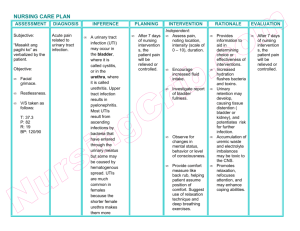
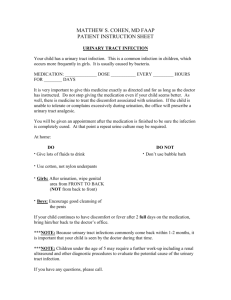
Urinary Tract Infection (UTI) 1. Definition: • A bacterial infection affecting any part of the urinary system, including the kidneys, bladder, ureters, and urethra. 2. Etiology: • Mainly caused by the invasion of pathogenic bacteria into the urinary tract. • Common causative agents include Escherichia coli (E. coli), Klebsiella, and Enterococcus. 3. Risk Factors: • Female gender (due to shorter urethra). • Urinary tract abnormalities. • Catheterization. • Sexual activity. • Diabetes. • Immunodeficiency. • Advanced age. • Obstruction in the urinary tract. 4. Manifestations: • Urgency and frequency of urination. • Dysuria (painful urination). • Hematuria (blood in the urine). • Lower abdominal pain or discomfort. • Fever and chills. • Cloudy or foul-smelling urine. 5. Diagnostic Tests: • Urinalysis: Detects the presence of white blood cells, bacteria, and other abnormalities. • Urine Culture and Sensitivity: Identifies the specific bacteria and determines antibiotic sensitivity. • Blood tests: Elevated white blood cell count indicating infection. • Imaging studies (if needed): To identify structural abnormalities. 6. Medical Management: • Antibiotic therapy: Targeted at the specific bacteria identified in urine culture. • Analgesics: To alleviate pain and discomfort. • Increased fluid intake: Flushes bacteria from the urinary system. • Antipyretics: For fever management. 7. Nursing Interventions: • Promote Hydration: Encourage increased fluid intake to flush out bacteria. • Administer Medications: Ensure timely and correct administration of prescribed antibiotics and analgesics. • Monitor Vital Signs: Especially temperature, to assess response to treatment. • Educate on Personal Hygiene: Emphasize the importance of maintaining good perineal hygiene. • Encourage Complete Antibiotic Course: Stress the importance of finishing the entire prescribed antibiotic course. • Assess and Manage Pain: Implement strategies to alleviate dysuria and discomfort.