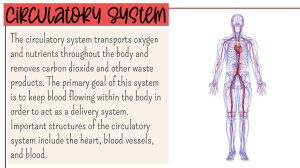
Veterinary Pathology Credit hrs 4(3+1) Wondewsen Bekele (DVM, MSc, PhD) 1 Chapter5: Circulatory Disturbances Pathology of blood circulation: – Hyperemia – Edema – Ischemia – hemorrhage – thrombosis – Infarction – Embolism – Shock CONGESTION/ HYPEREMIA Hyperemia is increased blood in circulatory system. It is of two types active • In active hyperemia blood accumulates in arteries passive • passive hyperemia the amount of blood increases in veins. 2 Circulatory Disturbances… o Etiology • As a result of inflammation. • Obstruction of blood vessels. o Macroscopic and microscopic features • Organ becomes dark red /cyanotic. • Size of organ increases. • Weight of organ increases. • Increased amount of blood in blood vessels 3 Chronic Venous Congestion in Lungs 4 Circulatory Disturbances… Haemorrhage It is escape of all the constituents of blood from blood vessels. It may occur through two processes: – rhexis- break in wall of blood vessel – diapedesis - blood leaves through widening wall of blood vessel. o Etiology • Mechanical trauma • Necrosis of the wall of blood vessels • Infections • Toxins • Neoplasm • Clotting factor deficiency (hemophilia) 5 Brain Trichinellosis petechial hemorrhages of the brain 6 Circulatory Disturbances… Macroscopic and microscopic features – Organ becomes pale due to escape of blood – ecchymoses is when diameter hemorrhage – Irregular hemorrhage on mucosal or serosal surfaces are known as suffusions. – Haemorrhage appear in line in crests or folds on mucous membrane are known as linear haemorrhage. – Hematoma is the accumulation of blood in spherical shaped mass. According to location, the haemorrhage is classified as: – Hemothorax: Blood in thoracic cavity. – Hemopericardium: Blood in pericardial sac. – Hemoperitonium: Blood in peritoneal cavity. – 7 Circulatory Disturbances… – Hemoptysis: Blood in sputum. – Hematuria: Blood in urine. – Epistaxis: Blood from nose. – Metrorrhagia: Blood from uterus. – Melena: Bleeding in faeces. – Hematemesis: Blood in vomit. – Blood constituents are seen outside the blood vessels. – Presence of red blood cells in tissues outside the blood vessels. o Forms of hemorrhages • Petechiae= pinpoint size • Purpura = small spots(<1cm in diameter) • Ecchymoses= large spots (> 1cm in diameter) • Hematoma = pouches of blood clots 8 Circulatory Disturbances… THROMBOSIS Formation of blood clot in the wall of blood vessel. – It occurs due to endothelial injury leading to accumulation • thrombocytes, • Fibrinogen • erythrocytes and leucocytes. o Etiology – Injury in endothelium of blood vessels. – Alteration in blood flow. – Alteration in composition of blood. o Macroscopic and microscopic features – Blood clot in wall of blood vessels. 9 Composition of a non-recent thrombus 10 – – – – Circulatory Disturbances… Mural thrombus is on the wall of heart. Valvular thrombus is on valves of heart. Saddle thrombus is at the bifurcation of blood vessel just like saddle on back of horse. Septic thrombus contains bacteria. EMBOLISM • Presence of foreign body in circulatory system which may cause obstruction in blood vessel. – Such particles are called embolus (emboli) o Etiology – – – – – Thrombus, Fibrin Bacteria Neoplasm Fat, Gas Parasites 11 Circulatory Disturbances… o Macroscopic and microscopic features – Emboli causing obstruction of blood vessels lead to formation of infarct in the area. – Organ/ tissue becomes pale. – Parasitic emboli e.g. Dirofilaria immitis – Presence of foreign material in blood. – Dependent area necrotic due to absence of blood supply. 12 fat emboli are seen as red dots within capillaries of the lung(200x). 13 Circulatory Disturbances… ISCHEMIA – Ischemia is deficiency of arterial blood in any part of an organ. – It is also known as local anemia. o Etiology – External pressure on artery – Narrowing/ obliteration of lumen of artery – Thrombi/emboli o Macroscopic and microscopic features – – – – Necrosis of dependent part. Occurrence of infarction. Dead tissue replaced by fibrous tissue. Lesions of infarction 14 Circulatory Disturbances… INFARCTION – Local area of necrosis resulting from ischemia. o Etiology – Thrombi – Emboli – Poisons like Fusarium toxins o Macroscopic and microscopic features – Necrosis in triangular area – Red infarct is observed as red triangle bulky surface. – Pale infarct is gray in colour and seen as triangle depressed surface. – Necrosis in cone shaped area. – Obstruction of blood vessels. 15 Circulatory Disturbances… EDEMA Accumulation of abnormal & excessive fluid in intercellular spaces and/ or in body cavity. • Normal mechanism happening in blood capillaries when pressure is regulated Two types of pressure in capillary bed – Hydrostatic pressure (push the fluid to the outside) – Oncotic pressure (fluid flow to inside) NB. If this mechanism malfunction it leads to edema in interstitial space When hydrostatic pressure increases it dominate oncotic pressure at the venous end results – minimal or no reabsorption at venous end =edema 16 Circulatory Disturbances… o Types of fluid accumulation – Ascites =fluid in peritoneum/ hydroperitonium. – Hydropericardium= fluid in pericardial sac. – Hydrocele = fluid in tunica vaginalis of the testicles. – Anasarca = generalized edema of body. – Hydrocephalus = fluid in brain. – Hydrothorax =fluid in thoracic cavity. 17 Circulatory Disturbances… o Etiology – Inflammation increased permeability of endothelium – protein malnutrition, proteinuria, reduced albumin synthesis =due to liver disease – heart failure, venous obstruction (Increased venous pressure ) – tumor blockage, resection of lymph nodes, filarial parasites (Lymphatic blockage ) Exudate – edema associated with increased vascular permeability Transudate – edema without change in vascular permeability 18 Circulatory Disturbances… o Macroscopic and microscopic features – Swelling of tissue/ organ/ body. – Weight and size of organ increased. – Colour becomes light. – Pitting impressions on pressure. – Inter cellular spaces becomes enlarged. – Serum/ fluid deposits (pink in colour on staining) in intercellular spaces. – Cells separated farther. . 19 20 Circulatory Disturbances… SHOCK It is a circulatory disturbance characterized by reduction blood supply causing: – O2 deprivation – Buildup of waste products – Eventually organ failure= death if untreated o Etiology It is classified in to: A. hypovolemic(low volume shock) it can be caused by – External blood loss = after an injury – Internal blood loss = ruptured blood vessels – Fluid loss = vomiting, diarrhea 21 Circulatory Disturbances… B. Cadiogenic shock due to – sudden heat attack – Valvular diseases C. Obstructive shock – Aorta obstruction , plumonary embolism D. Distributive shock due – to dilation of blood vessels results decrease blood pressures (infection, allergy, CNS damage) o Macroscopic and microscopic features – Acute general passive hyperemia – Dilation of capillaries – Cyanosis 22 Circulatory Disturbances… petechial haemorrhages – Edema – Capillaries and small blood vessels are distended –due to accumulation of blood. – Number of engorged blood vessels increased. – • Focal haemorrhage. • Edema, cells separated farther due to – accumulation of transudate in intercellular spaces. 23 Chapter 6: Immunopathology IMMUNOPATHOLOGY It is the disorders of immune system characterized by: increased response (hypersensitivity) response to self antigens (autoimmunity) decreased responses (Immuno deficiencies) o HYPERSENSITIVITY It is an accelerated immune response to an antigen (allergen). • The antigen is harmful to body rather than to provide protection or benefit to the body. –This condition is also known as allergy or atopy. 24 Immune pathology… A.Anaphylaxis/ Type-I Hypersensitivity(HPS) It is rapidly developing immune response to an Ag characterized by: humoral antibodies of IgE type (reagin). These reagins sensitize IgE Antibodies on the surface of a mast cell/ basophils. – causes cross-linking reactivity of cell receptor and release mediators (histamines…). HPS- doesn’t appear on first contact with the Ag, but usually occur after the immune system has already been exposed to an Ag. 25 Unusual responses – Allergy, Asthma Mediated IgE IgE Binds Mast Cells, Basophils Re-exposure Cross Links IgE 26 Immune pathology… o Etiology • Administration of drugs • Administration of serum • Bite of insects, bee etc. • Dust, pollens etc. o Macroscopic and microscopic features • Bronchial asthma. • burning reaction on skin. • erythema, itching • Rhinitis • Congestion • pulmonary edema • emphysema • constriction of bronchioles. 27 Immune dysfunction … b) TYPE II Hypersensitivity(cytotoxic) HPS II It involves Ab mediated destruction of healthy cells – HPS- II results when immune system targets: – tissue/organ with specific Ag – When there is a reaction of Ab(IgG) +Ag bind to a target cell which results: • In activation of certain mechanisms to damage target cells Eg. It occurs when incompatible blood transfusion 3 main Ab-dependent mechanisms in HPS- II Complement-dependent reaction) Ab- dependent cell mediated cytotoxicity(ADCC) Ab-mediated cellular dysfunction 28 Immune dysfunction … 1. Complement-dependent reaction i. Direct lysis: a. By complement activation formation of membrane attack complex occur • Ag- Ab initiate protein cleavage (C1 initiate C3 C3b initiating C9 attack the membrane of target cell=cell lysis b. Opsonization= By C3b, fragment of the complement to the cell surface enhances phagcytosis.. Example : – Mismatched transfused blood cells, Certain drug reaction 29 30 Immune dysfunction … 2. Ab-dependent cell-mediated cytotoxicity(ADCC) – Here antibody mediated cell injury does not involve complement fixation: • The target cells coated with IgG are killed by nonsensitized cells that have fc receptors. – The cell lysis without phagocytosis. • Example: graft rejection 3. Ab-mediated cellular dysfunction In some cases, Ab impair or deregulate function of cell surface receptors • without causing cell injury or inflammation. 31 Immune dysfunction … o Etiology • • • • • • • Blood transfusion reaction Hemolytic anemia Equine infectious anemia rickettsia Parasite( trypanosomiosis, babesiosis) transplanted kidney Drugs such as penicillin, Cephalo sporins 32 Immune dysfunction … o Macroscopic and microscopic features • Anemia • Jaundice • Haemoglobinuria • Erythrophagocytosis • Lysis of erythrocytes/ agglutination of erythrocytes. • Increased number of hemosiderin laden cells in spleen. C) Type III Hypersensitivity/ immune complex-mediated It is induced by Ag- Ab complex that produces tissue damage – as a result of activation of complement system. The antibodies involved in this reaction are IgG, IgM or IgA. 33 34 Immune dysfunction … o Etiology • Exogenous origin(bacteria, virus,fungi,parasites) • Endogeneous origin ( tumor antigen…) o pathogenesis of systemic immune complex The immune complex diseases has three phases: a. Formation of Ag-Ab complex • As the result of Ag introduction into the circulation, specific Ag-Ab formed b. Deposition of immune complexes • The formation of Ag-Ab complex in circulation does not imply presence of disease. c. Inflammatory reaction • the After deposition acute inflammatory reactions occurred. 35 Immune dysfunction … o Morphology of immune complex-mediated HPS reaction The morphologic consequences are dominated by: – Acute form results necrotizing vasculitis with neutrophilic exudation. – Chronic forms result from repeated or prolonged exposure of an antigen • Classification of immune complex-mediated diseases: • Systemic immune complexes diseases (e.g. serum sickness) • Localized diseases (e.g. Arthus reaction) – Arthur reaction is a localized area of tissue necrosis resulting from an immune 36 Immune dysfunction … o Clinical examples of systemic immune complex diseases: – Various types of glomerulonephritis – Rhematic fever – Various vasculitides – Rheumatoid arthritis 37 Immune dysfunction … d) Type IV Hypersensitivity(cell mediated) reaction It is initiated by specifically sensitized T lymphocytes It has two forms : 1. Delayed type hypersensitivity 2. T-cell mediated cytotoxicity • DTH is mediated by T-Iymphocytes has two phases: – Sensitization phase • As bacteria engulfed by macrophage or Ag presenting cells (APC’s) are forming: – Major histocompatibility complex(MHC) activating TH1 cells – Effector phase • Since once TH1cell activated producing more activated macrophage which induce hypersensitivity 38 Immune dysfunction … Example of type IV HPS are TB test, transplantation o Etiology • Tuberculin reaction • Granulomatous reaction o Macroscopic and microscopic features • Formation of nodules/ hard, painful to touch. • infiltrations of mononuclear cells (T lymphocytes and macrophages). • Congestion and oedema • Lymphocytic infiltration is common around the blood vessels 39 Immune dysfunction … Immunologic Tolerance It is incapability of immune response to specific antigens. – Self-tolerance refers to lack of responsiveness to an individual’s antigens. • Tolerance classified into two groups: – central = occurred in lymphoid organs(immature T& Blymphocytes) – peripheral tolerance=Clonal deletion by activation– induced cell death. 40 Immune dysfunction … AUTOIMMUNITY Inappropriate immune response against self components. – To distingiush b/n self(threat) /noself (safe) Autoimmune diseases- it is when immunity developed against self antigens – Which destroys the tissues of body & causes inflammation . o Etiology 1. Genetic factors 2. Immunologic factors Failure of peripheral tolerance: Breakdown of T-cell 3. Microbial agents(bacteria, mycoplasm and viruses) 4. Hormonal factors 5. Environmental factors 41 Immune dysfunction … o Macroscopic and microscopic features • Anti-glomerular basement membrane (GBM) nephritis • Lymphocytic thyroditis • antinuclear antibodies. • Hemolytic anemia • Leukopenia • Presence of antinuclear antibodies 42 Immune dysfunction … IMMUNODEFICIENCY • It is the alterations in immune system, which decrease response to various antigens. – This leads to develop immuno competence • as a result of genetic and environmental factors. • Immuno deficiencies are classified as: – congenital/primary – acquired/secondary. Congenital immunodeficiency • It is the defect of immunity genetically occurred – since from their birth. 43 Immune dysfunction … Types congenital immunodeficiency Combined immunodeficiency syndrome (CIS) • Absence of stem cells • Absence of T and B cells in blood Defects in T -lymphocytes • Thymus hypoplasia Defects in B- lymphocytes • In equines - equine a gamma globulinemia • Absence of primary lymphoid follicles • Selective IgA, IgM and IgG deficiency may also occur. • Transient hypogamma globulinemia in new born calves. Defects in phagocytosis • Neutropenia, leucopenia 44 Immune dysfunction … Acquired or secondary immunodeficiency o etiology • • • • • • • drugs diseases deficiency of nutrition neoplasm environmental pollution vaccination failures recurrent infections and occurrence of new diseases and neoplasms. 45 Chapter 7: Post Mortem Examination Techniques, Report Writing and Histopathological Techniques what is post mortem? It is a medical examination of a dead body to find out how the animal died. Histopathological examination o Sample selection and collection: The specimen should include – the typical lesion, – active margin, and adjacent unaffected/normal tissue. Only necrotic debris, often renders the specimen unsuitable for diagnosis. 46 Writing of post-mortem report (PM) PM report consists of 2 parts PM record PM examination PM record is having information related to animal and is supplied by the owner or person requesting PM examination – PM is a part of request form of the case for post mortem examination. • It is important for the identification of animals. 47 Post-mortem… Post mortem record /labelling It is necessary to have the following record s: Species (spps): such as bovine, equine, poultry, caprine, ovine etc. Age/ Born: – young, adult, in case of poultry grower, adult chick Sex Identification number/mark: the identification may be tattoo, brand number. Owner : here, the name of owner with complete address must be filled clearly. Breed : such as Jurey cattle, HF. 48 Post-mortem… Clinic name Date & time: date of the postmortem examination Case no: the serial number of your case book Referred by: in this column , the name of the veterinary officer. – Or any other officer who referred the case for PM examination – History of the case: this includes: • • • • • the clinical illness of animals Duration of illness Epidemiological data Tentative diagnosis Therapeutic and preventive measures adopted 49 Post-mortem… Histopathology techniques Sample collection Sample transport Sample accessioning/ sample receiver Tissue processing • Automated tissue processor(tissue-transfer machines and fluid-transfer machines) eg Macrotom Trimming, sectioning and labeling Haematoxyline staining 50 Post-mortem… o Types of specimen – biopsy or surgical specimen(Tissue/ organ) – Removing a piece of tissue from living animals – Autopsy – Removing of large tissue or organ from dead animals – Whole blood – Serum – Plasma – Urine – Stool – CSF – Body fluids 51 Post-mortem… o Specimen it- is a small quantity of substances which shows the kind and quality of the whole. o Purpose – To make the diagnosis and help in treatment – To note the progress and recess of the disease – To assess the general health – To investigate the nature of the disease o Universal precautions – Wear gloves – Wear face masks & gowns – Discard contaminated materials – Clean work area – Wash hand thoroughly 52 Post-mortem… Handling of Specimen * Specimen should be transported in – Glass – plastic – metal container or – a plastic bag in 10% formalin. • If formalin is not available at hand, place the specimen: – In refrigerator at 4oC to slow down autolysis. General Principle of Gross Examination: complete histopathology requisition consists: – patient’s name, age, sex, relevant clinical data, surgical findings, nature of operation and name of tissue submitted. 53 54 Post-mortem… Histological Technique: It deals with the preparation of tissue for microscopic examination. the following processes are indicated: 1. Fixation 6. staining 2. Dehydration 7.deparaffinzing 3. Clearing 4. Embedding 5. sectioning 8. cover slide 55 Post-mortem… o Fixation Should be carried out as soon as possible after removal of the biopsy or autopsy to prevent autolysis. – Most common fixative used in lab is 10% formalin. There are different groups fixatives: – Aldehydes, alcohols, oxidizing agents – The volume of alcohol should be 50- 100 times that of tissue. o Dehydration the water from the tissue must removed by dehydration. • Tissues are dehydrated by using increasing concentration of alcohol e.g. 50%, 70%, 90% and 100%. 56 Post-mortem… o Clearing It consist of removal of dehydrates with the substance that will be miscible with embedding medium. • the common clearing agent are: – xylene – toluene – methyle salicylate … o Embedding Finally the tissue is infiltrated with the embedding agent of paraffin. – paraffin provides hardness to the tissue for proper cutting. 57 Post-mortem… o Sectioning The tissue must be cutting into the sections (microtome) that can be placed into slide. Thickness of section cut in to 3-5 micrometer. – Sections are floated in warm water bath – They are picked up on microscopic slides – The glass slides are then placed in warm oven for 15min/to adhere o Staining Staining is a process by which we give colour to a section. Use paraffin wax to allow water soluble dyes to penetrate the section. 58 Post-mortem… The slides are deparaffinized by hydration step. – To remove paraffin wax immersing slide into xyline jar – Use alcohol in descending order (90%,70%,50%,30%) • Then use distilled water There are hundreds of stains available. Classification of Stains: Generally the stains are classified as: Acid stains Basic stains Neutral stains 59 Post-mortem… Acid Dyes: Acid dyes stain basic components *e.g. hematoxylin and eosin (H & E)stains cytoplasm red. • Basic Dyes: Basic dyes stain acidic components *e.g. basic fuchsin stains nucleus blue. • Neutral Dyes: When an acid dye is combined with a basic dye a neutral dye is formed. *As it contains both coloured radicals – It givesdifferent colours to cytoplasm and nucleus simultaneously. 60 Post-mortem… Staining can be done either manually or in an automatic stainer. *Haematoxylin and Eosin (H&E)staining: It is the most common used routine stain in histopathology laboratory Special Stains: 1.PAS (Periodic Acid Schiff) stain: This stain demonstrates glycogen 61 Post-mortem… 2.Stains for micro-organism: a. Gram-stain: b. Ziehl_Neelsen stain: This stain detect acid fast bacilli. c. PAS stain: It is used for fungi, amoeba and Tricomonas. d. Modified Giemsa (2% Giemsa in water): Used for Helicobacter pylori. 3.Congo-red It is used for identification of amyloid( abnormal protein accumulation). 4.Sudan-Black: It is used for fat staining. 5.Masson’s Trichrome It is used for differentiation of connective tissue 62 63