Chapter 22 Respiratory System
I. Intro
1. Respiratory & circulatory coupled
Respiratory
Phys:
O2 into lungs
Circulatory
blood exchange of
O2
Pulmonary
ventilation adults
12-15x/min
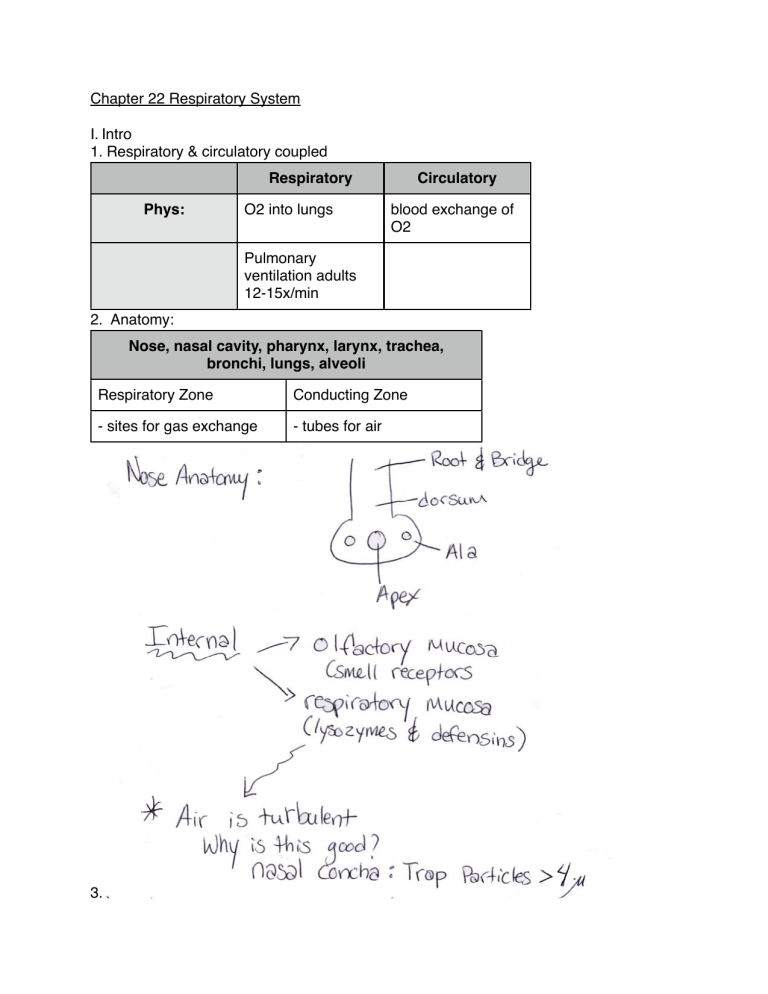
2. Anatomy:
Nose, nasal cavity, pha
arynx, larynx, trachea,
bronchi, lun
ngs, alveoli
Respiratory Zone
Conducting Zone
- sites for gas exchange
- tubes for air
3.
4. Pharynx “throat” (Connects nasal cavity to esophagus)
5. Larynx “voice box”
- connected by hyoid & trachea
- functions: opens airway for trachea
: voice production { tighter cords = higher pitch
- anatomy: 9 cartilages
6. Trachea
- cartilage rings hold open
- cilia - removes foreign objects
- factoid: coughing gives 100 mph air to rid food.
7. Bronchial subdivisions
- alveoli = air sacs at ends of bronchioles
- 300 million/lung
- squamous epithelial
- covered with pulmonary capillaries
2 Types of Alveoli Cells
Type 1
Type 2
Squamous epithelial
Cuboid epithelial
Respiratory membrane: gas exchange
(O2/CO2)
Secrete surfactant for lubrication
* alveoli macrophages - destroys airborne
* factoid - swallow 2 million per hour
II. Mechanics of Breathing
Inspiration = air into lungs
Expiration = air out of lungs
A. Intrapulmonary pressure = pressure in ALVEOLI
[760 mm Hg = 1 atm = atmospheric pressure]
Intrapleural pressure = pressure in pleural cavity
[ 756 mm Hg ] = - 4 mm Hg
* Gas goes from Hi -----> Lo pressure = pressure gradient
B. Boyles Law
Inspiration
Expiration
Ribs & sternum move upward &outward
Ribs & sternum move in & down
Diaphragm down therefore
intrapulmonary pressure goes down &
volume goes up
Diaphragm up therefore intrapulmonary
pressure goes up & volume goes down
Air rushes in
Air rushes out to restore lower pressure
(Change?) P = difference in pressure between atmosphere & alveoli
P
- amount of gas flowing into & out of alveoli depends on
D. Surfactant (Type II alveolar cells)
= Decreased surface tension of alveolar fluid } to allow air flow
* premature births - not enough surfactant (alveoli close)
* IRDS = Infant Respiratory Distress Syndrome
P
E. Lung Compliance = Measure of how much lung volume changes with
- more compliant, better
C.
- determined by 3 factors:
1. Surfactant (smoking)
2. Resilience of lung (Fibrosis
3. Respiratory passages (bronchitis)
III. Respiratory Volumes
A. Terms
a. Tidal Volume (500 mL) = normal air in & out of lungs (quiet breathing)
b. Inspiratory V (2100 - 3200 mL) = amt of air that can be inspired forcibly [after tidal]
c. Expiratory V = amout of air that can be expelled forcibly [after tidal] (1200 mL)
d. Residual V = amt of air left no matter what (~ 1200 mL)
e. Total lung capacity -- Max air held
Males 6000 mL
Females 4200 mL
* Spirometer = forced vital capacity [forced exhaled air]
forced VITAL = TV + IRV + ERV = 80% TLC
IV. Transport in respiratory gases: In blood
A. Oxygen Transport
- Dissolved in blood (1.5%)
- Hemoglobin (RBC) [ 98.55]
a. Hemoglobin:
a. Hemoglobin + Oxygen = oxyhemoglobin (HbO2)
w/o O2 = reduced Hemoglobin
b. Hemoglobin hold up to 4 O2
* NO (nitrous oxide) ----> Vasodilates capillaries
c. Hb holds on th most O2 even after tissue exchange
e.g. arterial blood 20% O2 vol.
venous blood 15% O2 vol.
Therefore: much O2 always on reserve
WHY?????
d. oxygen - Hb dissociation curve: Hb affinity for O2 (sponge)
e. ^ CO2; ^ Temp: v pH
- makes sense : ^ metabolism, ^ acid by-products & heat
Therefore: need more O2 so Hb gives it up.
* Hypoxia - Inadequate O2 to tissues
---> CO poinsoning: CO is 200x stickier to Hb than O2
- rosy cheeked
- Treat 100% O2 or hyperbaric therapy [ hi PO2]
III Carbon Dioxide
a. Bound to Hb (20%)
(Carbaminohemoglobin = HbCO2)
b. In blood (7 - 10%) - dissolved
c. In blood (bicarbonate: HCO3 -)
In RBCs
70%
* In Blood: HCO3- Moves quickly out of RBC into blood & RBC takes in Cl- to
compensate for loss = Chloride shift
* In Lungs: reverse chloride shift
- HCO3- enters RBC [Cl- out] & becomes H2CO3 <-------> CO2 + H20
B. Basic Properties of gasses:
a. Gases move from areas of Hi partial pressure to Low partial pressure [see:
Daltons Law; Henrys Law]
b.
c. O2 -------- 5% solubility
CO2 ------ Very soluble > 90%
N2 -------- insoluble in blood (bends)
d. Ventilation perfusion coupling
- pulmonary capillary + bronchiole dilate in areas where Pressure of O2 in
alveolus is Hi to maximize gas exchange & constrict where pressure of O2 are
Low
e. Gas transport by diffusion across respiratory membrane (.5 - 1.0 micrometers)
* Surface area of lungs = 60 m2
C. Haldane Effect
In blood: the Lower the O2 in blood, the more the CO2 able to be carried in
blood.
Why? ^ CO2 disolved ----> more H+
v Hb affinity for O2
REVIEW
D. CO2 & Blood pH
What happens
v O2 Intake
VI. Imbalances of respiratory system
a. Chronic Obstructive Pulmonary Disease (COPD)
Obstructive Emphysema
Deteriorated alveoli
Chronic Bronchitis
excess mucous +
infections
Asthma
Inflammation of air
passageways
Lungs less elastic
(collapse after exhalation)
Immune reaction
Therefore requires 15 - 20
% more in/exhalation
^ 2 x deaths
New trend: shift to steroids
b. Lung Cancer
- 1/3 cancer deaths ( > 90% patients smokers)
- 5 yr survival rate
- 3 types
Squamous Cell
Carcinoma
Bleeding mass
Adenocarcinoma
- Develop from bronchial
glands or alveoli
- Peripheral Masses
Small Cell Carcinoma
most responsive to chemo
c. High altitudes
a. 0-8000 ft. - no problem
> 8000 ft. - air density too low w/ abrupt changes = acute mountain sickness
b. Long term acclimatization
1. more RBCs made
2. More NO released from Hb therefore vasodilation
3. ^ Lung capacity
V. Respiratory Controls
A. Neurons of reticular formation:
in: Medulla
+ respiration
Pons
- respiration
B. Hypothalamus:
Emotion sensed here to affect respiration
C. CO2 level affects respiration rate:
- CO2 releases H+ in CSF ---> Stimulates chemoreceptors in reticular formation
to ^ respiration (see chart)