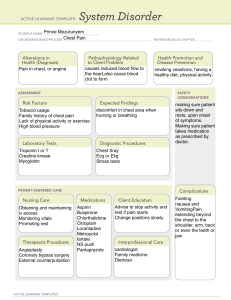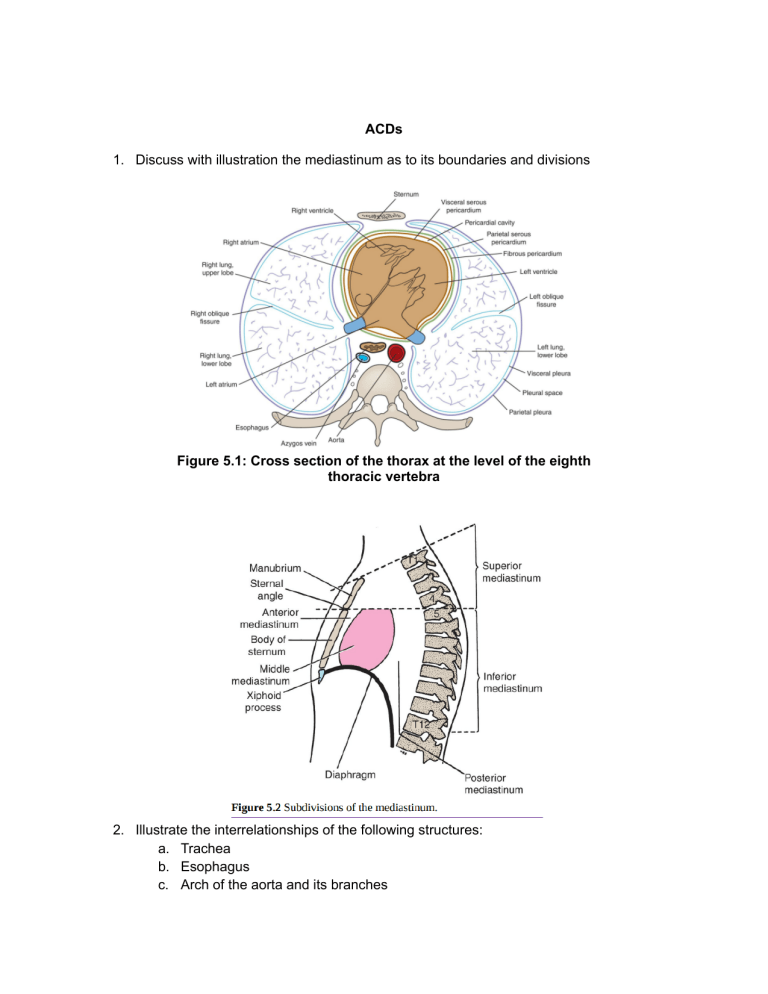
ACDs 1. Discuss with illustration the mediastinum as to its boundaries and divisions Figure 5.1: Cross section of the thorax at the level of the eighth thoracic vertebra 2. Illustrate the interrelationships of the following structures: a. Trachea b. Esophagus c. Arch of the aorta and its branches d. Brachiocephalic vein e. Vagus nerve & Left recurrent laryngeal nerve f. Phrenic nerve g. Thoracic Duct 3. Discuss the formation / origin, commencement, termination, course, branches / tributaries of the following vessels: a. Arch of the aorta b. Brachiocephalic artery c. Left and Right brachiocephalic veins d. Superior Vena Cava 4. Discuss the vagus nerve as to its course, component fibers, branches, area of distribution, and its spatial relationship in the superior mediastinum a. Course b. Component fibers c. Branches and Distribution d. Spatial relationship 5. Discuss the phrenic nerve as to its formation, component fibers, course in the superior mediastinum, and areas of distribution 6. Discuss the thymus gland as to its location, vascular supply, and clinical significance CASES CASE 1 A 67-year-old male known case of small cell cancer at the right upper-lung lobe (Figure 1) consulted because of neck swelling (noted in the morning), dilated neck veins, and purplish discoloration across his chest (Figure 2). On PE, vital signs were: BP 124/64, RR 20, CR 72 regular, Temp 37.0 °C. There was noted diffuse neck edema, engorged vessels on the neck, chest, and sublingual areas. The left upper extremity was also edematous. CT scan was requested and confirmed the diagnosis of SVC syndrome. Guide questions: 1. What is superior vena cava syndrome? 2. Give the anatomical basis for the following: a. edema of the face and purplish discoloration in the chest b. engorged blood vessels on the neck, chest and under the tongue c. diffuse edema in the neck, edema in the left upper extremity CASE 2 A 25 year old patient was referred for evaluation of an incidental finding of a 5.0 × 2.5 cm anterior mediastinal mass with rim-like calcification (Figure 1) on chest radiograph that was requested as part of his pre-employment medical assessment. Patient was asymptomatic and denied any comorbidities. Guide questions: 1. What are the boundaries of the anterior mediastinum? 2. What are the structures located in the anterior mediastinum that may explain the calcified mass? CASE 3 Baby C, who underwent surgical ligation of his PDA, had a complicated post-operative course because of recurrent aspiration pneumonia which developed after the initiation of oral feeding. He likewise had a weak cry and feeding difficulties, prompting an ENT specialist referral. Flexible laryngoscopy was done which revealed left vocal fold paralysis on the patient’s 99th day of life. The left vocal fold was noted to be in the paramedian position, while the right vocal fold was grossly normal. Guide questions: 1. What is patent ductus arteriosus? 2. Will the endoscopic findings explain the weak cry, feeding difficulties, and recurrent aspiration pneumonia of the patient? 3. What is the probable cause and anatomical basis of the abnormal position of the left vocal fold? CASE 4 An 81-year-old male consulted due to acute hoarseness of voice. Physical examination of cardiovascular and neurologic systems was normal. Further evaluation with a nasoendoscope revealed a left vocal cord palsy. Chest Xray revealed an aortic arch aneurysm. Guide Questions: 1. What is aortic arch aneurysm? 2. Why will the patient have hoarseness? 3. Look closely at the trachea and primary bronchi on the Chest X-ray. What do you observe?