ethical approval number, “2009 year 50”). 5. Conclusion Patient consent The present study identified five distinct trajectories of physical and mental QoL. Most people can deal with trauma well and show physical and mental health recovery. Interventions that promote physical health and avoid deterioration of mental health during the first six months positively impact long-term survival. Secondary prevention of recurrent strokes relies more on improving patients' physical QoL. The routine data collection of QoL can enable medical care providers to understand the changes in the health status of survivors and provide needed medical services promptly, such as prompt return to the hospital immediately, adjusting the medication plan, and others. It has reference significance for cost-benefit research of stroke treatment, health care planning pol­ icies, and research. All patients had signed informed consent before the baseline survey. We confirmed that all methods were performed in accordance with relevant guidelines and regulations. Provenance and peer review Not commissioned; externally peer reviewed. Declaration of Competing Interest The authors have no competing interests to report. 8 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 Acknowledgments [20] C. Ellis, A.L. Grubaugh, L.E. Egede, Factors associated with SF-12 physical and mental health quality of life scores in adults with stroke, J. Stroke Cerebrovasc. Dis. 22 (4) (2013) 309–317, https://doi.org/10.1016/j. jstrokecerebrovasdis.2011.09.007. [21] J.E. Ware, M.A. Kosinski, S.D. Keller, How to score the SF-12 physical and mental health summary scale, second ed., The Health Institute, New England Medical Center, Boston, 1995. [22] J.E. Ware, M. Kosinski, S.D. Keller, A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity, Med. Care 34 (3) (1996) 220–233, https://doi.org/10.1097/00005650-199603000-00003. [23] A.S. Pickard, J.A. Johnson, A. Penn, F. Lau, T. Noseworthy, Replicability of SF-36 summary scores by the SF-12 in stroke patients, Stroke 30 (6) (1999) 1213–1217, https://doi.org/10.1161/01.str.30.6.1213. [24] A. Wang, Y. Yang, Z. Su, W. Yue, H. Hao, L. Ren, Y. Wang, Y. Cao, Y. Wang, Association of oxidized low-density lipoprotein with prognosis of stroke and stroke subtypes, Stroke 48 (1) (2017) 91–97, https://doi.org/10.1161/ STROKEAHA.116.014816. [25] H. Andruff, N. Carraro, A. Thompson, P. Gaudreau, B. Louvet, Latent class growth modelling: a tutorial, tutorials in quantitative methods for psychology 5 (1) (2009) 11–24, https://doi.org/10.20982/tqmp.05.1.p011. [26] N.E. Mayo, L.K. Fellows, S.C. Scott, J. Cameron, S. Wood-Dauphinee, A longitudinal view of apathy and its impact after stroke, Stroke 40 (10) (2009) 3299–3307, https://doi.org/10.1161/STROKEAHA.109.554410. [27] N.B. Allen, J. Siddique, J.T. Wilkins, C. Shay, C.E. Lewis, D.C. Goff, D.R. Jacobs Jr., K. Liu, D. Lloyd-Jones, Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age, Jama 311 (5) (2014) 490–497, https:// doi.org/10.1001/jama.2013.285122. [28] J.P. Fine, R.J. Gray, A proportional hazards model for the subdistribution of a competing risk, J. Am. Stat. Assoc. 94 (446) (1999) 496–509, https://doi.org/ 10.2307/2670170. [29] G. Kwakkel, B.J. Kollen, Predicting activities after stroke: what is clinically relevant? Int. J. Stroke 8 (1) (2013) 25–32, https://doi.org/10.1111/j.17474949.2012.00967.x. [30] T.H. Murphy, D. Corbett, Plasticity during stroke recovery: from synapse to behaviour, Nat. Rev. Neurosci. 10 (12) (2009) 861–872, https://doi.org/10.1038/ nrn2735. [31] E.R. Coleman, R. Moudgal, K. Lang, H.I. Hyacinth, O.O. Awosika, B.M. Kissela, W. Feng, Early rehabilitation after stroke: a narrative review, Curr. Atheroscler. Rep. 19 (12) (2017) 59, https://doi.org/10.1007/s11883-017-0686-6. [32] S.D. Anker, S. Agewall, M. Borggrefe, M. Calvert, J. Jaime Caro, M.R. Cowie, I. Ford, J.A. Paty, J.P. Riley, K. Swedberg, L. Tavazzi, I. Wiklund, P. Kirchhof, The importance of patient-reported outcomes: a call for their comprehensive integration in cardiovascular clinical trials, Eur. Heart J. 35 (30) (2014) 2001–2009, https://doi.org/10.1093/eurheartj/ehu205. [33] G.A. Bonanno, A.D. Mancini, The human capacity to thrive in the face of potential trauma, Pediatrics 121 (2) (2008) 369–375, https://doi.org/10.1542/peds.20071648. [34] B. Löfgren, Y. Gustafson, L. Nyberg, Psychological well-being 3 years after severe stroke, Stroke 30 (3) (1999) 567–572, https://doi.org/10.1161/01.str.30.3.567. [35] T. van Middelaar, E. Richard, H.B. van der Worp, P. van den Munckhof, P. T. Nieuwkerk, M.C. Visser, J. Stam, P.J. Nederkoorn, Quality of life after surgical decompression for a space-occupying middle cerebral artery infarct: a cohort study, BMC Neurol. 15 (2015) 156, https://doi.org/10.1186/s12883-015-0407-0. [36] M. Hackett, Health-related quality of life among long-term survivors of stroke results from the Auckland stroke study, 1991–1992, Stroke 31 (2) (2000) 440–447, https://doi.org/10.1161/01.str.31.2.440. [37] I.J. Hubbard, K. Vo, P.M. Forder, J.E. Byles, Stroke, physical function, and death over a 15-year period in older Australian women, Stroke 47 (4) (2016) 1060–1067, https://doi.org/10.1161/STROKEAHA.115.011456. [38] W.K. Tang, H. Liang, V. Mok, G.S. Ungvari, K.S. Wong, Is pain associated with suicidality in stroke? Arch. Phys. Med. Rehabil. 94 (5) (2013) 863–866, https:// doi.org/10.1016/j.apmr.2012.11.044. [39] R. Magalhaes, P. Abreu, M. Correia, W. Whiteley, M.C. Silva, P. Sandercock, Functional status three months after the first ischemic stroke is associated with long-term outcome: data from a community-based cohort, Cerebrovasc. Dis. 38 (1) (2014) 46–54, https://doi.org/10.1159/000364938. [40] L.S. Williams, S.S. Ghose, R.W. Swindle, Depression and other mental health diagnoses increase mortality risk after ischemic stroke, Am. J. Psychiatry 161 (6) (2004) 1090–1095, https://doi.org/10.1176/appi.ajp.161.6.1090. [41] E.L. Glader, B. Stegmayr, K. Asplund, Poststroke fatigue: a 2-year follow-up study of stroke patients in Sweden, Stroke 33 (5) (2002) 1327–1333, https://doi.org/ 10.1161/01.str.0000014248.28711.d6. [42] L. Ayerbe, S.A. Ayis, S. Crichton, C.D. Wolfe, A.G. Rudd, Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: the South London stroke register, Age Ageing 43 (4) (2014) 542–547, https://doi.org/10.1093/ ageing/aft208. [43] J.T. Jiao, C. Cheng, Y.J. Ma, J. Huang, M.C. Dai, C. Jiang, C. Wang, J.F. Shao, Association between inflammatory cytokines and the risk of post-stroke depression, and the effect of depression on outcomes of patients with ischemic stroke in a 2year prospective study, Exp. Ther. Med. 12 (3) (2016) 1591–1598, https://doi.org/ 10.3892/etm.2016.3494. We thank all patients, and healthcare professionals involved. Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi. org/10.1016/j.jpsychores.2023.111466. References [1] V.L. Feigin, G. Nguyen, K. Cercy, C.O. Johnson, T. Alam, P.G. Parmar, A. A. Abajobir, K.H. Abate, F. Abd-Allah, et al., G.B.D.L.R.o.S. Collaborators, Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016, N. Engl. J. Med. 379 (25) (2018) 2429–2437, https://doi.org/10.1056/NEJMoa1804492. [2] C.O. Johnson, M. Nguyen, G.A. Roth, E. Nichols, T. Alam, D. Abate, F. Abd-Allah, A. Abdelalim, H.N. Abraha, N.M.E. Abu-Rmeileh, et al., Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the global burden of disease study 2016, Lancet Neurol. 18 (5) (2019) 439–458, https://doi.org/ 10.1016/s1474-4422(19)30034-1. [3] C. Haacke, A. Althaus, A. Spottke, U. Siebert, T. Back, R. Dodel, Long-term outcome after stroke: evaluating health-related quality of life using utility measurements, Stroke 37 (1) (2006) 193–198, https://doi.org/10.1161/01. STR.0000196990.69412.fb. [4] M. Baumann, E. Le Bihan, K. Chau, N. Chau, Associations between quality of life and socioeconomic factors, functional impairments and dissatisfaction with received information and home-care services among survivors living at home two years after stroke onset, BMC Neurol. 14 (2014) 92, https://doi.org/10.1186/ 1471-2377-14-92. [5] M.J.M. Ramos-Lima, I.C. Brasileiro, T.L. Lima, P. Braga-Neto, Quality of life after stroke: impact of clinical and sociodemographic factors, Clinics (Sao Paulo) 73 (2018), e418, https://doi.org/10.6061/clinics/2017/e418. [6] S. Rachpukdee, N. Howteerakul, N. Suwannapong, S. Tang-Aroonsin, Quality of life of stroke survivors: a 3-month follow-up study, J. Stroke Cerebrovasc. Dis. 22 (7) (2013) e70–e78, https://doi.org/10.1016/j.jstrokecerebrovasdis.2012.05.005. [7] S. Ayis, I. Wellwood, A.G. Rudd, C. McKevitt, D. Parkin, C.D. Wolfe, Variations in health-related quality of life (HRQoL) and survival 1 year after stroke: five European population-based registers, BMJ Open 5 (6) (2015), e007101, https:// doi.org/10.1136/bmjopen-2014-007101. [8] I.H. Suenkeler, M. Nowak, B.R. Misselwitz, C. Kugler, W. Schreiber, W.H. Oertel, T. Back, Timecourse of health-related quality of life as determined 3, 6 and 12 months after stroke, J. Neurol. 249 (9) (2002) 1160–1167, https://doi.org/ 10.1007/s00415-002-0792-3. [9] O.M. Ronning, K. Stavem, Determinants of change in quality of life from 1 to 6 months following acute stroke, Cerebrovasc. Dis. 25 (1–2) (2008) 67–73, https:// doi.org/10.1159/000111524. [10] G. Robinson-Smith, M.V. Johnston, J. Allen, Self-care self-efficacy, quality of life, and depression after stroke, Arch. Phys. Med. Rehabil. 81 (4) (2000) 460–464, https://doi.org/10.1053/mr.2000.3863. [11] W.M. Hopman, J. Verner, Quality of life during and after inpatient stroke rehabilitation, Stroke 34 (3) (2003) 801–805, https://doi.org/10.1161/01. STR.0000057978.15397.6F. [12] M. van Mierlo, C. van Heugten, M.W.M. Post, T. Hoekstra, A. Visser-Meily, Trajectories of health-related quality of life after stroke: results from a one-year prospective cohort study, Disabil. Rehabil. 40 (9) (2018) 997–1006, https://doi. org/10.1080/09638288.2017.1292320. [13] G. Pucciarelli, C.S. Lee, K.S. Lyons, S. Simeone, R. Alvaro, E. Vellone, Quality of life trajectories among stroke survivors and the related changes in caregiver outcomes: a growth mixture study, Arch. Phys. Med. Rehabil. 100 (3) (2019) 433–440, e1, htt ps://doi.org/10.1016/j.apmr.2018.07.428. [14] L.P. Larsen, S.P. Johnsen, G. Andersen, N.H. Hjollund, Determinants of health status after stroke: a cohort study with repeated measurements, Clin. Epidemiol. 12 (2020) 1269–1279, https://doi.org/10.2147/CLEP.S270249. [15] The World Health Organization MONICA project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA project principal investigators, J. Clin. Epidemiol. 41 (2) (1988) 105–114, https://doi.org/10.1016/0895-4356(88)90084-4. [16] C.H. Shah, J.D. Brown, Reliability and validity of the short-form 12 item version 2 (SF-12v2) health-related quality of life survey and disutilities associated with relevant conditions in the U.S. older adult population, J. Clin. Med. 9 (3) (2020) 661, https://doi.org/10.3390/jcm9030661. [17] C.L. Lam, E.Y. Tse, B. Gandek, Is the standard SF-12 health survey valid and equivalent for a Chinese population? Qual. Life Res. 14 (2) (2005) 539–547, https://doi.org/10.1007/s11136-004-0704-3. [18] E.T. Lam, C.L. Lam, D.Y. Fong, W.W. Huang, Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J. Eval. Clin. Pract. 19 (1) (2013) 200–208, https://doi.org/10.1111/ j.1365-2753.2011.01800.x. [19] G. Howard, M.M. Safford, J.F. Meschia, C.S. Moy, V.J. Howard, L. Pulley, C. R. Gomez, M. Crowther, Stroke symptoms in individuals reporting no prior stroke or transient ischemic attack are associated with a decrease in indices of mental and physical functioning, Stroke 38 (9) (2007) 2446–2452, https://doi.org/10.1161/ STROKEAHA.106.478032. 9 M. Hu et al. Journal of Psychosomatic Research 173 (2023) 111466 [44] S. Yu, H. Arima, C. Bertmar, Y. Hirakawa, M. Priglinger, K. Evans, M. Krause, Depression but not anxiety predicts recurrent cerebrovascular events, Acta Neurol. Scand. 134 (1) (2016) 29–34, https://doi.org/10.1111/ane.12503. [45] G. Sibolt, S. Curtze, S. Melkas, T. Pohjasvaara, M. Kaste, P.J. Karhunen, N. K. Oksala, R. Vataja, T. Erkinjuntti, Post-stroke depression and depressionexecutive dysfunction syndrome are associated with recurrence of ischaemic stroke, Cerebrovasc. Dis. 36 (5–6) (2013) 336–343, https://doi.org/10.1159/ 000355145. [46] L. Ayerbe, S. Ayis, S. Crichton, C.D. Wolfe, A.G. Rudd, The long-term outcomes of depression up to 10 years after stroke; the South London stroke register, J. Neurol. Neurosurg. Psychiatry 85 (5) (2014) 514–521, https://doi.org/10.1136/jnnp2013-306448. 10