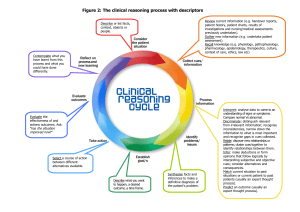
2: History-taking skills Station 2 History-taking skills Contents Introduction to history-taking skills Clinical reasoning The traditional medical history model Incorporating the patient’s perspective – ideas, concerns and expectations History-taking skills – the communication skills that make history taking effective The traditional model and communication skills – putting these together Cases Respiratory problems 2.1 Breathlessness and other respiratory symptoms 2.2 Asthma Abdominal problems 2.3 Dyspepsia and upper gastrointestinal bleeding 2.4 Dysphagia 2.5 Abdominal pain 2.6 Altered bowel habit and lower gastrointestinal bleeding Cardiovascular problems 2.7 Weight gain, obesity, and prevention of cardiovascular disease 2.8 Chest pain and stable angina 2.9 Acute coronary syndrome 2.10 Heart failure 2.11 Palpitations 2.12 Atrial fibrillation 2.13 Dyslipidaemia 2.14 Hypertension Neurological problems 2.15 Headache 2.16 Transient ischaemic attack 2.17 Weakness and wasting 2.18 Multiple sclerosis 2.19 Tremor Rheumatological problems 2.20 Back pain and osteoporosis 2.21 Joint pain Endocrine problems 2.22 Type 1 diabetes mellitus 2.23 Type 2 diabetes mellitus Eye problems 2.24 Visual loss Renal and metabolic problems 2.25 Acute kidney injury 2.26 Chronic kidney disease 2.27 Glomerulonephritis 2.28 Systemic vasculitis 2.29 Hypercalcaemia 2.30 Hyponatraemia 2.31 Poisoning and metabolic disturbance Haematological problems 2.32 Anaemia 2.33 Sickle cell disease and thalassaemia 2.34 Purpura 2.35 Haemophilia 2.36 Deep vein thrombosis 2.37 Thrombophilic tendency 2.38 Myeloma Other problems in acute and general medicine and elderly care 2.39 Human immunodeficiency virus infection 2.40 Falls 2.41 Syncope 2.42 Seizures 2.43 Delirium and acute confusion 2.44 Mild cognitive impairment and dementia 2.45 Incontinence 2.46 Raised inflammatory markers 2.47 Polymyalgia and giant cell arteritis 2.48 Pyrexia and sepsis 2.49 Weight loss and malignancy 2.50 Tiredness Introduction to history-taking skills Clinical reasoning Clinical reasoning – what it is Clinical or diagnostic reasoning is about: • Identifying relevant clinical information • Interpreting its meaning • Establishing a working diagnosis. The traditional medical history model (Box 2.1) aims, through many questions, to converge gradually towards a diagnosis. Alternative models tend to be based upon, or at least incorporate, communication skills. Box 2.1 The traditional medical history model Presenting complaint or complaints • Identification of the main symptoms – what is wrong and why the patient is in hospital History of presenting complaint or complaints • Eliciting symptoms (and consideration of possible causes for each symptom or possible risk factors and complications if a diagnosis is likely) • Enquiring about investigations and treatments to date Past medical history • Eliciting a list of active and past problems Drug and allergy history • Drugs past and present Family history • Often neglected, but often relevant Personal and social history A personal and social history might explore such details as: • Marital status and health of spouse or partner • Other family members and relevant medical problems • Involvement of family and external support services • Description of accomodation, e.g. flat with lift, house with stairs • Current and past occupation / s and effects of work on symptoms and effects of symptoms on work • Support from friends • Interests and hobbies, including the effects of illness on the quality of these • Alcohol intake, cigarette smoking and recreational drug use • Quality of life • Major effects of illness viewed by patient • Activities of daily living, e.g. bathing, dressing, shopping, cooking and sleep Systems review • Excluding other symptoms through a systems review Clinical reasoning strategies Various strategies can be used to get to the diagnosis. Three main ones are hypotheticodeductive reasoning, scheme-inductive reasoning and pattern recognition. Imagine three diagnosticians presented with a four-legged animal. Diagnostician 1 thinks it is a zebra because it looks like one. Diagnostician 2 agrees it is a zebra because it has hooves and stripes and weighs around 300 kg. Diagnostician 3 is from the North Pole and has only ever seen Arctic animals before; he agrees it might be zebra, but also thinks it might be a giraffe because of its hooves or a tiger because of its stripes. Hypothetico-deductive reasoning Diagnostician 3 will take some time reaching the diagnosis. He has little knowledge, and would approach the problem by identifying all relevant information, interpreting it, generating hypotheses and testing these. It is the traditional history taking–examination–investigation approach, converging to the diagnosis. It emphasises depth of data collection at the expense of more focused, structured enquiry. Scheme-inductive reasoning Diagnostician 2 got to the diagnosis through logic. He has some relevant knowledge and used a scheme or structure that reflected it. It is often an algorithmic approach. Pattern recognition Diagnostician 1 got to the diagnosis quickly, through experience. She has relevant knowledge. The ‘problem’ leads to the diagnosis, turning upside down the pyramid that is hypotheticodeductive reasoning. With experience, data are gathered more selectively from the unstructured mass of information. But the evidence is that it takes around 10 years in any field to move from novice to expert, and that experts use pattern recognition successfully most of the time, but when it does not work they must default to a framework. In PACES, you probably lie somewhere between novice and expert, but closer to expert. What is not in doubt is that you should be thinking about the data you are gathering during history taking, and relating it to the patient’s problem. The traditional medical history model The traditional model The traditional model is an essential checklist of the content to be covered in a medical history (Box 2.1). Limitations of the traditional model The traditional model does not ensure that history taking is effective. Effective history taking is more than asking a checklist of questions, noting responses and formulating a diagnosis at the end. Incorporating the patient’s perspective – ideas, concerns and expectations Understanding what patients are thinking In PACES you have 15 minutes to take a history, witnessed by examiners examining your history-taking skills – the communication skills that make history taking effective. Fifteen minutes may seem a short time in which to take a medical history, although general practitioners regularly have less than 10 minutes, relying on focused questions incorporating the patient’s perspective. In PACES, as in practice, feeling pressured because you are short of time and trying to extract the ‘facts’ at all costs from the patient is ultimately less effective than demonstrating these skills. Patients often report things in what seems a chaotic order, dodging from one area of the history to another; candidates might prefer patients to quickly and simply answer questions rather than volunteer extra information. Yet this extra information often contains vital elements of the real problem. History taking is a way of guiding what patients say. The best way to understand how historytaking skills can guide patients is to understand what patients are thinking. Scenario A PACES scenario is shown in Box 2.2. Box 2.2 PACES scenario You have taken a history from a 52-year-old woman with a painful left calf and mild swelling in the region of the popliteal fossa. You discover that she has had worsening pain for 3 weeks, exacerbated when going up and down stairs, and that sometimes it is so painful it reduces her to tears. She has had to stop work. You discover that she is a nurse on a surgical ward, married, with two children. She has no significant past medical history but 2 months ago was on a long- haul flight, returning from a visit to her sister in Australia. You are told that examination confirms mild swelling in the popliteal fossa and calf tenderness but is otherwise unremarkable. The patient’s perspective – ideas, concerns and expectations (ICE) Having taken such a history, you should of course consider the possibility of deep venous thrombosis (DVT). DVT is the most serious of the differential diagnoses, although intuitively you may have some doubts; the duration of symptoms is long and the flight 2 months ago probably irrelevant. Hypothesis testing (pursuing possibilities in turn until they are either excluded or warrant further testing) may also bring a popliteal cyst and muscle strain into the differential diagnosis. You might also wonder whether as a nurse she might be particularly worried about a DVT. She will have seen DVTs on the surgical wards and know them to be dangerous. She might also be aware of the risks of air travel, but unaware that 2 months is a long time to ‘harbour’ a thrombosis. She is probably apprehensive. Being a patient in hospital or clinic – as a health-care professional to a greater or lesser extent – is being in an alien environment amidst other unwell and sometimes dying people. Many patients have strong preconceptions about doctors and hospitals learned from relatives, friends or the media; doctors seem not to tell patients much, and what they do tell can be difficult to understand; they make mistakes, sometimes with fatal outcomes. This patient might have already decided that she has a blood clot in her leg until proven otherwise. She might know that blood clots can travel to the lung and prove fatal. Much convincing to the contrary might be needed if, for example, her grandmother died from a blood clot (albeit after a fractured hip). She may have seen patients on warfarin, a dangerous drug sometimes taken for life. She might be scared that she has a serious condition requiring dangerous treatment. These sorts of thoughts going through her mind may be summarised as her ideas (beliefs), concerns and expectations about what her symptoms might represent. She might: • believe she has a blood clot • be concerned about why it has happened and what needs to be done about it • and expect the worst if nothing is done. A 30-year-old athlete with similar symptoms might believe them to represent a strained muscle, have very few concerns and expect them to go away. But do not just assume! Patients do not present just with symptoms, but with thoughts about their symptoms. Some patients volunteer their thoughts. When patients do not volunteer their thoughts, asking is much better than assuming: What have you been told before / so far about this? What thoughts have gone through your mind about this? Are you worried about anything in particular? Without asking such a question, you will not discover (as the candidate here failed to discover) that the patient was worried she might have multiple sclerosis. Her sister in Australia had presented 2 years earlier with a painful left leg, later diagnosed as multiple sclerosis. She in fact: • believed that she had multiple sclerosis and that it had happened because it ran in her family • was concerned about needing a lumbar puncture • and expected to become wheelchair bound as her sister had. Failing to establish a patient’s thoughts can mean that doctor and patient are looking at the same problem from a different angle, or even two different problems. Discovering a patient’s thoughts and any hidden agenda is important. For all sorts of reasons patients do not always report their concerns, and a simple question can confirm: Your asthma has obviously been troubling you a lot recently. How do you feel we could best help you? By trying to improve the sleepless nights, or something else? ICE in practice Overt doctor centredness (pure information gathering) and overt patient centredness (purely addressing the patient’s perspective) are extremes of a spectrum. History taking naturally undulates within the spectrum, generally starting with patient-centred open questions: Your GP says you have had a painful leg. Would you be able to tell me more about that? Well, yes, I noticed it a week or two ago, but didn’t do anything about it. Why not? I hoped it would go away. I hoped it wasn’t anything serious. And what has happened since then? Patient-centred history taking aims to identify a patient’s ICE. The following questions are examples of this patient-centred approach: I expect you’ve been thinking about this for a while. Are you worried about anything in particular? I was wondering what thoughts you’d had yourself about this? What were your own thoughts about this problem? Have you had any thoughts yourself about what may be causing this? What did you think might be causing it? Were you worried it might be due to something in particular? Some people might have thought it might be due to blood pressure. Did that worry you at all? When you hear the word …, what does that mean to you? Tell me what you have heard about … What types of … have you heard of? You mentioned a family history of stroke. Is that what really worries you at the moment? Which part of this bothers you most – is it what the surgeon said or what your wife might think or something else? What exactly is it about the operation that worries you most? Patient centredness taken too far can render history taking just as ineffective as pure doctor centredness. History taking should certainly involve guiding a patient back on track if the account starts to wander into areas you feel will not yield useful information; it is perfectly acceptable to say something like: That is obviously important to you and perhaps we could return to it later, but didn’t you say that the main problem you were having was … How it all affects the patient Exploring the patient’s perspective fully should explore not just ICE, but how the illness or problem(s) affects that patient. This overlaps significantly with the social history. The principle is that it is as important to understand the person who has the disease as it is to understand the disease itself, and it can be helpful to encourage the patient to express their feelings. Opening questions could be: How is this affecting you at work? How are you coping at home with this? History-taking skills – the communication skills that make history taking effective Communication skills training is now a core component of medical education, and there is good evidence that these skills can be acquired. Important communication skills include: • Listening skills • Use of appropriate questions • ‘Eliciting’ or facilitating skills • Recognising and responding to cues • Use of appropriate language • Summarising. Listening skills As with examining patients and starting with inspection, good history-taking candidates are alert to how patients look, talk and behave. The patient may be relaxed or anxious, waiting for questions, may have already started talking or may pre-empt your opening question: I don’t know where to start. I don’t like hospitals. I don’t know what I’m going to do about my breathing. The important thing is not to rush in with questions, suppressing information that may provide a valuable insight into what the patient is thinking. Useful opening questions might be: What seems to be the problem? Your GP says you have had a painful leg. Could you tell me about that? Could you tell me why you have come into hospital? The response might be: It’s my heart, doctor. I just don’t seem to have any energy any more. Again, it is very important to continue listening. Many candidates respond immediately with questions, for example by asking about cardiac symptoms or by assuming the problem to be tiredness and asking about thyroid symptoms. Remember that asking a direct question usually only gives you the answer to that question! Careful listening for a minute or two, encouraging the patient to elaborate, will help you form a much more accurate assessment of what the problem is likely to be about: I just don’t seem to have any energy any more … It all started last October when I began to get short of breath … I’d never been in hospital in my life before that … now I seem to be here every few weeks. I first noticed it when I was out walking my dog. He’s always full of energy but I was beginning to find that I couldn’t keep up with him any more. I went to see my own doctor because you hear about people suddenly dropping down with heart attacks at my age, don’t you? I’d had a few pains in my chest as well. He said that the heart tracing was okay but thought I should have an X-ray – that was when he sent me into hospital. Your thoughts may now be quite different. Heart failure? Angina? Pulmonary emboli? Chronic obstructive pulmonary disease? Pulmonary fibrosis? The point is that listening, giving a little time for the patient to tell you what has been happening in their words, will give you a clearer idea of the direction you need to take. Active listening Active rather than passive listening is showing that you are interested in what the patient is saying. Active listening skills include: • An attentive manner (it helps to sit forward – not slouching! – and make eye contact) • Not interrupting (at least, not immediately) • Encouraging noises, posture and gestures, or the skilful use of silence • Reflecting back answers to create follow-up questions – What do you mean by dizzy? Use of appropriate questions Open questions These are particularly important if you are to avoid jumping to conclusions. They are essential early in the medical interview: Can you describe the pain in more detail? Can you tell me a little more about that incident? And what has been happening since then? So you’re worried about what this pain says about your health? Have you noticed if the pain is brought on by anything in particular? May I ask some general questions about your health? What has been the result of all of this? Closed questions These help to clarify what a patient has said or to obtain factual information that has not been volunteered: Have you coughed up any blood? In general, save closed questions until the patient has had the chance to tell their story. A relevant systems enquiry is, of course, an appropriate series of closed questions. Eliciting or facilitating skills Disclosure of relevant medical information and information important to a patient needs to be facilitated. Some patients need little encouragement to talk, and their account should be guided towards what you see as clinically relevant. Some patients are reserved, and need encouragement. Probably the two most important eliciting skills are active listening and the use of appropriate questions. As well as asking open and closed questions, remember that some questions may seem irrelevant to patients and it is important to explain why you are asking them. This may be especially important for sensitive issues: Some of my patients with emphysema get quite depressed. I often ask patients with emphysema if they have been feeling depressed. Encouragement There are many ways of encouraging a patient to continue their account. The simplest yet very effective methods are silence with encouraging facial gestures (smiling and showing concern), nodding, saying Mmm or Yes and echoing what is said: I have this headache sometimes. Headache? Not all the time, but I get it a lot. Which part of your head gets sore? This bit. It comes and goes. I wondered if it was serious. What do you mean by serious? Well you hear about headaches. What have you heard? Interpretation Reframing or recounting information for patients can help encapsulate information into meaningful ‘packages’ and show that you understand: I don’t know how best to say it. I’m not depressed exactly. No, I understand. But I would think you are lonely since your wife died. Clarification Sometimes it is necessary to clarify statements that are unclear or need amplification: Could you explain what you mean by … ? ‘Questions in disguise’ Questions that are not actually questions can be very useful for eliciting information. A statement may be used as question: It sounds as though that incident alarmed you. Conjecture may be used as a question: I was wondering whether … Sometimes people with headaches worry that it might be something serious … Sometimes when women have pain like this they worry they might be pregnant … Sharing an experience or examples can be used as a question: I had a patient recently who went through a similar … Legitimising Legitimising feelings can help a patient to talk openly: This is clearly worrying you a great deal. You have a lot to cope with; I think most people would feel the same way. Recognising and responding to cues A cue is hard to define, and more easily recognisable. It could be defined as a signpost to an area in the history you might otherwise ignore but which may be very important to the patient. Cues are very common. They are often not consciously presented by patients, but offer an insight into undeclared concerns. Verbal cues Examples of verbal cues are: I hoped it wasn’t anything serious. I don’t get paid when I don’t work. It’s my chest again. I just seem to be losing it. Of course it could just be stress. Of course it could be my heart. I’m not worried … after all a lot of those TV programmes just show the worst cases. It doesn’t help that my sisters aren’t here. I hope this won’t mean lots of tests. I’ve got a lot on my plate at the moment. There may also be cues in the pace, pitch, volume, rhythm or modulation of speech and there may be cues in censored speech – in what is not said. Patients frequently hesitate or appear to omit information you intuitively feel should be included: It’s no better (what’s no better?) Something will have to be done (what will have to be done?) I’m worried (about what?) I feel worse (worse than what or when?) I’m suffering (from what?) I feel a failure (why?) Sometimes, patients use generalisations to express their concerns: I don’t like hospitals. No one understands. I always get headaches. It never seems to get any better. Non-verbal cues Cues may be non-verbal, expressed through body language, facial expression or affect. A patient may look sad or anxious and it might be appropriate to respond: You look worried about that. Further, not all cues need an immediate response. Sometimes storing a piece of information and returning to it later is effective: You mentioned earlier that you hadn’t wanted to come into hospital. Was there anything worrying you in particular about hospital? You will not detect all cues and you do not need to act on all cues that you detect. But examiners will notice if you ignore what seems to be an important cue. Use of appropriate language Most importantly, use clear and concise language that you think the patient will understand, and avoid technical terms or jargon that might not be understood, or at least explain any necessary jargon. It can sometimes help to ‘match’ a patient’s verbal and non-verbal behaviour. Patients often speak in visual or auditory terms or in concepts and might say: I don’t see a way out. It sounds like bad news to me. It’s all a bit much. Sometimes harnessing the patient’s language in this way can enhance rapport and you may find yourself doing it naturally: I see what you mean but whilst it may look that way … It sounds bad and not what you wanted to hear but … I can imagine what you must be going through. Sometimes, in subtle ways, it is possible to match body language as well as speech. Matching is a two-way process. Speaking loudly and clearly will often encourage a patient to do the same. Summarising Summarising periodically Summarising periodically, as well as at the end of the interview, can be useful in verifying your understanding and in inviting the patient to correct any misinterpretation or add information. Summarising at the end Always give your patient a chance to add information or ask questions before concluding. You might ask: Is there anything you would like to ask? Is there anything else you feel I should know? Is there anything important to you that you feel I have left out? It is good practice to confirm shared understanding: May I take a moment to summarise what you’ve told me so I can check that I’ve understood everything that is important to you. Finish by thanking the patient. The traditional model and communication skills – putting these together Content versus process The traditional history model describes the content of the interview – what to cover. Communication models describe the process of the interview – how to do it. Doctors often revert to closed questions and a tightly structured history directed towards gathering medical information. This is understandable because most doctors learned this model, and doctors are seldom observed taking histories but often observed presenting their findings, engendering the erroneous belief that the format for presenting information is the same as that of gathering information. Further, doctors document their findings using the traditional model, augmenting this belief. Because communication skills have previously been taught on courses separate to content skills taught at the bedside, the belief that ‘real’ doctors take ‘histories’ and communication skills disregard the clinical history is all too common. Yet the traditional model fails to elicit much of the information needed to understand and manage a patient’s problems. Indeed, studies of patient satisfaction, concordance, recall and physiological outcomes validate the need to combine the traditional model with communication skills models. Many communication models exist, such as the Calgary–Cambridge guides. Communication models provide alternative frameworks and lists of skills that are the means by which doctors get through the medical interview, develop rapport, gather information and then discuss their findings and management options with patients. Content plus process Because content and process are different frameworks it is easy to see them as alternatives and use only one. Indeed, if not learned and practised together, the tendency is to allow one (usually the traditional model) to inhibit the other. This can lead to many of the common faults in history taking (Box 2.3). Box 2.3 Common faults in history taking • Poor introduction • Inappropriate questions • Avoiding personal issues • Lack of warmth or empathy • Repetition • Poor clarification • Poor control • Poor facilitation of patient disclosure • Premature or restricted focus Comprehensive clinical methods that explicitly integrate the traditional model with effective communication skills have been proposed. Table 2.1 is a summary of content working with process that is suitable for Station 2 of PACES. Table 2.1 Putting it together – the traditional history model (content) and communication skills (process) ICE, ideas, concerns and expectations. Cases Respiratory problems Case 2.1 Breathlessness and other respiratory symptoms Candidate information Role You are a doctor in the medical outpatient clinic. Please read the following letter from the patient’s general practitioner (GP). You may make notes on the paper provided. When the bell sounds, enter the examination room to begin the consultation. Scenario Dear Doctor Re: Mr John Thorn, aged 56 years Thank you for seeing this man who has become progressively breathless over six months. Three months ago he developed a lower respiratory tract infection that responded to amoxicillin and doxycycline but he continues to be breathless, particularly on exertion. He smokes and I wonder if he is developing chronic obstructive pulmonary disease. His peak flow is slightly lower than predicted at 420 l / min, although salbutamol and ipratropium inhalers appear to have made little difference. A course of prednisolone did not improve his breathing. Your assessment is appreciated. Yours sincerely Please take a history from the patient (you may continue to make notes if you wish on the paper provided). Your examiners will warn you when 12 minutes have elapsed. You have 14 minutes to take a history from the patient followed by 1 minute of reflection. There will then follow 5 minutes of discussion with the examiners. Be prepared to discuss solutions to the problems posed by the case and how you might reply to the GP’s letter. You are not required to examine the patient. Patient information Mr John Thorn is a 56-year-old man who has been troubled by progressive breathlessness on exertion for the past 6 months, with a dry cough. He saw his GP 3 months ago when he developed purulent sputum and although this settled over about 2 weeks with two different courses of antibiotics, his breathlessness and dry cough persisted. He is not breathless at rest, or lying down. He thinks he may have lost a little weight, but has no other notable symptoms. He has smoked 20 cigarettes a day since he was a young man and attributes his symptoms to this. He has no other past medical history of note. He has worked for 30 years as a roadbuilder. He has never worked in shipyards or building construction and to his knowledge has not been exposed to asbestos. He is not prone to allergies. He has owned the same parrot for the last 8 years and has no other pets. Inhalers have not helped his breathlessness. A course of steroids helped his breathing only marginally. He is worried that if his breathing deteriorates he will no longer be able to visit his brother, who lives in America. How to approach the case Data gathering in the interview and interpretation and use of information gathered Presenting problem(s) and symptom exploration Elicit details of breathlessness. Find out: • If it is chronic, and, if so, if it is progressive • If it came on suddenly or insidiously • If it is continuous, discrete or with stepwise episodes of worsening (pulmonary emboli; infective exacerbations of chronic obstructive pulmonary disease (COPD)) • If it is present only on exertion, or also at rest, and if there is orthopnoea (left ventricular failure). Ask about trigger factors. Ask about exercise, cold, smoking and allergens. Explore associated symptoms. Ask about: • Cough, with sputum (characteristics and volumes – large volumes suggest bronchiectasis) or dry (interstitial lung disease) • Haemoptysis (lung cancer, pneumonia, pulmonary tuberculosis, bronchiectasis, pulmonary embolus, vasculitis, pulmonary haemorrhage) • Wheeze (asthma, COPD) • Symptoms suggesting a cardiac cause (exertional chest pain, orthopnoea, paroxysmal nocturnal dyspnoea, ankle swelling – which may also be due to cor pulmonale) • Alarm symptoms for malignancy such as weight loss, anorexia, haemoptysis or hoarseness. Patient perspective Explore his concerns about the limitations caused by breathlessness, and reassure him that you will do all you can to improve his breathing to enable him to fly. Past medical history Ask breathless patients about previous respiratory diseases, such as tuberculosis or asthma, cardiovascular disease or risk factors, and atopy (personal or family history of asthma, eczema or allergic rhinitis). Drug and allergy history Many drugs may contribute to dyspnoea, cough or wheeze; specifically ask about nonsteroidal anti-inflammatory drugs and angiotensin-converting enzyme inhibitors. Family history Ask about atopy or respiratory disease. Social history Ask about: • Smoking (including passive smoking and pipe smoking – when started / stopped, quantity and pack years) • Occupations past and present (specifically about the shipyard and building industries for asbestos exposure and road-building for silicosis) • Travel (atypical pneumonia) • Pets (cats and dogs commonly trigger asthma, and birds can trigger atypical pneumonia and extrinsic allergic alveolitis).