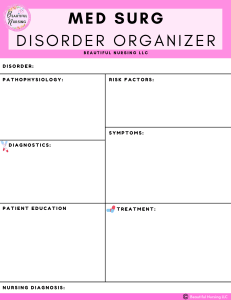
48 Hour Cram Sheets for Med Surg
advertisement

48 Hour Cram Sheets for Med Surg BRAIN TUMOR 48 Hour Cram Sheets for Med Surg Simplenursing.com Less Study Time HIGHER test scores! Page 1 of 106 48 Hour Cram Sheets for Med Surg BRAIN TUMOR Table of Contents 1. CANCER (ONCOLOGY) ...................................................................................................................... 7 BRAIN TUMOR...................................................................................................................................... 7 COLON CANCER.................................................................................................................................... 8 LEUKEMIA............................................................................................................................................. 9 OVARIAN CANCER .............................................................................................................................. 11 PROSTATE CANCER ............................................................................................................................ 12 PANCREATIC CANCER ......................................................................................................................... 13 2. NEURO: CNS ................................................................................................................................... 15 ALZHEIMERS ....................................................................................................................................... 15 BRAIN TUMORS .................................................................................................................................. 17 CEREBERAL VASCULAR ACCIDENT (CVA) ........................................................................................... 18 EPILEPSY ............................................................................................................................................. 20 HEAD INJURY ...................................................................................................................................... 23 MULTIPLE SCLEROSIS (MS)................................................................................................................. 24 MENINGITIS........................................................................................................................................ 25 PARKINSON’S ..................................................................................................................................... 26 SEIZURE .............................................................................................................................................. 27 SPINAL INJURY.................................................................................................................................... 30 3. NEURO: PNS ................................................................................................................................... 32 GUILLAIN-BAR SYNDROME ................................................................................................................ 32 MYASTHENIA GRAVIS ......................................................................................................................... 33 4. GASTRO INTESTINAL (Lower) ......................................................................................................... 36 APPENDICITIS ..................................................................................................................................... 36 SBO (SMALL BOWEL OBSTRUCTION) ................................................................................................. 37 CONSTIPATION ................................................................................................................................... 38 HERNIA ............................................................................................................................................... 39 PARALYTIC ILEUS ................................................................................................................................ 40 ISCHEMIC BOWEL/COLITIS ................................................................................................................. 41 VOLVULUS .......................................................................................................................................... 42 DIVERTICUITIS .................................................................................................................................... 43 RESECTION OF INTESTINES ................................................................................................................ 44 Page 2 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg BRAIN TUMOR INFLAMMATORY BOWEL DISEASE ..................................................................................................... 46 COLORECTAL CANCER ........................................................................................................................ 46 5. ORTHOPEDICS (BONES) .................................................................................................................. 48 HIP FRACTURE .................................................................................................................................... 48 TOTAL KNEE REPLACEMENT (TKR) ..................................................................................................... 49 LONG BONE INJURY ........................................................................................................................... 50 OSTEOARTHRITIS (OA) ....................................................................................................................... 51 RHUMATOID ARTHRITIS (RA) ............................................................................................................. 52 GOUT .................................................................................................................................................. 53 6. VASCULAR DISORDERS ................................................................................................................... 55 PAD (PERIPHERAL ARTERY DISEASE) .................................................................................................. 55 PVD (PERIPHERAL VASCULAR DISEASE) ............................................................................................. 56 ANEURYSMS ....................................................................................................................................... 58 7. RESPIRATORY ................................................................................................................................. 60 ASTHMA ............................................................................................................................................. 60 BRONCHITIS ....................................................................................................................................... 61 COPD (CHRONIC OBSTRUCTIVE PULMONARY DISEASE) ................................................................... 62 EMPHYSEMA ...................................................................................................................................... 63 HEMOTHORAX ................................................................................................................................... 64 PNEUMOTHORAX............................................................................................................................... 65 PNEUMONIA ...................................................................................................................................... 66 PULMONARY EMBOLISM ................................................................................................................... 67 RESPIRATORY FAILURE ....................................................................................................................... 68 TUBERCULOSIS ................................................................................................................................... 69 URI (UPPER RESPIRATORY INFECTION) ............................................................................................. 70 8. CARDIAC (HEART) ........................................................................................................................... 71 ANGINA .............................................................................................................................................. 71 ARRHYTHMIAS ................................................................................................................................... 72 ACUTE CORONARY SYND. (ACS) ......................................................................................................... 73 ATRIAL FIBRILLATION (A-FIB) ............................................................................................................. 74 CARDIOGENIC SHOCK......................................................................................................................... 75 CABG (Coronary Artery Bypass Graft) ................................................................................................ 76 Simplenursing.com Less Study Time HIGHER test scores! Page 3 of 106 48 Hour Cram Sheets for Med Surg BRAIN TUMOR CHF (Congestive Heart Failure) .......................................................................................................... 77 CAD (Coronary Artery Disease) .......................................................................................................... 78 HTN (Hypertension) ........................................................................................................................... 79 HYPERLIPIDEMIA (High Cholesterol) .................................................................................................. 80 9. ENDOCRINE .................................................................................................................................... 81 DIABETES TYPE I ................................................................................................................................. 81 DIABETES TYPE II ................................................................................................................................ 82 HYPOGLYCEMIA ................................................................................................................................. 83 HYPERGLYCEMIA ................................................................................................................................ 84 DIABETIC KETOACIDOSIS (DKA).......................................................................................................... 86 10. GALLBLADDER & LIVER & APPENDIX.......................................................................................... 87 APPENDICITIS ..................................................................................................................................... 87 CHOLECYSTITIS ................................................................................................................................... 88 HEPATITIS ........................................................................................................................................... 89 PANCREATITIS .................................................................................................................................... 90 CIRRHOSIS .......................................................................................................................................... 91 11. KIDNEY (RENAL).......................................................................................................................... 93 ACUTE RENAL FAILURE (ARF) ............................................................................................................. 93 CHRONIC RENAL FAILURE (CRF) ......................................................................................................... 95 CHRONIC RENAL INSUFFICIENCY........................................................................................................ 96 NEPHROTIC SYNDROME..................................................................................................................... 97 KIDNEY STONES .................................................................................................................................. 98 GLOMERULONEPHRITIS ..................................................................................................................... 99 TURP (Trans urethral resection of prostate) .................................................................................... 101 URINARY TRACT INFECTION (UTI) .................................................................................................... 102 BPH (Benign Prostate Hypertrophy) ................................................................................................ 103 12. WOMEN’s HEALTH ................................................................................................................... 104 UTERINE FIBROIDS ........................................................................................................................... 104 OVARIAN CANCER ............................................................................................................................ 105 13. Bibliography ............................................................................................................................. 106 Page 4 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg BRAIN TUMOR With over 8 years in the medical field, Mike Linares has worked both out in the field on an Ambulance in the dangerous streets of Los Angeles County and the in crazy busy the Emergency Rooms. Coupled with his passion for teaching & desire to help other students and mixed with his chronic typpos and bad grammmer, SIMPLEnursing.com was born to not only help his fellow RN students, but nursing students worldwide. "I hope you enjoy the valuable jewels that Simplenursing.com has to offer. If so please let me know! I am a real person & I´d love to hear your thoughts good or bad on Face book, Twitter, or Youtube." Committed to Your Success, Mike P.S.Feel free to Face book, Twitter, or Youtube me!! Mike Linares Student Nurse Mentor & Certified EKG Instructor HOW THIS WHOLE THING CAME TO BE... Before Helping Multiple Successful Nursing Students Excel I Was The "Drone" Nursing Student Working Too Hard & Eventually I FAILED OUT of Nursing School. Before Helping Hundreds of Struggling Nursing Students Reach Graduation Day & Before Becoming a Student Nurse Mentor & Certified EKG Instructor, I Myself Was A Struggling "At Risk" Student Nurse Drowning In My Books & Lost In Clinical. I was that struggling student working full time in the Emergency Room at one of those MEGA hospitals in Orange, California. I worked as an EMT aka a "medic" for 8 years prior to failing out. I knew how to take care patients, I knew the basics of the ABCs of basic life support, I knew how to take vital signs and how to fix minor injuries. I thought I had enough experience to skate right through nursing school, I remember thinking "how hard can it be" right? After two semesters, I FAILED out of the Program. I felt defeated, depressed and like a loser. It was one of the lowest points of my life. Sitting in my room practically bawling my eyes out, I remember quotes my mom and dad used to encourage me with, "son, whatever doesn´t kill you, Makes you Stronger" & " Failing is Not a Bad Thing, As long as learn, become better, and NEVER EVER QUIT" Simplenursing.com Less Study Time HIGHER test scores! Page 5 of 106 48 Hour Cram Sheets for Med Surg BRAIN TUMOR My Clinial FAILURE form had bold red letters stating: LACK In Prepared LACK Organizational Skills LACK Critical Thinking with Nursing Process Ending with: "able to return next semester contingent upon demonstrating INCREASED COMPETANCIES in these core areas." "NEVER GIVE UP!!" my mom & dad used to tell me, so I set out on a Quest to develop a system to make Simplify Nursing School! What Happened Next Might Surprise you, In a systematic way to put all the "core competencies" of nursing school that instructors look for to pass students. My quest was to make it SIMPLE first and foremost, by cutting out the fluff and getting down to the nitty critty making it easier. The Goal Was To Make A Simple System... And the best part is it was really helping myself and other students in my class pass their tests when I would share with them my strategies and systems to help them pass their tests without having to memorize everything in the book! This is where my mentoring for student nurses began. That's when something clicked and everything changed for me. It was like I had an Ah - HA moment! At that moment I realized there are better, more predictable, and more low cost ways to get higher test scores and have more critical thinking skills than the money I had been spending on dead end study books that claimed to help but really just confuse me more. I needed simplicity!!! Within the next six months I had created over 27 different student help systems, strategies and tactics that produced better results for me - some better than others. Then over the next few semesters I tracked, tested, and tweaked each system until my students were passing with a 82% or better on each and every test, 2 students being out of School for over 25 years & coming back to score 94% on their EKG cardiac test! Truly amazing & truly making me proud to be their mentor. Page 6 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg BRAIN TUMOR 1. CANCER (ONCOLOGY) DIAGNOSIS/PATHO BRAIN TUMOR Patho: Defined as an intracranial solid neoplasm, or an abnormal growth of cells in brain or central spinal canal. No known cause or risk factor. Graded as: low, intermediate or high Can be located in several areas of the brain: -Healthy cells transform/mutate into malignant cells upon exposure to certain etiologic factors such as: Viruses, Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the lymph nodes and lymphatic system, the DATA ACTION Assess: Neurological status, ALOC, worsening symptoms/impairment, ↑ICP Vitals: Normal, until near death S/S & PHYS. EXAM: - Headache -Nausea/Vomiting -ALOC/Changes in speech, vision or hearing -Issues with gait, balance or walking -Changes in mood, personality, ALOC -Memory problems/inability to concentrate - Seizures/Convulsions -Muscle twitching/jerking -Numbness/Tingling in extremities Nursing Interventions: Pharm: **DEPENDS ON SIZE & TYPE OF TUMOR, AS WELL AS OVERALL HEALTH STATUS: - Chemotherapy Targeted therapy: -Avastin/bevacizumab (for Labs: Spinal tap, biopsy Dx Tests: Neurological exam, MRI, CT Scan, Angiogram Simplenursing.com Less Study Time HIGHER test scores! glioblastoma) - Afinitor/everolimus (used to treat a benign brain tumor) Alternative Medicine: -Acupuncture -Hypnosis -Music Therapy -Relaxation Techniques Pt. Ed: Referral to OT, PT, ST (Speech therapy) and tutoring (if child, and learning/memory problems Surgery: Removal of tumor (If able to) Page 7 of 106 RESPONSE Nursing Dx: -Disturbed Body Image r/t changes in the structure and function of the brain/body -Fear r/t recent diagnosis and unknown future Pt. Goals/ Evaluation: -Pt will verbalize concerns and fears about body, self perception and change of lifestyle -Pt will verbalize anxiety as well as ways to reduce it/minimize with it. 48 Hour Cram Sheets for Med Surg COLON CANCER blood, and system wide to other organs/cavities. (Most common types of brain tumors/locations) COLON CANCER Patho: Colon cancer occurs in the lower part of the digestive system. Cancer in the colon can begin as small benign clumps in the colon, known as adenomatous polyps. In time, these polyps can develop into colon cancer. Assess: Last Colonoscopy? RISK FACTORS: -Older Adult men/women -Race (African-American) -Genetic/Family history/Personal Hx -Diet high in red meat and fat and low in fiber -Inflammatory bowel diseases The American Cancer Society 7 WARNING SIGNS for Cancer: C – Change in bowel/bladder habits A – A sore that that doesn’t heal U – Unusual Bleeding/Discharge T – Thickening/lumps in breast/body I – Indigestion/Difficulty swallowing O – Obvious change in wart/mole N - Nagging, coughing or hoarseness -Healthy cells transform/mutate into malignant cells upon exposure to certain Page 8 of 106 Nursing Interventions: Pharm: Chemotherapy, Radiation therapy, and Targeted drug therapy (bevacizumab/Avastin, cetuximab/ Erbitux, panitumumab/Vectibix and regorafenib/Stivarga) Pt. Ed: Maintenance of Colostomy bag/care if needed, returning for testing, side effects of meds/ colostomy bag, support system Surgery: Removal of polyps (If possible), Partial Colostomy, Full colostomy/surgical removal Vitals: Normal unless distressed S/S & PHYS. EXAM: Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Anticipated loss of physiological well-being r/t loss of body part, change in body function, change in lifestyle and perceived potential death of patient -Situational low self-esteem r/t disfiguring surgery, chemotherapy or radiotherapy side effects, e.g., loss of hair, nausea/vomiting, weight loss, anorexia, impotence, sterility, overwhelming fatigue, uncontrolled pain Pt. Goals/ Evaluation: -Pt will continue daily activities, identify feelings and fears towards lifestyle change and diagnosis, Pt will understand and verbalize the grieving and death process - Pt will verbalize acceptance of diagnosis, control over health 48 Hour Cram Sheets for Med Surg LEUKEMIA etiologic factors such as: Viruses, Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the lymph nodes and lymphatic system, the blood, and system wide to other organs/cavities. All cancers are staged between I-IV, with Stage I being the least severe and Stage IV being the most severe. - Change in your bowel habits (diarrhea, constipation, consistency) - Blood in your stool - Persistent abdominal discomfort, such as cramps, gas or pain - Feeling your bowel doesn't empty completely - Weakness/fatigue - Unexplained weight loss Labs: Stool sample to check for blood or dead cancerous cells Dx Tests: Colonoscopy, CT Scan Assess: LEUKEMIA RISK FACTORS: Patho: MALIGNANCIES OF THE BLOOD-Genetic/Family history: FORMING CELLS: - Philadelphia chromosome: DNA exchange between chromosomes 9 & 22, creating an oncogene - Li-Fraumeni syndrome: an inherited mutation in a tumorsuppressor gene (TP53) -Exposure to: Radiation, Benzene, Cigarette smoke -Down syndrome -Healthy cells transform/mutate into malignant cells upon exposure to certain etiologic factors such as: Viruses, The American Cancer Society 7 WARNING SIGNS for Cancer: C – Change in bowel/bladder habits A – A sore that that doesn’t heal U – Unusual Bleeding/Discharge Simplenursing.com Less Study Time HIGHER test scores! status and demonstrate utilization of support systems and therapy as prescribed Nursing Interventions: (**Depends on type of Leukemia, severity and Age of Patient) Pharm: Chemotherapy, Radiation, Biological therapy, Targeted Therapy (Imatinib/Gleevec & dasatinib/ Sprycel), Stem Cell Transplant Pt. Ed: DON’T WAIT TO GET TREATMENT! TIMING IS IMPORTANT! Know the side effects of medication as well as supportive measures: - Vaccines - Blood/Platelet Transfusions Page 9 of 106 Nursing Dx: - Pain r/t enlarged organs/ lymph nodes and treatment for diagnosis -Risk for infection r/t compromised immune system Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it - Pt will identify signs and symptoms of infection and verbalize ways to minimize chances of infection 48 Hour Cram Sheets for Med Surg LEUKEMIA Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the lymph nodes and lymphatic system, the blood, and system wide to other organs/cavities. All cancers are staged between I-IV, with Stage I being the least severe and Stage IV being the most severe. T – Thickening/lumps in breast/body I – Indigestion/Difficulty swallowing O – Obvious change in wart/mole N - Nagging, coughing or hoarseness - Antibiotics - Analgesics for Pain - Immunoglobulins - Red & White cell growth factors Surgery: Removal of spleen (if inflamed) Vitals: Normal unless distressed S/S & PHYS. EXAM: - Fever/Night sweats - Swollen lymph nodes (usually painless) - Feelings of fatigue, tiredness - Easily bleeding or bruising, causing bluish or purplish patches on the skin/nosebleeds - Frequent infections - Bone/joint pain - Unexplained weight loss/Anorexia -Enlargement of the spleen or liver, which can lead to abdominal pain or swelling - Red spots on the skin (petechiae) (** If leukemia cells have infiltrated the brain: headaches, Page 10 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg OVARIAN CANCER seizures, confusion, loss of muscle control, and vomiting may occur) Labs: Abnormal blood test, bone marrow tests, genetic testing Dx Tests: Chest X-Ray, Lumbar puncture, MRI, CT Scan OVARIAN CANCER Patho: Cancer of the ovaries: -Healthy cells transform/mutate into malignant cells upon exposure to certain etiologic factors such as: Viruses, Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the lymph nodes and lymphatic system, the blood, and system wide to other organs/cavities. All cancers are staged between I-IV, with Stage I being the least severe and Stage IV being the most severe. Assess: Assess for menstrual cycle/ovulation history of patient and family… Most At Risk: -Staring period at young age -Ending period (Menopause) at older age -Never been pregnant (nulliparity) -Frequent cycles **10% are genetic and can be tested for BRCA1 and BRCA2 gene changes (mutations) The American Cancer Society 7 WARNING SIGNS for Cancer: C – Change in bowel/bladder habits A – A sore that that doesn’t heal U – Unusual Bleeding/Discharge T – Thickening/lumps in breast/body I – Indigestion/Difficulty swallowing O – Obvious change in wart/mole Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Chemotherapy (carboplatin and paclitaxel) Pt. Ed: Educate patient on side effects of chemotherapy, changes in hormone levels due to diagnosis and possible hormonal side effects, as well as ways to prevent infection as patient will be immunocompromised. Surgery: “Surgical Debulking”, where the abdomen is cleared of all masses, with NONE over the size of 1 cm. Removal of Ovaries/Fallopian tubes (Salpingo-oophorectomy), removal of uterus (hysterectomy) or omentum (omenectomy) and Lymph node dissection may be needed based on Page 11 of 106 Nursing Dx: - Pain r/t enlarged organs/ lymph nodes and treatment for diagnosis -Risk for infection r/t compromised immune system Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage - Pt will identify signs and symptoms of infection and verbalize ways to minimize chances of infection 48 Hour Cram Sheets for Med Surg PROSTATE CANCER N - Nagging, coughing or hoarseness the severity of the tumor(s). Vitals: Normal unless distressed S/S & PHYS. EXAM: -Fatigue -Abdominal/pain swelling -Swelling of legs -Shortness of Breath -Changes in bladder/bowel habits Labs: Genetic testing, Biopsy (if needed), CA-125 Cancer Screening blood Test (MAY be elevated but not guaranteed) Dx Tests: Ultrasound, CT Scan PROSTATE CANCER Patho: Cancer of the prostate gland: -Healthy cells transform/mutate into malignant cells upon exposure to certain etiologic factors such as: Viruses, Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the lymph nodes and lymphatic system, the Page 12 of 106 Assess: Assess for Risk Factors: Pt/Family hx of BPH and prostate cancer, MEN OVER 40, African American, Obese The American Cancer Society 7 WARNING SIGNS for Cancer: C – Change in bowel/bladder habits A – A sore that that doesn’t heal U – Unusual Bleeding/Discharge T – Thickening/lumps in breast/body I – Indigestion/Difficulty swallowing O – Obvious change in wart/mole N - Nagging, coughing or hoarseness Vitals: Normal unless distressed Nursing Interventions: Pharm: Chemotherapy, Biological therapy, Hormone therapy: Luteinizing Hormone – Release Hormone/LH-RH (To Stop the release of testosterone, such as LUPRON, TRELSTAR, ZOLIDEX) Pt. Ed: Encourage medication compliance, as well as the importance of check-ups/colonoscopy as recommended by doctor. Inform patient of side effects of prostate cancer, Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Altered urinary elimination r/t enlarged prostate and bladder distension -Risk for infection r/t surgical procedure/immunocompromise Pt. Goals/ Evaluation: -Patient will maintain effective voiding measures within limits of his/her condition - Pt will identify signs and symptoms of infection and verbalize ways to minimize chances of infection 48 Hour Cram Sheets for Med Surg PANCREATIC CANCER blood, and system wide to other organs/cavities. All cancers are staged between I-IV, with Stage I being the least severe and Stage IV being the most severe. PANCREATIC CANCER Patho: Cancer of the Pancreas, NO KNOWN CAUSE! -Healthy cells transform/mutate into malignant cells upon exposure to certain etiologic factors such as: Viruses, Chemicals, and Physical agents. When cells are malignant, they can metastasize into tissues surrounding the area, to the S/S & PHYS. EXAM: - Urinary problems - Decreased force in the urine stream - Blood in semen - Erectile dysfunction - Pelvic Discomfort - Pain in Bone including ERECTILE DYSFUNCTION, and encourage them to utilize support system/ affection/coping skills. Refer to support group. Also ambulation and catheter care after surgery. Labs: PSA (Prostate Specific Antigen) Level, Biopsy Dx Tests: Ultrasound, DRE (digital rectal exam) Surgery: Freezing Prostate tissue, Removal of Prostate, remove the testicles (orchiectomy) Assess: Assess for Risk Factors: - Chronic pancreatitis - Personal or family history of pancreatic cancer - Smoking/Excessive drinking - Obese - Diabetes - African-American - Family history of genetics that can increase cancer risk Nursing Interventions: **THIS CANCER IS USUALLY DIAGNOSED AT VERY LATE STAGES DUE TO IT’S ASYMPTOMATIC NATURE Pharm: Analgesics for pain, Chemotherapy, Targeted therapy, Radiation therapy The American Cancer Society 7 WARNING SIGNS for Cancer: C – Change in bowel/bladder habits A – A sore that that doesn’t heal U – Unusual Bleeding/Discharge T – Thickening/lumps in breast/body Simplenursing.com Less Study Time HIGHER test scores! Pt. Ed: THE HEALING PROCESS AFTER THE WHIPPLE PROCEDURE IS VERY LONG! Surgery: WHIPPLE PROCEDURE (removal of head of pancreas, and portion of small intestine Page 13 of 106 Nursing Dx: -Fear r/t recent diagnosis and unknown future -Risk for infection r/t surgical procedure/immunocompromise Pt. Goals/ Evaluation: -Pt will verbalize anxiety as well as ways to reduce it/minimize with it. - Pt will identify signs and symptoms of infection and verbalize ways to minimize chances of infection 48 Hour Cram Sheets for Med Surg PANCREATIC CANCER lymph nodes and lymphatic system, the blood, and system wide to other organs/cavities. All cancers are staged between I-IV, with Stage I being the least severe and Stage IV being the most severe. I – Indigestion/Difficulty swallowing O – Obvious change in wart/mole N - Nagging, coughing or hoarseness Vitals: Normal unless distressed S/S & PHYS. EXAM: (**Can be asymptomatic) - Yellowing of your skin and the whites of your eyes (jaundice) - Upper abdominal pain (can radiate to back) - Weight Loss/ Anorexia - Depression - Blood clots (duodenum), gallbladder and part of your bile duct. Part of stomach may be removed in addition. The remaining parts of your pancreas are reconnected to the Patient’s stomach and intestines to allow the digestion of food. -Also, removal of cancer on tail of Pancreas if possible Labs: Biopsy, Blood tests: CMP, CA 19-9 (Tumor Marker), CEA (Carcinogen Embryonic Antigen), Serum Amylase, Fecal Fat, Lipase, Stool Trypsin Dx Tests: Ultrasound, MRI, CT Scan, Endoscopic Ultrasound (EUS), Endoscopic retrograde cholangiopancreatography (ERCP) Page 14 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg ALZHEIMERS 2. NEURO: CNS DIAGNOSIS/PATHO ALZHEIMERS Patho: The most common cause of Dementia in older adults. This disease is progressive and is marked by impaired memory and thinking skills. The classic neuropathology findings in AD include amyloid plaques, neurofibrillary tangles, and synaptic and neuronal cell death. DATA ACTION Assess: Use GLASCOW/COMA SCALE (see below), LOC, Advancement of disease, ADL issues (speak to caretaker if any) Degree of Memory loss, Motor function, reflexes, speech, cognition, affect Nursing Interventions: Pharm: Cholinesterase Inhibitors: -Donepezil -Galantamine NMDA Antagonist: -Memantine Selective Serotonin Reuptake Inhibitors (SSRI’s): -Citalopram -Paroxetine Anti-Anxiety Meds: -Lorazepam - Oxazepam Vitals: ↑BP & ↑Pulse (May indicate ↑ Cranial pressure) S/S & PHYS. EXAM: STAGES: 1. Mild – Slow and gradual progression of decline of intellectual activity; loss of energy/drive, difficulty learning 2. Moderate – Evident deterioration. Client can’t remember address/phone number. Memory gaps, decreased hygiene, memory gaps, mood swings, paranoia, anger, jealousy and apathy. Fulltime care needed. Pt. Ed: **Education is better Simplenursing.com Less Study Time HIGHER test scores! absorbed by the Caretaker; as the patient may not be a reliable source to remember Have clocks, calendars and personal items in clear view. Speak in short phrases/words. Speak slowly. Assess vital signs/Neuro status. Identify threats to patient’s safety. Review all meds patient is taking, use family to obtain history. Page 15 of 106 RESPONSE Nursing Dx: -Altered urinary and bowel elimination r/t cognitive impairment and loss of muscle tone - Self-care deficit r/t cognitive impairment and physical limitations Pt. Goals/ Evaluation: -Pt will identify need to urinate/defecate and/or understand the need for assistance with these activities -Pt will identify need to urinate/defecate and/or understand the need for 48 Hour Cram Sheets for Med Surg ALZHEIMERS 3. Moderate to Severe- Repeated instructions needed. Inability to recognize common items and perform simple tasks. Patient wanders a lot. Client is a danger to himself. TOTAL CARE NEEDED. 4. Late- Client becomes unable to read or write. Bunted emotions, loses ability to talk and walk. STUPOR AND COMA… **DEATH SECONDARY TO INFECTION AND CHOKING Surgery: None available at this time Labs: Genetic testing for gene (APOE-e4) & Autosomal Dominant Alzheimers disease (ADAD) to indicate likelihood of having disease Dx Tests: Physical exam, Neuro exam, Mental status tests Page 16 of 106 Simplenursing.com Less Study Time HIGHER test scores! assistance with these activities 48 Hour Cram Sheets for Med Surg BRAIN TUMORS BRAIN TUMORS Patho: Brain tumors may be classified into several groups: those arising from the coverings of the brain (e.g., Dural meningioma), those developing in or on the cranial nerves (e.g., acoustic neuroma), Those originating with in brain tissue and metastatic lesions originating elsewhere in the body. Tumors of the pituitary and pineal glands and of cerebral blood vessels are also types of brain tumors. Relevant clinical considerations include the location and the histology character of the tumor. Tumors may be benign or malignant. A benign tumor CAN BE SERIOUS!! If occurs in a vital area and can grow large enough to have effects as serious as those of a malignant tumor. Assess: Neuro exam, Head to toe assessment, Assess coordination Vitals: Severe headache in the morning, increased when coughing, bending Convulsions Signs of increased intra-cranial pressure: blurred vision, nausea, vomiting, decreased Auditory function, changes in vital signs, aphasia. Changes in personality Impaired memory Natural disturbance of taste Classic triad: o Headache o Papilledema (intra-ocular pressure) o Vomiting S/S & PHYS. EXAM: Labs: Blood & Urine tests, Biopsy Dx Tests: MRI, Functional MRI (fMRI) CT Scan, Angiogram, Brain Scan, Diffusion Tensor Imaging (DTI), Positron Emission technology (PET Scan), Bone Scan Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: (Depends on size and location of the tumor) Radiation Therapy, Chemotherapy, Medications to reduce ICP (Mannitol), Anticonvulsants, Analgesics (**All prn, depending on situation) Pt. Ed: Caregiver information about assistance with ADL’s, keeping up with check-ups, options of care/symptom relief, support groups, communication with medical personnel and sources Surgery: Surgery if possible to remove tumor (Depends on size, location and degree of damage if removed) Page 17 of 106 Nursing Dx: -Acute pain r/t tumor and increased intercranial pressure -Anxiety r/t unknown future after surgery, cognitive impairment and health issues. Pt. Goals/ Evaluation: -Pt will verbalize pain level using numeric chart or “FACES” chart, as well as ways to reduce/treat pain -Pt will verbalize anxiety as well as ways to reduce it/minimize with it. 48 Hour Cram Sheets for Med Surg CEREBERAL VASCULAR ACCIDENT (CVA) CEREBERAL VASCULAR ACCIDENT (CVA) Patho: *Commonly referred to as Stroke or “Brain attack”. In a stroke, the sudden interruption of blood supply to areas of the brain results in cerebral necrosis and impaired cerebral metabolism, which permanently damages brain tissues and produces focal neurologic deficit of varying severity. A cerebral aneurysm is prone to rupture, which causes blood to leak into the subarachnoid space (and sometimes into brain tissue, where it forms a clot), resulting in increased intracranial pressure (ICP) and brain tissue damage -In a TIA, there is a temporary decrease in blood flow to a specific region of the brain, but there is no necrosis of brain tissue. The symptoms (lasting seconds to hours) produce transient neurologic deficits that completely clear within 12 to 24 hours. Assess: Assess for ALOC, change in speech/mental status, aphagia, dysphagia, visual disturbance, loss of balance, coordination, sudden SEVERE headache Vitals: ↑Pain S/S & PHYS. EXAM: Stroke -Hemiplegia and sensory deficit -Aphasia (impairment may be in speaking, listening, writing, or comprehending, Most cases are mixed expressive and receptive). -Hemipoeis – weakening of one side -Unilateral neglect of paralyzed side -Bladder impairment -Possibly respiratory impairment -Impaired mental activity and psychological deficits/ALOC -STROKE: F-A-S-T – Face, affect, smile, -Transient Ischemic Attack -Temporary loss of consciousness or dizziness -Paresthesias -Garbled speech -Cerebral aneurysm -Blurred vision and headache Signs and symptoms of ICP -Nuchal rigidity and pain on neck movement -Photophobia Labs: Urinalysis, Lumbar Puncture, brain biopsy Page 18 of 106 Nursing Interventions: Pharm: (Depends on type/ cause) -Aspirin -TPA (“Clot Buster”): Given within first 3-4.5 hours as indicated. ***TPA CONTRAINDICATIONS Intercranial hemorrhage, internal bleeding, recent trauma/surgery in last 3 mos., uncontrolled hypertension -Anticoagulants/Anti-platelets Pt. Ed: Watch for signs of bleeding/hemorrhage/Stroke, blood tests as requested, control Hypertension & diabetes, maintain diet low in saturated fat, and exercise as advised. QUIT SMOKING! Drink moderately/stop drinking. If trouble communicating, utilize props/tools, If physical ailments, utilize tools to assist in mobility, join a support group/obtain emotional support. Surgery: FOR CLOTS: Mechanical removal of clot, Carotid endarterectomy FOR HEMHORRAGING: -Coiling Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Ineffective Cerebral Tissue Perfusion -Impaired physical mobility r/t neuromuscular involvement: cognitive impairment, perceptual impairment, paresthesia, weakness Pt. Goals/ Evaluation: -Pt will maintain improved/usual cognition, LOC and motor/sensory function -Pt will maintain/increase function, of affected body part or compensatory body part 48 Hour Cram Sheets for Med Surg CEREBERAL VASCULAR ACCIDENT (CVA) Dx Tests: CT Scan, MRI, Carotid Doppler, EKG, ECG, cerebral arteriogram, magnetic resonance angiogram Simplenursing.com Less Study Time HIGHER test scores! -Surgical Clipping -Surgical AVM removal -Intracranial bypass Page 19 of 106 48 Hour Cram Sheets for Med Surg EPILEPSY EPILEPSY Patho: A disorder involving abnormal, sudden discharge of electrical activity in the brain. Epilepsy is not a singular disease, but is heterogeneous in terms of clinical expression, underlying etiologies, and pathophysiology . As such, specific mechanisms and pathways underlying specific seizure types may vary. Epileptic seizures are broadly classified according to their site of origin and pattern of spread. Assess: ASSESS FOR SAFE ENVIRONMENT WHILE PATIENT IS SEIZING! Maintain patent airway (Good to position the patient side-lying) Initiate seizure precautions/protect client from injury. DOCUMENT THE SEIZURE!! (Precipitating factors, type, duration, behavior before, during and after seizure/ aka “Postictal phase”, and if incontinent) Vitals: ↑TEMP, ↑HR, ↓BP S/S & PHYS. EXAM: Sensory/Thought: o Black out/Loss of consciousness o Confusion o Deafness/Sounds o Electric Shock Feeling o Spacing out o Out of body experience o Visual loss or blurring Nursing Interventions: Pharm: Dilantin, Phenobarbital, Tegretol, Depakote, Valium, Klonopin, Pt. Ed: Adherence to medication regimen as well as contra-indications and side effects! Surgery: Removal of anterior temporal lobe (For partial epilepsy/seizures), Usually in children: hemispherectomy, corpus callosotomy (separating of nerve fibers that connect the two sides of the brain) Emotional: o Fear/Panic o Pleasant feeling Physical: o Chewing movements o Convulsion o Difficulty talking/Drooling o Eyelid fluttering/rolling o Falling down o Foot stomping o Hand waving o Inability to move o Incontinence o Lip smacking/Making sounds o Shaking Page 20 of 106 Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Low self-esteem r/t social role changes, loss of control and stigma associated with disease -Risk for Trauma/Suffocatio n r/t loss of consciousness, coordination, weakness and reduced muscle/sensation Pt. Goals/ Evaluation: -Pt will verbalize concerns and fears about body, self perception and change of lifestyle -Pt will verbalize understanding of factors that contribute to trauma during a seizure, pt will be aware of seizure precautions that should be utilized, especially by 48 Hour Cram Sheets for Med Surg EPILEPSY CLASSIFIED AS GENERALIZED OR FOCAL: Generalized: 1. Tonic-clonic (grand-mal) Seizure: This seizure causes you to lose consciousness and often collapse. Your body becomes stiff during what's called the "tonic" phase. During the "clonic" phase, muscle contractions cause your body to jerk. 2. Absence (petit mal) Seizure: During these brief episodes, you lose awareness and stare blankly. Usually, there are no other symptoms. 3. Myoclonic Seizure: These very brief seizures cause your body to jerk, as if shocked by electricity, for a second or two. The jerks can range from a single muscle jerking to involvement of the entire body. 4. Clonic Seizure: This seizure cause rhythmic jerking motions of the arms and legs, sometimes on both sides of your body. 5. Tonic Seizure: Tonic seizures cause your muscles to suddenly stiffen, sometimes for as long as 20 seconds. If you're standing, you'll typically fall. o Staring o Stiffening o Swallowing o Sweating o Teeth clenching/grinding o Tongue biting o Twitching movements o Breathing difficulty o Tachycardia o Bruising o Difficulty talking o Injuries o Sleeping o Exhaustion o Headache o Nausea o Pain o Thirst o Weakness o Urge to urinate/defecate caretaker, family or friend Labs: CBC, Glucose, CSF (cerebral spinal fluid) analysis, Blood Culture (To rule out infection Dx Tests: EEG, MRI, CT Scan, PET Scan, ECG Simplenursing.com Less Study Time HIGHER test scores! Page 21 of 106 48 Hour Cram Sheets for Med Surg EPILEPSY 6. Akinetic or Atonic Seizure: This seizure causes your muscles to relax or lose strength, particularly in the arms and legs. Although you usually remain conscious, it can cause you to suddenly fall and lead to injuries. These seizures also are called "drop attacks" FOCAL SEIZURES 1. Simple Focal Seizure: During these seizures, you remain conscious although some people can't speak or move until the seizure is over. Uncontrolled movements, such as jerking or stiffening, can occur throughout your body. You also may experience emotions such as fear or rage or even joy; or odd sensations, such as ringing sounds or strange smells. 2. Complex Focal Seizure: During these seizures, you are not fully conscious and may appear to be in a dreamlike state. Typically, they start with a blank stare. You may involuntarily chew, walk, fidget, or perform other repetitive movements or simple actions, but actions are typically unorganized or confused 3. Secondarily Generalized Seizure: These seizures begin as a focal seizure and develop Into generalized ones as the electrical abnormality spreads throughout the brain. When the seizure begins, you may be fully conscious but then lose consciousness and Experience convulsions as it develops. Page 22 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg HEAD INJURY HEAD INJURY Patho: brain injuries can be classified as traumatic or acquired, with additional types under each heading. All brain injuries are described as either mild, moderate, or severe. Traumatic Brain Injury Traumatic brain injury is a result of an external force to the brain that results in a change to cognitive, physical, or emotional functioning. The impairments can be temporary or permanent Acquired Brain Injury An acquired brain injury is an injury to the brain that is not hereditary, congenital, degenerative, or the result of birth trauma. Acquired brain injury generally affects cells throughout the entire brain. A. Direct injury: Depression of skull, Direct injury or skull fracture B. Blow to head: Blow to the skull that may move the brain to a point which can cause damage to vessels or veins, contusion or hematoma Assess: Perform Neuro assessment, Assess for ALOC, Signs of confusion, bleeding/CSF in ears (halo sign), Assess intracranial pressure (Shouldn’t exceed 2025mmHg) Monitor MAP (Keep above 90mmHg), Elevate HOB to 30°, Monitor vital signs/ABG’s Vitals: ↑PAIN, may have ↑TEMP and/or ↑↓BP (depending on Injury) S/S & PHYS. EXAM: (Symptoms depend on the severity and distribution of brain injury) -A common manifestation is loss of consciousness, ranging from a few minutes to 1 hour or longer -Ecchymosis may be seen over the mastoid (Battle’s sign) -CT scan may reveal the area that is contused or injured X-Rays may reveal skull fractures Bloody spinal fluid suggests brain laceration or contusion -Brain injury may have various signs, including altered level of conscious-ness, pupil abnormalities, altered or absent gag reflex or corneal reflex, neurologic deficits, change in vital signs (e.g. respiration pattern, hypertension, bradycardia), hyperthermia or hypothermia, and sensory, vision or hearing impairment -Signs of a post-concussion symptoms may include headache, dizziness, anxiety, irritability, and lethargy -In acute or sub-acute subdural hematoma, changes in level of consciousness, papillary Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Analgesics, Mannitol, Lasix, barbiturates, corticosteroids Pt. Ed: Inform patient of signs and symptoms of ICP, confirm understanding of treatment regimen including medication, drains, etc. Communicate with family for signs of worsening condition and allow them to voice concerns. Surgery: To relieve excessive fluid/ICP (May install a drain), “Bone Flap” removed to relieve pressure, Removal of hematoma Page 23 of 106 Nursing Dx: -Ineffective Cerebral Tissue Perfusion -Impaired physical mobility r/t neuromuscular involvement: cognitive impairment, perceptual impairment, paresthesia, weakness Pt. Goals/ Evaluation: -Pt will maintain improved/usual cognition, LOC and motor/sensory function -Pt will maintain/increase function, of affected body part or compensatory body part 48 Hour Cram Sheets for Med Surg MULTIPLE SCLEROSIS (MS) C. Rebound/Contrecoup Injury: Rebound of cranial contents an cause an injury of the head on the OPPOSITE side of injury. Also known as contrecoup injury MULTIPLE SCLEROSIS (MS) Patho: REMEMBER! MS, Myelin Sheath!! Demyelination of nerve fibers within long conducting pathway of spinal cord and brain. Impaired transmission of never impulses. Degenerative changes myelin sheath are scattered irregularly throughout the central nervous system. Nerve axon also deteriorates. The areas involved are not consistent when it comes to deterioration thereby showing the signs and symptoms appear whenever the nerve conduction is interrupted -There are periods of remission also, however there are cases that symptoms are exacerbated especially when nerve impulse travel through the patchy never fibers. Page 24 of 106 signs, hemiparesis, coma, hyper-tension, bradycardia, and slowing respiratory rate are signs of expanding mass Labs: Na, Mg, PTT, aPTT, Platelets, BAC, renal function Dx Tests: MRI, CT scan, EEG, X-Ray Assess: Assess for cognitive, sensory and physical impairment, pain, numbness/paresthesia, extreme fatigue and inflammation. Also assess for medication adherence Vitals: S/S & PHYS. EXAM: -Spastic weakness – the most common sign -Charcots Triad: A combination of symptoms that includes nystagmus, intention tremor (motor weakness in coordination), scanning speech which is elicited by slowing enunciation with tendency to hesitate at beginning of a word. Nursing Interventions: Pharm: -Immuno-suppressants to reduce exacerbation: (Avonex IM weekly), Betaseron (Subcut), Copaxone (Subcut) -For muscle spasicity/tremors: Neurontin, Baclofen, Clonazapam -For Urinary Problems: Ditropan, Detrol -For sexual Dysfunction: Viagra -Depression: Zoloft. Prozac -Fatigue: Provigil, Symmetrel Pt. Ed: 1. Self-Injection techniques 2. Promote independence Visual disturbances 3. Self-Catheterization Nausea/Vomiting 4. Promote exercise daily, with Urinary retention or urinary incontinence fall precautions 5. Injury Prevention Dysphagia (difficulty in swallowing) 6. Stress reduction and immune Ataxia (decreased coordination) support to avoid infection Labs: CSF Analysis Hyper-emotions as well as euphoria Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx -Impaired physical mobility r/t neuromuscular involvement: cognitive impairment, perceptual impairment, parasthesia, weakness -Ineffective individual coping r/t uncertainty of course of MS Pt. Goals/ Evaluation: -Pt will maintain/ increase function, of affected body part or compensatory body part 48 Hour Cram Sheets for Med Surg MENINGITIS Dx Tests: MRI (Will show sclerotic patches brain/spinal cord) MENINGITIS Patho: Meningitis is the inflammation of the protective membranes covering the central nervous, known collectively as the meninges. Meningitis can be caused from a direct spread of a severe infection such as an ear infection or sinus infection. In some cases, meningitis is noted after head trauma or an injury to the head or brain. There are several causes of meningitis: Bacterial infection, Viral infection, Fungal infection, A reaction to medications, A reaction to medical treatments, Lupus, Some forms of cancer, A trauma to the head or back. Anyone can catch Surgery: None available at this time Assess: MONITOR TEMPERATURE!! Extremely high temp can be fatal. Assess for ALOC, Pain, sensory awareness/response Vitals: TEMP, PAIN S/S & PHYS. EXAM: -Fever -Nuchal (Neck) Rigidity/Pain/tenderness -Loss of appetite -Difficulty swallowing. -Anorexia/vomiting -Poor skin turgor/dry mucous membranes Labs: CSF Analysis Dx Tests: Lumbar puncture/spinal Tap Nursing Interventions: Pharm: IV Antibiotics (Rifampin/Vancomycin) Pt. Ed: Sit patient in comfortable position with adequate neck support, reduce environmental stimuli/stress, monitor hydration, antibiotics, seizure precautions Surgery: N/A meningitis. This is especially true if your immune system is weak. Simplenursing.com Less Study Time HIGHER test scores! Page 25 of 106 -Pt will verbalize acceptance of diagnosis, control over health status and demonstrate utilization of support systems Nursing Dx: -Pain r/t acute condition - Risk for infection transmission r/t contagious nature of organism Pt. Goals/ Evaluation: -Pt will verbalize pain level using numeric chart or “FACES” chart, as well as ways to reduce/treat pain -Initiate infection precautions and antibiotic therapy as ordered 48 Hour Cram Sheets for Med Surg PARKINSON’S PARKINSON’S Patho: Parkinson’s disease is a slowly progressive degenerative neurological disorder caused by the loss of nerve cell function in the basal ganglia. Loss of nerve cells in the substantia nigra causes a reduction of dopamine production. Dopamine is the neurotransmitter essential for such functions as control of posture, supporting the body in an upright position and voluntary motions. Assess: Assess for the 4 Cardinal signs of Parkinson’s: 1. Resting tremor 2. Rigidity 3. Bradykinesia 4. Postural instability *PATIENT IS A FALL RISK! Vitals: Normal, unless distressed S/S & PHYS. EXAM: Nursing Interventions: Pharm: Depends on age/severity: - Carbidopa/Levodopa therapy - Dopamine Agonists - Anticholinergics - MAO-B Inhibitors - COMT Inhibitors Pt. Ed: Assistance with ADL’s, Caretaker info, important information regarding the disease and depression, Surgery: None at this time -Tremor (rhythmic, purposeless, fine trembling, quivering movement), resting or passive tremor -Muscle rigidity (stiffness seen with resistance to passive muscle stretching), cogwheel rigidity -Akinesia (loss of movement) and bradykinesia (slowness of voluntary movement and speech) -Mask-like expression -Dysphagia (difficulty of swallowing) -Monotonous speech -Postural disturbances (stooped posture, shuffling gait, broad-based turns) Page 26 of 106 Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Impaired physical mobility r/t neuromuscular involvement: tremors, muscle rigidity, weakness -Self care deficit r/t neuromuscular weakness, decreased strength and loss of muscle control/ coordination, cognitive changes & postural changes Pt. Goals/ Evaluation: -Pt will maintain/ increase function, of affected body part or compensatory body part -Pt and caretaker will verbalize understanding of physical, cognitive and emotional limitations due to diagnosis 48 Hour Cram Sheets for Med Surg SEIZURE -Generalized muscle fatigue -Cognitive changes (impaired memory, depression) -Drooling -Constipation -Orthostatic hypotension - Urinary dysfunction Labs: NONE YET! Specialized imaging centers may have Brain Scans to measure dopamine and metabolism of brain, as well as genetic disposition/Biological marker Dx Tests: NONE YET! (A neurologist will diagnose based on history and symptoms) SEIZURE Patho: A disorder involving abnormal, sudden discharge of electrical activity in the brain. Epilepsy is not a singular disease, but is heterogeneous in terms of clinical expression, underlying etiologies, and pathophysiology. As such, specific mechanisms and pathways underlying specific seizure types may vary. Epileptic seizures are broadly classified according to their site of origin and pattern of spread. Assess: ASSESS FOR SAFE ENVIRONMENT WHILE PATIENT IS SEIZING! Maintain patent airway (Good to position the patient side-lying) Initiate seizure precautions/protect client from injury. DOCUMENT THE SEIZURE!! (Precipitating factors, type, duration, behavior before, during and after seizure/ aka “Postictal phase”, and if incontinent) Vitals: ↑TEMP, ↑HR, ↓BP S/S & PHYS. EXAM: Sensory/Thought: o Black out/Loss of consciousness o Confusion o Deafness/Sounds o Electric Shock Feeling o Spacing out Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Dilantin, Phenobarbital, Tegretol, Depakote, Valium, Klonopin, Pt. Ed: Adherence to medication regimen as well as contra-indications and side effects! Surgery: Removal of anterior temporal lobe (For partial epilepsy/seizures), Usually in children: hemispherectomy, corpus callosotomy (separating of nerve fibers that connect the two sides of the brain) Nursing Dx: -Low self-esteem r/t social role changes, loss of control and stigma associated with disease -Risk for Trauma/ Suffocation r/t loss of consciousness, coordination, weakness and reduced muscle/sensation Pt. Goals/ Evaluation: Page 27 of 106 48 Hour Cram Sheets for Med Surg SEIZURE o Out of body experience o Visual loss or blurring Emotional: o Fear/Panic o Pleasant feeling CLASSIFIED AS GENERALIZED OR FOCAL: Generalized: 1. Tonic-clonic (grand-mal) Seizure: This seizure causes you to lose consciousness and often collapse. Your body becomes stiff during what's called the "tonic" phase. During the "clonic" phase, muscle contractions cause your body to jerk. 2. Absence (petit mal) Seizure: During these brief episodes, you lose awareness Page 28 of 106 Physical: o Chewing movements o Convulsion o Difficulty talking/Drooling o Eyelid fluttering/rolling o Falling down o Foot stomping o Hand waving o Inability to move o Incontinence o Lip smacking/Making sounds o Shaking o Staring o Stiffening o Swallowing o Sweating o Teeth clenching/grinding o Tongue biting o Twitching movements o Breathing difficulty o Tachycardia o Bruising o Difficulty talking o Injuries o Sleeping o Exhaustion o Headache o Nausea o Pain o Thirst o Weakness o Urge to urinate/defecate Simplenursing.com Less Study Time HIGHER test scores! -Pt will verbalize concerns and fears about body, self perception and change of lifestyle -Pt will verbalize understanding of factors that contribute to trauma during a seizure, pt will be aware of seizure precautions that should be utilized, especially by caretaker, family or friend 48 Hour Cram Sheets for Med Surg SEIZURE and stare blankly. Usually, there are no other symptoms. 3. Myoclonic Seizure: These very brief seizures cause your body to jerk, as if shocked by electricity, for a second or two. The jerks can range from a single muscle jerking to involvement of the entire body. 4. Clonic Seizure: This seizure cause rhythmic jerking motions of the arms and legs, sometimes on both sides of your body. 5. Tonic Seizure: Tonic seizures cause your muscles to suddenly stiffen, sometimes for As long as 20 seconds. If you're standing, you'll typically fall. 6. Akinetic or Atonic Seizure: This seizure causes your muscles to relax or lose strength, particularly in the arms and legs. Although you usually remain conscious, it can cause you to suddenly fall and lead to injuries. These seizures also are called Labs: CBC, Glucose, CSF (cerebral spinal fluid) analysis, Blood Culture (To rule out infection Dx Tests: EEG, MRI, CT Scan, PET Scan, ECG "drop attacks" FOCAL SEIZURES 1. Simple Focal Seizure: During these seizures, you remain conscious although some people can't speak or move until the seizure is over. Uncontrolled movements, such as jerking or stiffening, can occur throughout your body. You also may experience emotions such as fear or rage or even joy; or odd sensations, such as ringing sounds or strange smells. Simplenursing.com Less Study Time HIGHER test scores! Page 29 of 106 48 Hour Cram Sheets for Med Surg SPINAL INJURY 2. Complex Focal Seizure: During these seizures, you are not fully conscious and may Appear to be in a dreamlike state. Typically, they start with a blank stare. You may involuntarily chew, walk, fidget, or perform other repetitive movements or simple actions, but actions are typically unorganized or confused 3. Secondarily Generalized Seizure: These seizures begin as a focal seizure and develop Into generalized ones as the electrical abnormality spreads throughout the brain. When the seizure begins, you may be fully conscious but then lose consciousness and Experience convulsions as it develops. SPINAL INJURY Patho: Spinal cord injuries cause myelopathy or damage to white matter or myelinated fiber tracts that carry signals to and from the brain. It also damages gray matter in the central part of the spine, causing segmental losses of interneurons and motorneurons. Spinal cord injury can occur from many causes, including: -Trauma such as automobile crashes, falls, gunshots, diving accidents, war injuries, etc. -Tumors such as right, ependymomas, astrocytomas, and metastatic cancer. -Ischemia resulting from occlusion of spinal blood vessels, including dissecting aortic aneurysms, emboli, arteriosclerosis. Page 30 of 106 Assess: ABC’s!! For reflexes, response to stimuli and level of injury, Neuro-exam! (GLASCOW COMA SCALE): Nursing Interventions: Pharm: None at this time to TREAT, but methylprednisolone/Solumedr ol may be given as medication to treat ACUTE spinal injury Pt. Ed: Assistance with ADL’s as needed, PT to become adjusted to wheelchair/prosthesis, Psychological care to deal with mental aspect of the loss, catheter care as needed, avoiding pressure ulcers/self care Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Impaired physical mobility r/t neuromuscular involvement: sensory/ perceptual impairment, parasthesia, weakness -Low self-esteem r/t social role changes, loss of control and recent diagnosis 48 Hour Cram Sheets for Med Surg SPINAL INJURY -Developmental disorders such as spina bifida, meningomyolcoele, and other Neurodegenerative diseases, such as Friedreich’s ataxia, spinocerebellar ataxia, etc. -Demyelinative diseases, such as Multiple Sclerosis. -Transverse myelitis, resulting from spinal cord stroke, inflammation, or other causes -Vascular malformations, such as arteriovenous malformation (AVM), dural Arteriovenous fistula (AVF), spinal hemangioma, cavernous angioma and Aneurysm. Surgery: None at this time for parasthesia, but surgery may be required to remove bone fragments (if any), or further secure the spine to prevent deformity. Vitals: DEPENDS ON THE INJURY!! S/S & PHYS. EXAM: -Impaired physical mobility -Disturbed sensory perception -Acute pain -Anticipatory grieving -Low self-esteem -Constipation or bowel incontinence -Impaired urinary elimination Labs: N/A Dx Tests: CT Scan, MRI, X-Ray Simplenursing.com Less Study Time HIGHER test scores! Page 31 of 106 Pt. Goals/ Evaluation: -Pt will maintain function, of unaffected body parts or compensatory body parts as well as correctly utilizing support and assistive devices -Pt will verbalize concerns and fears about body, self perception and change of lifestyle 48 Hour Cram Sheets for Med Surg GUILLAIN-BAR SYNDROME 3. NEURO: PNS DIAGNOSIS/PATHO GUILLAIN-BAR SYNDROME DATA Patho: Guillain-Barré syndrome is the result of a cellmediated and humoral immune attack on peripheral nerve myelin proteins that causes inflammatory demyelination. With the autoimmune attack, there is an influx of macrophages and other immune-mediated agents that attack myelin, cause inflammation and leave the axon unable to support nerve conduction Assess: Asses for S/S of ARDS! Assess respiratory status, monitor VS and ECG, Monitor for infection and signs of progression Vitals: HR, B P S/S & PHYS. EXAM: Autonomic changes: o Tachycardia, bradycardia, hypertension, or orthostatic hypotension o Increased sweating o Increased salivation o Constipation Other Symptoms: -Dyskinesia (inability to executive involuntary movements) -Weakness usually begins in the legs and progress upward (ascending paralysis) -Hyporeflexia (decreased DTRs) -Paresthesia (numbness), clumsiness -Blindness -Inability to swallow (dysphagia) or clear secretions Page 32 of 106 ACTION RESPONSE Nursing Interventions: Pharm: Plasmapheresis, IVIG (IV Immunoglobulin), Analgesics as needed Pt. Ed: Healing/recovery time may take up to 2 years. Referral to PT, OT, RT & ST (Speech therapy), educate patient on strategies to prevent complications/immobility Surgery: Laminectomy (Remove portion of the vertebrae) Diskectomy (Removal of herniated disk), Spinal Fusion (Fusion of vertebrae via the spinal process by using a bone graft) Nursing Dx: -Ineffective breathing pattern r/t respiratory muscle weakness or paralysis, decreased cough reflex and immobilization -Impaired physical mobility r/t neuromuscular involvement: cognitive impairment, perceptual impairment, paresthesia, weakness Simplenursing.com Less Study Time HIGHER test scores! Pt. Goals/ Evaluation: -Pt will maintain patent airway, demonstrate effective 48 Hour Cram Sheets for Med Surg MYASTHENIA GRAVIS -Alternate hypotension/hypertension Arrhythmias Labs: Lumbar Puncture Ganglioside Antibody tests Dx Tests: MRI, Pulmonary Function tests, Nerve conduction test, EMG (Electromyography) MYASTHENIA GRAVIS Patho: In myasthenia gravis, antibodies directed at the acetylcholine receptor sites impair transmission of impulses across the myoneural junction. Therefore, fewer receptors are available for stimulation, resulting in voluntary muscle weakness that escalates with continued activity… 80% of people with myasthenia gravis have either thymic hyperplasia or a thymic tumor, and the thymus gland is believed to be the site of antibody production Assess: Assess for Respiratory status/ABC’s, patent airway, progression of deterioration, muscle wasting. Also assess for factors that can contribute to exacerbation: -Infection -Pregnancy -Stress/Fatigue -Pregnancy -Increase in body temp/fever - Non-Compliance with meds Vitals: TEMP S/S & PHYS. EXAM: Simplenursing.com Less Study Time HIGHER test scores! breathing pattern and show evidence of adequate oxygenation -Pt will maintain/ increase function, of affected body part or compensatory body part Nursing Interventions: Pharm: Anticholinesterase medications (Atropine is the antidote), Pyridostimine, IMMUNOSUPPRESANTS: Prednisone, Azathioprine (A cytotoxic med), Plasmapheresis, IVIG (IV Immunoglobulin), Analgesics as needed Pt. Ed: Importance medication compliance, Aspiration precautions – Watch amount and consistency of food as well scheduling feedings during peak times of medication effect. Grouping ADL’s and Page 33 of 106 Nursing Dx: -Impaired gas exchange, r/t ineffective breathing pattern and muscle weakness -Risk for aspiration r/t difficulty swallowing Pt. Goals/ Evaluation: -Pt will maintain patent airway, demonstrate effective 48 Hour Cram Sheets for Med Surg MYASTHENIA GRAVIS -Ptosis - check palpebral fissure for drooping of upper eyelids implementing rest periods, referral to speech therapy and support (MG Foundation of America) Surgery: Thymectomy (Excision of the thymus) -Double vision -Mask like facial expression -Weakened laryngeal muscles leads to dysphagia (difficulty of swallowing, without food) -Hoarseness of voice -Respiratory muscle weakness leads to respiratory arrest -Extreme muscle weakness especially during activity or exertion in AM Labs: Edrophonium Choride (TENSOLIN IV TEST) – If given and after 5 minutes Page 34 of 106 Simplenursing.com Less Study Time HIGHER test scores! breathing pattern and show evidence of adequate oxygenation -No aspiration will occur. Patient and patients family will verbalize understanding of aspiration risk 48 Hour Cram Sheets for Med Surg MYASTHENIA GRAVIS symptoms are relived, it is considered a positive test for MG) Serum Acetylcholine Receptor Antibody test) Dx Tests: MRI, EMG (Electromyography) Simplenursing.com Less Study Time HIGHER test scores! Page 35 of 106 48 Hour Cram Sheets for Med Surg APPENDICITIS 4. GASTRO INTESTINAL (Lower) DIAGNOSIS/PATHO APPENDICITIS Patho: Appendicitis is usually caused by blockage of the lumen of the appendix. Obstruction causes the mucus produced by mucous appendix suffered dam. The longer the mucus is more and more, but the elastic wall of the appendix has limitations that lead to increased intraluminal pressure. These pressures will impede the flow of lymph resulting in mucosal edema and ulceration. At that time there was marked focal acute appendicitis with epigastric pain. If the flow is disrupted arterial wall infarction will occur followed by gangrene appendix. This stage is called appendicitis gangrenosa. If the appendix wall fragile, there will be a perforation, called perforated appendicitis. Page 36 of 106 DATA ACTION RESPONSE Assess: For guarding, with pain in RLQ, Positive McBurney’s sign (Pain located the right side of abdomen, located 1/3 the distance from the anterior superior iliac spine to the umbilicus): Nursing Interventions: Pharm: PAIN MANAGEMENT & ANTIBIOTICS UNTIL SURGERY!! Continue after surgery as well. Possibly blood if lost in surgery. Pt. Ed: Avoid applying heat to the area, Monitor for signs/symptoms of infection, mobility after surgery Surgery: APPENDECTOMY! **Must remove before appendix perforation– CAN CAUSE SEPTIC SHOCK!! Patient will notice a “Sudden relief of pain” which is a BAD SIGN!! Abdomen will become rigid, fever will SPIKE! Nursing Dx: -Acute pain r/t inflammation of tissues -Risk for infection r/t Inadequate primary defenses/surgery/perforation of tissues Vitals: TEMP S/S & PHYS. EXAM: Aching pain that begins around your navel and often shifts to your lower right abdomen. The pain occurs when you apply pressure to your lower right abdomen THEN, release the pressure on that area. When released, the Pt. will feel A LOT of pain!! (REBOUND TENDERNESS!!) Pain that worsens if you cough, walk Simplenursing.com Less Study Time HIGHER test scores! Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Pt will show no signs of infection including: Elevated temperature, WBC count, as well as pain and swelling at incision site 48 Hour Cram Sheets for Med Surg SBO (SMALL BOWEL OBSTRUCTION) or make other jarring movements, also Nausea, Vomiting, Loss of appetite, Lowgrade fever, Constipation, Inability to pass gas, Diarrhea, Abdominal swelling Labs: WBC, CBC, hematologic tests pre-surgery Dx Tests: CT scan/Ultrasound to assess for appendicitis, SBO (SMALL BOWEL OBSTRUCTION) Patho: Intestinal contents, fluid and gas accumulative above the intestinal obstruction. The abdominal distention and retention of fluid reduce the absorption of fluids and stimulate more gastric secretion. With increasing distention, pressure within the intestinal lumen increases, causing a decrease in venous and arteriolar capillary pressure. This causes edema, congestion, necrosis and eventual rupture or perforation of the intestinal wall, with resultant peritonitis. Reflux vomiting may be caused by abdominal distention. Vomiting results in a loss of hydrogen ions and potassium from the stomach, leading to a reduction of chlorides and potassium in the blood and to metabolic alkalosis. Dehydration and acidosis develop from loss of water and sodium. Assess: Observe and palpate abdomen for swollen/tender areas and lump, Listen to bowel sounds (or absence of), Assess for signs of perforation and sepsis/septic shock Vitals: TEMP S/S & PHYS. EXAM: - Cramping intermittent abdominal pain - Nausea - Vomiting - Diarrhea - Constipation - Inability to have a bowel movement/ pass gas - Swelling of the abdomen (distention) -Bad breath Labs: Serum chemistry, BUN, Creatinine, CBC, WBC, Urinalysis Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Stool Softener, STIMULANT Laxative Pt. Ed: eat foods high in fiber, drink lots of liquids Surgery: Laparoscopy, or Surgical Removal (For complete strangulation) Nursing Dx: -Deficient Fluid Volume related to nausea/vomiting, fever or diaphoresis -Acute Pain related to intestinal blockage, distention and rigidity Pt. Goals/ Evaluation: -Pt will demonstrate normal vital signs, balanced input and output - Pt will report pain at tolerable level and verbalize ways to manage it Page 37 of 106 48 Hour Cram Sheets for Med Surg CONSTIPATION With acute fluid losses hypovolemic shock may occur. CONSTIPATION Patho: Constipation, costiveness, or irregularity, is a condition of the digestive system in which a person experiences hard feces that are difficult to expel. This usually happens because the colon absorbs too much water from the food. If the food moves through the gastro-intestinal tract too slowly, the colon may absorb too much water, resulting in feces that are dry and hard. Defecation may be extremely painful, and in severe cases (fecal impaction) lead to symptoms of bowel obstruction Causes of constipation: -Diet -Hormones -Anatomical a side effect of medications (Opiates/Narcotics) -An illness or disorder Page 38 of 106 Dx Tests: Abdominal X-RAY, CT Scan Assess: For signs of bowel obstruction Vitals: PAIN S/S & PHYS. EXAM: - Pass fewer than three stools a week - Hard stools - Excessive strain during bowel movements - A sense of rectal blockage - Have a feeling of incomplete evacuation after having a bowel movement - Need to use manual maneuvers to have a bowel movement, such as finger evacuation or manipulation of your lower abdomen Nursing Interventions: Pharm: Stool softeners, Laxatives Pt. Ed: Stick to diet high in fiber, Know/PREVENT CAUSES: -Anal fissure -Bowel Obstruction -Colon Cancer -Bowel Stricture (Narrowing of Colon) -Abdominal/Rectal Cancer Surgery: Bowel obstruction removal if needed Labs: Blood tests for hormone imbalances Dx Tests: -Barium studies to look for obstruction of the colon -Colonoscopy to look for obstruction of the colon -Sigmoidoscopy Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Altered bowel elimination r/t low-fiber diet/inactivity -Alteration in Nutrition: Less Than Body Requirements related to loss of appetite/pain Pt. Goals/ Evaluation: -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids -Pt will report desire to eat, achieves an adequate Nutritional intake, Avoidance of irritating foods, increased awareness of dietary management and relief of pain. 48 Hour Cram Sheets for Med Surg HERNIA HERNIA Patho: When part of an internal organ bulges through a weak area of muscle. There are several types of hernias, including: -Inguinal: in the groin(most common type Think, “IN-GROINial” -Umbilical: around the belly button - Incision, through a scar - Hiatal, a small opening in the diaphragm where the upper part of the stomach can move up into the chest -Congenital diaphragmatic: A birth defect that requires surgery SIDE VIEW: Assess: Palpate for mass, Auscultate for bowel sounds! ABSENCE OF BOWEL SOUNDS COULD INDICATE STRANGULATION F HERNIA, A MEDICAL EMERGENCY!! This strangulation can lead to: OBSTRUCTION, ISCHEMIA, NECROSIS, AND PERFORATION! Vitals (Strangulation): TEMP, HR S/S & PHYS. EXAM: INGUINAL: -BUMP/Bulge in groin/testicles -Burning or tenderness -Pain when lifting something heavy or when exercising -Pressure in the groin or thigh HIATAL: -Acidic taste in the mouth - Belching - Difficulty swallowing - Epigastric pain/ burning (Can be from the stomach area up to the mouth) - Heartburn/Indigestion - Nausea/ Vomiting UMBILICAL: -BUMP/Bulge near umbilical area -Burning or tenderness -Pain when lifting something heavy or when exercising Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Analgesics for pain, stool softeners Pt. Ed: Hernias are common. They can affect men, women and children. A combination of muscle weakness and straining, such as with heavy lifting, might contribute. Some people are born with weak abdominal muscles and may be more likely to get a hernia. Surgery: Surgical repair of hernia a.k.a. Minimally Invasive Inguinal Hernia Repair (MIIHR), Herniorraphy laparoscopic repair Page 39 of 106 Nursing Dx: -Pain r/t abdominal swelling and pressure -Risk for infection r/t abdominal mass/obstruction Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -The patient will remain free from signs or symptoms of infection 48 Hour Cram Sheets for Med Surg PARALYTIC ILEUS -Pressure in abdomen Labs: WBC’s Dx Tests: Barium Swallow w/ Flouroscopy, X-RAY, Physical exam PARALYTIC ILEUS Patho: Paralytic ileus is the occurrence of intestinal blockage in the absence of an actual physical obstruction. This type of blockage is caused by a malfunction in the nerves and muscles in the intestineimpairing digestive movement. Causes include: Electrolyte imbalances, gastroenteritis, appendicitis, pancreatitis, surgical complications, and obstruction of the mesenteric artery, which supplies blood to the abdomen. Certain drugs and medications, such as opioids/sedatives, can cause ileus by slowing peristalsis (contractions that propel food through the digestive tract) Page 40 of 106 Assess: Presence of bowel sounds, Vitals: N/A (See S & S below ) S/S & PHYS. EXAM: - Abdominal swelling, distension or bloating -Constipation -Diarrhea -Foul-smelling breath -Gas -Absent bowel sounds -Nausea w/without vomiting - Stomach pain/spasms Labs: N/A Dx Tests: CT w/ Contrast, XRays, Clinical Evaluation Nursing Interventions: Pharm/TX: NG Tube w/ Continuous suction, Fluid and Electrolyte replacement, Pt. Ed: Avoid opiods and anticholingergics. Common causes of Paralytic Ileus: -Appendicitis -Botulism -Certain medications, such as opiates/ sedatives -Diabetic ketoacidosis (DKA) -Electrolyte imbalance -Gastroenteritis -Neonatal necrotizing enterocolitis (disease that causes death of intestinal tissue in newborns) Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Impaired bowel elimination r/t constipation and decreased dietary intake -Risk for shock r/t lack of body fluid volume Pt. Goals/ Evaluation: -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids -Pt will exhibit stable vital signs, consistently stable input and output, as well as satisfactory fluid and nutritional intake to meet the patients specific needs and avoid shock 48 Hour Cram Sheets for Med Surg ISCHEMIC BOWEL/COLITIS ISCHEMIC BOWEL/COLITIS Patho: Ischemia occurs secondary to hypo-perfusion of an intestinal segment. When hypo-perfusion occurs, collateral blood flow may preclude or minimize ischemia; however, the regions of the intestine with a solitary arterial supply, and the watershed areas, are both at increased risk of developing ischemia. The degree of intestinal injury is dependent on the duration and severity of ischemia. -In turn, Ischemia can cause Acute or sub-acute mucosal sloughing and ulcerations. The loss of the mucosal barrier allows for bacterial translocation and toxin absorption. Re-perfusion injury can also occur if blood supply is reestablished after a prolonged interruption. Segments of bowel which do not cause acute necrosis or perforation can heal with stenosis or stricture. These can cause ischemic bowel disease with long-term effects Assess: For signs and symptoms of sock/infection Vitals: TEMP/ HR, BP (if shock) S/S & PHYS. EXAM: Abdominal pain: o Abdominal pain is usually worse after meals and may be suddenly severe o Cramping abdominal pain o Generalized abdominal pain o Upper/Lower abdominal pain Abdominal tenderness o Right lower abdominal tenderness o Left lower abdominal tenderness o Right upper abdominal tenderness o Left upper abdominal tenderness o Upper abdominal tenderness o Lower abdominal tenderness Blood in the stool: o Black stool Simplenursing.com Less Study Time HIGHER test scores! -Obstruction of the mesenteric artery, which supplies blood to the abdomen -Pancreatitis -Surgical complications Surgery: Colonoscopic decompression, cecostomy (RARELY) Nursing Interventions: Pharm: IV fluids, Antibiotics (to prevent infection) Treatment for comorbidity/ underlying condition (Ex.- CHF) Pt. Ed: AVOID VASOCONSTRICTORS!! Surgery: IF NEEDED (Depending on the Cause), Surgery to: -Remove dead/ischemic tissue -Bypass/Repair blockage in intestine/intestinal artery -Repair a hole in your colon - Remove part of intestinal tract that is narrowed/causing a blockage Page 41 of 106 Nursing Dx: -Risk for shock r/t inadequate tissue perfusion -Impaired bowel elimination r/t constipation and decreased dietary intake Pt. Goals/ Evaluation: -Pt will exhibit stable vital signs, consistently stable input and output, as well as satisfactory fluid and nutritional intake to meet the patients specific needs and avoid shock -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids 48 Hour Cram Sheets for Med Surg VOLVULUS that can be: Mild and chronic or acute and resolved. VOLVULUS Patho: A volvulus is a bowel obstruction with a loop of bowel that has abnormally twisted on itself Strangulating obstruction is obstruction with compromised blood flow; it occurs in nearly 25% of patients with smallbowel obstruction. It is usually associated with hernia, volvulus, and intussusceptions. Strangulating Page 42 of 106 o Rectal bleeding o Red stools o Maroon stools o Constipation o Indigestion o Diarrhea o Nausea/Vomiting o Anorexia Labs: ↑WBC, Blood in GI Tract Dx Tests: Cinical Assessment, Endoscopy, Angiogram, Doppler Ultrasound or CT Scan of Abdomen Assess: Auscultate for highpitched bowel sounds, “rushing” sounds or absence of bowel sounds Vitals: ↓BP, ↑HR, ↑TEMP (Signs of infection/Shock) S/S & PHYS. EXAM: -Severe abdominal pain -Nausea -Vomiting (A lot of Bile) -Bloody Stools -Abdominal Distension -Palpable Mass Nursing Interventions: Pharm: Analgesics for pain, antibiotics for infection, IV Fluid replacement to facilitate perfusion and prevent shock Pt. Ed: -Smaller feedings are recommended, because large quantities of food overload the stomach and promote gastric reflux. -Encourage to eat slowly and to chew all food thoroughly so that it can pass easily into the stomach Labs: Stool Sample, Blood/Electrolyte abnormalities (↓Na, K, Chl. r/t vomiting), ↑HG Surgery: Surgical repair of & WBC’s (r/t strangulation) Volvulus Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Ineffective breathing pattern r/t abdominal distension interfering with normal lung expansion -Ineffective tissue perfusion: GI r/t bowel obstruction Pt. Goals/ Evaluation: -Pt will exhibit normal breathing pattern, effective depth, and report little to know difficulty breathing as well as Sp02 within normal limits for patient -Pt will exhibit stable vital signs, consistently stable input and output, as well as satisfactory fluid and nutritional intake to meet the 48 Hour Cram Sheets for Med Surg DIVERTICUITIS obstruction can progress to infarction and gangrene in as little as 6 h. Dx Tests: Upper GI X-ray WILL SHOW “COFFEE BEAN SIGN → ) Barium enema, CT scan DIVERTICUITIS Assess: Auscultate for ↓Bowel sounds Vitals: ↑HR, ↑RR, ↑TEMP S/S & PHYS. EXAM: -Tenderness, usually in the LLQ (left lower quadrant) -Bloating or gas -Fever and chills -Nausea and vomiting -Anorexia Labs: ↑WBC’s, ↓H&H Dx Tests: Abdominal X-Ray, colonoscopy, barium enema Patho: Diverticulitis is a common digestive disease particularly found in the large intestine. Diverticulitis develops from diverticulosis, which involves the formation of pouches (diverticula) on the outside of the colon. Diverticulitis results if one of these diverticula becomes inflamed. Simplenursing.com Less Study Time HIGHER test scores! patients specific needs and avoid shock Nursing Interventions: Pharm: Analgesics/Pain Management, Bulk Laxatives, Stimulant Laxatives, Saline Laxatives, Stool softeners, Antibiotics such as Metronidazole (FLAGYL), Antisposmodics Pt. Ed: Risk Factors for Dicerticula: • Low-fiber diet • Chronic constipation • Obesity Risk Factors for Diverticulitis: • Bacteria / food trapped in diverticula • Infection/Inflammation • Most common site for diverticulitis is the Sigmoid colon, because of fecal masses that irritate and increase pressure in the colon. Page 43 of 106 Nursing Dx: -Pain r/t inflamed bowel and possible peritonitis -Impaired bowel elimination r/t constipation and decreased dietary intake Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids 48 Hour Cram Sheets for Med Surg RESECTION OF INTESTINES Surgery: To remove the diseased/infected part of colon Assess: For signs of infection, peritonitis, shock Patho: Small bowel resection is surgery Vitals: TEMP to remove part or all of your small S/S & PHYS. EXAM: Depends bowel. It is done when part of your small on the reason for bowel bowel is blocked or diseased. The small resection surgery! Many bowel is also called the small intestine. diseases or ailments can lead to Most digestion (breaking down and this surgery s an option absorbing (Cancer? Polyp Groths? nutrients) of the food you eat takes place Tumors?) in the small intestine. Labs: CBC Dx Tests: Abdominal Ultrasound, CT Scan, EKG, Chest X-Ray, RESECTION OF INTESTINES Page 44 of 106 Nursing Interventions: Pharm: Enema, Antibiotics, Analgesics for pain, IV Fluids, Anesthesia Pt. Ed: BOWEL PREP!! If you have laparoscopic surgery: -You will have 3 - 5 small cuts in your lower belly. The surgeon will pass a camera and medical instruments through these cuts -You may also have a cut of about 2 to 3 inches if your surgeon needs to put a hand inside your belly to feel the intestine or remove the diseased segment -Your belly will be filled with gas to expand it. This makes it easy for the surgeon to see and work Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Pain r/t inflamed bowel and possible peritonitis -Impaired bowel elimination r/t constipation and decreased dietary intake Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids -The patient will remain free from signs or symptoms of infection 48 Hour Cram Sheets for Med Surg RESECTION OF INTESTINES If you have open surgery, you will probably have a cut about 6 inches long in your mid-belly: -Your surgeon will locate the part of your small intestine that is diseased -Then your surgeon will put clamps on both ends of this part to close it off -The surgeon will remove the diseased part In both kinds of surgery: -If there is enough healthy small intestine left, your surgeon will sew or staple the healthy ends of the small intestine back together -If you do not have enough healthy small intestine to reconnect, your surgeon will make an opening called a stoma through the skin of your belly. Your small intestine will be attached to the outer wall of your belly. Stool will go through the stoma into a drainage bag outside your body. This is called an ileostomy. The ileostomy may either be short term or permanent Simplenursing.com Less Study Time HIGHER test scores! Page 45 of 106 48 Hour Cram Sheets for Med Surg INFLAMMATORY BOWEL DISEASE INFLAMMATORY BOWEL DISEASE Patho: CROHNS!! Ulcerative colitis • Is an inflammatory disease of the submucosal layer of the colon and rectum characterized by continuously occurring ulcerations and shedding of intestinal epithelium. Fat deposits and muscular hypertrophy result in a narrow, short, and thickened bowel. COLORECTAL CANCER Patho: Colorectal cancer is a disease in which normal cells in the lining of the colon or rectum begin to change, start to grow uncontrollably, and no longer die. These changes usually take years to develop; however, in some cases of hereditary disease, changes can occur within months to years. Both genetic and Page 46 of 106 Assess: Color, volume frequency and consistency of stools, monitor F&E levels for dehydration Vitals: TEMP (Low-grade) S/S & PHYS. EXAM: CROHNS!! Ulcerative colitis • Severe diarrhea containing pus, blood and mucosa • Abdominal cramping and tenderness, fever • Anorexia and weight loss • Usually occurs in the descending colon and rectum Labs: H&H, C-Reactive protein, WBC, Dx Tests: Abdominal X-Ray Assess: Risk factors of colon cancer, Recently changed bowel habits Vitals: Normal unless infection, possibly TEMP S/S & PHYS. EXAM: Ascending (Right) Colon Cancer -Occult blood in stool -Anemia -Anorexia and weight loss Nursing Interventions: Pharm: Anti-Diarrheals, Aminosalicyates (5-ASA’s), Immune Modulators (Humira), TPN, Corticosteroids, Multivitamin and supplemental Iron, Pt. Ed: Refrain from foods that can be irritating to the bowel! Oral fluids, Surgery: IF needed, Proctolectomy with Ileostomy/ Colectomy with ileostomy Nursing Dx: -Pain r/t inflamed bowel -Impaired bowel elimination r/t constipation and decreased dietary intake Nursing Interventions: Pharm: Analgesics for pain Pt. Ed: Don’t miss your annual checkups!! Use of colostomy bag, avoid food that cause odor and gas, Medical supply stores locally to obtain bags/materials Nursing Dx: -Anticipatory grieving r/t change in body function and perceived potential death of patient - Disturbed body image r/t loss of diseased body part/loss of good health Surgery: Colostomy Simplenursing.com Less Study Time HIGHER test scores! Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Bowel Elimination as evidenced by Comfort of passage of stool, stool is soft and formed, passage of stool is achieved without aids 48 Hour Cram Sheets for Med Surg COLORECTAL CANCER environmental factors can cause the changes. Initially, the cell growth appears as a benign (noncancerous) polyp that can, over time, become a cancerous tumor. If not treated or removed, a polyp can become a potentially lifethreatening cancer. Recognizing and removing precancerous polyps before they become cancer can prevent colorectal cancer! Pt. Goals/ Evaluation: -Pt will identify and express feelings appropriately, verbalize understanding of the dying process, and support to cope - Client will discuss concerns, what to expect after chemo/surgery, and ways to limit anxiety about body image -Abdominal pain above umbilicus -Palpable mass Distal Colon/Rectal Cancer -Rectal bleeding -Changed in bowel habits -Constipation or Diarrhea -Pencil or ribbon – shaped stool - Tenesmus -Sensation of incomplete bowel emptying Dukes’ Classification of Colorectal Cancer -Stage A: Confined bowel mucosa, 80-90% 5-year survival rate -Stage B: Invading muscle wall -Stage C: Lymph node involvement -Stage D: Metastases or locally unresectable tumor, less than 5% 5-year survival rate Labs: Dx Tests: Colonoscopy Simplenursing.com Less Study Time HIGHER test scores! Page 47 of 106 48 Hour Cram Sheets for Med Surg HIP FRACTURE 5. ORTHOPEDICS (BONES) DIAGNOSIS/PATHO HIP FRACTURE DATA Patho: Fracture pathophysiology includes cortical disruption, peri-osteal damage, and damage to the intra-medullary and cancellous architecture. Histomorphometric studies have shown that cortical thinning and some decrease in trabecular bone mass and connectivity can be seen especially in Osteoporosis suggesting a lower quality of bone, and thus decreased mechanical strength resulting in fracture. An age-related decline in osteocyte viability has also been observed in experimental studies. An inflammatory response also occurs following fractures of the proximal femur. Page 48 of 106 Assess: For Hemhorrage and SHOCK!! **ALSO ASSESS for distal pulses to ensure circulation! Observe for signs of thrombophlebitis, report immediately Vitals: PAIN, BP, HR, S/S & PHYS. EXAM: -Inability to move immediately after a fall -Severe pain in your hip or groin -Inability to put weight on your leg on the side of your injured hip -Stiffness, bruising and swelling in and around your hip area -Shorter leg on the side of your injured hip -Turning outward of your leg on the side of your injured hip ACTION Nursing Interventions: Pharm: Analgesics for pain, Antibiotics for surgery prep, FLUIDS/BLOOD as necessary, *** Pt. Ed: Instruct client regarding fracture healing process, diagnostic procedures, treatment and its complications, home care, daily activities, diet, restrictions and follow-up. Encourage fluid intake and high protein, high vitamin, highcalcium diet. Teach the client appropriate crutch walking techniques Surgery: Hip Fracture repair, specific to injured site: Simplenursing.com Less Study Time HIGHER test scores! RESPONSE Nursing Dx: -Pain r/t injury -Risk for Shock r/t blood loss/Injury Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Pt will show signs of adequate tissue perfusion including stable vital signs and fluid status 48 Hour Cram Sheets for Med Surg TOTAL KNEE REPLACEMENT (TKR) Labs: CBC, PTT, PT, INR, H&H Dx Tests: X-RAY of Hip, MRI TOTAL KNEE REPLACEMENT (TKR) Patho: Knee replacement, or knee arthroplasty, is a surgical procedure to replace the weight bearing surfaces of the knee joint to relieve the pain and disability of osteoarthritis. It may be performed for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long standing Osteo- arthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement. Other major causes of debilitating pain include meniscus tears, cartilage defects, and ligament tears. Debilitating pain from osteoarthritis is much more common in the elderly. Knee replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal Assess: Assess wound/surgical incision for signs and symptoms of infection following surgery and for signs of shock, for pain, extreme shortening, circulation/ neurovascular status Vitals: PAIN, HR, RR S/S & PHYS. EXAM: Signs/Symptoms of whatever injury is causing the need for surgery! For Example… -Pain -Inflammation -Difficulty moving your knee -Popping/Clicking of knee -Joint Pain/Stiffness Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Anti-Coagulants, NSAIDS/Analgesics for pain (Including Morphine PCA) Pt. Ed: The operation typically involves substantial postoperative pain, and includes vigorous physical rehabilitation. The recovery period may be 6 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility. Use of helpful items such as toilet seat extender, Exercises to reduce risk of DVT Surgery: TKR is the surgery! Page 49 of 106 Nursing Dx: -Pain r/t surgical procedure -Impaired mobility r/t injury/recent surgery Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Patient will show signs and verbalize effective ways to properly mobilize using tools/physical assistance provided 48 Hour Cram Sheets for Med Surg LONG BONE INJURY and plastic components shaped to allow continued motion of the knee. -Lack of range of motion LONG BONE INJURY Labs: PT, PTT/INR, CBC, H&H Dx Tests: X-Ray, MRI, Bone Scan Assess: Distal pulses/neurovascular status, signs of infection, range of motion, complications Patho: When a bone is broken, the periosteum and blood vessels in the cortex, marrow, and surrounding soft tissues are disrupted. Bleeding occurs from the damaged ends of the bone and from the neighboring soft tissue. A clot (hematoma) forms within the medullary canal, between the fractured ends of the bone, and beneath the periosteum. Bone tissue immediately adjacent to the fracture dies. This necrotic tissue along with any debris in the fracture area stimulates an intense inflammatory response characterized by vasodilation, exudation of plasma and leukocytes, and infiltration by inflammatory leukocytes and mast cells. Within 48 hours after the injury, vascular tissue invades the fracture area from surrounding soft tissue and the marrow cavity, and blood flow to the entire bone is increased. Page 50 of 106 Vitals: PAIN, HR, RR S/S & PHYS. EXAM: -Pain at site -Edema/swelling -Decreased range of motion -Pressure at site -Muscle Spasms Nursing Interventions: Pharm: Analgesics for pain Pt. Ed: Instruct client about restrictions like not bending at waist or sitting with Buck traction and not turning below the waist with Russell traction. Encourage client verbalize feelings and problems regarding fracture. Labs: CBC, H&H PT, PTT/INR Dx Tests: X-RAY, MRI Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Pain r/ injury - Risk for peripheral Neurovascular dysfunction Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Pt will maintain adequate tissue perfusion AEB palpable pulses, skin warm and dry, normal sensation, stable vital signs, and adequate urinary output for patient. 48 Hour Cram Sheets for Med Surg OSTEOARTHRITIS (OA) OSTEOARTHRITIS (OA) Patho: The most common form of arthritis. It causes the deterioration of the joint cartilage and formation of reactive new bone at the margins and subchondral areas of the joint. This chronic degeneration results from a breakdown of chondrocytes, most often in the hips and knees. Osteoarthritis occurs equally in both sexes after age 40. The earliest symptoms appear in middle age and progress with advancing age. Depending on the site and severity of joint involvement, Assess: For contributing factors such as: -Female -Aging -Metabolic Disease -Smoker -Obesity -Repetitive use/abuse of Joints Surgery: Repair as needed Nursing Interventions: Pharm: NSAIDS, Corticosteroids, Topical analgesics Pt. Ed: Safe use of mobility devices provided, Correctly performing exercises as prescribed/treatment plan, physical therapy, prevention of complication, immuno-suppression caused by steroid use Surgery: Total Joint arthroplasty, total joint replacement as required Vitals: PAIN S/S & PHYS. EXAM: Simplenursing.com Less Study Time HIGHER test scores! Page 51 of 106 Nursing Dx: -Acute Pain r/t distension of tissues -Impaired physical mobility r/t skeletal deformity Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it 48 Hour Cram Sheets for Med Surg RHUMATOID ARTHRITIS (RA) disability can range from minor limitation of the fingers to near immobility in persons with hip or knee disease. Progression rates vary; joints may remain stable for years in the early stage of deterioration. RHUMATOID ARTHRITIS (RA) Patho: Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks the joints producing an inflammatory synovitis that often progresses to destruction of the articular cartilage and ankylosis of the joints. Rheumatoid arthritis can also produce diffuse inflammation in the lungs, pericardium, pleura, and sclera, and also nodular lesions, most common in subcutaneous tissue under the skin. Although the cause of rheumatoid arthritis is unknown, autoimmunity plays a pivotal role in its Page 52 of 106 -Joint pain -Joint stiffness -Joint tenderness -Limited range-ofmotion -Crepitus (crackling, grinding noise with movement) -Joint effusion (swelling) -Local inflammation -Bony enlargements and osteophyte formation Labs: Dx Tests: Bone scan, Dual Energy X-Ray Absorptiometry Scan (DEXA-Scan) Assess: For contributing factors such as: -Female -Physical and Emotional Stress -Young to middle age -Family History Vitals: PAIN S/S & PHYS. EXAM: -Tender, warm, swollen joints -Pt will maintain a position with absence r limitation of contractures, and display techniques/behaviors that enable continuation of activities Nursing Interventions: Pharm: NSAIDS, Corticosteroids, Disease Modifying Anti-Rheumatic drugs (DMARDs) like METHOTREXATE, LEFLUNOMIDE, BIOLOGIC RESPONSE MODIFIERS (BRM) administered parenterally HUMIRA, ENBREL Pt. Ed: Use of mobility devices and safety, prevention of infection/complications, Physical therapy exercises/Rehab, Surgery: Total Joint arthroplasty, total joint replacement as required Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Acute Pain r/t distension of tissues -Impaired physical mobility r/t skeletal deformity Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Pt will maintain a position with absence r 48 Hour Cram Sheets for Med Surg GOUT chronicity and progression. About 1% of the world’s population is afflicted by rheumatoid arthritis, women three times more often than men. Onset is most frequent between the ages of 40 and 50, but people of any age can be affected. It can be a disabling and painful condition, which can lead to substantial loss of functioning and mobility. It is diagnosed chiefly on symptoms and signs, but also with blood tests (especially a test called rheumatoid factor) and X-rays. Diagnosis and long-term management are typically performed by a rheumatologist, an expert in the diseases of joints and connective tissues. -Morning stiffness that may last for hours -Firm bumps of tissue under the skin on your arms (rheumatoid nodules) -Fatigue, fever and weight loss Labs: Positive Rheumatoid factor, synovial fluid analysis, antinuclear antibody test, Erythrocyte sedimentation rate, CReactive protein Dx Tests: X-Ray, MRI Assess: GOUT Vitals: Patho: Gout is a disorder of purine metabolism S/S & PHYS. EXAM: characterized by elevated uric acid levels with -Intense joint pain. deposition of urate crystals in joints and other Gout usually affects tissues. High uric acid levels result from the large joint of your decreased excretion of uric acid (90% of cases) big toe, but it can due to a wide variety of causes. The disorder occur in may progress from an asymptomatic stage your feet, ankles, through acute gouty arthritis, to chronic knees, hands and tophaceous gout. wrists. The pain is likely to be most severe within the first 12 to 24 hours after it begins. Simplenursing.com Less Study Time HIGHER test scores! limitation of contractures, and display techniques/behaviors that enable continuation of activities Nursing Interventions: Pharm: Short-Term Relief: Corticosteroids, Ibuprofen/ NSAIDS, Colchicines **DO NOT TAKE ASPIRIN, AS IT CAN RAISE URIC ACID LEVELS IN THE BLOOD! Uricosuric agents (Help to increase elimination of uric acid by the kidneys) Xanthine oxidase inhibitors (decreases uric acid production by the body) Colchicine (prevents flare-ups during the first months you have gout and are taking other medicines to lower uric acid levels) Page 53 of 106 Nursing Dx: -Impaired Physical Mobility r/t pain Pt. Goals/ Evaluation: -Patient will show signs and verbalize effective ways to properly mobilize using tools/physical assistance provided 48 Hour Cram Sheets for Med Surg GOUT -Lingering discomfort. After the most severe pain subsides, some joint discomfort may last from a few days to a few weeks. Later attacks are likely to last longer and affect more joints. -Inflammation and redness. The affected joint or joints become swollen, tender and red. Pegloticase (Krystexxa) Last resort, for Gout that hasn't responded to other treatment. Pt. Ed: Obesity, Excessive alcohol intake, Meats and fish high in purine and diuretics can cause Gout to flare up. Complications include erosive deforming arthritis, uric acid kidney stones, and urate nephropathy caused by hyperuricemia. Utilize rest periods to minimize additional pain. Surgery: Labs: Uric Acid Dx Tests: Page 54 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg PAD (PERIPHERAL ARTERY DISEASE) 6. VASCULAR DISORDERS DIAGNOSIS/PATHO DATA DX: PAD (PERIPHERAL ARTERY DISEASE) Patho: Peripheral ARTERIAL disease (PAD) is a systemic atherosclerotic process for which the major risk factors are similar to those for atherosclerosis in the carotid, coronary, and other vascular beds. Among the traditional risk factors for PAD, those with the strongest associations are advanced age, smoking, and diabetes mellitus. More recently, a number of nontraditional risk factors for PAD have also been recognized. This article briefly reviews the pathophysiology of PAD and the evidence supporting established and emerging risk factors for its development. Simplenursing.com Less Study Time HIGHER test scores! ACTION Assess: Assess skin for: Dependent rubor, cyanosis, ulcers, gangrene, decreased sensation or pulses Vitals: Cap Refill, Unequal/Weak Pulses, Pain S/S & PHYS. EXAM: Painful cramping in your hip, thigh or calf muscles after activity, such as walking or climbing stairs (inter-mittent claudication), Leg numb-ness or weakness, Cold feeling in your lower leg or foot, especially when compared with the other leg, Sores on your toes, feet or legs that won't heal, A change in the color of your legs, Hair loss or slower hair growth on your feet Nursing Interventions: Pharm: Anticoags: (Heparin, Lovenox, Aspirin, Coumadin), AntiPlatelets (Trental, Plavix), Vasodilators (Isoxsuprine, papaverine) Pt. Ed: Good foot care, do not cross legs, stop smoking, regular exercise, healthy diet, monitor/report symptoms Surgery: Angioplasty, Arterial revasculartization, artherectomy, arterial bypass (at arterial blockage), thrombectomy Page 55 of 106 RESPONSE Nursing Dx: -Chronic pain r/t intermittent claudication/ischemia -Activity intolerance r/t peripheral oxygen supply and demand - Risk for impaired skin integrity r/t altered circulation/sensation Pt. Goals/ Evaluation: -Client will report increased comfort level and adequate pain control - Client will demonstrate increased tolerance to physical activity and utilize the use of rest periods -Client will be free from signs of impaired skin integrity during their hospital stay. 48 Hour Cram Sheets for Med Surg PVD (PERIPHERAL VASCULAR DISEASE) and legs, Slower growth of your toenails, Shiny skin on your legs, No pulse/weak pulse in your legs or feet, ED in men Labs: Total Cholesterol, LDL (Lousy Cholest.), HDL (Happy Cholest.), Lipids, Triglycerides Dx Tests: Angiogram, Exercise/ Stress Test, Skin temperature studies, Oscillometry Dx: PVD (PERIPHERAL VASCULAR DISEASE) Patho: Peripheral VASCULAR disease, also known as arteriosclerosis obliterans, is primarily the result of athero-sclerosis. The atheroma consists of a core of cholesterol joined to proteins with a fibrous intravascular covering. This process may gradually progress to complete occlusion of medium and large arteries. The disease typically is segmental, with significant variation from patient to patient. Vascular Page 56 of 106 Assess: Cool, brown skin, Edema, ulcers, pain, Normal or decreased pulses, open wounds Vitals: Cap Refill, Unequal/Weak Pulses, Pain S/S & PHYS. EXAM: The most common symptom of peripheral vascular disease in the legs is pain in one or both calves, thighs, or hips. The pain usually occurs while you are Nursing Interventions: Pharm: Anti-coags: (Heparin, Lovenox, Aspirin, Coumadin), Pt. Ed: Good foot care, do not cross legs, stop smoking, regular exercise, healthy diet, monitor/report symptoms, avoid extreme temperatures, Use TED hose/Compression stockings Surgery: thrombectomy, Angioplasty, Arterial revasculartization, artherectomy, arterial bypass (at arterial blockage) Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: - Ineffective Tissue Perfusion: peripheral r/t interruption of vascular flow -Ineffective health maintenance r/t deficient knowledge regarding disease process Pt. Goals/ Evaluation: -Pt. will demonstrate adequate tissue perfusion AEB palpable peripheral pulses, and warm and dry skin 48 Hour Cram Sheets for Med Surg PVD (PERIPHERAL VASCULAR DISEASE) disease may manifest acutely when thrombi, emboli, or acute trauma compromises perfusion. Thromboses often occur in the lower extremities more frequently than in the upper extremities. Multiple factors pre-dispose patients for thrombosis. These factors include sepsis, hypotension, low cardiac output, aneurysms, aortic dissection, bypass grafts, and underlying atherosclerotic narrowing of the arterial lumen. Emboli, the most common cause of sudden ischemia, usually are of cardiac origin (80%); they also can originate from proximal atheroma, tumor, or foreign objects. Emboli tend to lodge at artery bifurcations or in areas where vessels abruptly narrow. The femoral artery bifurcation is the most common site (43%), followed by the iliac arteries (18%), the aorta (15%), and the popliteal arteries (15%). walking or climbing stairs and stops when you rest. This is because the muscles' demand for blood increases during walking and other exercise. The narrowed or blocked arteries cannot supply more blood, so the muscles are deprived of oxygen and other nutrients. This pain is called intermittent (comes and goes) claudication. It is usually a dull, cramping pain. It may also feel like a heaviness, tightness, or tiredness in the muscles of the legs. Cramps in the legs have several causes, but cramps that start with exercise and stop with rest most likely are due to intermittent. When the blood vessels in the legs are completely blocked, leg at night is very typical, and the individual almost always hangs his or her feet down to ease the pain. Hanging the legs down allows for blood to passively flow into the distal part of the legs Simplenursing.com Less Study Time HIGHER test scores! -Pt. will verbalize understanding of the disease process and adhere to the prescribed medication regimen Page 57 of 106 48 Hour Cram Sheets for Med Surg ANEURYSMS Labs: Total Cholesterol, LDL (Lousy Cholest.), HDL (Happy Cholest.), Lipids, Triglycerides Dx Tests: Isotope Studies, Ultra-Sonic flow detection Doppler Studies, Venous Pressure measurements Assess: For increasing severity of symptoms, **SUDDEN Dx: ANEURYSMS Patho: An aneurysm is a permanent localized dilation of an artery. This can enlarge the artery. The locations can differ, as well as the type and how they form, with DISSECTING being the most life-threatening: Types/Location: 1. AORTIC 2. CEREBERAL 3. PERIPHERAL Page 58 of 106 RELIEF OF A PAINFUL ANUERYMS IS A BAD SIGN!! LIKELY MEANS THAT THE ANUERYSM HAS RUPTURED AND IMMEDIATE SURGERY IS REQUIRED!! Vitals: HR (Weak pulses distal to aneurysm), BP, RR S/S & PHYS. EXAM: 1. AORTIC: AAA (Abdominal Aortic Aneurysm) w/ gnawing pain/pulsing in abdomen/back, Thoracic Aortic Nursing Interventions: Pharm: Pre-surgical Meds/Antibiotics, AntiHypertensives (to reduce blood pressure and decrease a chance of rupture), Beta Blockers, Calcium Channel Blockers, Vasodilators, Anti-Lipid/Plaque meds (STATINS!) Pt. Ed: Reduce stress, STOP SMOKING!! Lower BP, Healthy Diet/Lifestyle, Monitor changes to doctor, adhere to medication regimen. Surgery: Open abdominal Chest repair, Endovascular Repair (Aneurysm not removed but strengthened): Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Risk for deficient fluid volume r/t potential hemorrhage -Fear/Anxiety r/t emergency condition Pt. Goals/ Evaluation: -Pt will show no signs of hypovolemia/shock, and maintain fluid and electrolytes within acceptable levels for Patient -Pt will verbalize fears and Anxiety and ways to cope with such fears 48 Hour Cram Sheets for Med Surg ANEURYSMS Aneurysm : Pain radiates up to jaw, neck, coughing/hoarseness, shoulder blade pain. 2. CEREBERAL: Aneurysm in brain, “Worst headache of your life”, nausea/vomiting, pain behind eyes, , 3. PERIPHERAL: Pulsations, pains and sores in extremities, also gangrene (due to lack of circulation) Labs: Blood work such as Hg and Hct, Coags, checking for bleeding, monitoring for signs of hypovolemia Dx Tests: Ultrasound, Echocardiogram, Angiogram, MRI, CT Scan Simplenursing.com Less Study Time HIGHER test scores! Page 59 of 106 48 Hour Cram Sheets for Med Surg ASTHMA 7. RESPIRATORY DIAGNOSIS/PATHO ASTHMA Patho: Bronchial asthma is a chronic inflammatory disease of the airways, associated with recurrent, reversible airway obstruction with intermittent episodes of wheezing and dyspnea. Bronchial hypersensitivity is caused by various stimuli, which innervate the vagus nerve and beta adrenergic receptor cells of the airways, leading to bronchial smooth muscle constriction, hypersecretion of mucus, and mucosal edema. Page 60 of 106 DATA ACTION RESPONSE Assess: Assess for change in skin color/cyanosis, use of accessory muscles/labored breathing (Is this an attack or emergency?) Also changes in mentation/ALOC Vitals: Shallow RR (Commonly with Audible Wheezing), HR during attacks S/S & PHYS. EXAM: Feeling of tightness in the chest, difficulty in breathing or shortness of breath, wheezing, coughing (particularly at night). Labs: O2/cap. Refill, hypoxemia Dx Tests: Chest X-Rays, & Pulmonary Fx tests: Forced Vital Capacity/FVC (Volume of air exhaled from full inhalation to full exhalation), Forced Expiratory Volume in the first Second/FEV1 (Vol. of air blown out as hard as possible in the first SECOND of the most Nursing Interventions: Pharm: PREVENTATIVE THERAPY: (Flovent, Serevent, Singulair) RESCUE DRUGS (Albuterol, Atrovent, Theophylline) Pt. Ed: STOP SMOKING!! Adhere to medication regimen as prescribed, Reduce stress, monitor symptoms daily especially signs of an attack, report increasing symptoms to doctor. Surgery: N/A Nursing Dx: -Activity Intolerance r/t energy shift to meet muscle needs for breathing to overcome airway obstruction -Anxiety r/t inability to breathe effectively -Ineffective breathing pattern r/t anxiety Simplenursing.com Less Study Time HIGHER test scores! Pt. Goals/ Evaluation: -the patient will be able to demonstrate behaviors to improve airway clearance -Client will report ability to breathe comfortably 48 Hour Cram Sheets for Med Surg BRONCHITIS BRONCHITIS Patho: Bronchitis is an inflammation of the air passages within the lungs. It occurs when the trachea (windpipe) and the large and small bronchi (airways) within the lungs become inflamed because of infection or other causes. forceful exhalation after the greatest inhalation & Peak Expiratory Flow (Fastest airflow reached at any time during exhalation) Assess: Assess respiratory rate, depth. Note use of accessory muscles, pursed lip breathing, Inability to speak. Evaluate level of activity tolerance. Vitals: RR, S/S & PHYS. EXAM: Chronic Bronchitis: History of productive cough that lasts 3 months per year for 2 consecutive years, Persistent cough, known as smoker’s cough usually in cold weather, Persistent sputum production, Recurrent acute respiratory infection, Dusky color leading to cyanosis, Clubbing of fingers Labs: O2/cap. Refill, hypoxemia, H&H Dx Tests: Chest X-RAY, Sputum test, Pulmonary FX Tests (See above) Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Antibiotics for infection, Cough meds/Expectorants, NSAIDS Pt. Ed: STOP SMOKING!! Adhere to medication regimen as prescribed, Reduce stress, monitor symptoms daily especially signs of an attack, report increasing symptoms to doctor. Surgery: N/A Page 61 of 106 Nursing Dx: -Ineffective airway clearance r/t excessive thickened mucus secretion -Anxiety r/t potential chronic condition Pt. Goals/ Evaluation: -Client will demonstrate effective coughing and clear breath sounds -Client will identify, verbalize, and demonstrate techniques to control anxiety. 48 Hour Cram Sheets for Med Surg COPD (CHRONIC OBSTRUCTIVE PULMONARY DISEASE) Assess: Assist patient to assume position of comfort (ex. Elevate head of bed, encourage patient to lean on Patho: COPD disrupts airway side bed table dynamics, resulting in obstruction of or sit on the edge of the bed airflow into or out of the lungs. Vitals: RR (Shallow) Chronic Bronchitis: Hypertrophy and S/S & PHYS. EXAM: Chronic hypersecretion in goblet cells and cough, SOB while performing bronchial mucus glands leading to ADL’S (dyspnea), Frequent increased sputum secretions, respiratory infections, bronchial congestion, narrowing of Cyanosis, Fatigue, Producing a bronchioles, and small bronchi. lot of mucus/ Emphysema: Increased size of air phlegm/sputum), Wheezing spaces (i.e. “dead space”) with loss of Labs: ABG’s, H&H, O2 elastic recoil of lung due to Dx Tests: Chest X-RAY, hyperinflation of distal airways Sputum test, Pulmonary FX causing airway obstruction. Tests (See above), & Destruction of alveolar walls and Spirometry diffuse airway narrowing causes resistance to airflow because of loss of supporting structure and bronchospasm further impede airflow. COPD (CHRONIC OBSTRUCTIVE PULMONARY DISEASE) Page 62 of 106 Nursing Interventions: Pharm: Short and long acting Bronchodilators (tiotropium (Spiriva) salmeterol (Serevent) formoterol (Perforomist), OXYGEN! Pt. Ed: STOP SMOKING!! Adhere to medication regimen as prescribed, Reduce stress, monitor symptoms daily especially signs of an attack, report increasing symptoms to doctor. *Alternate activity and rest periods to prevent fatigue Surgery: Lung Reduction, Lung Transplant **For selected cases only, end-stage COPD Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Activity intolerance r/t imbalance between oxygen supply and demand -Ineffective Health Maintenance r/t deficient knowledge regarding care of disease Pt. Goals/ Evaluation: -Client will participate in physical activity and demonstrate appropriate changes in heart rate, breathing rate and blood pressure -Client will follow mutually agreed health maintenance plan 48 Hour Cram Sheets for Med Surg EMPHYSEMA EMPHYSEMA Patho: Decreased pulmonary elastic recoil. At any pleural pressure, the lung volume is higher than normal. Additionally, the altered relation between pleural and alveolar pressure facilitates expiratory dynamic compression of airways. Such compression limits airflow during forced expiration and, in severe instances, during tidal expiration. Another factor contributing to airflow limitation is disease of the airways, both large and small. In general, patients with relatively pure emphysema maintain blood gases in or near the normal range until very late in their course. PaO2 is maintained because of the preserved matching of ventilation and perfusion as alveolar walls are destroyed. PaCO2 is maintained because the ventilatory response to CO2 is not usually impaired. It is not clear why patients who are categorized clinically as "chronic bronchitics" are more likely to respond to an increased flowresistive work of breathing by hypoventilating. Physical findings in emphysema are not specific. Radiologic changes are insensitive Assess: Assess for signs and symptoms of hypoxia and hypercapnia, Monitor/record blood gas examination, examine trend in the increase or decrease in PaO2 or PaCO2 Vitals: RR (SOB/Adventitious lung sounds), HR, O2 S/S & PHYS. EXAM: Shortness of Breath, Rapid Breathing, Chronic Cough (With or Without Sputum), Wheezing, Reduced Exercise Tolerance, Loss of Appetite Leading to Weight Loss, Barrel Chest Labs: CBC, O2, ABG’S Dx Tests: Chest X-RAY, Pulmonary Fx Tests, CT scan Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Bronchodilators, Expectorants, Corticosteroids, Oxygen Pt. Ed: STOP SMOKING!! Adhere to medication regimen as prescribed, Reduce stress, monitor symptoms daily especially signs of an attack, report increasing symptoms to doctor. *Alternate activity and rest periods to prevent fatigue Surgery: Lung Reduction, Lung Transplant **For selected cases only, Emphysema NOT caused by smoking Page 63 of 106 Nursing Dx: -Activity intolerance r/t imbalance between oxygen supply and demand -Ineffective Health Maintenance r/t deficient knowledge regarding care of disease Pt. Goals/ Evaluation: -Client will participate in physical activity and demonstrate appropriate changes in heart rate, breathing rate and blood pressure -Client will follow mutually agreed health maintenance plan 48 Hour Cram Sheets for Med Surg HEMOTHORAX and are of less value than physiologic measurements. HEMOTHORAX Patho: Roughly Translated, HEMOTHORAX means blood (HEMO) in the pleural cavity (THORAX). This condition can be caused by a number of factors, when anything penetrates the pleural wall causing blood to enter the pleural space, including a gun shot wound or stabbing. A hemothorax is managed by removing the source of bleeding and by draining the blood already in the thoracic cavity. Blood in the cavity can be removed by inserting a drain (chest tube) in a procedure called a tube thoracostomy. Usually the lung will expand and the bleeding will stop after a chest tube is inserted. The blood in the chest can thicken as the clotting cascade is activated when the blood leaves the blood vessels and is activated by the pleural surface, injured lung or chest wall, or contact with the chest tube. Page 64 of 106 Assess: Trauma (penetrating or blunt) Signs of Shock or Arrest Vitals: O2 Sat, RR, HR S/S & PHYS. EXAM: Dyspnea, Cyanosis, Tachypnea, Hyperventilation, Dullness on percussion, Diminished/Absent lung sounds Retained Hemothorax: In this case, patients can be hypoxic, short of breath, or in some cases, the retained hemothorax can become infected (empyema). Labs: H& H, CBC, Red Blood Cell, ABG’s, PT, INR Dx Tests: Chest X-Ray , Thoracentesis, MRI Nursing Interventions: Pharm: Oxygen, Morphine/ analgesics for pain, Antibiotics for infection Pt. Ed: Sit in High-Fowlers, Monitor chest tube/dressing Surgery: Chest tube insertion/ drainage system Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Deficient Fluid Volume r/t blood in pleural space -Ineffective breathing pattern r/t chest pain/lung injury Pt. Goals/ Evaluation: -Patient will maintain blood pressure, pulse, body temperature and breathing patterns within acceptable range for patient - 48 Hour Cram Sheets for Med Surg PNEUMOTHORAX As the blood thickens, it can clot in the pleural space (leading to a retained hemothorax) or within the chest tube, leading to chest tube clogging or occlusion. Chest tube clogging or occlusion can lead to worse outcomes as it prevents adequate drainage of the pleural space, contributing to the problem of retained hemothorax. PNEUMOTHORAX Patho: Pneumothorax refers to gas within the pleural space. Normally, the alveolar pressure is greater than the intrapleural pressure, while the intrapleural pressure is less than atmospheric pressure. Therefore, if a communication develops between an alveolus and the pleural space or between the atmosphere and the pleural space, gases will follow the pressure gradient and flow into the pleural space. This flow will continue until the pressure gradient no longer exists or the abnormal communication has been sealed. Since the thoracic cavity is normally below its resting volume, and the lung is above its resting volume, the thoracic cavity enlarges and the lung Assess: Trauma (penetrating or blunt) Signs of Shock or Arrest Vitals: O2 Sat, RR, HR S/S & PHYS. EXAM: Dyspnea, Cyanosis, Tachypnea, Hyperventilation, Dullness on percussion, Diminished/Absent lung sounds Labs: H& H, CBC, Red Blood Cell, ABG’s, PT, INR Dx Tests: Chest X-Ray , Thoracentesis, MRI Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Oxygen, Morphine/ analgesics for pain, Antibiotics for infection, O2 Pt. Ed: Sit in High-Fowlers, Monitor chest tube/dressing, verbalize signs of infection, medication compliance Surgery: Chest tube insertion Nursing Dx: -Ineffective Breathing pattern r/t decreased lung expansion - Risk for Suffocation r/t dependence on external device (Chest Tube) Pt. Goals/ Evaluation: -Pt will establish a normal and effective breathing pattern with ABG’s within normal range for patient -Pt will recognize need for assistance to prevent complications Page 65 of 106 48 Hour Cram Sheets for Med Surg PNEUMONIA becomes smaller when a Pneumothorax develops. -A tension Pneumothorax is a medical emergency and occurs when the intrapleural pressure exceeds atmospheric pressure, especially during expiration, and results from a ball valve mechanism that promotes inspiratory accumulation of pleural gases. The build-up of pressure within the pleural space eventually results in hypoxemia and respiratory failure from compression of the lung. PNEUMONIA Patho: Pneumonia is an acute inflammatory disorder of lung parenchyma that results in edema of lung tissues and movement of fluid into the alveoli. These impair gas exchange resulting in hypoxemia. Pneumonia can be classified in several ways. Based on microbiologic etiology, it may be viral, bacterial, fungal, protozoa, myobacterial, mycoplasmal, or rickettsial in origin. Based on location, pneumonia may be classified as broncho-pneumonia, lobular pneumonia, or lobar pneumonia. Broncho-pneumonia Page 66 of 106 Assess: For respiratory shock, abnormal sputum, Fluid status Vitals: S/S & PHYS. EXAM: Tachypnea, Tachycardia, Crackles, Productive cough, WBC, O2 Sat. Dyspnea w/ Pleural pain, chills, fever, diaphoresis Labs: WBC, Sputum culture and sensitivity (C&S) Dx Tests: Chest X-Ray, Pulse Oximetry Nursing Interventions: Pharm: Antibiotics, Antipyretics, antiinflammatory, bronchodilators Pt. Ed: Medication Administration/compliance, Pneumonia/Influenza vaccine Surgery: chest tube/Thoracentesis Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Impaired gas exchange r/t changes in alveolar membrane -Ineffective airway clearance r/t inflammation and secretion build-up Pt. Goals/ Evaluation: -Pt will show improved ventilation and gas exchange, -Pulmonary Ventilation is adequate with no secretion build-up 48 Hour Cram Sheets for Med Surg PULMONARY EMBOLISM involves distal airways and alveoli; lobular pneumonia, part of the lobe; and labor pneumonia, the whole lobe. PULMONARY EMBOLISM Patho: A thrombus that has separated from its site of origin travels through the circulation to the inferior vena cava. The right ventricle pumps this thrombus to the pulmonary arteries where the thrombus finally lodges. PE may occur singly or multiply. They can be microscopic in size or be big enough to occlude the major branches of the pulmonary artery. Recurrent PE may gradually obstruct the pulmonary vasculature and ultimately lead to chronic obstructive pulmonary hypertension and cor pulmonale. Assess: Respiratory Status and Vital signs, IV access, Signs of Stroke/Shock, Position of comfort/HIGH FOWLERS Vitals: HR, O2 Sat. RR (Dyspnea) S/S & PHYS. EXAM: *PETICHIAL RASH PRESENT WITH FAT EMBOLISM! Chest Pain, Anxiety, Diaphoresis, Pleural Effusion, crackles/cough Labs: D-dimer, H&H, CBC Dx Tests: Chest X-Ray, MRI, Pulmonary Angiography Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Anti-thrombolytics/clotbusters (tPA if within 3 Hour time frame) , Anticoagulants, OXYGEN Pt. Ed: Follow up on labs (PT/INR), Report new symptoms/worsening pain. Preventative measures/ medication , Dietary precautions (Vitamin K), Bleeding Precautions, Follow up on PT/INR Surgery: Embolectomy, Vena Cava filter Page 67 of 106 Nursing Dx: -Impaired gas exchange r/t decreased pulmonary perfusion -Acute Pain r/t pulmonary flow obstruction Pt. Goals/ Evaluation: -Pt will demonstrate improved ventilation and adequate oxygenation as evidenced by ABG’s within normal limits for patient -Pt. will report pain at a comfortable and tolerable level 48 Hour Cram Sheets for Med Surg RESPIRATORY FAILURE Assess: Chest Pain, SOB, Restless, anxiety, confusion, Patho: Respiratory failure can arise **ASSESS FOR SIGNS OF from an abnormality in any of the SHOCK components of the respiratory Vitals: RR, HR, O2, system, including the airways, BP alveoli, central nervous system (CNS), S/S & PHYS. EXAM: peripheral nervous system, Bluish coloration of the lips or respiratory muscles, and chest wall. fingernail, Confusion or loss of Patients who have hypoperfusion consciousness, Fainting or secondary to cardiogenic, change in level of Hypovolemic, or septic shock often consciousness or lethargy present with respiratory failure. Fatigue, Irregular heart rate (arrhythmia), Rapid breathing (tachypnea) or shortness of breath Labs: CBC, Chem Panel, Serum Creatinine Kinease & Troponin (To rule out MI) and TSH (To rule out hypothyroidism) Dx Tests: Monitor location of embolism if any, Chest X-Ray, RESPIRATORY FAILURE Page 68 of 106 Nursing Interventions: Pharm: Oxygen, Diuretics (Lasix), Nitroglycerin (To reduce preload/ afterload), Morphine (Pain/Venodilation), Beta2 Agonists (Albeuterol, Terbutaline), Atrovent, Corticosteroids (Methylprednisolone) Pt. Ed: Sit in a position of comfort (one that promotes effective breathing) such as High Fowlers, medication compliance, Oxygen use and need, report new/worsening symptoms. Surgery: Tracheotomy/Ventilator if needed, (AIRWAY IS ALWAYS #1!!), Lung Transplant (if eligible) Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Ineffective breathing pattern r/t decreased lung compliance -Impaired respiratory function r/t inability to maintain adequate oxygenation of the respiratory tract and perfusion of oxygen Pt. Goals/ Evaluation: -Pt will report ability to breathe comfortably and -Client will exhibit positive signs of perfusion including O2 Sat. levels and ABG’s within normal patient limits 48 Hour Cram Sheets for Med Surg TUBERCULOSIS TUBERCULOSIS Patho: Tuberculosis is an infectious disease caused by the Myobacterium Tuberculosis. Transmission occurs when droplet nuclei are produced form an infected person’s coughs or sneezes. (AIRBORNE ROUTE). If inhaled, tubercle bacillus settles in the alveolus and infection occurs, with alveolocapillary dilation and endothelial swelling. The incubation time for TB is 4 to 8 weeks. TB is usually asymptomatic in primary infection. The risk of TB is a higher in older people who have close contact with a newly diagnosed TB patient, those who have TB before, gastrectomy patients, and those affected with diabetes mellitus. The aging process weakens the immune system, further increasing the likelihood of tubercular infection in older adults. Assess: *AIRBORNE ISOLATION PRECAUTIONS!! Assess Lung sounds, Hemoptysis, Monitor Liver/Kidney function Vitals: TEMP (low grade) S/S & PHYS. EXAM: Cough, Hemoptysis, Low grade fever/NIGHT SWEATS, Anorexia/Weight-loss, Malaise/Fatigue Labs: POSITIVE Sputum Culture for for acid-fast bacillus (AFB), Serum analysis, Serum Analysis QFT-G (Quantiferon Tuberculosis Gold) Dx Tests: Chest X-RAY, Mantoux Tuberculin skin test (TST) Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: COMBINATION DRUG THERAPY: Isonazid (INH), Rifampin, Pyrazinamide, Streptomycin, Ethambutol Pt. Ed: Prevent the spread of this airborne infection! Practice good hand hygiene, cover mouth when coughing or sneezing, ensure medication compliance as well as diligent follow up appointments *AS A MEDICAL PROFESSIONAL, ALL DIAGNOSED CASES OF TB MUST BE REPORTED TO LOCAL/STATE HEALTH DEPARTMENT! Surgery: N/A Page 69 of 106 Nursing Dx: -Ineffective breathing pattern related to acute infection and decreased lung capacity -Risk for infection (spread) r/t lowered resistance/suppressed inflammatory process Pt. Goals/ Evaluation: - Pt’s breathing will return to rate and pattern within their normal limits -Pt will exhibit minimal or no signs of infection. 48 Hour Cram Sheets for Med Surg URI (UPPER RESPIRATORY INFECTION) URI (UPPER RESPIRATORY INFECTION) Patho: A URI is a common infection that affects the nose, throat and airways. Caused by Bacteria and Viruses, this type of infection is very common and contagious as well. Examples include: Sinus infection, Common Cold (aka Rhinitus) nasopharyngitis, Laryngitis, Laryngotracheitis, and Tracheitis The common time of occurrence is in the winter months, from September to March. Page 70 of 106 Assess: Lung breath sounds, labor of breathing, cough, related symptoms Vitals: Temp S/S & PHYS. EXAM: Itchy, watery eyes, nasal discharge, nasal congestion, Sneezing, sore throat, cough, head- ache, fever, malaise, fatigue, weakness, muscle pain Labs: Sputum/Culture Dx Tests: Sputum/Culture, Rapid strep test (if suspected), Monospot test (If enlarged lymphnodes/Mono suspected), and Allerfy/Asthma evaluation Nursing Interventions: Pharm: Treat the cause! If infection (strep throat, epiglottitis & bacterial sinusitis): Antibiotics, Common cold (Can only treat symptoms) with Tylenol/NSAID’s for fever/body aches, Steriods for broncho-inflammation, & Decongestants for nasal issues. Pt. Ed: Decongestants are NOT recommended for Pt’s w/ high BP. Surgery: N/A Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -ineffective Airway Clearance related to thick secretions and airway obstructions -Acute pain r/t swelling in throat Pt. Goals/ Evaluation: -Pt will be able to cough effectively and clear own secretions, and maintain patency of airway and had clear breath sounds -Patient will report relief of pain with analgesic administration 48 Hour Cram Sheets for Med Surg ANGINA 8. CARDIAC (HEART) DIAGNOSIS/PATHO ANGINA Patho: Basic term for “Chest Pain”. Commonly assoc. w/ CAD, cholesterol & plaque in vessels. Triggered by phys. Activity/stress. SNS sys. Activates vasoconstriction of vessels… smaller tube brings more O2 back to heart, brain and lungs, where it is needed most. 2 types: Stable: caused by phys. Activity, but stops when activity stops. STABLE STOPS! Unstable: Even after stopping activity, pain is still there. May be due to blockage/clot in artery, or a clot that becomes loose as the vessels shrink and expand. Lack of O2 to heart…Can lead to MI/ Ischemia!! DATA Assess: Vital signs/pain such as facial grimacing, rubbing of neck or jaw, reluctance to move, increased blood pressure, and tachycardia. Vitals: BP, HR, O2 SAT S/S & PHYS. EXAM: pain (May radiate down L arm), SOB, Diaphoresis/Cool/Clammy skin, Syncope, anxiety Labs: Cardiac Enzymes, Cholesterol/Lipids, H&H Dx Tests: EKG, Echocardiogram, Stress test, Angiogram Simplenursing.com Less Study Time HIGHER test scores! ACTION Nursing Interventions: Pharm: M – O – N – A MORPINE (Pain mgmt, last resort, can numb Pt./mask symptoms) OXYGEN (O2 to left ventricle) NITROGYLCERIN ( vasodilation) **Contraindicated in Pts on Vasodilators/Viagra! ASPIRIN (Breaks up congregating plts) *Position Pt. in Semi-Fowlers position. Pt. Ed: NO smoking, healthy diet, limit sodium, exercise program, stress, cholesterol, BP Surgery: Angioplasty/Stent, CABG to check for and clear blockage if present. Page 71 of 106 RESPONSE Nursing Dx: -Acute Pain r/t decreased myocardial blood flow -Activity Intolerance r/t acute pain/dysrhythmias Pt. Goals/Evaluation: -Patient will be free from pain, maintain stable vital signs and show no visual signs of pain -Pt. will demonstrate tolerance to activity. Assess effectiveness of nitro; assess vital signs, pain control, as well as Pt. S/S and EKG for any sign of infarction/ arrhythmias. 48 Hour Cram Sheets for Med Surg ARRHYTHMIAS ARRHYTHMIAS Patho: Disturbance in impulse formation/conduction/communication. 4 TYPES: Suppressed Automaticity (SA node doesn’t fire effectively/up to speed, can lead to Pacemaker Placement), Enhanced Automaticity (Can result in multiple arrhythmias, ATRIAL & FIB. due to increased rate/impulse) Triggered Activity (An early or late depolarizations can trigger/ precipitate Ventricular arrhythmias… EX: torsades de pointes, Digoxin Toxicity) & Re-entry (Current or past MI/infarction/scarring or a block at a node can conceal accessory pathways and cause the re-entry of the conduction signal in the heart. Page 72 of 106 Assess: Assess and record apical pulse, peripheral pulses, blood pressure, capillary filling time, fluid intake/output, and skin for striped skin, skin color, edema, temperature, diaphoresis. Vitals: Pain, Change in HR/Rhythm, O2, BP S/S & PHYS. EXAM: Palpitations (a feeling of skipped heart beats, fluttering or feeling that your heart is "running away"). Pounding in your chest, Dizziness/ Syncope, SOB, Chest discomfort, Weakness or fatigue (feeling very tired). Labs: ECG/EKG, no blood tests to determine. Dx Tests: EKG Nursing Interventions: Pharm: OXYGEN! Nitro (Vasodilator) RX Depends on the Arrhythmia: PSVT/WPW Synd/A-Flutt: Diltiazem, Adenosine (Slows Vent. Rate by AV Block). Digoxin (Supraventricular Arrhythmias) Pt. Ed: Report S/S to Physician, Limit salt intake, Monitor B/P, Follow up with meds as prescribed, DO NOT take nitro w/ other Vasodilators like Viagra, Monitor BP/HR/Daily weights Surgery: Pacemaker to regulate heart rate, Cardio-aversion, Vagal Stimulation (Temporary) Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Activity intolerance r/t decreased cardiac output -Decreased cardiac output r/t altered electrical conduction Pt. Goals/Evaluation: -Patient will participate in phys. Activity with appropriate changes in vital signs. -Patient will demonstrate adequate cardiac output AEB: BP, HR and Rhythm within normal parameters for Patient and without pain. 48 Hour Cram Sheets for Med Surg ACUTE CORONARY SYND. (ACS) ACUTE CORONARY SYND. (ACS) Patho: Acute coronary syndrome is a term used for any condition brought on by sudden, reduced blood flow to the heart. Can be chest pain you feel during a heart attack, or chest pain you feel while you're at rest or doing light physical activity (unstable angina). It is believed that atherosclerotic plaque ruptures in the artery, resulting in clot formation and vasoconstriction, thus leading to decreased cardiac output. The “Freeways”/ Arteries of your heart become blocked or Jammed. Assess: Reported Pain, BP, Apical HR & Urinary output. Vitals: Pain, BP, HR & O2 (may lead to bradycardia/inadequate perfusion) S/S & PHYS. EXAM: Chest pain, Referred pain, N/V, SOB, Diaphoresis & Anxiety Labs: Cholesterol, Triglycerides, Blood Glucose, Serum Lipid levels Dx Tests: EKG (To rule out MI), Computed tomography coronary angiography (CTCA), Angiogram (To determine blockage, if any) Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Depends on the lipid levels, but most commonly used are the “Statins” (ex. Atorvastatin/Lipitor, Rosuvastatin/Crestor) Pt. Ed: Modify common risk factors, including: Smoking, Tobacco use, Diet, Exercise, Stress, Alcohol Use Surgery: Angioplasty, Stent/Balloon placement, CABG if necessary. Page 73 of 106 Nursing Dx: -Decreased cardiac output r/t ischemia -Acute pain r/t myocardial issue damage r/t inadequate blood supply. Pt. Goals/Evaluation: -Patient will demonstrate adequate cardiac output AEB: BP, HR and Rhythm within normal parameters for Patient and without pain. -Pt. will report that pain management regimen is satisfactory to pain tolerance standards. 48 Hour Cram Sheets for Med Surg ATRIAL FIBRILLATION (A-FIB) ATRIAL FIBRILLATION (A-FIB) Patho: 1. Primary arrhythmia in the absence of identifiable structural heart disease 2. Secondary arrhythmia in the absence of structural heart disease but in the presence of systemic abnormality that predisposes the individual to the arrhythmia 3. Secondary arrhythmia associated with cardiac disease that affects the atria CAN BE: Acute, Chronic, and Lone/Primary. - Acute AF: This has an onset within 2448 hours of the causative event and usually converts spontaneously or in response to an antiarrhythmic agent (cardioversion). - Chronic AF - The most debilitating form of AF because of its abrupt onset. It may be persistent or permanent, requires int./TX by cardioversion to sinus rhythm. Page 74 of 106 Assess: Pulses, urine output, bloodtinged sputum, EKG strip & SIGNS of STROKE (ALOC, changes in speech, motor function, or facial droop) Vitals: HR (Up to 350-600 Atrial BPM) BP (r/t Cardiac output) S/S & PHYS. EXAM: Palpitations, Dyspnea, Pulmonary edema, Signs of cerebrovascular insufficiency, fatigue, distended jug. veins, Labs: PT, PTT, INR, H&H, EKG Dx Tests: Trans-esophageal electrocardiogram (TEE) to assess for signs of clots BEFORE cardioversion. Physiologic Mapping Studies (Before MAZE procedure) Nursing Interventions: Pharm: Calcium Channel Blockers (Diltiazem), Antidysrhythmics Amioderone (Unlabeled use), & Anticoagulants (Heparin, Coumadin, Lovenox) Pt. Ed: Advise Pt on blood thinners that regular blood tests may be required, to take caution as excessive bleeding may occur. Surgery: Cardioversion, Radiofrequency Catheter Ablation (Creates scar tissue to defer abnormal pathways/rhythms of A-fib) & “Maze Procedure” (usually performed with CABG, sutures are strategically placed to prevent electrical circuits from causing AF) & Pacemaker implant. Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Decreased Cardiac Output r/t altered electrical conduction -Activity intolerance r/t decreased cardiac output Pt. Goals/ Evaluation: -Patient will display adequate cardiac output AEB Pt’s BP/HR/Rhythm are in normal parameters for the client. -Patient will participate in phys. Activity with appropriate changes in vital signs. 48 Hour Cram Sheets for Med Surg CARDIOGENIC SHOCK CARDIOGENIC SHOCK Patho: Signs and symptoms of cardiogenic shock reflects the nature of the circulation/ patho of heart failure. MI/Dysrrhythmias and Cardiomyopathies cause heart damage resulting in decreased cardiac output, BP out of artery to the vital organs. Blood flow to coronary arteries Oxygen to the heart leading to ischemia and Heart's ability to pump, thus causing inadequate perfusion of body tissues = SHOCK Assess: Signs of inadequate tissue perfusion, including: Pulse, muscle weakness, metabolic acidosis, shallow respirations, tachycardia, cool, clammy skin. Vitals: HR, BP, RR, O2/Cap. Refill, Temp. S/S & PHYS. EXAM: Anxiety, restlessness, altered mental state due to decreased cerebral perfusion and subsequent hypoxia. Hypotension due to decrease in cardiac output. Rapid/weak/thready pulse, tachycardia, Cool/clammy/mottled skin, Distended jugular veins. Oliguria Labs: ABG’s (For signs of acidosis) as well as CVP (Central Venous Pressure) Hemodynamic monitoring, H&H, CK-MB/Cardiac panel to rule out MI. Dx Tests: EKG, Echocardiogram Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Meds to reverse shock: Dopamine and dobutamine (to improve cardiac contractility), Vasopressors (Nitro), Epinepherine, Norepinepherine, Fluids (Blood/Plasma/Platelets/Crystalloids/ Colloids), Diuretics (Lasix, HCTZ), Oxygen Pt. Ed: Teach Pt. how to reduce controllable risk factors for heart disease. Encourage attendance Ensure the patient understands the medication prescribed. Surgery: Immediate re-perfusion (Pt is taken to Cardiac Cath. Lab and immediate Left sided heart catheterization, PCI (Percutaneaous Coronary Intervention) stent/balloon. *Pt. may be intubated/on ventilator for O2 support Page 75 of 106 Nursing Dx: -Altered tissue perfusion (cardiopulmonary) r/inadequate cardiac output Pt. Goals/Evaluation: Circulation status; Cardiac pump effectiveness; Tissue perfusion: Cardiopulmonary, Cerebral, Renal, Peripheral; Vital sign status *Evaluate for signs of arrhythmia/MI/Shock to prevent relapse. Assess Pt’s vital signs for values within acceptable limit. 48 Hour Cram Sheets for Med Surg CABG (Coronary Artery Bypass Graft) CABG (Coronary Artery Bypass Graft) Patho: Essentially Building a “SIDESTREET” The occluded coronary arteries are bypassed with the client’s own venous or arterial blood vessel or synthetic grafts. The internal mammary artery (IMA) is the best choice for success over a long period of time for patency. Recommended for patients that do not respond to other forms of medication and treatment Other indications include: Angina with 50% or more occlusion of main Coronary artery that cannot be stented, Acute MI/Cardiogenic shock, Ischemia with heart failure, Valvular disease, coronary arteries not suitable for Percutaneaous transluminal coronary angioplasty (PTCA), or those who have signs of ischemia or pending MI after PTCA. Page 76 of 106 Assess: Signs of anxiety, decreased cardiac output/Hemodynamics, chest pain, and feeling of impending doom. Assess pulses, heart rate, EKG and O2 perfusion, Pre/Post Op. Pt. Ed. and allergies. Vitals: O2, BP, Peripheral pulses, RR S/S & PHYS. EXAM: Pt may be grimacing, chest pain, SOB, Tacypnea, arrhythmias/elevated ST wave, JVD, ALOC Nursing Interventions: Pharm: O2, Aspirin, Heparin/ Lovenox/Coumadin, Nitro for chest pain Pt. Ed: Schedule uninterrupted rest/sleep periods, assistance with/Early ambulation, Turn, Cough, Deep breath as ordered, monitor site for signs of infection/bleeding Surgery: CABG is the surgery! AFTER CABG: Observe for ALOC, Labs: Cardiac enzymes, ABG, Cholesterol, Lipids Dx Tests: EKG, PTCA, Echocardiogram, Stress test Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: - Risk for reduced cardiac output r/t depressed cardiac function - Risk for bleeding r/t incision site/surgery - Anxiety r/t surgery/hospital stay. Pt. Goals/ Evaluation : Patient will be able to demonstrate hemodynamic stability such as stable blood pressure and adequate cardiac output 48 Hour Cram Sheets for Med Surg CHF (Congestive Heart Failure) CHF (Congestive Heart Failure) Assess: Apical pulses for Rate/Rhythm, Patho: Heart failure means the tissues of the body are temporarily not receiving as much blood and oxygen as needed. Whether acute or chronic, there is much risk associated with Heart Failure, each set of systems assoc. w/ a side of the heart (see next column) Think ANATOMICALLY: The two upper chambers are called atria and the two lower chambers are called ventricles. The right atrium and right ventricle receive blood from the body through the veins (DE-OXYGENATED) and then pump the blood to the lungs. The left atrium and left ventricle receive blood from the lungs and pump it out through the aorta into the arteries (OXYGENATED), which feed all organs and tissues of the body with oxygenated blood. Because the left ventricle has to pump blood to the entire body, the LEFT VENTRICLE a stronger pump than the right ventricle. Assess skin for pallor/cyanosis, Monitor urine output for decrease, and dark concentrated urine. ALOC Vitals: O2, HR, S/S & PHYS. EXAM: Dysrhythmias Left-sided heart failure *Dyspnea on exertion or orthopnea *Moist crackles on lung auscultation *Frothy, blood-tinged sputum *Tachycardia with S3 heart sound *Pale, cool extremities * Peripheral and central cyanosis *peripheral pulses, capillary refill time * urinary output (<30 ml/hour) *Fatigue* Insomnia/restlessness Right-sided heart failure * Dependent pitting edema (peripheral and sacral) * Weight gain * Nausea/ anorexia Jugular vein distention (JVD) * Hepatomegaly, ascites or weakness Left and right-sided heart failure: *Cardiomegaly *Vascular congestion of lung fields *Electrocardiogram identifies hypertrophy or MI/damage ABG (Arterial blood gas) studies reveal decreased partial pressure of arterial oxygen (95%), Labs: ABG, Cardiac Enzymes Dx Tests: EKG, PTCA, Echo- Nursing Interventions: Pharm: O2, Diuretics, as indicated Pt. Ed: Fluid/Sodium restriction, Combine ADL’S/Alternate breaks, Relaxation/ Stress, Surgery: Heart Transplant is ULTIMATE CHOICE, but if not, VAD (Ventricular Assist Device *usually used as a bridge until surgery), PLV (Partial Left Ventriculectomy), Endoventricular Circular Patch, Acorn Cardiac Support Device, Myosplint Pt. Goals/ Evaluation : - The patient will be able to display vital signs within acceptable limits, dysrhythmias controlled and no symptoms of failure. cardiogram, Stress test Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: - Decreased cardiac output r/t impaired cardiac function - Excessive fluid volume r/t impaired excretion of sodium and water - Impaired gas exchange r/t excessive fluid in interstitial space of lungs/alveoli Page 77 of 106 48 Hour Cram Sheets for Med Surg CAD (Coronary Artery Disease) CAD (Coronary Artery Disease) Patho: Chronic disease of the Coronary arteries, where over time plaque has built up and hardening has occurred causing a “narrowing” of the artery walls, similar to a “TRAFFIC JAM” on the freeway… LESS LANES ARE OPEN! Because of this, the built-up plaque can occlude partially (causing stable angina) or completely (Causing UNSTABLE angina). Assess: Pain, anxiety, Activity intolerance, Vitals: BP, HR , Cap. Refill time/Oxygenation S/S & PHYS. EXAM: -Angina -Nausea and vomiting -Dizziness and syncope -Diaphoresis clammy skin -Apprehension or a sense of impending doom Nursing Interventions: Pharm: Cholesterol meds (STATINS), Nitro for Chest Pain, Antiplatelets/Anti-Coagulants Pt. Ed: Healthy diet, exercise as directed by doctor Surgery: Angioplasty, Stent/Balloon placement, CABG Labs: Lipids, Cholesterol Dx Tests: Echocardiogram, Stress test, Angiogram Nursing Dx: - Acute pain related to the imbalance o myocardial oxygen supply and demand. - Ineffective tissue perfusion related to myocardial ischemia and decreased cardiac output. - Anxiety related to pain, feeling of impending doom, lifestyle changes/diagnosis of CAD. Pt. Goals/ Evaluation: Reduce pain, Prevent angina episodes by balancing rest/activity, achieve and maintain a suitable blood pressure for patient. Page 78 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg HTN (Hypertension) HTN (Hypertension) Patho: Chronic High Blood pressure due to some or a combination of many factors/Imbalances in the body. When blood volume falls or blood flow to the kidneys decreases, juxtaglomerular cells in the kidneys secrete renin into the bloodstream. In sequence, renin and angiotensin converting enzyme (ACE) act on their substrates to produce the active hormone angiotensin II, which raises blood pressure in two ways. First, angiotensin II is a potent vasoconstrictor; it raises blood pressure by increasing systemic vascular resistance. Second, it stimulates secretion of aldosterone, which increases re-absorption of sodium ions and water by the kidneys. The water reabsorption increases total blood volume, which increases blood pressure. Assess: Headache Vitals: HR BP: S/S & PHYS. EXAM: Headache, dizziness, blurred vision, nausea/vomiting, chest pain, SOB. Heart attack, CHF, Stroke or transient ischemic attack (TIA), Kidney failure, Eye damage with progressive vision loss, Peripheral arterial disease causing leg pain with walking (claudication), Aneurysms Labs: BP in all extremities, Checking regularly Dx Tests: No DX tests are necessary, except when determining secondary causes such as Renal Disease, Diabetes, and Atherosclerosis. Can use an EKG to determine the level of cardiac involvement. Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Beta Blockers (Metropolol, Atenolol, Carvedilol *BETA BLOCKERS like to LOL!! ) Diuretics (Aldactone, Furosemide, HCTZ), ACE Inhibitors, Calcium Channel Blockers, Vasdilators Pt. Ed: Monitor Blood Pressure Daily, Daily weights, side effects of meds, Modifiable risk factors Surgery: May need surgery to repair damage caused by chronic hypertension, such as aneurysm repair, kidney transplant/Dialysis, CABG Page 79 of 106 Nursing Dx: -Ineffective health maintenance r/t deficient knowledge of disease process - Risk for prone behavior r/t lack of knowledge about the disease Pt. Goals/ Evaluation: -Pt will verbalize understanding of disease process -Pt will check BP daily and report significant changes -Pt will adhere to medication regimen -Pt will adhere to ordered low salt diet and exercise regimen -Pt will change modifiable risk factors 48 Hour Cram Sheets for Med Surg HYPERLIPIDEMIA (High Cholesterol) HYPERLIPIDEMIA (High Cholesterol) Patho: Hyperlipidemia is an excess of fatty substances called lipids, largely cholesterol and triglycerides, in the blood. It is also called hyperlipoproteinemia because these fatty substances travel in the blood attached to proteins. This is the only way that these fatty substances can remain dissolved. Page 80 of 106 Assess: What is the Pt.’s diet? Any past problems/family Hx of high cholesterol? Is the Pt. Taking medication for it? Associated Diseases/Dx… Palpate pulses, assess distal pulses for circulation, assess pulses for bruit Vitals: BP S/S & PHYS. EXAM: Cholesterol/Lipid levels, May be obese, may have associated chest pain, SOB, Cap. Refill/ Circulation, Unequal pulses Labs: Total Cholesterol, HDL, LDL, Lipid Panel, Triglycerides Dx Tests: Angiogram, Echocardiogram, Stress test Nursing Interventions: Pharm: Statins! STATINS, STOP! (Atorvastatin, Simvastatin, Lovastatin) Fibric Acids (Advicor, Tricore) Pt. Ed: Modify diet/exercise, compliance with medication, report new symptoms immediately. Surgery: Stent/Balloon, CABG, angioplasty Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Inadequate perfusion of body tissues r/t interruption of vascular flow - Insufficient knowledge r/t disease process Pt. Goals/Evaluation: -Pt will verbalize understanding of healthy diet and exercise -Pt. will be able to state modifiable factors -Pt. will adhere to a specific medication regimen to reduce cholesterol levels in body 48 Hour Cram Sheets for Med Surg DIABETES TYPE I 9. ENDOCRINE DIAGNOSIS/PATHO DIABETES TYPE I Patho: Diabetes Mellitus (DM) is a chronic metabolic disorder caused by an absolute or relative deficiency of insulin, an anabolic Hormone. Type 1 diabetes mellitus can occur at any age and is characterized by the marked and progressive inability of the pancreas to secrete insulin because of autoimmune destruction of the beta cells. It commonly occurs in children, with a fairly abrupt onset; however, newer antibody tests have allowed for the identification of more people with the new-onset adult form of type 1 diabetes mellitus called latent autoimmune diabetes of the adult (LADA). These patients are dependent on exogenous insulin. Type 1 diabetes (formerly called juvenile-onset or insulin-dependent diabetes), accounts for 5% to 10% of all people with diabetes. In Type 1 diabetes, the body’s immune DATA ACTION RESPONSE Assess: For signs of hyperglycemia & hypoglycemia! Vitals: HR, BP (Longterm) S/S & PHYS. EXAM: The 3 P’s! POLURIA, POLYPHAGIA, POLYDIPSIA! Extreme thirst, frequent urination, drowsiness, lethargy, increased appetite, sudden weight loss for no reason, sudden vision changes, sugar in urine, ketones in urine, heavy or labored breathing, unconsciousness Labs: Fasting plasma glucose of 126 mg/dL or greater, Random plasma glucose of 200 mg/dL greater, Glucose tolerance test, HbA1c, ABG’s, electrolytes, Urine glucose tests, Thyroid function Dx Tests: Same as labs Nursing Interventions: Pharm: Insulin! Pt. Ed: Insulin compliance (maintain normal range!), Do not stop taking insulin if within normal range! Diet management, education on the signs of hypo/hyperglycemia, long term education for complications, foot care, med-alert bracelet, “SICK DAY RULES”: Nursing Dx: -Risk for infection r/t high glucose levels -Lack of knowledge r/t disease process *EXAMPLE of Insulin Times (See you School/Hospital book/policy): Surgery: N/A, unless organ complication as needed Simplenursing.com Less Study Time HIGHER test scores! Page 81 of 106 Pt. Goals/ Evaluation: -Pt. will take proper precautions and verbalize signs and symptoms of infection -Pt will be able to verbalize understanding of disease process and daily management regimen 48 Hour Cram Sheets for Med Surg DIABETES TYPE II system destroys the cells that release insulin, eventually eliminating insulin production from the body. Without insulin, cells cannot absorb sugar (glucose), which they need to produce energy. DIABETES TYPE II Patho: Type 2 diabetes mellitus occurs when the pancreas produces insufficient amounts of the hormone insulin and/or the body’s tissues become resistant to normal or even high levels of insulin. This causes high blood glucose (sugar) levels, which can lead to a number of complications if untreated. Type 2 diabetes is a chronic medical condition that requires regular monitoring and treatment. Treatment, which includes lifestyle adjustments, self-care measures, and sometimes medications, can control blood glucose levels in the near-normal range and Minimize the risk of diabetesrelated complications. Type 2 diabetes accounts for around 85% of all people with diabetes. Page 82 of 106 Assess: Sign of Hyperglycemia, HHS (Hyperglycemic Hyperosmolar State) Vitals: HR, BP (Longterm) S/S & PHYS. EXAM: Any symptoms of DM Type 1, recurring or hard-to heal skin, gum or urinary tract infections, drowsiness, tingling of hands and feet, itching of skin and genitals. Labs: Fasting plasma glucose of 126 mg/dL or greater, Random plasma glucose of 200 mg/dL greater, Glucose tolerance test, HbA1c, ABG’s, electrolytes, Urine glucose tests, Thyroid function Dx Tests: N/A Nursing Interventions: Pharm: Anti-diabetic drugs, insulin as needed Pt. Ed: Teach strategies to prevent HHS, Regular monitor blood glucose, adherence to insulin regimen, regular blood tests, monitor for long term effects Surgery: N/A Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Risk for infection r/t high glucose levels -Lack of knowledge r/t disease process Pt. Goals/ Evaluation: -Pt. will take proper precautions and verbalize signs and symptoms of infection -Pt will be able to verbalize understanding of disease process and daily management regimen 48 Hour Cram Sheets for Med Surg HYPOGLYCEMIA HYPOGLYCEMIA Patho: Hypoglycemia, also called low blood glucose or low blood sugar, occurs when blood glucose drops below normal levels. Glucose, an important source of energy for the body, comes from food. Carbohydrates are the main dietary source of glucose. Rice, potatoes, bread, tortillas, cereal, milk, fruit, and sweets are all carbohydrate-rich foods. After a meal, glucose is absorbed into the bloodstream and carried to the body's cells. Insulin, a hormone made by the pancreas, helps the cells use glucose for energy. If a person takes in more glucose than the body needs at the time, the body stores the extra glucose in the liver and muscles in a form called glycogen. The body can use glycogen for energy between meals. Extra glucose can also be changed to fat and stored in fat cells. Fat can also be used for energy. When blood glucose begins to fall, glucagon-another hormone made by the pancreassignals the liver to break down glycogen and release glucose into Assess: For tachycardia, diaphoresis, weakness, anxiety, ALOC Vitals: HR, BP S/S & PHYS. EXAM: COLD & CLAMMY = NEED SOME CANDY Hypoglycemia causes symptoms such as hunger, shakiness, nervousness, sweating, dizziness or lightheadedness, sleepiness, confusion, difficulty speaking, anxiety, weakness *Hypoglycemia can also happen during sleep: Some signs of hypoglycemia during sleep include: crying out or having nightmares, finding pajamas or sheets damp from perspiration, feeling tired, irritable, or confused after waking up Labs: Blood Glucose test Dx Tests: Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Glucose Tabs/Glucagon! 15g of fast- acting Carbs (fruit juice, candies, honey) Pt. Ed: Knowledge of signs and symptoms of hypoglycemia, ways to alleviate, Dietary recommendations Surgery: N/A Nursing Dx: -Risk for complications r/t low glucose levels -Risk for Infection r/t altered body functions To Help you remember… Pt. Goals/ Evaluation: -Pt will be free from complications and verbalize signs of hypoglycemia -Pt will be free from infection and verbalize signs of infection, as well as proper hand hygiene Page 83 of 106 48 Hour Cram Sheets for Med Surg HYPERGLYCEMIA the bloodstream. Blood glucose will then rise toward a normal level. In some people with diabetes, this glucagon response to hypoglycemia is impaired and other hormones such as epinephrine, also called adrenaline, may raise the blood glucose level. But with diabetes treated with insulin or pills that increase insulin production, glucose levels can't easily return to the normal range. HYPERGLYCEMIA Patho: High levels of serum glucose are excreted in the kidneys, causing glycosuria which can lead to excessive osmotic diuresis (polyuria). The impact of polyuria would cause excessive fluid loss, and followed the loss of potassium, sodium and phosphate. Due to lack of insulin the glucose cannot be converted into glycogen to increase blood sugar levels and hyper-glycemia occurs. The kidneys cannot resist hyperglycemia, and cannot filter out and absorb the amount of glucose in the blood. The sugar, which absorbs all the excess Page 84 of 106 Assess: For general appearance of patient, signs of DKA/HHS Vitals: Temp S/S & PHYS. EXAM: HOT & DRY = SUGAR HIGH, Frequency in urination, Thirst, Dry mouth, Urination at night, Drowsiness or fatigue, Loss of weight, Increase in appetite, Slow healing of wounds, Blurriness in vision, Dry and itchy skin, Rapid loss in weight, Unconsciousness, Increased confusion or drowsiness, Breathing difficulty, Dizziness when you stand up, Coma Nursing Interventions: Pharm: Depends on need!! Can take “anti-diabetic pills (Glyburide, Metformin) also INSULIN, as prescribed, many also be given in a insulin pump. Pt. Ed: Diet and exercise regimen should be followed as prescribed by doctor. Surgery: N/A Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Ineffective management of therapeutic regimen r/t deficient knowledge of disease process -Risk for unstable blood glucose r/t deviation from normal range Pt. Goals/ Evaluation: -Pt will verbalize understanding of proper care and testing of blood sugar as well as the 48 Hour Cram Sheets for Med Surg HYPERGLYCEMIA water removed with the urine is called glycosuria. In glycosuria, some water is lost in the urine, called POLYURIA. Polyuria results in intracellular dehydration, which will stimulate the thirst center so that patients will feel constantly thirsty, so the patient will continue to drink and have POLYDIPSIA. The lack of insulin production will cause a decrease in glucose transport into the cells so the cells are starved of food and stores carbohydrates, fats and proteins to be depleted. Because it is used to burn as fuel the body, then the client will feel hungry and eat, known as POLYPHAGIA. Failure to restore the body's homeostasis situation will lead to hyper-glycemia, hyperosmolar, excessive osmotic diuresis and dehydration. Central nervous system dysfunction due to transport oxygen to the brain disorder can result in a coma. Hemoconcentration increases the blood viscosity (Thickness) which may lead to the formation of blood clots, thromboembolism, cerebral infarction, heart. Labs: Blood Glucose, A1c, Glucose tolerance test Dx Tests: Same as above Simplenursing.com Less Study Time HIGHER test scores! prescribed medications to manage it -Pt will maintain blood glucose level within healthy limits of the patient’s condition. Page 85 of 106 48 Hour Cram Sheets for Med Surg DIABETIC KETOACIDOSIS (DKA) Assess: For hyperglycemia, Acetone (FRUITY) Breath, ALOC, Orthostatic Patho: Diabetic ketoacidosis is a Hypotension serious complication of diabetes Vitals: HR, BP that occurs when your body S/S & PHYS. EXAM: N/V, produces very high levels of ABD pain, Exacerbated blood acids called ketones. Polyuria, Polydipsia and Diabetic ketoacidosis develops Polyphagia, ALOC, when you have too little insulin weak/rapid pulse, Orthostatic in your body. Insulin normally hypotension, Kussmaul’s plays a key role in helping sugar respirations, blurred vision, (glucose) which is a major source headache, FRUITY BREATH!! of energy for your muscles and Labs: Blood Glucose! (CAN other tissues — enter your cells. VARY FROM 300-800MG/dL Without enough insulin, your OR MORE!) ABG’s, CBC, body begins to breaks down fat Chem 7 (To assess body for as an alternate fuel. In turn, this dehydration/shock) process produces toxic acids in Dx Tests: Same as above the bloodstream called ketones, eventually leading to diabetic ketoacidosis if untreated. DIABETIC KETOACIDOSIS (DKA) Page 86 of 106 Nursing Interventions: Pharm: REGULAR INSULIN! (IV @ 0.1 mg/kg/hr) Saline/Fluids (To make up for body losses), ELECTROLYTES as needed (ex. Potassium) Pt. Ed: Proper testing of blood sugar, verbalization on signs/symptoms of DKA. “Sick Day Rules” , Teach strategies to prevent DKA Surgery: N/A Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Imbalanced nutrition less than body requirements r/t biological factors -Knowledge deficient (learning need) r/t condition/ treatment regimen, self-care, Pt. Goals/ Evaluation: -Pt will maintain homeostasis and be free from signs of malnutrition -Pt will verbalize understanding of condition/disease process and signs/symptoms of complications 48 Hour Cram Sheets for Med Surg APPENDICITIS 10. GALLBLADDER & LIVER & APPENDIX DIAGNOSIS/PATHO Dx: APPENDICITIS Patho: Appendicitis is usually caused by blockage of the lumen of the appendix. Obstruction causes the mucus produced by mucous appendix suffered dam. The longer the mucus is more and more, but the elastic wall of the appendix has limitations that lead to increased intra-luminal pressure. These pressures will impede the flow of lymph resulting in mucosal edema and ulceration. At that time there was marked focal acute appendicitis with epigastric pain. If the flow is disrupted arterial wall infarction will occur followed by gangrene appendix. This stage is called appendicitis gangrenosa. If the appendix wall fragile, there will be a perforation, called perforated appendicitis. DATA Assess: For guarding, with pain in RLQ, Positive McBurney’s sign (Pain located the right side of abdomen, located 1/3 the distance from the anterior superior iliac spine to the umbilicus): Vitals: TEMP S/S & PHYS. EXAM: Aching pain that begins around your navel and often shifts to your lower right abdomen. The pain occurs when you apply pressure to your lower right abdomen THEN, releases the pressure on that area. When released, the Pt. will feel A LOT of pain!! (REBOUND TENDERNESS!!) Pain that worsens if you cough, walk or make other jarring movements, also Nausea, Vomiting, Loss of appetite, Low-grade fever, Constipation, Inability to pass gas, Diarrhea, Abdominal swelling Simplenursing.com Less Study Time HIGHER test scores! ACTION RESPONSE Nursing Interventions: Pharm: PAIN MANAGEMENT & ANTIBIOTICS UNTIL SURGERY!! Continue after surgery as well. Possibly blood if lost in surgery. Pt. Ed: Avoid applying heat to the area, Monitor for signs/symptoms of infection, mobility after surgery Surgery: APPENDECTOMY! **Must remove before appendix perforation– CAN CAUSE SEPTIC SHOCK!! Patient will notice a “Sudden relief of pain” which is a BAD SIGN!! Abdomen will become rigid, fever will SPIKE! Nursing Dx: -Acute pain r/t inflammation of tissues -Risk for infection r/t Inadequate primary defenses/surgery/perforation of tissues Page 87 of 106 Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Pt will show no signs of infection including: Elevated temperature, WBC count, as well as pain and swelling at incision site 48 Hour Cram Sheets for Med Surg CHOLECYSTITIS Labs: WBC, CBC, hematologic tests presurgery Dx Tests: CT scan/Ultrasound to assess for appendicitis, Assess: For RUQ Epigastric pain, jaundice, contributing factors: THE 5 F’S!! Female, Forty, Fat, Fertile, Family CHOLECYSTITIS Hx Patho: “INFLAMMATION OF THE Vitals: Temp, BP/HR (r/t Pain) GALLBLADDER” One of the most S/S & PHYS. EXAM: Nausea/ vomiting, common types of cholecystitis is Tenderness in the right abdomen, Fever, Pain acute cholecystitis. This is when that gets worse during a deep breath, Dark the onset of inflammation of the colored urine, Pain for more than 6 hours, gallbladder is sudden and intense, particularly after meals. with fast progression of the Labs: CBC, WBC, Liver Fx Tests, disease. More often than not, the Amylase/Lipase Levels inflammation is caused due to Dx Tests: Ultrasound, Hepatobiliary scan, obstruction of the bile duct, which Endoscopic Retrograde is known as calculous Cholangiopancreatography (ERCP), cholecystitis, as they are caused Cholangiography, Abdominal X-RAY due to gallstones, or cholelithiasis. There are other causes of acute cholecystitis as well, such as ischemia, chemical poisoning, motility disorders, infections with protozoa, collagen disease, allergic reactions, etc. The obstruction results in gallbladder distension, which results in edema of the cells lining the gallbladder. The lining wall of the gallbladder may eventually undergo necrosis Dx: Page 88 of 106 Nursing Interventions: Pharm: Analgesics, Antiemetics, Anticholinergics, Antibiotics, Ursodeoxyxholic Acid (Urso) to internally break up stones if possible Pt. Ed: Manage a lowfat diet & exercise program, Care of T-Tube if sent home with one, Prevent “Dumping Syndrome”: Surgery: Sphinterectomy with stone removal with ERCP, Extracorporeal Shock Wave Lithotripsy Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Acute pain r/t obstruction/spasm -Risk for deficient fluid volume r/t excessive losses due to vomiting Pt. Goals/ Evaluation: -Pt will report pain at tolerable level and verbalize ways to manage it -Pt will show evidence of adequate fluid volume by: stable vital signs, moist mucus membranes, good skin turgor, and urine output within normal level for patient 48 Hour Cram Sheets for Med Surg HEPATITIS and gangrene, which is known as gangrenous cholecystitis. Dx: HEPATITIS Patho: Inflammation that spreads to the liver (hepatitis) can be caused by infection by viruses and toxic reactions to drugs and chemicals. Basic functional units of the liver are called lobules, and these units are unique because they have their own blood supply. Disruption of the normal blood supply to the cells causes hepatic necrosis and damage to liver cells. After passing his time, the liver cells become damaged & eliminated from the body by the immune system response and replaced by new cells of a healthy liver. Therefore, most clients who have hepatitis recovered with normal liver function. (ESWL) to break up small stones, Cholecystectomy Assess: Depends on the type! Type B & C may be ASYMPTOMATIC, Type A can cause “Flu-like” Symptoms, Vitals: Fever most common S/S & PHYS. EXAM: Circulation problems (only toxic/drug-induced hepatitis), Dark urine, Dizziness (only toxic/drug-induced hepatitis), Drowsiness (only toxic/drug-induced hepatitis), Enlarged spleen (only alcoholic hepatitis), Headache (only toxic/drug-induced hepatitis),Hives, Itchy skin, Light colored feces, the feces may contain pus, Yellow skin, whites of eyes, tongue (jaundice) Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: *SPECIFIC TO TYPE AND SYMPTOMS: -Treat Symptoms for TYPE A -Anti-viral drugs for TYPE B & C: Penginterferonalpha 2B (PEGLNTRON) Pt. Ed: PREVENT SPREAD OF INFECTION! Wash hands, Vaccines for Types A & B, Avoid “High-Risk” Behaviors such as unprotected sex, sharing/using unclean needles, blood-to-blood contact, *NOT ELIGIBLE TO DONATE BLOOD Surgery: Liver transplant if eligible (Type C) Page 89 of 106 Nursing Dx: -Fatigue r/t decreased metabolic energy production -Risk for deficient fluid r/t altered clotting factors (Hep C) or vomiting/anorexia (HEP A) and altered body chemistry Pt. Goals/ Evaluation: -Pt will report increased energy and is able to participate in ADL’s - Pt will show evidence of adequate fluid volume by: stable vital signs, moist mucus membranes, good skin turgor, and urine output within normal level for patient 48 Hour Cram Sheets for Med Surg PANCREATITIS Labs: Hepatitis Virus Panel, Antibody/Antigen tests Dx Tests: Liver Biopsy Dx: PANCREATITIS Patho: Pancreatitis is an inflammatory disease, which varies in severity from mild to severe. Factors determining the severity of pancreatitis are not known. It is generally believed that the earliest events in the evolution of acute pancreatitis lead to premature intra-acinar cell activation Page 90 of 106 Assess: For contributing factors such as: 1. Excessive alcohol/drug use 2. Gallstones 3. Infection 4. Blunt Abdominal Trauma 5. Surgical trauma/manipulation Also… TURNER’s SIGN (Bruising between the last rib and the top of the hip) & CULLEN’s SIGN (Bruising of fatty tissue around umbilicus) Vitals: TEMP, HR, Sometimes BP S/S & PHYS. EXAM: Nursing Interventions: Pharm: Antibiotics, Opiod analgesics/Pain meds (Demorol is CONTRAINDICATED!), Anticholinergics, Pancreatic enzymes, Proton pump inhibitors (Omeprozole/Prilosec), TPN Pt. Ed: Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Acute pain r/t obstruction of pancreatic bile ducts/inflammation -Risk for deficient fluid volume r/t loss of fluid from vomiting/gastric suction Pt. Goals/ Evaluation: -Patient will report controlled/relief of pain, and adhere to medication regimen 48 Hour Cram Sheets for Med Surg CIRRHOSIS of digestive zymogens and that those enzymes, once activated cause acinar cell injury. Recent studies have suggested that the ultimate severity of resulting pancreatitis may be determined by events which occur subsequent to acinar cell injury. These include inflammatory cell recruitment and activation as well as the generation and release of cytokines and other chemical mediators of inflammation. Dx: CIRRHOSIS Patho: A CHRONIC liver disease characterized by an irreversible scarring of the liver. This extensive scarring causes a disruption in the normal function of the liver. The liver is a very important organ that functions in the body to help: -Store Blood Sugar (as GLYCOGEN) -Produce Bile (TO DIGEST FOOD) -Filter out toxins/wastes in blood stream (INCLUDING DRUGS/ALCOHOL) Signs and symptoms of acute pancreatitis include: -Abdominal pain to the upper quadrants, radiates to the clients back and worsens after meals -Nausea and vomiting -Tenderness on the abdomen Signs and symptoms of chronic pancreatitis include: -Upper abdominal pain -Indigestion -Sudden weight loss -Steatorrhea (oily, foul smelling stools) Labs: Liver enzymes, Bilirubin, Pancreatic enzymes Dx Tests: CT w/ contrast Assess: For signs of Jaundice/Liver failure, ALOC, Contributing factors Vitals: RR, S/S & PHYS. EXAM: EARLY STAGE: -Enlarged Liver -GI Disturbances -Jaundice -Weight Loss LATE STAGE: -Small/Nodular Liver -Ascites -Splenomegaly -Esophogeal Varices/Coughing up blood - Dyspnea - Pruitis Simplenursing.com Less Study Time HIGHER test scores! -Take Pancreatic enzymes before meals and snacks -High caloric diet/needs -NO ALCOHOL! (Refer to program as needed) -Limit fat intake -Follow up with all appts/lab work - Pt will show evidence of adequate fluid volume by: stable vital signs, moist mucus membranes, good skin turgor, and urine output within normal level for patient Surgery: N/A (Unless eligible for transplant, ALCOHOL & DRUG RELATED NOT ELIGIBLE) Nursing Interventions: Pharm: Diuretics (Lasix, Aldactone), Flagyl (to reduce bacteria in intestine), Lactulose to Ammonia, supplemental vitamins, PPI’s (Prevacid), Albumin (to decrease ascites) Nursing Dx: -Imbalanced Nurtrition: less than body requirements r/t poor nutrition and nausea/vomiting -Fluid volume excess r/t compromised regulatory mechanism and excessive fluid/ sodium intake Pt. Ed: -NO ALCOHOL! Referral to TX Program if needed -Follow Dietary guidelines for condition Pt. Goals/ Evaluation: -Pt will exhibit no further signs of malnutrition and show weight gain appropriate for body. Page 91 of 106 48 Hour Cram Sheets for Med Surg CIRRHOSIS -Manufacturing proteins in the blood that assist in clotting and oxygen transport -Helps to break down fat/produce cholesterol CONTRIBUTING FACTORS: -Excessive Alcohol (Laennec’s) -Post Necrotic (r/t Hepatitis/chemicals) -Billiary Disease -SEVERE Right-sided heart failure Page 92 of 106 - Clay colored stools, TEA colored Urine Labs: Liver enzymes, Bilirubin, H&H, hematologic testing, WBC, PLT’s, CBC, PT, INR & AMMONIA (Could indicate hepatic encephalopathy) Dx Tests: MRI/ULTRASOUND for Liver size (EARLY stages will be LARGE, Later stages of cirrhosis will be small/nodular) Remember: “If SIR ‘ROHSIS’ gets to a party EARLY, then he’s LARGE and in charge… if he gets there LATER, he will be NODDED at and SMALL” - Bleeding precautions/Risk for bleeding Surgery: Transplant (*ONLY IF ELIGIBLE!! Will not be a candidate if alcoholic/drug related) Simplenursing.com Less Study Time HIGHER test scores! -Patient will maintain stable fluid volume AEB vital signs within normal range, balanced I&O 48 Hour Cram Sheets for Med Surg ACUTE RENAL FAILURE (ARF) 11. KIDNEY (RENAL) DIAGNOSIS/PATHO ACUTE RENAL FAILURE (ARF) Patho: An acute and abrupt decrease in renal function; usually caused by: Trauma, allergic reactions, Kidney stones drug overdose and shock. REMEMBER!! Your kidneys and your Glomeruli are like your “Washing Machine”…. And wash and filter out your blood… helping excrete waste products through urine! DATA ACTION Assess: Oliguria ( 400 ml/day for onset of ARF), Then diuresis as it progresses toward recovery (4,000-5,000 ml/day) Vitals: BP, TEMP S/S & PHYS. EXAM: Dizziness, Dry mouth, hypotension, Tachycardia, Thirst, Weight loss Nursing Interventions: Pharm: TREAT THE CAUSE!! Electrolyte ImbalancesHYPERKALEMIA: Kayexalate (Usually given by enema) ANEMIA: EPOGEN (Procrit) PHOSPHATE / CALCIUM: PHOSLO, CALCUM ACETATE Diuretics (as directed) Labs: BUN, Creatinine and Potassium (Will be ), Dx Tests: Assess cause! If TRAUMA, may need CT / Ultrasound. If INFECTION, C&S (Culture and Sensitivity). If KIDNEY STONES/TUMOR, CT/MRI/Ultra- sound Pt. Ed: Adhere to diet: OLIGURIC PHASE: Protein, Potassium, Carb DIURESIS PHASE: Protein, Calorie, Restricted Fluids (As indicated), Bed rest in Oliguric Phase, Dialysis as ordered. Also…. Daily weights, Monitor I&O’s Surgery: N/A unless needed for kidney stones/trauma STAGES: Phase 1. Onset ARF begins with the underlying clinical condition leading to tubular necrosis (Ex. hemorrhage, which Simplenursing.com Less Study Time HIGHER test scores! Page 93 of 106 RESPONSE Nursing Dx: -Fluid Volume excess related to compromised regulatory mechanism (renal failure) -Risk for infection r/t altered immune functioning Pt. Goals/ Evaluation: -Fluid volume will be within normal limits for patient and homeostasis will be achieved. -Pt will show no signs or symptoms of infection prior to discharge 48 Hour Cram Sheets for Med Surg ACUTE RENAL FAILURE (ARF) reduces blood volume and renal perfusion. If adequate treatment is provided in this phase then the individual's prognosis is good. Phase 2. Maintenance A persistent decrease in GFR and tubular necrosis characterizes this phase. Oliguria is often present during the beginning of this phase. Efficient elimination of metabolic waste, water, electrolytes, and acids from the body cannot be performed by the kidney during this phase. Therefore, azotemia, fluid retention, electrolyte imbalance and metabolic acidosis occurs. The patient is at risk for heart failure and pulmonary edema during this phase because of the salt and water retention. Phase 3. Recovery Renal function of the kidney improves quickly the first five to twenty-five days of this phase. It begins with the recovery of the GFR and tubular function (BUN and serum Creatinine stabilize). Improvement in renal function may take up to a year as more nephrons regain function. Page 94 of 106 Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg CHRONIC RENAL FAILURE (CRF) Assess: For contributing factors such as: Diabetes (Leading Cause), Uncontrolled HTN, Patho: Progressive, long-term Chronic Glomerularnephritis, failure of kidney function. This is an Congenital Kidney Disease, IRREVERSIBLE condition that can only Pyelonephritis, Ethnicity (African be corrected by regular dialysis or American, Native American & kidney transplant, or will be terminal. Asian). Chronic renal failure can be present for many years before you notice any Vitals: BP symptoms. If your doctor suspects S/S & PHYS. EXAM: increased that you may be likely to develop urination (especially at night), renal failure, he or she will probably decreased urination, blood in catch it early by conducting regular the urine (not a common blood and urine tests. If regular symptom of chronic renal monitoring isn't done, the symptoms failure) urine that is cloudy or may not be detected until the tea-colored kidneys have already been damaged. MORE SERIOUS S&S: Some of the symptoms, such as Puffy eyes, hands, and feet fatigue - may have been present for (edema), High BP, fatigue, some time, but come on gradually, shortness of breath and may not be noticed or attributed loss of appetite, to kidney failure. nausea/vomiting (common symptom), thirst, bad taste in TYPES: the mouth or bad breath, weight loss, persistent itchy skin, muscle twitching or cramping, yellowish-brown tint to the skin Labs: BUN/Cr, Kidney Fxn Tests, GFR Dx Tests: Ultrasound/Biopsy CHRONIC RENAL FAILURE (CRF) Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: ANEMIA: EPOGEN (Procrit) PHOSPHATE / CALCIUM: PHOSLO, CALCUM ACETATE, also: BLOOD TRANSFUSION if necessary HEMODIALYSIS!! (Can be in hospital, or at home/Peritoneal) Nursing Dx: -Impaired urinary elimination r/t effects of disease, need for dialysis -Fatigue r/t effects of chronic anemia and uremia Pt. Ed: Monitor electrolyes, BP (For HTN), Strict I&O’s, RENAL DIET, Meticulous skin care. Dialysis Education! Based on the type, schedule, at home or in facility. Pt. Goals/ Evaluation: -Patient will maintain effective voiding measures within limits of his/her condition -Pt will state that he/she is able to accomplish ADL’s with minimal assistance by utilizing rest periods Surgery: Kidney Transplant (if needed/eligible) DIALYSIS: Page 95 of 106 48 Hour Cram Sheets for Med Surg CHRONIC RENAL INSUFFICIENCY Assess: Vitals: S/S & PHYS. EXAM: (aka, END STAGE RENAL FAILURE/ -anemia (may begin earlier than END-STAGE RENAL DISEASE) this) easy bleeding and bruising Patho: This is a long-term -Headache condition caused by several factors!! -Fatigue (more than normal or Diabetes is a common one… usual )and weakness Remember the washing machine that -Mental symptoms such as is your kidneys? Chronic high blood ALOC/confusion, inability to sugar increases the blood’s viscosity, concentrate much like putting cement in a -Nausea, vomiting, anorexia & washing machine and expecting it to thirst work the same! This “syrupy” blood -Muscle cramps, muscle can reduce blood flow, oxygen twitching transport, and necrosis. Very similar, -Nocturia HYPERTENSION can cause the same -Numb sensation in the problem. If there is too much water extremities filtering through your -Diarrhea Glomeruli/washing machine, it - Itchy skin/Eyes CANNOT work the way it needs to!! -Grayish complexion, can also be Thus causing LOW GLOMERULAR yellowish-brownish tone FILTRATION RATE (GFR). -Generalized Edema (more than Remember, ONCE THESE you had while in advanced renal GLOMERULI DIE, THEY CANNOT failure, and most likely in the HEAL AND RETURN TO NORMAL! feet and/or ankles) Causes kidney death!! -SOB (due to fluid in the lungs, anemia) End Stage Renal Disease is technically -Hypertension that last phase of the above renal CHRONIC RENAL INSUFFICIENCY Page 96 of 106 Nursing Interventions: Pharm: ANEMIA: EPOGEN (Procrit) PHOSPHATE / CALCIUM: PHOSLO, CALCUM ACETATE, also: BLOOD TRANSFUSION if necessary HEMODIALYSIS!! (Can be in hospital, or at home/Peritoneal) Nursing Dx: -Impaired urinary elimination r/t effects of disease, need for dialysis -Fatigue r/t effects of chronic anemia and uremia Pt. Ed: Monitor electrolyes, BP (For HTN), Strict I&O’s, RENAL DIET, Meticulous skin care. Dialysis Education! Based on the type, schedule, at home or in facility. Pt. Goals/ Evaluation: -Patient will maintain effective voiding measures within limits of his/her condition -Pt will state that he/she is able to accomplish ADL’s with minimal assistance by utilizing rest periods Surgery: Dialysis, Kidney Transplant (if eligible) Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg NEPHROTIC SYNDROME conditions, with manifestations and signs/symptoms usually indicating the need for dialysis and transplant. KIDNEY FUNCTION IS DOWN TO 1015% -Decreased sex drive -Decreased urine output NEPHROTIC SYNDROME Assess: Edema, usually starts with eyes), Massive Proteinuria, Pallor, Anorexia Nursing Interventions: Pharm: Corticosteroids (Prednisone), Diuretics (LASIX), Salt-poor Albumin Vitals: BP S/S & PHYS. EXAM: -Hypoalbuminemia (low level of albumin in the blood) -Proteinuria (Protein in urine) -Edema (Starts w/ eyes, then systemic, called ANASARCA) -Hypercholesterolemia (high level of cholesterol in the blood) -Hematuria (blood in urine) - Ascities - Oiliguria - Anorexia - Malaise - Nausea Pt. Ed: Maintain Diet: -SODIUM -POTASSIUM - CALORIE -Moderate PROTEIN Aeseptic techniques (To prevent infection) -Bed rest to preserve renal function -Daily Weights/ I&O’s Patho: auto-immune “Body is attacking itself”… The big “NERF BALLS OF PROTEIN” are let through the once tight-knit net of the Glomeruli. This disorder consists of PROTEIN WASTING (Proteinuria) which occurs as a result of diffuse glomelular damage. Proteinuria occurs because of changes to capillary endothelial cells, the glomerular basement membrane (GBM), which normally filters serum protein selectively by size and charge: Labs: GFR, BUN, Cr, CBC, Electrolytes Dx Tests: Biopsy, Ultrasound, CT (NO CONTRAST due to kidney fxn) Surgery: N/A Labs: Protein (For Hypoalbuminuria), CBC, Urine (HYPERalbuminuria, meaning the protein is NOT in the blood Simplenursing.com Less Study Time HIGHER test scores! Page 97 of 106 Nursing Dx: -Excess fluid volume r/t compromised regulatory mechanism -Activity intolerance r/t generalized edema Pt. Goals/ Evaluation: -Patient was able to display stable weight, vital signs within patient’s normal range, and nearly absence/ reduction of edema. 48 Hour Cram Sheets for Med Surg KIDNEY STONES where it should be, but in the Urine) Dx Tests: Kidney Biopsy KIDNEY STONES Patho: Kidney stones (renallithiasis) are small, hard deposits that form inside your kidneys. The stones are made of mineral and acid salts. Kidney stones have many causes and can affect any part of your urinary tract — from your kidneys to your bladder. Often, stones form when the urine becomes concentrated, allowing minerals to crystallize and stick together. Page 98 of 106 Assess: For passing of stones (Strain Urine), Hx or Risk for Kidney stones, Pain Mgmt Vitals: BP, HR S/S & PHYS. EXAM: Severe pain in the side and back, below the ribs, Pain that spreads to the lower abdomen and groin, Pain that comes in waves and fluctuates in intensity (SPOSMOTIC PAIN) Pain on urination, Pink, red or brown urine, Cloudy or foul-smelling urine, Nausea/vomiting, Persistent urge to urinate, Frequent urination, Fever and chills (if infection is present) Labs: Calcium, Uric Acid, Urine (For sediments/Minerals) Dx Tests: Ultrasound, CT SCAN, ABD X-ray Nursing Interventions: Pharm: NARCOTICS for PAIN MANAGEMENT!! Also FLUIDS to help Flush/Pass stone, Corticosteroids for Inflammation, as well as Antisposmotics Pt. Ed: Report increasing pain, or feeling of “Passing Stone”. Drink LOTS of fluids to promote passing. Refrain from foods that may contribute to stone formation, Foods that contain high levels of OXYLATE, including: Peanuts, rhubarb, spinach, beets, choc olate and sweet potatoes Surgery: Surgical removal of stones as needed Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Acute pain r/t Inflammation/obstruction, and abrasion of urinary tract by migration of stones. -Altered urinary Elimination Pt. Goals/ Evaluation: -Pt will report pain as “tolerable” and verbalize ways to distract themselves from pain -Pt will show an adequate urinary output for their status/condition 48 Hour Cram Sheets for Med Surg GLOMERULONEPHRITIS GLOMERULONEPHRITIS Patho: Antibody reaction SECONDARY to infection else ware inside the body. SAME INFLAMMATION, DIFFERENT CAUSE! The initial reaction is usually either an upper respiratory infection or skin infection due to group A betahemolytic Streptococcus. This leads to the formation of an antigenantibody reaction. It is followed by the release of a membrane-like material from the organism into the body’s circulation. Antibodies produced react against the glomerular tissue, thus forming immune complexes. The immune complexes become trapped in the glomerular loop and cause an inflammatory reaction in the affected Assess: Contributing Factors such as: Recent Tonsillitis, Pharyngitis or STREP! Also Flank or Abdominal Pain Vitals: BP, TEMP S/S & PHYS. EXAM: Pink or cola-colored urine from red blood cells in your urine (Hematuria), Frothy urine due to Proteinuria, Hypertension, Edema (with swelling evident in your face, hands, feet and abdomen) Fatigue (from anemia or kidney failure) Labs: BUN, Creat. WBC’s RBC’s/Hgb Urine RBC’s, Spec. Gravity Dx Tests: Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: -Penicillin (For Strep) -Corticosteroids (For inflammation) -Anti-hypertensives (For BP) Pt. Ed: Bed rest during acute phase, Patient can resume normal activities gradually as symptoms subside. Diet: Calories, Protein, Sodium, Potassium, Fluids. Hand hygiene, prevent contact with infected people. -Monitor intake and output/daily Weight -Teach Pt. to report peripheral edema or the formation of ascites. -Explain to the patient taking diuretics They may experience orthostatic hypotension and dizziness when changing positions quickly Page 99 of 106 Nursing Dx: - Acute pain r/t edema of kidney -Imbalanced Nutrition, Less than body requirements r/t anorexia/restrictive diet Pt. Goals/ Evaluation: -Pt will report pain as “tolerable” and verbalize ways to distract themselves from pain -Pt will be free from signs of malnutrition and verbalize understanding of proper diet for condition/disease process 48 Hour Cram Sheets for Med Surg GLOMERULONEPHRITIS Glomeruli. Changes in the glomerular capillaries REDUCE GFR, thereby allowing passage of blood cells and protein into the infiltrate, and reducing the amount of sodium and water that is passed into the tubules for reabsorption. This affects the vascular tone and permeability of the kidney, resulting to tissue injury. Page 100 of 106 -Light microscopy: Enlarged Glomeruli with exudation of neutrophils -Immunnofluorescent microscopy: Granular pattern of immuno-globulin deposition -Electron microscopy: reveals electron dense humps (immune complex) on the epithelial side of glomerular basal membrane Surgery: N/A Simplenursing.com Less Study Time HIGHER test scores! 48 Hour Cram Sheets for Med Surg TURP (Trans urethral resection of prostate) TURP (Trans urethral resection of prostate) Patho: The process by which the enlarged portion of the prostate (BPH) is removed by an endoscopic instrument. TURP (Transurethral Resection of the Prostate) is the most common procedure used to treat BPH. It can be carried out through endoscopy. The surgical and optical instrument is introduced directly through the urethra to the prostate, which can then be viewed directly. The gland is removed in small chips with an electrical cutting loop. This procedure, which requires no incision, may be used for glands of varying size and is ideal for patients who have small glands and for those who are considered poor surgical risks. Newer technology uses bipolar electrosurgery and reduces the risk of TURP syndrome (hyponatremia, hypovolemia).TURP usually requires an Assess: For signs of shock or blockage, monitor and maintain indwelling catheter/Irrigation, also ASSESS FOR TURP SYNDROME! (Cluster of manifestations as the result of absorbing fluids during irrigation through prostate tissue causing: ALOC, Bradycardia, Hyponatremia, N/V, Hypo/Hyper- tension) Vitals: TEMP S/S & PHYS. EXAM: -Urgency/Frequency of urination -Abdominal straining -Nocturia -Impairment of size and force of stream/ Intermittent hesitancy -Incomplete bladder emptying -Terminal dribbling -Dysuria -Eventual renal failure from urinary obstruction Labs: PSA- Prostate Specific Antigen to test for BPH Dx Tests: Digital Rectal Exam, Cytoscopy Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Narcotics for pain and to prevent/decrease bladder spasm, FOR BPH: Urinary Antibiotics, Alpha-Blocker Meds (To promote urinary flow, such as FLOMAX), Enzyme inhibitors (To decrease size of Prostate, such as AVODART / PROSCAR Pt. Ed: TURP rarely causes erectile dysfunction, but may trigger retrograde ejaculation because removal of the prostatic tissue at the bladder neck can cause seminal fluid to flow backward into the bladder rather forward through the urethra during ejaculation. Surgery: THIS IS THE SURGERY! Page 101 of 106 Nursing Dx: -Acute pain r/t incision, bladder irrigation, bladder spasms -Risk for urinary retention r/t Obstruction of urethra catheter with clots Pt. Goals/ Evaluation: -Pt will report pain as “tolerable” and verbalize ways to distract themselves from pain -Pt will show an adequate urinary output for their status/condition 48 Hour Cram Sheets for Med Surg URINARY TRACT INFECTION (UTI) overnight hospital stay. Urethral strictures are more frequent than with (non-trans-urethral procedures, and repeated procedures may be necessary because the residual prostatic tissue grows back. URINARY TRACT INFECTION (UTI) Patho: A urinary tract infection (UTI) may occur in the bladder, where it is called cystitis, or in the urethra, where it is called urethritis. Upper tract infection results in pyelonephritis. Most UTIs result from ascending infections by bacteria that have entered through the urinary meatus but some may be caused by hematogenous spread. UTIs are much common in females because the shorter female urethra makes them more vulnerable to entry of organisms from surrounding structures (vagina, periurethral glands, and rectum). Page 102 of 106 Assess: For kidney pain Vitals: TEMP (Infection) S/S & PHYS. EXAM: -Burning sensation at the start of urination -Uncomfortable pressure above pubic bone -Fullness in rectum (in men only) -Small amount of urine, despite urge to urinate (DYSURIA) -Irritability (in children only) -Abnormal eating (in children only) Nursing Interventions: Pharm: Antimicrobial (Sulfonamides, UNLESS ALERGIC!! THEN, Bactrim or Macrodantin) Pt. Ed: FLUIDS!! Also cranberry juice, WIPE FROM FRONT TO BACK!! Just think of my song… “I GOT ANOTHER UTI!... DON’T SAY I DON’T KNOW HOW TO WIPE!!” Women (You have shorter Urethras): Avoid bubble baths, VOID AFTER SEX, Wear cotton underwear. Surgery: N/A Labs: Urine C&S, WBC Dx Tests: N/A Simplenursing.com Less Study Time HIGHER test scores! Nursing Dx: -Acute Pain r/t inflammation of urinary tract -Urinary retention r/t acute condition Pt. Goals/ Evaluation: -Pt will report pain as “tolerable” and verbalize ways to distract themselves from pain -Pt will show an adequate urinary output for their status/condition 48 Hour Cram Sheets for Med Surg BPH (Benign Prostate Hypertrophy) BPH (Benign Prostate Hypertrophy) Patho: As males age, production of androgenic hormones decreases, causing an imbalance in androgen and estrogen levels and high levels of dihydrotestosterone, the main prostatic intracellular androgen. -Other causes of Benign prostatic hyperplasia (BPH) include: o Neoplasm o Arteriosclerosis o Inflammation o Metabolic Imbalance o Nutritional disturbances. Assess: DRE (Digital Rectal Exam) to check for enlargement of prostate, Assess for history/family hx of BPH Vitals: ↑TEMP S/S & PHYS. EXAM: -Urgency/Frequency of urination -Abdominal straining -Nocturia -Impairment of size and force of stream/ Intermittent hesitancy -Incomplete bladder emptying -Terminal dribbling /Dysuria -Eventual renal failure from urinary obstruction Labs: PSA- Prostate Specific Antigen to test for BPH, Urine culture, Blood test/Clotting studies Dx Tests: Digital Rectal Exam, Cytoscopy, Ultrasound Simplenursing.com Less Study Time HIGHER test scores! Nursing Interventions: Pharm: Urinary Antibiotics, AlphaBlocker Meds (To promote urinary flow, such as FLOMAX), Enzyme inhibitors (To decrease size of Prostate, such as AVODART / PROSCAR Pt. Ed: If you require TURP: Rarely causes erectile dysfunction, but may trigger retrograde ejaculation because removal of the prostatic tissue at the bladder neck can cause seminal fluid to flow backward into the bladder rather forward through the urethra during ejaculation. Surgery: TURP! Page 103 of 106 Nursing Dx: - Acute pain r/ t mucosal Irritation: bladder distention & urinary infection -Urinary retention r/t mechanical obstruction/ enlarged prostate Pt. Goals/ Evaluation: -Pt will report pain as “tolerable” and verbalize ways to distract themselves from pain -Pt will show an adequate urinary output for their status/condition 48 Hour Cram Sheets for Med Surg UTERINE FIBROIDS 12. WOMEN’s HEALTH DIAGNOSIS/PATHO UTERINE FIBROIDS Patho: Benign Fibroid tumors on the uterine muscle. Also known as “Myoma”. Can be as small as an apple seed or grow as big as a grapefruit. There could be one, or MANY. Cause is unknown, but over 80% of women have some type of fibroids in their life. DATA ACTION Assess: Location of pain (For medication and assessment of complications) On a scale of 1-10, Physical exam Vitals: Not usually, but… ↑HR (If in pain), ↓(If loosing fluid/shock) S/S & PHYS. EXAM: -Pelvic Pain -Pelvic Pressure -Hyper Menhorrhea -Pain during sex -Lower back pain -Abdominal Distension -Frequent Urination Nursing Interventions: Pharm: Analgesics for pain, Hormone therapy as needed, Antibiotic if surgery Pt. Ed: Common in young African American women, Family history of fibroids, Obese, Age 30+, and eating a lot of red meat/pork Surgery: To remove mass/part of reproductive as necessary per patients situation (Myoectomy, Hysterectomy), Endometrial Ablation, Fibroid Ablation, Uterine Fibroid Embolisation Labs: Hormone Levels, CBC, PTT/INR, H&H Dx Tests: Physical exam, ultrasound, CT scan, MRI, Hysteroscopy, hysterosalpingiogram Page 104 of 106 Simplenursing.com Less Study Time HIGHER test scores! RESPONSE Nursing Dx: -Acute Pain r/t Inflammation of Uterus -Anxiety r/t changes in health status Pt. Goals/ Evaluation: - Pt will report pain at tolerable level and verbalize ways to manage it -Client will report reduced anxiety level, ways to reduce anxiety, and understanding of diagnosis/health process 48 Hour Cram Sheets for Med Surg OVARIAN CANCER OVARIAN CANCER Patho: Cancerous growth, originating from different parts of the ovary: Contributing Factors: -Over 40 -Never been Pregnant OR -First pregnancy after 30 years of age -Family hx of ovarian, breast, or colon cancer -Hx of Dysmenorrhea or heavy breathing -Hormone replacement therapy -Infertility medication use Simplenursing.com Less Study Time HIGHER test scores! Assess: Assess for risk Factors-Over 40 y/o -Nulliparity/First pregnancy age 30+ -Family history of ovarian, breast or colon cancer -Dysmenhorrea/heavy bleeding -Hormone replacement therapy -Use of fertility medications Nursing Interventions: Pharm: Chemotherapy and Radiation as needed Pt. Ed: Genetic testing for risk, Check-up for reoccurrence (CA-125 Blood test/HE-4) , signs and symptoms of reoccurrence, side effects of chemo/medications Surgery: Surgery to remove diseased parts as needed Vitals: Normal, unless septic S/S & PHYS. EXAM: Labs: CA-125 Blood test (35 u/ml= ABNORMAL) Dx Tests: Intra-Vaginal Ultrasound, Pelvic Exam Page 105 of 106 Nursing Dx: -Anxiety r/t prognosis, lack of knowledge of disease process and threat of malignancy - Disturbed body image r/t loss of diseased body part/loss of good health Pt. Goals/ Evaluation: -Client will report reduced anxiety level, ways to reduce anxiety, and understanding of diagnosis/health process - Client will discuss concerns, what to expect after chemo/surgery, and ways to limit anxiety about body image 48 Hour Cram Sheets for Med Surg OVARIAN CANCER 13. Bibliography Ebersole, P., Hess, P., Touhy, T.A., Schmidt Logan, A., & Jett, K. (2008) Toward healthy aging: Human needs and nursing response ( 7th ed.). St. Louis, MO: Mosby. Eliopoulous C. (2009). Gerontological nursing. ( 7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Grodner, M., Long, S., & Walkingshaw,B.C. (2007). Foundations and clinical application of nutrition: A nursing approach ( 4th ed.). St. Louis, MO: Mosby. Ignatavicius, D. D., & Workman, M. L. (2010). Medical-Surgical nursing (6th ed.). St. Louis, MO: Saunders. Lowdermilk, D.L.,& Perry, S.E. ( 2007) . Maternity & women’s health care (9th ed.). St. Louis, MO: Mosby. Lehne, R.A. (2010). Pharmacology for nursing care (7th ed.). St. Louis, MO: Saunders. Lilley, L. L., Harrington, S., & Snyder, J.S. (2007). Pharmacology and the nursing process (5th ED.). St. Louis, MO: Mosby. Roach, S. S.,& Ford, S. M. (2008). Introductory clinical pharmacology. Philadelphia, PA: Lippincott Williams & Wilkins. Smeltzer, S. C., Bare, B.G., Hinkle, J. L., & Cheever, K.H. ( 2008). Brunner and Suddarth’s textbook of medical-surgical nursing ( 11th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Simplenursing.com Less Study Time HIGHER test scores! Page 106 of 106