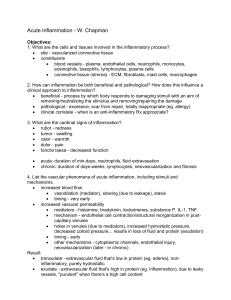
Using examples, explain five ways in which our bodies are physiologically protected from injury (defense mechanisms). 1. Physical barriers- skin, mucous membrane, hair. 2. Chemical barriers- mucous secreted by mucous membranes, saliva, gastric juice in stomach, tears, urine, sweat. 3. Inflammation. 4. Fever. 5. Immune system. Define and contrast inflammation and infection. An infection is the invasion of an organism's body tissues by disease-causing agents, their multiplication, and the reaction of host tissues to the infectious agents and the toxins they produce. Inflammation is a response of vascularized tissues to infections and tissue damage that brings cells and molecules of host defense from the circulation to the sites where they are needed, to eliminate the offending agents. Define and contrast exudation and transudation. The escape of fluid, proteins, and blood cells from the vascular system into interstitial tissues or body cavities is known as exudation. The process of passing through membrane pore or interstice known as transudation. List and explain the mechanism of production of the cardinal signs of inflammation. Heat (calor): Vasodilation leads to increase blood flow, more blood arrives, blood is warm. Redness(rubor): Vasodilation leads to increase blood flow, more blood arrives, blood is red. Swelling(tumor): increase vascular permeability lead to leakage of fluid, proteins and blood cells from vascular system to interstitial tissues lead to edema or swelling. Pain(dolor): direct damage to the nerve fibers, pressure of swelling on nerve endings, chemical irritants: histamine, bradykinin and prostaglandin. Loss of function (function laesa): increased pain and swelling. Using an example, explain the series of steps that take place in the capillary bed during an acute inflammatory process. 1- Alterations in vessel caliber resulting in increased blood flow (vasodilation) and changes in the vessel wall that permit plasma proteins to leave the circulation (increased vascular permeability). 2- The microvasculature becomes more permeable, and protein-rich fluid moves into the extravascular tissues. This causes the red cells in the flowing blood to become more concentrated, thereby increasing blood viscosity and slowing the circulation. These changes are reflected microscopically by numerous dilated small vessels packed with red blood cells, called stasis. 3- In addition, endothelial cells are activated, resulting in increased adhesion of leukocytes and migration of the leukocytes through the vessel wall. Using an example define normal and abnormal permeability at the microcirculation during inflammation. According to timing and severity: Immediate transient vascular permeability 15-30 minutes>normal Abnormal- such as a Burn- prolonged leakage and tissue damage, delayed prolonged leakage-2-12 or more hours, like a burn or radiation or bacterial toxin Severity- Endothelial damage also abnormal-high thermal injuries List and contrast the three common patterns of increased vascular permeability. 1. Retraction of endothelial cells resulting in opening of inter-endothelial spaces is the most common mechanism of vascular leakage. (Induced by histamine, other mediators. Rapid and short-lived (minutes). 2. Endothelial injury, resulting in endothelial cell necrosis and detachment. Caused by burns, some microbial toxins. Rapid; may be long-lived (hours to days). 3. Lysis of the basement membrane by collagenase released from injured endothelial cells. Describe the cellular events of inflammation. 1. Margination and rolling. 2. Adhesion. 3. Diapedesis(transmigration). 4. Chemotaxis. 5. Phagocytosis. Define chemotaxis and list four common chemotactic factors. After exiting the circulation, leukocytes move in the tissues toward the site of injury by a process called chemotaxis, which is defined as locomotion along a chemical gradient. Chemotactic factors: 1234- IL-8. C5a. Leukotriene B4. Platelet activating factor. Using an example, describe the steps involved in phagocytosis. Defining what is opsonization. (biochemical formulas are not required). Phagocytosis consists of three steps: (1) recognition and attachment of the particle to the ingesting leukocyte; (2) engulfment, with subsequent formation of a phagocytic vacuole; (3) killing and degradation of the ingested material. Some of these receptors recognize components of the microbes and dead cells and other receptors recognize host proteins, called opsonins, that coat microbes and target them for phagocytosis (the process called opsonization). Coating of bacteria with antibodies or the complement protein C3b (opsonization) elicits phagocytosis of bacteria by macrophages. List and explain the three possible mechanisms of release of leukocyte products during phagocytosis and inflammation. Reactive oxygen species- oxidative burst Nitric oxide Lysosomal products Enzymes Formation of neutrophil extracellular traps Define chemical mediation in inflammation. Explain the mechanisms of action and effects of: vasoactive amines, and plasma proteases (biochemical formulas are not required). The two vasoactive amines, histamine and serotonin, are stored as preformed molecules in mast cells and other cells and are among the first mediators to be released in acute inflammatory reactions. In humans, histamine causes arteriolar dilation and rapidly increases vascular permeability by inducing venular endothelial contraction and formation of inter-endothelial gaps. Soon after its release, histamine is inactivated by histaminase. Serotonin induces vasoconstriction during clotting. It is produced mainly in some neurons and enterochromaffin cells, and is a neurotransmitter and regulates intestinal motility. Define arachidonic acid metabolites. Give examples describing some of their actions. Conversion of arachidonic acid into prostaglandins by the enzyme cyclooxygenase-2 (COX-2). PGI2, a vasodilator and a potent inhibitor of platelet aggregation PGE2 augments pain sensitivity to a variety of other stimuli and interacts with cytokines to cause fever. Conversion of arachidonic acid to leukotrienes by lipoxygenase. 1. 2. 3. 4. Increased vascular permeability Leukotrienes C4, D4, E4 Classify inflammatory exudates. Give examples. Serous- ↓protein ↑fluid →skin bruises Fibrinous→ fibrinous pericardis Catarrhal- mucus →common cold Suppurative (Purulent)- pus →skin boils (dead neutrophils, organisms, necrotizing cells) 5. Hemorrhagic Define cytokines. Give examples including their effects. TNF and IL-1 stimulate the expression of adhesion molecules on endothelial cells, resulting in increased leukocyte binding and recruitment, and enhance the production of additional cytokines (notably chemokines) and eicosanoids. Mention in details the possible outcomes of acute inflammation. 1. Complete resolution: Neutralize chemicals- elimination of offending agent Mediators disappear- normalization of permeability Apoptosis of neutrophils Lymphatic draining [Healing – labile cells regenerate all the time while stable cells regenerate when needed] 2. Abscess: (if not drained) Sinus fistula – chronic abscess Lymphangitis- vessles, lymphadenitis- lymph nodes Toxemia, septicemia, bacteremia Septic thrombophlebitis Septic emboli 3. Healing by scaring: Need ↓blood/ function less cell 4. Spread 5. Chronic inflammation Define: abscess, empyema and two other special forms of inflammation. Abscesses are focal collections of pus that may be caused by seeding of pyogenic organisms into a tissue or by secondary infections of necrotic foci. Empyema; suppurative material may accumulate in the pleural cavity. Describe different morphological patterns of acute inflammation. 1- Serous inflammation- characterized by the outpouring of a watery, relatively protein-poor fluid that, depending on the site of injury, derives either from the plasma or from the secretions of mesothelial cells lining the peritoneal, pleural, and pericardial cavities. Example: the skin blister resulting from a burn or viral infection. 2- Fibrinous inflammation- occurs as a consequence of more severe injuries, resulting in greater vascular permeability that allows large molecules (such as fibrinogen) to pass the endothelial barrier. 3- Suppurative (purulent) inflammation and abscess formation. These are manifested by the collection of large amounts of purulent exudate (pus) consisting of neutrophils, necrotic cells, and edema fluid. Abscesses are focal collections of pus that may be caused by seeding of pyogenic organisms into a tissue or by secondary infections of necrotic foci. Certain organisms (e.g., staphylococci) are more likely to induce such localized suppuration and are therefore referred to as pyogenic (pusforming). 4- An ulcer is a local defect, or excavation, of the surface of an organ or tissue that is produced by necrosis of cells and sloughing (shedding) of necrotic and inflammatory tissue Define and contrast: bacteremia, septicemia, toxemia. Bacteremia: Presence of bacteria in blood stream. Septicemia: blood poisoning by bacteria. Toxemia: Presence of toxic substance in the blood. List three common possible defects in leukocyte function that may affect the Inflammatory response (use examples). Defect in adhesion (Leukocyte Adhesion Deficiency) Chronic granulomatous disease (defective in phagocytosis) Chediac Higashi syndrome (problem in trafficking inside the cells) MPO deficiency which will effect the inflammatory response Describe the role of lymphatics in inflammation. Lymphatics drain the small amount of extravascular fluid that seeps out of capillaries under normal circumstances. In inflammation, lymph flow is increased to help drain edema fluid that accumulates because of increased vascular permeability. In addition to fluid, leukocytes and cell debris, as well as microbes, may find their way into lymph. Lymphatic vessels, like blood vessels, proliferate during inflammatory reactions to handle the increased load. 123- List three systemic effects of inflammation. Increased blood pressure Fever Sepsis